Inflammatory Biomarkers as Prognostic Factors of Acute Deep Vein Thrombosis Following the Total Knee Arthroplasty
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Collection
2.3. Systemic Inflammatory Markers
- -
- MLR = total number of monocytes/total number of lymphocytes
- -
- NLR = total number of neutrophils/total number of lymphocytes
- -
- PLR = total number of platelets/total number of lymphocytes
- -
- SII = (total number of neutrophils × total number of platelets)/total number of lymphocytes
- -
- SIRI = (total number of monocytes × total number of platelets)/total number of lymphocytes
- -
- AISI = (total number of neutrophils × total number of monocytes × total number of platelets)/total number of lymphocytes
2.4. Knee Osteoarthritis Severity
2.5. Surgical Technique
2.6. Study Outcomes
2.7. Follow-up Strategy
2.8. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Maradit Kremers, H.; Larson, D.R.; Crowson, C.S.; Kremers, W.K.; Washington, R.E.; Steiner, C.A.; Jiranek, W.A.; Berry, D.J. Prevalence of Total Hip and Knee Replacement in the United States. J. Bone Jt. Surg. Am. 2015, 97, 1386–1397. [Google Scholar] [CrossRef] [PubMed]
- Brander, V.; Gondek, S.; Martin, E.; Stulberg, S.D. Pain and Depression Influence Outcome 5 Years after Knee Replacement Surgery. Clin. Orthop. 2007, 464, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Cram, P.; Lu, X.; Kates, S.L.; Singh, J.A.; Li, Y.; Wolf, B.R. Total Knee Arthroplasty Volume, Utilization, and Outcomes among Medicare Beneficiaries, 1991–2010. JAMA 2012, 308, 1227–1236. [Google Scholar] [CrossRef] [PubMed]
- Caracciolo, B.; Giaquinto, S. Self-Perceived Distress and Self-Perceived Functional Recovery after Recent Total Hip and Knee Arthroplasty. Arch. Gerontol. Geriatr. 2005, 41, 177–181. [Google Scholar] [CrossRef]
- Brander, V.A.; Stulberg, S.D.; Adams, A.D.; Harden, R.N.; Bruehl, S.; Stanos, S.P.; Houle, T. Predicting Total Knee Replacement Pain: A Prospective, Observational Study. Clin. Orthop. 2003, 416, 27–36. [Google Scholar] [CrossRef]
- Bourne, R.B.; Chesworth, B.M.; Davis, A.M.; Mahomed, N.N.; Charron, K.D.J. Patient Satisfaction after Total Knee Arthroplasty: Who Is Satisfied and Who Is Not? Clin. Orthop. 2010, 468, 57–63. [Google Scholar] [CrossRef]
- Shahi, A.; Chen, A.F.; Tan, T.L.; Maltenfort, M.G.; Kucukdurmaz, F.; Parvizi, J. The Incidence and Economic Burden of In-Hospital Venous Thromboembolism in the United States. J. Arthroplast. 2017, 32, 1063–1066. [Google Scholar] [CrossRef]
- Dai, W.-L.; Lin, Z.-M.; Shi, Z.-J.; Wang, J. Venous Thromboembolic Events after Total Knee Arthroplasty: Which Patients Are at a High Risk? J. Knee Surg. 2020, 33, 947–957. [Google Scholar] [CrossRef] [PubMed]
- Warren, J.A.; Sundaram, K.; Kamath, A.F.; Molloy, R.M.; Krebs, V.E.; Mont, M.A.; Piuzzi, N.S. Venous Thromboembolism Rates Did Not Decrease in Lower Extremity Revision Total Joint Arthroplasty From 2008 to 2016. J. Arthroplast. 2019, 34, 2774–2779. [Google Scholar] [CrossRef]
