Is Biportal Endoscopic Spine Surgery More Advantageous Than Uniportal for the Treatment of Lumbar Degenerative Disease? A Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Surgical Technique of Biportal Endoscopy
2.2. Literature Search
2.3. Inclusion Criteria
- (1)
- Research type: randomized controlled trials (RCTs) and retrospective/prospective cohort or case–control studies
- (2)
- Patients with lumbar degenerative disease (LDH/LSS) with indications for surgery
- (3)
- Comparison of clinical results between uniportal endoscopic and biportal endoscopic decompression in treating lumbar degenerative disease (LDH/LSS)
- (4)
- Articles with at least one of the following results: primary results including pain intensity (Visual Analog Scale [VAS] scores) and disability (Oswestry Disability Index [ODI] scores), or secondary results including operation time, intraoperative estimated blood loss, length of hospital stay, and complications.
2.4. Exclusion Criteria
- (1)
- Non-English and non-Chinese studies
- (2)
- Studies that have not been peer-reviewed or those without relevant data, such as case series, conference reports, letters, and reviews
- (3)
- Repeatedly published data
- (4)
- Patients with serious cardiovascular and cerebrovascular diseases, mental diseases, malignant tumors, etc.
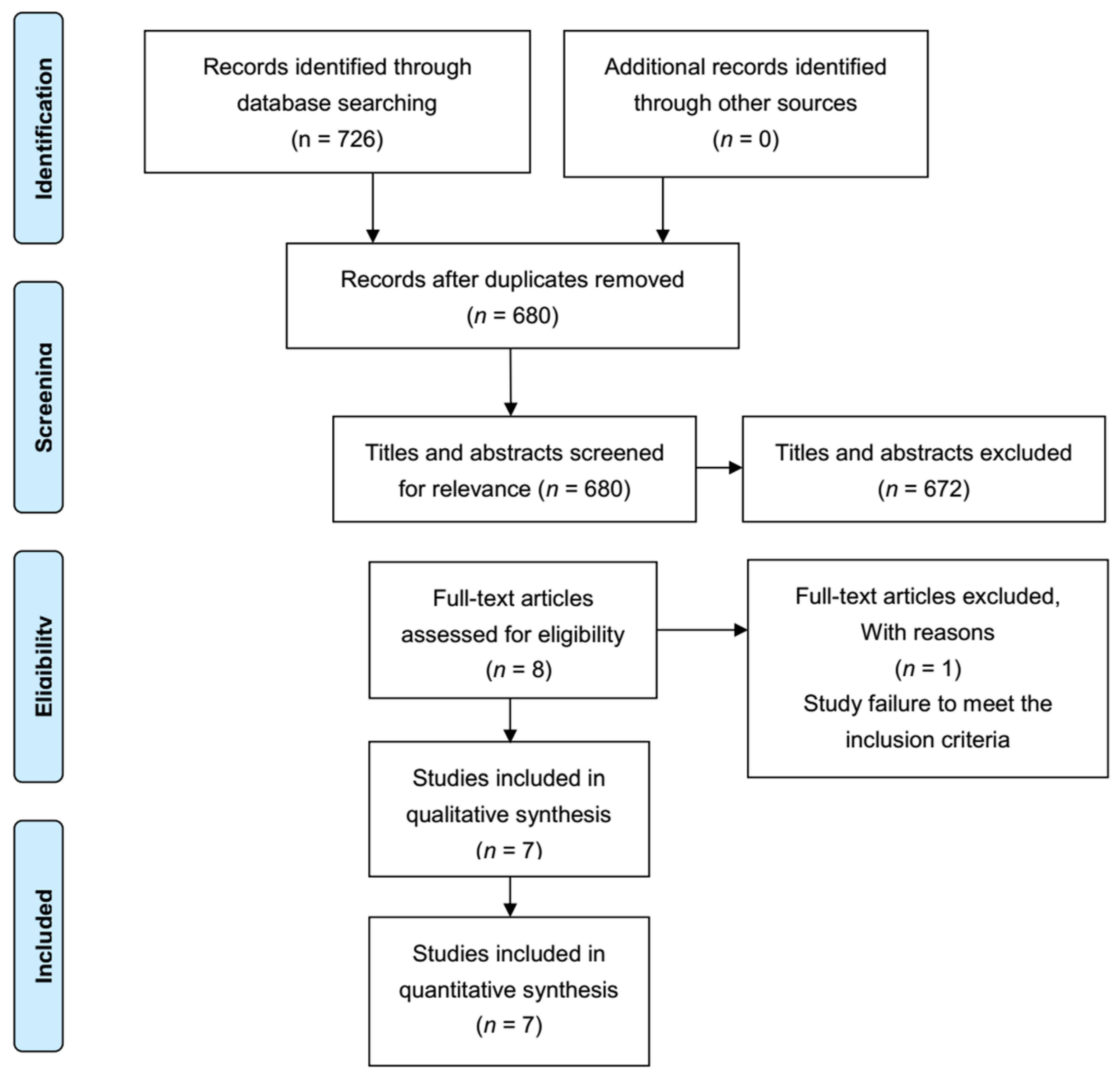
2.5. Study Selection
2.6. Risk of Bias within Included Articles
2.7. Data Extraction
2.8. Data Analysis
3. Results
3.1. Description of Articles
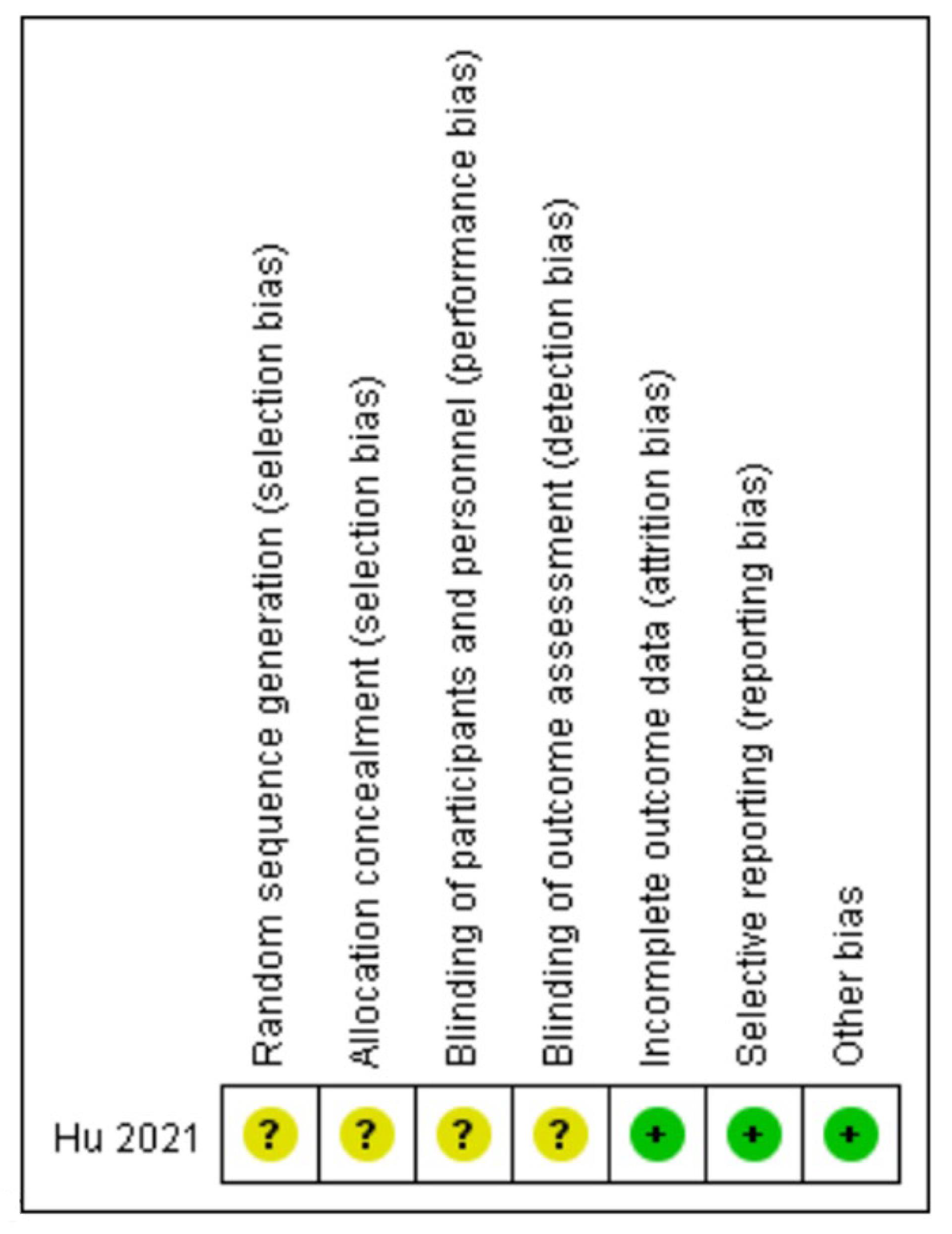
3.2. Quality Evaluation
3.3. Meta-Analysis Results
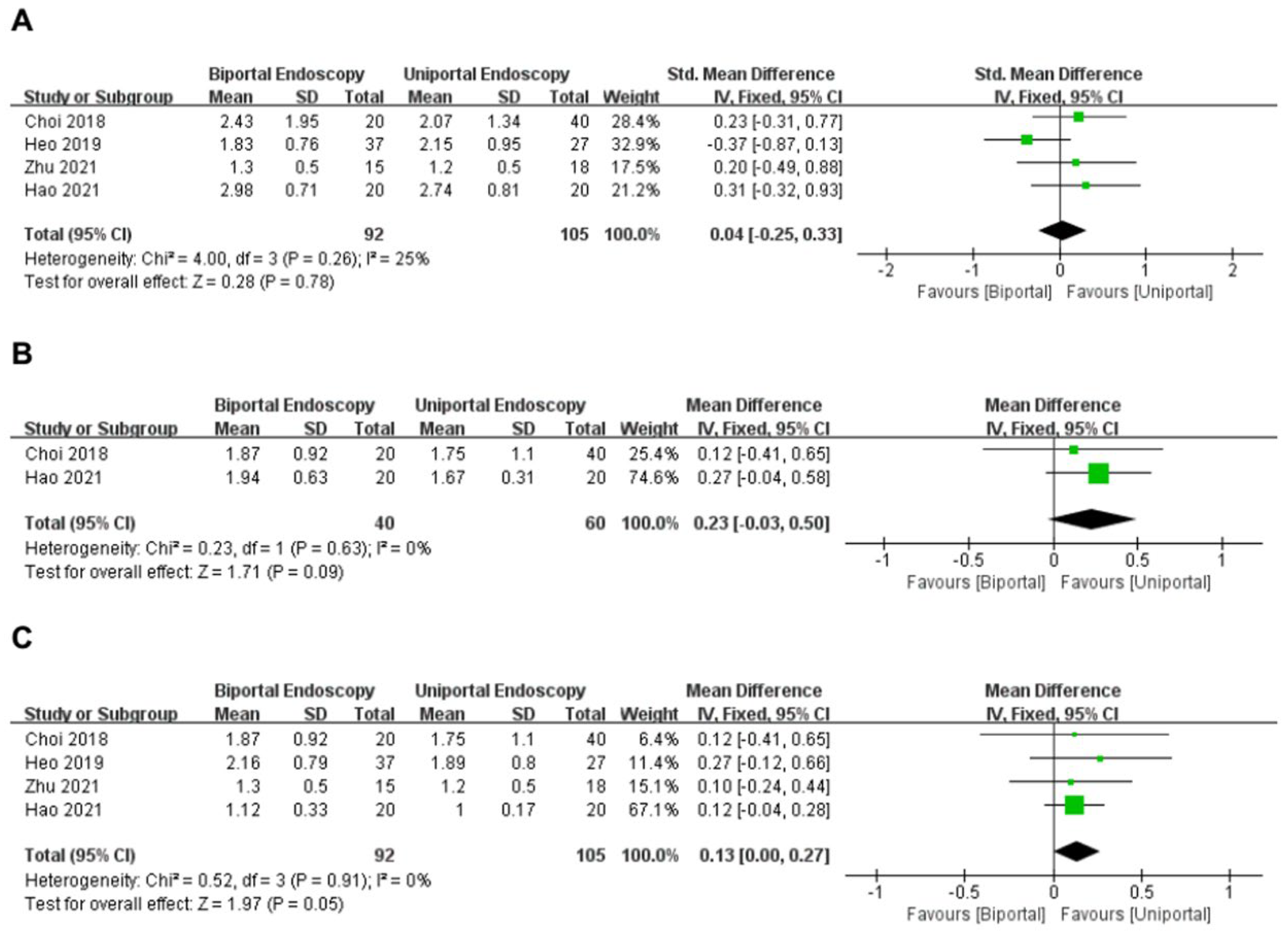
3.3.1. VAS for Back (within 3 Days)
3.3.2. VAS for Back (within 3 Months)
3.3.3. VAS for Back (Last Follow-Up)
3.3.4. VAS for Leg
3.3.5. ODI
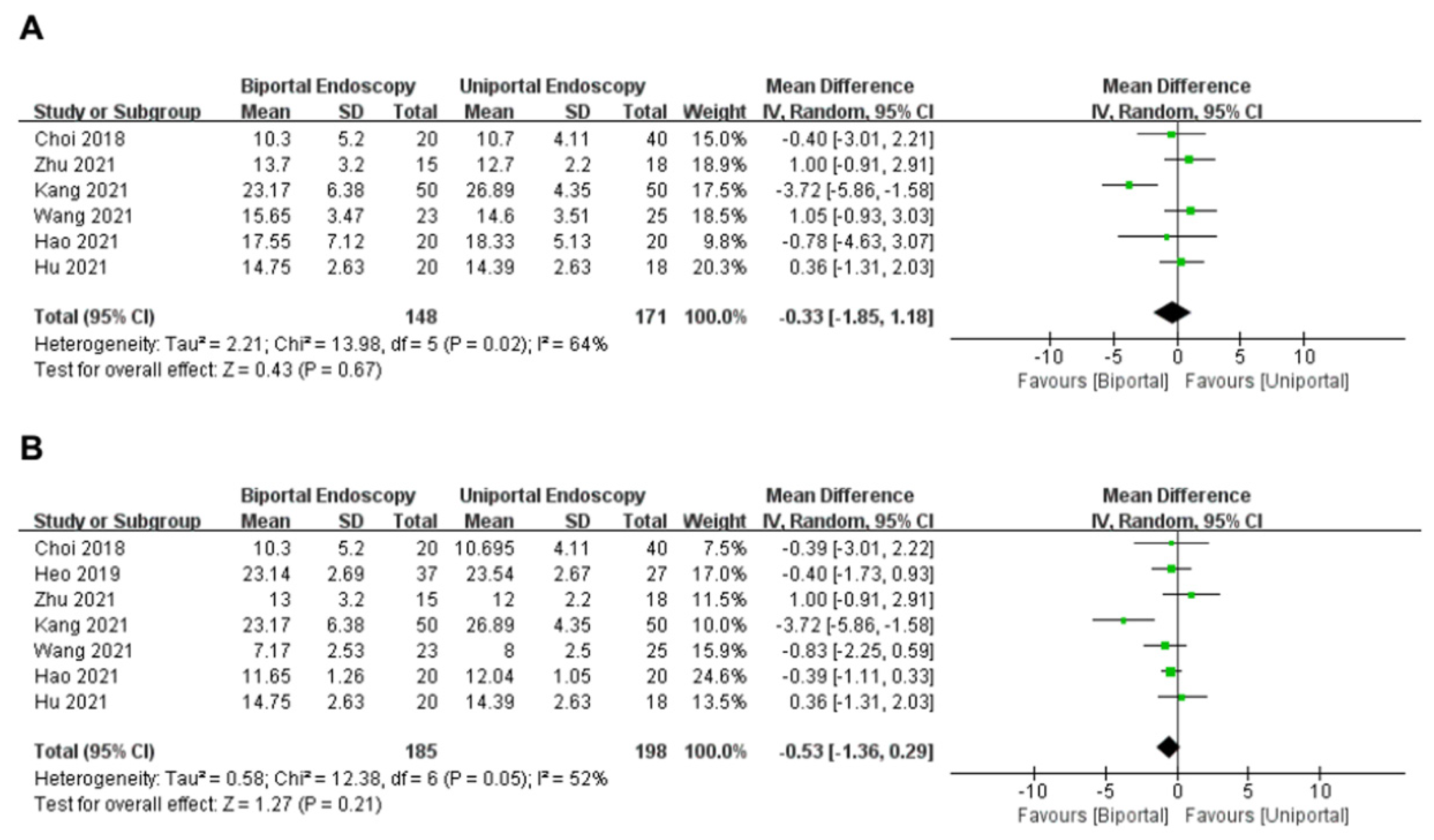
3.3.6. Operation Time
3.3.7. Length of Hospital Stay
3.3.8. Complications
3.3.9. Intraoperative Estimated Blood Loss
3.4. Sensitivity Analysis
3.5. Publication Bias
4. Discussion
4.1. Perioperative Data
4.2. VAS Score and ODI
4.3. Complication
4.4. Limitations and Strength
