Is the Numbness after Knee Replacement a More Critical Complication Than Thought? A Detailed Analysis of Neuropathic Pain and Functional Outcomes
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- OECD. Health at a Glance 2021: OEC Indicators. Available online: https://www.oecd-ilibrary.org/social-issues-migration-health/health-at-a-glance-2021_ae3016b9-en (accessed on 14 May 2022).
- Knee Replacement Surgery by the Numbers. The Center. 2017. Available online: https://www.thecenteroregon.com/medical-blog/knee-replacement-surgery-by-the-numbers/ (accessed on 14 May 2022).
- Vitiello, R.; Bocchi, M.B.; Gessi, M.; Greco, T.; Cianni, L.; de Maio, F.; Pesce, V.; Maccauro, G.; Perisano, C. Induced membrane by silver-coated knee megaprosthesis: Keep oross? J. Biol. Homeost. Agents 2020, 34, 12. [Google Scholar]
- Black, R.; Green, C.; Sochart, D. Postoperativeumbness ofhe knee followingotal knee arthroplasty. Ann. R. Coll. Surg. Engl. 2013, 95, 565–568. [Google Scholar] [CrossRef] [PubMed]
- Blackburn, J.; Wylde, V.; Greenwood, R.; Blom, A.; Levy, A. Theffect ofumbness on outcome fromotal kneeeplacement. Ann. R. Coll. Surg. Engl. 2017, 99, 385–389. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Nöropatik, S.; Anketi, A. Available online: https://www.ftronline.com/4-soru-noropatik-agri-anketi/ (accessed on 8 May 2022).
- Alkan, H.; Ardic, F.; Erdogan, C.; Sahin, F.; Sarsan, A.; Findikoglu, G. Turkish Version ofhe painDETECT Questionnaire inhe Assessment of Neuropathic Pain: A Validity and Reliability Study. Pain Med. 2013, 14, 1933–1943. [Google Scholar] [CrossRef] [PubMed]
- SF-36 Nasıl Hesaplanır? Available online: https://www.ftronline.com/sf-36-nasil-hesaplanir/ (accessed on 15 May 2022).
- WOMAC. Available online: https://www.ftronline.com/womac/ (accessed on 8 May 2022).
- Free Online SF-36 Score Calculator—Ortho ToolKit. Available online: https://orthotoolkit.com/sf-36/ (accessed on 8 May 2022).
- Jamovi—Stats. Open. Now. Available online: https://www.jamovi.org/ (accessed on 15 May 2022).
- Anterior View of Knee Joint. Available online: https://togotv.dbcls.jp/en/togopic.2021.103.html (accessed on 15 May 2022). [CrossRef]
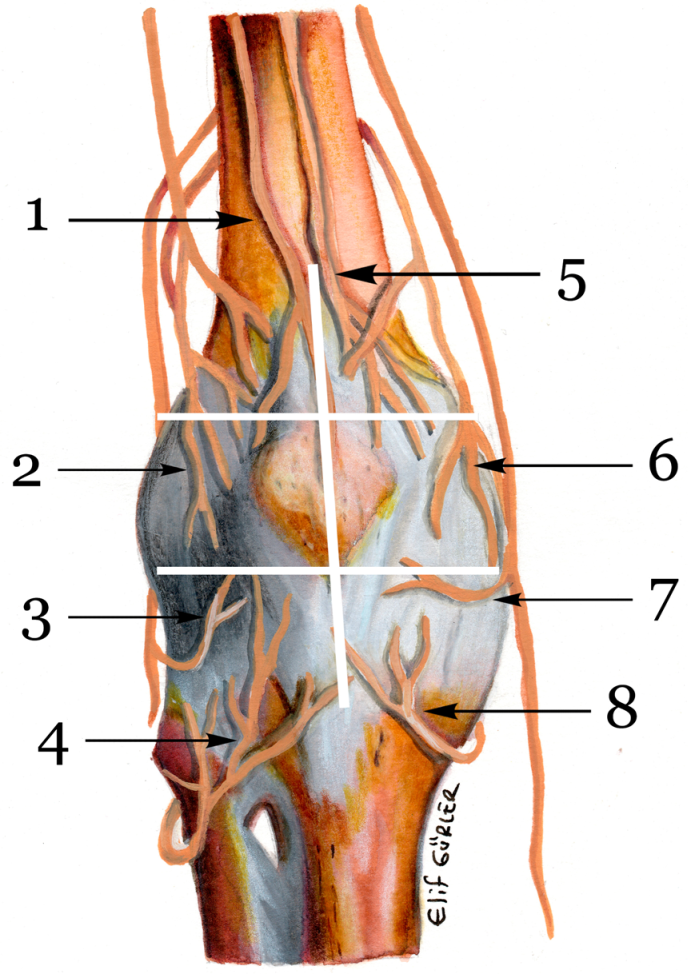
- Gardner, E. The innervation ofhe knee joint. Anat Rec. 1948, 101, 109–130. [Google Scholar] [CrossRef] [PubMed]
- Kerver, A.L.A.; Leliveld, M.S.; den Hartog, D.; Verhofstad, M.H.J.; Kleinrensink, G.J. The Surgical Anatomy ofhenfrapatellar Branch ofhe Saphenous Nerve in Relationoncisions for Anteromedial Knee Surgery. J. Bone Jt. Surg. 2013, 95, 2119–2125. [Google Scholar] [CrossRef] [PubMed]