- Warren, J.A.; Sundaram, K.; Anis, H.K.; Kamath, A.F.; Higuera, C.A.; Piuzzi, N.S. Have Venous Thromboembolism Rates Decreased in Total Hip and Knee Arthroplasty? J. Arthroplast. 2020, 35, 259–264. [Google Scholar] [CrossRef]
- Gionis, M.N.; Ioannou, C.V.; Katsamouris, A.N.; Katonis, P.; Balalis, K.; Sfyridaki, K.; Elalamy, I.; Gerotziafas, G.T. The Study of the Thrombin Generation Mechanism and the Effect of Low Molecular Weight Heparin as Thromboprophylaxis in Patients Undergoing Total Knee and Hip Replacement. Thromb. Res. 2013, 132, 685–691. [Google Scholar] [CrossRef] [PubMed]
- Virchow, R. Gesammelte Abhandlungen zur Wissenschaftlichen Medicin; Meidinger Sohn & Company: Frankfurt-am-Main, German, 1856. [Google Scholar]
- Reganon, E.; Vila, V.; Martínez-Sales, V.; Vayá, A.; Mira, Y.; Ferrando, F.; Aznar, J. Sialic Acid Is an Inflammation Marker Associated with a History of Deep Vein Thrombosis. Thromb. Res. 2007, 119, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Matos, M.F.; Lourenço, D.M.; Orikaza, C.M.; Bajerl, J.A.H.; Noguti, M.A.E.; Morelli, V.M. The Role of IL-6, IL-8 and MCP-1 and Their Promoter Polymorphisms IL-6 -174GC, IL-8 -251AT and MCP-1 -2518AG in the Risk of Venous Thromboembolism: A Case-Control Study. Thromb. Res. 2011, 128, 216–220. [Google Scholar] [CrossRef]
- Hou, H.; Ge, Z.; Ying, P.; Dai, J.; Shi, D.; Xu, Z.; Chen, D.; Jiang, Q. Biomarkers of Deep Venous Thrombosis. J. Thromb. Thrombolysis 2012, 34, 335–346. [Google Scholar] [CrossRef]
- Shi, D.; Xu, X.; Xu, Z.; Nakamura, T.; Pang, Y.; Yao, C.; Wang, F.; Chen, D.; Dai, J.; Jiang, Q. P-Selectin: An Unpredicted Factor for Deep Vein Thrombosis after Total Hip Arthroplasty. BioMed Res. Int. 2014, 2014, 783967. [Google Scholar] [CrossRef]
- Xu, Z.; Shi, D.; Zhang, C.; Chen, D.; Dai, J.; Teng, H.; Jiang, Q. Postoperative Plasma D-Dimer Value for Predicting Deep Venous Thrombosis Following Hip Arthroplasty with Nadroparin Prophylaxis. Hip Int. J. Clin. Exp. Res. Hip Pathol. Ther. 2013, 23, 411–416. [Google Scholar] [CrossRef]
- Huang, Z.; Xie, X.; Li, L.; Huang, Q.; Ma, J.; Shen, B.; Kraus, V.B.; Pei, F. Intravenous and Topical Tranexamic Acid Alone Are Superior to Tourniquet Use for Primary Total Knee Arthroplasty: A Prospective, Randomized Controlled Trial. J. Bone Jt. Surg. Am. 2017, 99, 2053–2061. [Google Scholar] [CrossRef]
- Bottner, F.; Wegner, A.; Winkelmann, W.; Becker, K.; Erren, M.; Götze, C. Interleukin-6, Procalcitonin and TNF-Alpha: Markers of Peri-Prosthetic Infection Following Total Joint Replacement. J. Bone Jt. Surg. Br. 2007, 89, 94–99. [Google Scholar] [CrossRef] [PubMed]
- Niskanen, R.O.; Korkala, O.; Pammo, H. Serum C-Reactive Protein Levels after Total Hip and Knee Arthroplasty. J. Bone Jt. Surg. Br. 1996, 78, 431–433. [Google Scholar] [CrossRef]
- Park, K.K.; Kim, T.K.; Chang, C.B.; Yoon, S.W.; Park, K.U. Normative Temporal Values of CRP and ESR in Unilateral and Staged Bilateral TKA. Clin. Orthop. 2008, 466, 179–188. [Google Scholar] [CrossRef]