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Buser, Z.; Ortega, B.; D’Oro, A.; Pannell, W.; Cohen, J.R.; Wang, J.; Golish, R.; Reed, M.; Wang, J.C. Spine Degenerative Conditions and Their Treatments: National Trends in the United States of America. Glob. Spine J. 2017, 8, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Abdu, W.A.; Sacks, O.A.; Tosteson, A.N.; Zhao, W.; Tosteson, T.D.; Morgan, T.S.; Pearson, A.; Weinstein, J.N.; Lurie, J.D. Long-Term Results of Surgery Compared With Nonoperative Treatment for Lumbar Degenerative Spondylolisthesis in the Spine Patient Outcomes Research Trial (SPORT). Spine 2018, 43, 1619–1630. [Google Scholar] [CrossRef] [PubMed]
- Pan, L.; Zhang, P.; Yin, Q. Comparison of tissue damages caused by endoscopic lumbar discectomy and traditional lumbar discectomy: A randomised controlled trial. Int. J. Surg. 2014, 12, 534–537. [Google Scholar] [CrossRef] [PubMed]
- Jacquot, F.; Gastambide, D. Percutaneous endoscopic transforaminal lumbar interbody fusion: Is it worth it? Int. Orthop. 2013, 37, 1507–1510. [Google Scholar] [CrossRef] [PubMed]