- Leliveld, M.S.; Verhofstad, M.H.J. Injuryohe infrapatellar branch of hesaphenouserve, a possible cause for anterior knee pain afteribialailing? Injury 2012, 43, 779–783. [Google Scholar] [CrossRef] [PubMed]
- Tsukada, S.; Kurosaka, K.; Nishino, M.; Hirasawa, N. Cutaneous Hypesthesia and Kneeling Ability After Total Knee Arthroplasty: A Randomized Controlled Trial Comparing Anterolateral and Anteromedial Skinncision. J. Arthroplast. 2018, 33, 3174–3180. [Google Scholar] [CrossRef]
- Hassaballa, M.; Artz, N.; Weale, A.; Porteous, A. Alteration in skin sensation following knee arthroplasty and its impact on kneeling ability: A comparison ofhree common surgical incisions. Knee Surg. Sports Traumatol. Arthrosc. 2012, 20, 1983–1987. [Google Scholar] [CrossRef]
- Laffosse, J.M.; Potapov, A.; Malo, M.; Lavigne, M.; Vendittoli, P.A. Hypesthesia after Anterolateral versus Midline Skinncision in TKA: A Randomized Study. Clin. Orthop. 2011, 469, 3154–3163. [Google Scholar] [CrossRef] [PubMed]
- Hopton, B.P.; Tommichan, M.C.; Howell, F.R. Reducing lateral skin flapumbness afterotal knee arthroplasty. Knee 2004, 11, 289–291. [Google Scholar] [CrossRef] [PubMed]
- Jariwala, A.C.; Parthasarathy, A.; Kiran, M.; Johnston, L.R.; Rowley, D.I. Numbness Aroundhe Total Knee Arthroplasty Surgical Scar: Prevalence and Effect on Functional Outcome. J. Arthroplast. 2017, 32, 2256–2261. [Google Scholar] [CrossRef] [PubMed]
- Tanavalee, A.; Limtrakul, A.; Veerasethsiri, P.; Amarase, C.; Ngarmukos, S. Area of Skin Numbness After Total Knee Arthroplasty: Does Minimallynvasive Approach Make Any Difference From Standard Approach? J. Arthroplast. 2016, 31, 2499–2503. [Google Scholar] [CrossRef] [PubMed]
- Şahin, F.; Beyaz, S.G.; Karakuş, N.; İnanmaz, M.E. Total Knee Arthroplasty Postsurgical Chronic Pain, Neuropathic Pain, andhe Prevalence of Neuropathic Symptoms: A Prospective Observational Study in Turkey. J. Pain Res. 2021, 14, 1315–1321. [Google Scholar] [CrossRef] [PubMed]
- Wylde, V.; Hewlett, S.; Learmonth, D.; Dieppe, P. Persistent pain after jointeplacement: Prevalence, sensory qualities, and postoperative determinants. Pain 2011, 152, 566–572. [Google Scholar] [CrossRef] [PubMed]
- Sharkey, P.F.; Miller, A.J. Noise, Numbness, and Kneeling Difficulties After Total Knee Arthroplasty. J. Arthroplast. 2011, 26, 1427–1431. [Google Scholar] [CrossRef] [PubMed]
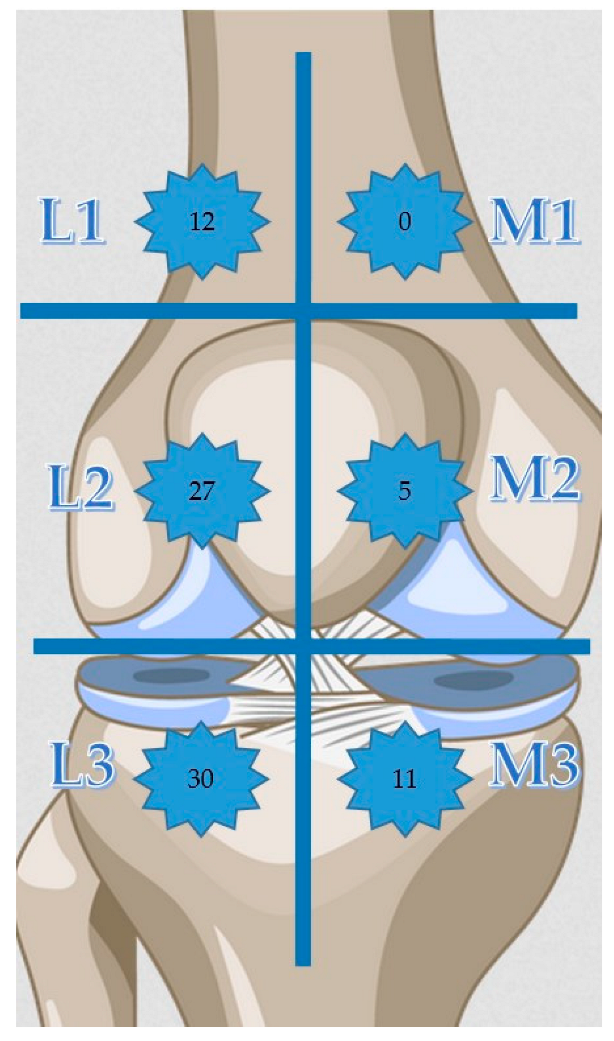
| n | L1 | L2 | L3 | M1 | M2 | M3 |
|---|---|---|---|---|---|---|