- Ettinger, M.; Savov, P.; Calliess, T.; Windhagen, H.; Lichtinghagen, R.; Lukasz, A.; Omar, M. Improved Diagnostic Accuracy with the Classification Tree Method for Diagnosing Low-Grade Periprosthetic Joint Infections by Quantitative Measurement of Synovial Fluid Alpha-Defensin and C-Reactive Protein. Int. Orthop. 2020, 44, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Bauer, T.W.; Parvizi, J.; Kobayashi, N.; Krebs, V. Diagnosis of Periprosthetic Infection. J. Bone Jt. Surg. Am. 2006, 88, 869–882. [Google Scholar] [CrossRef]
- Arbănași, E.M.; Mureșan, A.V.; Coșarcă, C.M.; Kaller, R.; Bud, T.I.; Hosu, I.; Voidăzan, S.T.; Arbănași, E.M.; Russu, E. Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio Impact on Predicting Outcomes in Patients with Acute Limb Ischemia. Life 2022, 12, 822. [Google Scholar] [CrossRef] [PubMed]
- Russu, E.; Mureșan, A.V.; Arbănași, E.M.; Kaller, R.; Hosu, I.; Voidăzan, S.; Arbănași, E.M.; Coșarcă, C.M. The Predictive Role of NLR and PLR in Outcome and Patency of Lower Limb Revascularization in Patients with Femoropopliteal Disease. J. Clin. Med. 2022, 11, 2620. [Google Scholar] [CrossRef] [PubMed]
- Taurino, M.; Aloisi, F.; Del Porto, F.; Nespola, M.; Dezi, T.; Pranteda, C.; Rizzo, L.; Sirignano, P. Neutrophil-to-Lymphocyte Ratio Could Predict Outcome in Patients Presenting with Acute Limb Ischemia. J. Clin. Med. 2021, 10, 4343. [Google Scholar] [CrossRef] [PubMed]
- Drugescu, A.; Roca, M.; Zota, I.M.; Costache, A.-D.; Gavril, O.I.; Gavril, R.S.; Vasilcu, T.F.; Mitu, O.; Esanu, I.M.; Roca, I.-C.; et al. Value of the Neutrophil to Lymphocyte Ratio and Platelet to Lymphocyte Ratio in Predicting CPET Performance in Patients with Stable CAD and Recent Elective PCI. Med. Kaunas Lith. 2022, 58, 814. [Google Scholar] [CrossRef]
- Efros, O.; Beit Halevi, T.; Meisel, E.; Soffer, S.; Barda, N.; Cohen, O.; Kenet, G.; Lubetsky, A. The Prognostic Role of Neutrophil-to-Lymphocyte Ratio in Patients Hospitalized with Acute Pulmonary Embolism. J. Clin. Med. 2021, 10, 4058. [Google Scholar] [CrossRef]
- Strazzulla, A.; Abroug Ben Halima, S.; Chouchane, I.; Rezek, M.; Pinto Stiebler, M.; Hamrouni, S.; Maalaoui, M.; Ghriss, N.; Guedec-Ghelfi, R.; Moini, C.; et al. The Predictive Value of Cell Blood Count Parameters to Diagnose Pulmonary Embolism in Patients with SARS-CoV-2 Infection: A Case Control Study. Antibiotics 2022, 11, 60. [Google Scholar] [CrossRef]
- Pasqui, E.; de Donato, G.; Lazzeri, E.; Molino, C.; Galzerano, G.; Giubbolini, M.; Palasciano, G. High Neutrophil-to-Lymphocyte and Platelet-to-Lymphocyte Ratios Are Associated with a Higher Risk of Hemodialysis Vascular Access Failure. Biomedicines 2022, 10, 2218. [Google Scholar] [CrossRef]
- Kaller, R.; Arbănași, E.M.; Mureșan, A.V.; Voidăzan, S.; Arbănași, E.M.; Horváth, E.; Suciu, B.A.; Hosu, I.; Halmaciu, I.; Brinzaniuc, K.; et al. The Predictive Value of Systemic Inflammatory Markers, the Prognostic Nutritional Index, and Measured Vessels’ Diameters in Arteriovenous Fistula Maturation Failure. Life 2022, 12, 1447. [Google Scholar] [CrossRef]