- Choi, D.-J.; Kim, J.-E. Efficacy of Biportal Endoscopic Spine Surgery for Lumbar Spinal Stenosis. Clin. Orthop. Surg. 2019, 11, 82–88. [Google Scholar] [CrossRef]
- Heo, D.H.; Quillo-Olvera, J.; Park, C.K. Can Percutaneous Biportal Endoscopic Surgery Achieve Enough Canal Decompression for Degenerative Lumbar Stenosis? Prospective Case–Control Study. World Neurosurg. 2018, 120, e684–e689. [Google Scholar] [CrossRef]
- Kang, T.; Park, S.Y.; Kang, C.H.; Lee, S.H.; Park, J.H.; Suh, S.W. Is biportal technique/endoscopic spinal surgery satisfactory for lumbar spinal stenosis patients?: A prospective randomized comparative study. Medicine 2019, 98, e15451. [Google Scholar] [CrossRef]
- Min, W.-K.; Kim, J.-E.; Choi, D.-J.; Park, E.J.; Heo, J. Clinical and radiological outcomes between biportal endoscopic decompression and microscopic decompression in lumbar spinal stenosis. J. Orthop. Sci. 2020, 25, 371–378. [Google Scholar] [CrossRef]
- Kim, J.-E.; Choi, D.-J.; Park, E.J.J.; Lee, H.-J.; Hwang, J.-H.; Kim, M.-C.; Oh, J.-S. Biportal Endoscopic Spinal Surgery for Lumbar Spinal Stenosis. Asian Spine J. 2019, 13, 334–342. [Google Scholar] [CrossRef]