- Mureșan, A.V.; Russu, E.; Arbănași, E.M.; Kaller, R.; Hosu, I.; Arbănași, E.M.; Voidăzan, S.T. The Predictive Value of NLR, MLR, and PLR in the Outcome of End-Stage Kidney Disease Patients. Biomedicines 2022, 10, 1272. [Google Scholar] [CrossRef] [PubMed]
- Halmaciu, I.; Arbănași, E.M.; Kaller, R.; Mureșan, A.V.; Arbănași, E.M.; Bacalbasa, N.; Suciu, B.A.; Cojocaru, I.I.; Runcan, A.I.; Grosu, F.; et al. Chest CT Severity Score and Systemic Inflammatory Biomarkers as Predictors of the Need for Invasive Mechanical Ventilation and of COVID-19 Patients’ Mortality. Diagnostics 2022, 12, 2089. [Google Scholar] [CrossRef]
- Parthasarathi, A.; Padukudru, S.; Arunachal, S.; Basavaraj, C.K.; Krishna, M.T.; Ganguly, K.; Upadhyay, S.; Anand, M.P. The Role of Neutrophil-to-Lymphocyte Ratio in Risk Stratification and Prognostication of COVID-19: A Systematic Review and Meta-Analysis. Vaccines 2022, 10, 1233. [Google Scholar] [CrossRef] [PubMed]
- Citu, C.; Gorun, O.M.; Motoc, A.; Citu, I.M.; Gorun, F.; Malita, D. Correlation of Lung Damage on CT Scan with Laboratory Inflammatory Markers in COVID-19 Patients: A Single-Center Study from Romania. J. Clin. Med. 2022, 11, 4299. [Google Scholar] [CrossRef] [PubMed]
- Cocoş, R.; Mahler, B.; Turcu-Stiolica, A.; Stoichiță, A.; Ghinet, A.; Shelby, E.-S.; Bohîlțea, L.C. Risk of Death in Comorbidity Subgroups of Hospitalized COVID-19 Patients Inferred by Routine Laboratory Markers of Systemic Inflammation on Admission: A Retrospective Study. Viruses 2022, 14, 1201. [Google Scholar] [CrossRef] [PubMed]
- Regolo, M.; Vaccaro, M.; Sorce, A.; Stancanelli, B.; Colaci, M.; Natoli, G.; Russo, M.; Alessandria, I.; Motta, M.; Santangelo, N.; et al. Neutrophil-to-Lymphocyte Ratio (NLR) Is a Promising Predictor of Mortality and Admission to Intensive Care Unit of COVID-19 Patients. J. Clin. Med. 2022, 11, 2235. [Google Scholar] [CrossRef]
- Kudlinski, B.; Zgoła, D.; Stolińska, M.; Murkos, M.; Kania, J.; Nowak, P.; Noga, A.; Wojciech, M.; Zaborniak, G.; Zembron-Lacny, A. Systemic Inflammatory Predictors of In-Hospital Mortality in COVID-19 Patients: A Retrospective Study. Diagnostics 2022, 12, 859. [Google Scholar] [CrossRef]
- Festa, E.; Ascione, T.; Bernasconi, A.; Di Gennaro, D.; Basso, M.A.; Guarino, A.; Balato, G. Diagnostic Performance of Neutrophil to Lymphocyte Ratio, Monocyte to Lymphocyte Ratio, Platelet to Lymphocyte Ratio, and Platelet to Mean Platelet Volume Ratio in Periprosthetic Hip and Knee Infections: A Systematic Review and Meta-Analysis. Diagnostics 2022, 12, 2033. [Google Scholar] [CrossRef]
- Xu, H.; Xie, J.; Zhang, S.; Wang, D.; Huang, Z.; Zhou, Z. Potential Blood Biomarkers for Diagnosing Periprosthetic Joint Infection: A Single-Center, Retrospective Study. Antibiotics 2022, 11, 505. [Google Scholar] [CrossRef]
- Sigmund, I.K.; Puchner, S.E.; Windhager, R. Serum Inflammatory Biomarkers in the Diagnosis of Periprosthetic Joint Infections. Biomedicines 2021, 9, 1128. [Google Scholar] [CrossRef]
- Kellgren, J.H.; Lawrence, J.S. Radiological Assessment of Osteo-Arthrosis. Ann. Rheum. Dis. 1957, 16, 494–502. [Google Scholar] [CrossRef] [PubMed]
- Zixuan, L.; Chen, W.; Li, Y.; Wang, X.; Zhang, W.; Zhu, Y.; Zhang, F. Incidence of Deep Venous Thrombosis (DVT) of the Lower Extremity in Patients Undergoing Surgeries for Ankle Fractures. J. Orthop. Surg. 2020, 15, 294. [Google Scholar] [CrossRef] [PubMed]
- Tay, K.; Bin Abd Razak, H.R.; Tan, A.H.C. Obesity and Venous Thromboembolism in Total Knee Arthroplasty Patients in an Asian Population. J. Arthroplast. 2016, 31, 2880–2883. [Google Scholar] [CrossRef] [PubMed]
- Xiong, X.; Cheng, B. Preoperative Risk Factors for Deep Vein Thrombosis in Knee Osteoarthritis Patients Undergoing Total Knee Arthroplasty. J. Orthop. Sci. 2021, in press. [Google Scholar] [CrossRef] [PubMed]
- Santana, D.C.; Emara, A.K.; Orr, M.N.; Klika, A.K.; Higuera, C.A.; Krebs, V.E.; Molloy, R.M.; Piuzzi, N.S. An Update on Venous Thromboembolism Rates and Prophylaxis in Hip and Knee Arthroplasty in 2020. Medicina 2020, 56, 416. [Google Scholar] [CrossRef]
- Risk of and Prophylaxis for Venous Thromboembolism in Hospital Patients. Thromboembolic Risk Factors (THRIFT) Consensus Group. BMJ 1992, 305, 567–574. [Google Scholar] [CrossRef]
- Frank, B.; Maher, Z.; Hazelton, J.P.; Resnick, S.; Dauer, E.; Goldenberg, A.; Lubitz, A.L.; Smith, B.P.; Saillant, N.N.; Reilly, P.M.; et al. Venous Thromboembolism after Major Venous Injuries: Competing Priorities. J. Trauma Acute Care Surg. 2017, 83, 1095–1101. [Google Scholar] [CrossRef]
- Dahl, O.E.; Harenberg, J.; Wexels, F.; Preissner, K.T. Arterial and Venous Thrombosis Following Trauma and Major Orthopedic Surgery: Molecular Mechanisms and Strategies for Intervention. Semin. Thromb. Hemost. 2015, 41, 141–145. [Google Scholar] [CrossRef]
- Albayati, M.A.; Grover, S.P.; Saha, P.; Lwaleed, B.A.; Modarai, B.; Smith, A. Postsurgical Inflammation as a Causative Mechanism of Venous Thromboembolism. Semin. Thromb. Hemost. 2015, 41, 615–620. [Google Scholar] [CrossRef]
- Wanderling, C.; Liles, J.; Finkler, E.; Carlsgaard, P.; Hopkinson, W.; Guler, N.; Hoppensteadt, D.; Fareed, J. Dysregulation of Tissue Factor, Thrombin-Activatable Fibrinolysis Inhibitor, and Fibrinogen in Patients Undergoing Total Joint Arthroplasty. Clin. Appl. Thromb. Hemost. 2017, 23, 967–972. [Google Scholar] [CrossRef]
- Myers, S.P.; Kutcher, M.E.; Rosengart, M.R.; Sperry, J.L.; Peitzman, A.B.; Brown, J.B.; Neal, M.D. Tranexamic Acid Administration Is Associated with an Increased Risk of Posttraumatic Venous Thromboembolism. J. Trauma Acute Care Surg. 2019, 86, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Henry, D.A.; Carless, P.A.; Moxey, A.J.; O’Connell, D.; Stokes, B.J.; Fergusson, D.A.; Ker, K. Anti-fibrinolytic Use for Minimising Perioperative Allogeneic Blood Transfusion. Cochrane Database Syst. Rev. 2011, 1, CD001886. [Google Scholar] [CrossRef]