- Choi, C.-M. Biportal endoscopic spine surgery (BESS): Considering merits and pitfalls. J. Spine Surg. 2020, 6, 457–465. [Google Scholar] [CrossRef]
- Lixing, K.; Sumei, Y.; Peng, Z.; Yani, G.; Weiliang, D.; Zichao, J. Comparison of clinical efficacy of single channel, unilateral double channel and bilateral three channel spinal endoscopy in the treatment of lumbar spinal stenosis. J. North Sichuan Med. Coll. 2021, 36, 1323–1328. [Google Scholar]
- Hongjian, W.; Zhipeng, W. Comparison of single channel-spinal endoscopy (Delta) and unliateral biportal endoscopic technique for the treatment of senile lumbar spinal stenosis. J. Xi’an Jiaotong Univ. 2021, 42, 797–801. [Google Scholar]
- Hu, T.-H.; Xu, W.-X. Efficacy of unilateral biportal endocopic spinal surgery for the treatment of highly free disc herniation. Zhejiang Clin. Med. J. 2021, 23, 499–501. [Google Scholar]
- Chengyue, Z.; Wenshuo, G.; Hao, P. A comparison of clinical efficacy of percutaneous endoscopic interlaminar discectomy and unilateral biportal endocopic discectomy in treatment of L5-S1 lumber disc herniation. Jinagsu Med. J. 2021, 47, 996–1000. [Google Scholar]
- Choi, K.-C.; Shim, H.-K.; Hwang, J.-S.; Shin, S.H.; Lee, D.C.; Jung, H.H.; Park, H.A.; Park, C.-K. Comparison of Surgical Invasiveness Between Microdiscectomy and 3 Different Endoscopic Discectomy Techniques for Lumbar Disc Herniation. World Neurosurg. 2018, 116, e750–e758. [Google Scholar] [CrossRef]
- Heo, D.H.; Lee, D.C.; Park, C.K. Comparative analysis of three types of minimally invasive decompressive surgery for lumbar central stenosis: Biportal endoscopy, uniportal endoscopy, and microsurgery. Neurosurg. Focus 2019, 46, E9. [Google Scholar] [CrossRef]
- Hao, J.; Cheng, J.; Xue, H.; Zhang, F. Clinical comparison of unilateral biportal endoscopic discectomy with percutaneous endoscopic lumbar discectomy for single l4/5-level lumbar disk herniation. Pain Pract. 2021, 22, 191–199. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions; Cochrane: London, UK, 2021; Available online: www.training.cochrane.org/handbook (accessed on 21 November 2021).