- Ng, W.; Jerath, A.; Wąsowicz, M. Tranexamic Acid: A Clinical Review. Anaesthesiol. Intensive Ther. 2015, 47, 339–350. [Google Scholar] [CrossRef] [PubMed]
- Zhao, G.; Chen, J.; Wang, J.; Wang, S.; Xia, J.; Wei, Y.; Wu, J.; Huang, G.; Chen, F.; Shi, J.; et al. Predictive Values of the Postoperative Neutrophil-to-Lymphocyte Ratio, Platelet-to-Lymphocyte Ratio, and Lymphocyte-to-Monocyte Ratio for the Diagnosis of Early Periprosthetic Joint Infections: A Preliminary Study. J. Orthop. Surg. 2020, 15, 571. [Google Scholar] [CrossRef] [PubMed]
- Jiao, J.; Huang, J.; Chen, X.; Jin, Y. Albumin to Globulin Ratio, Neutrophil to Lymphocyte Ratio, and Globulin Levels Do Not Outperform ESR or CRP When Diagnosing Periprosthetic Joint Infection. BMC Musculoskelet. Disord. 2022, 23, 404. [Google Scholar] [CrossRef]
- Klemt, C.; Tirumala, V.; Smith, E.J.; Xiong, L.; Kwon, Y.-M. Complete Blood Platelet and Lymphocyte Ratios Increase Diagnostic Accuracy of Periprosthetic Joint Infection Following Total Hip Arthroplasty. Arch. Orthop. Trauma Surg. 2022. [Google Scholar] [CrossRef]
- Yao, C.; Zhang, Z.; Yao, Y.; Xu, X.; Jiang, Q.; Shi, D. Predictive Value of Neutrophil to Lymphocyte Ratio and Platelet to Lymphocyte Ratio for Acute Deep Vein Thrombosis after Total Joint Arthroplasty: A Retrospective Study. J. Orthop. Surg. 2018, 13, 40. [Google Scholar] [CrossRef]
- Seo, W.-W.; Park, M.-S.; Kim, S.E.; Lee, J.-H.; Park, D.-G.; Han, K.-R.; Oh, D.-J.; Hyon, M.-S. Neutrophil–Lymphocyte Ratio as a Predictor of Venous Thromboembolism after Total Knee Replacement. J. Knee Surg. 2021, 34, 171–177. [Google Scholar] [CrossRef]

| Variables | All Patients n = 273 | No-DVT n = 245 | DVT n = 28 | p Value (OR; CI 95%) |
|---|---|---|---|---|
| Age mean ± SD (min–max) | 66.36 ± 6.91 (51–82) | 65.26 ± 6.81 (51–82) | 68.71 ± 6.55 (51–77) | 0.006 |
| Male/Female sex no. (%) | 122 (44.69%) 151 (55.31%) | 110 (44.90%) 135 (55.10%) | 12 (42.86%) 16 (57.14%) | 0.83 (0.92; 0.41–2.02) |
| Comorbidities and Risk Factors | ||||
| AH, no. (%) | 158 (57.87%) | 136 (55.51%) | 22 (78.57%) | 0.02 (2.93; 1.15–7.50) |
| IHD, no. (%) | 134 (49.08%) | 119 (48.57%) | 15 (53.57%) | 0.61 (1.22; 0.55–2.67) |
| AF, no. (%) | 65 (23.80%) | 53 (21.63%) | 12 (42.85%) | 0.01 (2.71; 1.21–6.09) |
| CHF, no. (%) | 101 (36.99%) | 90 (36.73%) | 11 (39.28%) | 0.79 (1.11; 0.49–2.48) |
| MI, no. (%) | 55 (20.14%) | 46 (18.77%) | 9 (32.14%) | 0.10 (2.04; 0.87–4.82) |
| T2D, no. (%) | 99 (36.23%) | 87 (35.51%) | 12 (42.85%) | 0.44 (1.36; 0.61–3.009) |
| CKD, no. (%) | 21 (7.69%) | 19 (7.75%) | 2 (7.14%) | 0.90 (0.91; 0.20–4.15) |
| Malignancy, no. (%) | 20 (7.32%) | 14 (5.71%) | 6 (21.42%) | 0.005 (4.50; 1.57–12.88) |
| CVI, no. (%) | 82 (30.03%) | 72 (29.38%) | 10 (35.71%) | 0.49 (1.33; 0.58–3.03) |
| Tobacco, no. (%) | 80 (29.30%) | 67 (27.34%) | 13 (46.42%) | 0.03 (2.30; 1.04–5.09) |
| Obesity, no. (%) | 61 (22.34%) | 50 (20.40%) | 11 (39.28%) | 0.02 (2.52; 1.11–5.72) |