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gotzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Healthcare Interventions: Explanation and Elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (prisma-p) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef]
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef]
- Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef] [PubMed]
- Choi, D.-J.; Choi, C.-M.; Jung, J.-T.; Lee, S.-J.; Kim, Y.-S. Learning Curve Associated with Complications in Biportal Endoscopic Spinal Surgery: Challenges and Strategies. Asian Spine J. 2016, 10, 624–629. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-E.; Choi, D.-J.; Kim, M.-C.; Park, E.J. Risk Factors of Postoperative Spinal Epidural Hematoma After Biportal Endoscopic Spinal Surgery. World Neurosurg. 2019, 129, e324–e329. [Google Scholar] [CrossRef] [PubMed]
- Kang, M.-S.; Chung, H.-J.; Jung, H.-J.; Park, H.-J. How I do it? Extraforaminal lumbar interbody fusion assisted with biportal endoscopic technique. Acta Neurochir. 2021, 163, 295–299. [Google Scholar] [CrossRef]
- Kang, M.S.; Park, H.J.; Hwang, J.H.; Kim, J.E.; Choi, D.J.; Chung, H.J. Safety Evaluation of Biportal Endoscopic Lumbar Discectomy: Assessment of Cervical Epidural Pressure During Surgery. Spine 2020, 45, E1349–E1356. [Google Scholar] [CrossRef]
- Schubert, M.; Hoogland, T. Endoscopic transforaminal nucleotomy with foraminoplasty for lumbar disk herniation. Oper. Orthop. Und Traumatol. 2005, 17, 641–661. [Google Scholar] [CrossRef]
- Gadjradj, P.S.; Harhangi, B.S. Percutaneous Transforaminal Endoscopic Discectomy for Lumbar Disk Herniation. Clin. Spine Surgery A Spine Publ. 2016, 29, 368–371. [Google Scholar] [CrossRef]
- Hwa Eum, J.; Hwa Heo, D.; Son, S.K.; Park, C.K. Percutaneous biportal endoscopic decompression for lumbar spinal stenosis: A technical note and preliminary clinical results. J. Neurosurg. Spine 2016, 24, 602–607. [Google Scholar] [CrossRef]
- Aydın, Y.; Ziyal, I.M.; Duman, H.; Türkmen, C.S.; Başak, M.; Şahin, Y. Clinical and radiological results of lumbar microdiskectomy technique with preserving of ligamentum flavum comparing to the standard microdiskectomy technique. Surg. Neurol. 2002, 57, 5–13. [Google Scholar] [CrossRef]
- Altun, I.; Yüksel, K.Z. Histopathological Analysis of Ligamentum Flavum in Lumbar Spinal Stenosis and Disc Herniation. Asian Spine J. 2017, 11, 71–74. [Google Scholar] [CrossRef]
- Liu, H.; Tao, H.; Luo, Z. Validation of the Simplified Chinese Version of the Oswestry Disability Index. Spine 2009, 34, 1211–1216. [Google Scholar] [CrossRef]
- Yin, J.; Jiang, Y.; Nong, L. Transforaminal approach versus interlaminar approach: A meta-analysis of operative complication of percutaneous endoscopic lumbar discectomy. Medicine 2020, 99, e20709. [Google Scholar] [CrossRef]
- Park, H.-J.; Kim, S.-K.; Lee, S.-C.; Kim, W.; Han, S.; Kang, S.-S. Dural Tears in Percutaneous Biportal Endoscopic Spine Surgery: Anatomical Location and Management. World Neurosurg. 2020, 136, e578–e585. [Google Scholar] [CrossRef]



| Study (Year) | Country Study Type | Patient | Surgery Procedures | Sample Size | Age (Mean ± SD) | Gender (M/F) | Follow-Up (m) | Outcomes |
|---|---|---|---|---|---|---|---|---|
| Choi et al., 2018 [15] | Korea prospective | LDH | Biportal | 20 | 47.43 ± 12.21 | 10/10 | 1 | ①③⑤⑥ |
| Uniportal | 40 | 44.45 ± 7.87 | 20/20 | 1 | ||||
| Heo et al., 2019 [16] | Korea Retrospective | LSS | Biportal | 37 | 66.7 ± 9.4 | 15/22 | 12.5 ± 3.3 | ①④⑤⑥ |
| Uniportal | 27 | 67.3 ± 9.9 | 11/16 | 12.5 ± 3.3 | ||||
| Zhu et al., 2021 [14] | China Retrospective | LDH | Biportal | 15 | 54 (Median) | 7/8 | 6–18 | ①③⑤⑥ |