| Dyslipidemia, no. (%) | 66 (24.17%) | 55 (22.44%) | 11 (39.28%) | 0.053 (2.23; 0.98–5.05) |
| Laboratory Data | ||||
| Hemoglobin g/dL median (Q1–Q3) | 14.4 (12.8–15.3) | 14.47 (12.9–15.31) | 13.2 (12.27–15.15) | 0.02 |
| Hematocrit % median (Q1–Q3) | 41.2 (38.2–43.45) | 41.23 (38.5–43.45) | 39.1 (36.07–42.58) | 0.03 |
| Neutrophils ×103/μL median (Q1–Q3) | 5.86 (4.47–7.6) | 5.68 (4.39–7.5) | 7.42 (6.37–9.61) | 0.0001 |
| Lymphocytes ×103/μL median (Q1–Q3) | 1.82 (1.46–2.4) | 1.9 (1.53–2.44) | 1.27 (1.02–1.79) | <0.0001 |
| Monocyte ×103/μL median (Q1–Q3) | 0.63 (0.46–0.89) | 0.62 (0.46–0.86) | 0.83 (0.59–1.22) | 0.001 |
| PLT ×103/μL median (Q1–Q3) | 239 (202–301.45) | 235.4 (200.2–297.8) | 285.9 (240.25–342.75) | 0.0007 |
| Glucose mg/dL median (Q1–Q3) | 118 (96–142) | 117 (96–143) | 120.5 (95.25–139.25) | 0.43 |
| Cholesterol mg/dL median (Q1–Q3) | 129.1 (104.7–163.7) | 130.8 (105.6–164) | 121.3 (94.12–144.47) | 0.11 |
| Triglyceride mg/dL median (Q1–Q3) | 123.7 (90.8–176) | 123 (90.8–176) | 136.8 (101.87–173.4) | 0.36 |
| BUN mg/dL median (Q1–Q3) | 40 (31.9–49.2) | 39.4 (31.8–48.6) | 46 (37.77–55.22) | 0.02 |
| Creatinine mg/dL median (Q1–Q3) | 0.89 (0.75–1.04) | 0.88 (0.73–1.02) | 1.02 (0.90–1.24) | <0.0001 |
| GFR (mL/min/1.73 M2) median (Q1–Q3) | 86.15 (75.11–89.2) | 86.15 (75.11–88) | 86.15 (75.83–98.5) | 0.22 |
| Serum albumin mg/dL median (Q1–Q3) | 3.44 (2.9–3.96) | 3.55 (2.93–4) | 3 (2.69–3.62) | 0.002 |
| Serum calcium mg/dL median (Q1–Q3) | 8.55 (8.13–9.19) | 8.58 (8.09–9.23) | 8.43 (8.36–8.71) | 0.37 |
| Potassium mmol/L median (Q1–Q3) | 4.58 (4.1–5.31) | 4.56 (4.08–5.24) | 4.95 (4.44–5.74) | 0.03 |
| Sodium mmol/L median (Q1–Q3) | 140 (139–141) | 140 (139–141) | 140 (139–141) | 0.47 |
| MLR, median (Q1–Q3) | 0.34 (0.24–0.52) | 0.32 (0.23–0.46) | 0.60 (0.48–0.77) | <0.0001 |
| NLR, median (Q1–Q3) | 3.12 (2.34–4.18) | 2.97 (2.25–3.92) | 5.71 (4.16–6.75) | <0.0001 |
| PLR, median (Q1–Q3) | 129.81 (102.62–169.10) | 123.8 (100.33–160.60) | 209.55 (166.46–289.81) | <0.0001 |
| SII, median (Q1–Q3) | 717.95 (531.61–1144.33) | 686.82 (514.28–1058.05) | 1534.73 (1168.03–2251.45) | <0.0001 |
| SIRI, median (Q1–Q3) | 1.96 (1.28–3.40) | 1.86 (1.19–2.85) | 4.63 (3.10–6.99) | <0.0001 |
| AISI, median (Q1–Q3) | 493.85 (272.82–849.03) | 449.32 (250.29–772.92) | 1360.18 (701.71–2305.76) | <0.0001 |
| Outcomes | ||||
| DVT, no. (%) | 28 (10.25%) | - | 28 (10.25%) | <0.0001 |
| Length of hospital stay, median (Q1–Q3) | 8 (7–10) | 8 (7–10) | 8.5 (7.75–10.25) | 0.15 |
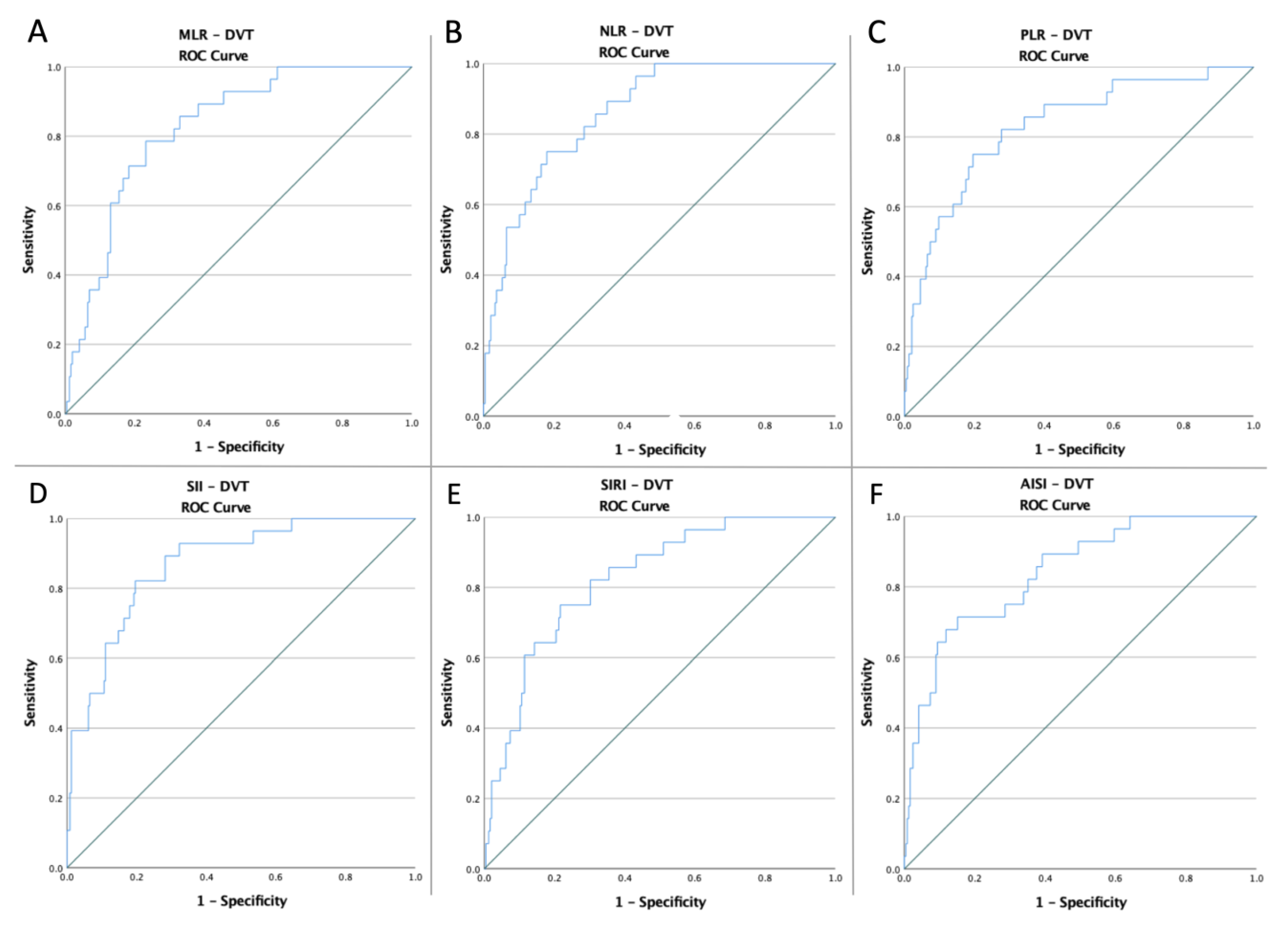
| Variables | Cut-Off | AUC | Std. Error | 95% CI | Sensitivity | Specificity | p Value |
|---|---|---|---|---|---|---|---|
| DVT | |||||||
| MLR | 0.47 | 0.825 | 0.035 | 0.757–0.894 | 78.6% | 76.7% | <0.0001 |
| NLR | 3.88 | 0.862 | 0.030 | 0.802–0.922 | 78.6% | 73.5% | <0.0001 |
| PLR | 168.88 | 0.829 | 0.042 | 0.747–0.911 | 75% | 80.4% | <0.0001 |
| SII | 1133.83 | 0.870 | 0.032 | 0.806–0.933 | 82.1% | 80.4% | <0.0001 |
| SIRI | 3.25 | 0.824 | 0.037 | 0.751–0.897 | 75% | 78.4% | <0.0001 |
| AISI | 925.49 | 0.842 | 0.038 | 0.767–0.916 | 71.4% | 84.9% | <0.0001 |
| Variables | Length of Hospital Stay | DVT |
|---|---|---|
| Low-MLR vs. high-MLR | 8.38 ± 1.95 vs. 8.61 ± 2.28 p = 0.33 | 6/190 (3.15%) vs. 22/83 (26.50%) p < 0.0001 OR:11.06 CI: (4.28–28.54) |
| Low-NLR vs. high-NLR | 8.27 ± 2.006 vs. 8.83 ± 2.13 p = 0.01 | 6/186 (3.22%) vs. 22/87 (25.28%) p < 0.0001 OR:10.15 CI: (3.94–26.15) |
| Low-PLR vs. high-PLR | 8.39 ± 1.99 vs. 8.62 ± 2.24 p = 0.28 | 7/204 (3.43%) vs. 21/69 (30.43%) p < 0.0001 OR:12.31 CI: (4.94–30.64) |
| Low-SII vs. high-SII | 8.35 ± 1.97 vs. 8.73 ± 2.28 p = 0.13 | 5/202 (2.47%) vs. 23/71 (32.39%) p < 0.0001 OR:14.6 CI: (3.02–70.60) |
| Low-SIRI vs. high-SIRI | 8.26 ± 1.95 vs. 8.95 ± 2.26 p = 0.02 | 7/199 (3.51%) vs. 21/74 (28.37%) p < 0.0001 OR:13.14 CI: (5.32–32.43) |
| Low-AISI vs. high-AISI | 8.21 ± 1.94 vs. 9.36 ± 2.25 p = 0.0004 | 8/216 (3.70%) vs. 20/57 (35.08%) p < 0.0001 OR:14.05 CI: (5.76–34.27) |
| Variables | DVT | ||
|---|---|---|---|
| OR | 95% CI | p Value | |
| >70 years | 2.96 | 1.33–6.57 | 0.007 |
| AH | 2.93 | 1.15–7.50 | 0.02 |
| AF | 2.71 | 1.21–6.05 | 0.01 |
| Malignancy | 3.98 | 1.68–9.43 | 0.002 |
| Obesity | 2.34 | 1.03–5.30 | 0.04 |
| Tobacco | 2.30 | 1.04–5.09 | 0.04 |
| HIGH-MLR | 11.06 | 4.28–28.54 | <0.001 |
| high-NLR | 10.15 | 3.94–26.15 | <0.001 |
| HIGH-PLR | 12.31 | 4.94–30.64 | <0.001 |
| high-SII | 18.87 | 6.82–52.21 | <0.001 |
| high-SIRI | 10.86 | 4.38–26.94 | <0.001 |
| high-AISI | 14.05 | 5.76–34.27 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Melinte, R.M.; Arbănași, E.M.; Blesneac, A.; Zolog, D.N.; Kaller, R.; Mureșan, A.V.; Arbănași, E.M.; Melinte, I.M.; Niculescu, R.; Russu, E. Inflammatory Biomarkers as Prognostic Factors of Acute Deep Vein Thrombosis Following the Total Knee Arthroplasty. Medicina 2022, 58, 1502. https://doi.org/10.3390/medicina58101502
Melinte RM, Arbănași EM, Blesneac A, Zolog DN, Kaller R, Mureșan AV, Arbănași EM, Melinte IM, Niculescu R, Russu E. Inflammatory Biomarkers as Prognostic Factors of Acute Deep Vein Thrombosis Following the Total Knee Arthroplasty. Medicina. 2022; 58(10):1502. https://doi.org/10.3390/medicina58101502
Chicago/Turabian StyleMelinte, Răzvan Marian, Emil Marian Arbănași, Adrian Blesneac, Dan Nicolae Zolog, Réka Kaller, Adrian Vasile Mureșan, Eliza Mihaela Arbănași, Ioana Marta Melinte, Raluca Niculescu, and Eliza Russu. 2022. "Inflammatory Biomarkers as Prognostic Factors of Acute Deep Vein Thrombosis Following the Total Knee Arthroplasty" Medicina 58, no. 10: 1502. https://doi.org/10.3390/medicina58101502
APA StyleMelinte, R. M., Arbănași, E. M., Blesneac, A., Zolog, D. N., Kaller, R., Mureșan, A. V., Arbănași, E. M., Melinte, I. M., Niculescu, R., & Russu, E. (2022). Inflammatory Biomarkers as Prognostic Factors of Acute Deep Vein Thrombosis Following the Total Knee Arthroplasty. Medicina, 58(10), 1502. https://doi.org/10.3390/medicina58101502