| Uniportal | 18 | 56 (Median) | 11/7 | 6–19 | ||||
| Kang et al., 2021 [11] | China Retrospective | LSS | Biportal | 50 | 64.97 ± 9.83 | 22/28 | 3 | ①②③④⑤⑥ |
| Uniportal | 50 | 65.18 ± 11.12 | 26/24 | 3 | ||||
| Wang et al., 2021 [12] | China Retrospective | LSS | Biportal | 23 | 61.52 ± 4.09 | 13/10 | 9.26 ± 0.75 | ①②③④⑤⑥ |
| Uniportal | 25 | 59.24 ± 4.11 | 13/12 | 8.96 ± 0.89 | ||||
| Hao et al., 2021 [17] | China Retrospective | LDH | Biportal | 20 | 58.2 ± 10.2 | 14/6 | 6 (at least) | ①②③④⑤⑥ |
| Uniportal | 20 | 59.3 ± 7.8 | 8/12 | 6 (at least) | ||||
| Hu et al., 2021 [13] | China RCT | LDH | Biportal | 20 | 59.3 | 25 | 3 | ①⑤⑥ |
| Uniportal | 18 | 13 | 3 |
| Study | Selection | Comparability | Outcome/Exposure | Quality Judgment |
|---|---|---|---|---|
| Choi et al., 2018 [15] | 3 | 2 | 1 | 6 |
| Heo et al., 2019 [16] | 3 | 2 | 2 | 7 |
| Zhu et al., 2021 [14] | 3 | 2 | 2 | 7 |
| Kang et al., 2021 [11] | 3 | 2 | 1 | 6 |
| Wang et al., 2021 [12] | 3 | 2 | 3 | 8 |
| Hao et al., 2021 [17] | 4 | 2 | 2 | 8 |
| Study (Year) | Surgery Procedures | Sample Size | No. of Complications | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Dural Tear | Nerve Root Injury | Transient Weakness | Postop Hematoma | Postop Instability | Infection | Transient Paresthesia | Cerebrospinal Fluid Leakage/Headache | Total Complications | |||
| Choi et al., 2018 [15] | UBE | 20 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| PIED + PTED | 40 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Heo et al., 2019 [16] | UBE | 37 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 2 |
| PIED | 27 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 3 | |
| Zhu et al., 2021 [14] | UBE | 15 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| PIED | 18 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Kang et al., 2021 [11] | UBE | 50 | 2 | 3 | 0 | 0 | 0 | 2 | 0 | 0 | 5 |
| PIED | 50 | 3 | 2 | 0 | 0 | 0 | 4 | 0 | 0 | 6 | |
| Wang et al., 2021 [12] | UBE | 23 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 2 |
| PIED | 25 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 2 | |
| Hao et al., 2021 [17] | UBE | 20 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 2 |
| PTED | 20 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | |
| Hu et al., 2021 [13] | UBE | 20 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| PIED | 18 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu, W.-B.; Kotheeranurak, V.; Zhang, H.-L.; Chen, Z.-X.; Wu, H.-J.; Chen, C.-M.; Lin, G.-X.; Rui, G. Is Biportal Endoscopic Spine Surgery More Advantageous Than Uniportal for the Treatment of Lumbar Degenerative Disease? A Meta-Analysis. Medicina 2022, 58, 1523. https://doi.org/10.3390/medicina58111523
Xu W-B, Kotheeranurak V, Zhang H-L, Chen Z-X, Wu H-J, Chen C-M, Lin G-X, Rui G. Is Biportal Endoscopic Spine Surgery More Advantageous Than Uniportal for the Treatment of Lumbar Degenerative Disease? A Meta-Analysis. Medicina. 2022; 58(11):1523. https://doi.org/10.3390/medicina58111523
Chicago/Turabian StyleXu, Wen-Bin, Vit Kotheeranurak, Huang-Lin Zhang, Zhang-Xin Chen, Hua-Jian Wu, Chien-Min Chen, Guang-Xun Lin, and Gang Rui. 2022. "Is Biportal Endoscopic Spine Surgery More Advantageous Than Uniportal for the Treatment of Lumbar Degenerative Disease? A Meta-Analysis" Medicina 58, no. 11: 1523. https://doi.org/10.3390/medicina58111523
APA StyleXu, W.-B., Kotheeranurak, V., Zhang, H.-L., Chen, Z.-X., Wu, H.-J., Chen, C.-M., Lin, G.-X., & Rui, G. (2022). Is Biportal Endoscopic Spine Surgery More Advantageous Than Uniportal for the Treatment of Lumbar Degenerative Disease? A Meta-Analysis. Medicina, 58(11), 1523. https://doi.org/10.3390/medicina58111523