| 1 | - | + | - | - | - | - |
| 2 | - | + | + | - | - | + |
| 3 | - | + | - | - | - | - |
| 4 | - | + | + | - | - | - |
| 5 | - | + | + | - | - | - |
| 6 | - | + | + | - | - | - |
| 7 | + | + | + | - | - | - |
| 8 | + | + | + | - | - | - |
| 9 | + | + | + | - | - | - |
| 10 | + | + | + | - | - | - |
| 11 | - | - | + | - | - | - |
| 12 | - | + | + | - | - | - |
| 13 | - | + | + | - | - | - |
| 14 | + | + | + | - | - | - |
| 15 | + | + | + | - | - | - |
| 16 | - | + | + | - | - | - |
| 17 | + | + | + | - | - | - |
| 18 | - | + | + | - | - | - |
| 19 | + | + | + | - | + | + |
| 20 | + | + | + | - | - | - |
| 21 | - | + | + | - | - | - |
| 22 | + | + | + | - | + | + |
| 23 | - | + | + | - | - | - |
| 24 | - | + | + | - | - | - |
| 25 | + | + | + | - | - | + |
| 26 | - | - | + | - | - | + |
| 27 | - | - | + | - | - | + |
| 28 | - | + | + | - | - | + |
| 29 | - | - | + | - | + | + |
| 30 | - | + | + | - | - | + |
| 31 | - | - | + | - | + | + |
| 32 | - | - | - | - | + | + |
| 33 | + | + | + | - | - | - |
| PF | RLPH | RLEP | Energy | EW | SF | Pain | GH | HC | |
|---|---|---|---|---|---|---|---|---|---|
| N | 105 | 105 | 105 | 105 | 105 | 105 | 105 | 105 | 105 |
| Mean | 69.7 | 60.7 | 62.9 | 50.7 | 53.7 | 68.4 | 67.3 | 51.5 | 65.2 |
| Median | 75 | 75 | 66.7 | 55 | 56.0 | 75.0 | 67.5 | 50 | 75 |
| Standard deviation | 18.8 | 20.5 | 25.5 | 8.55 | 6.51 | 18.4 | 22.5 | 6.54 | 21.8 |
| Minimum | 10 | 0 | 0.00 | 25 | 32.0 | 12.5 | 10.0 | 35 | 25 |
| Maximum | 95 | 100 | 100 | 70 | 68.0 | 100 | 100 | 70 | 100 |
| Skewness | −1.36 | −0.516 | −0.466 | −0.635 | −0.736 | −0.243 | −0.493 | −0.251 | −0.210 |
| Std. error skewness | 0.236 | 0.236 | 0.236 | 0.236 | 0.236 | 0.236 | 0.236 | 0.236 | 0.236 |
| Kurtosis | 1.44 | 0.406 | 0.135 | 0.530 | 1.05 | 0.210 | −0.362 | 0.230 | −0.578 |
| Std. error kurtosis | 0.467 | 0.467 | 0.467 | 0.467 | 0.467 | 0.467 | 0.467 | 0.467 | 0.467 |
| Shapiro–Wilk W | 0.858 | 0.856 | 0.833 | 0.927 | 0.934 | 0.918 | 0.934 | 0.941 | 0.872 |
| Shapiro–Wilk p | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Wpain | Wstiff | WPFunc | WOMAC | |
|---|---|---|---|---|
| N | 105 | 105 | 105 | 105 |
| Mean | 5.77 | 2.27 | 20.0 | 29.2 |
| Median | 5 | 2 | 18 | 25.0 |
| Standard deviation | 3.81 | 1.61 | 12.8 | 18.6 |
| Minimum | 1 | 0 | 4 | 5.21 |
| Maximum | 15 | 6 | 51 | 72.9 |
| Skewness | 0.618 | 0.461 | 0.622 | 0.636 |
| Std. error skewness | 0.236 | 0.236 | 0.236 | 0.236 |
| Kurtosis | −0.588 | −0.741 | −0.476 | −0.483 |
| Std. error kurtosis | 0.467 | 0.467 | 0.467 | 0.467 |
| Shapiro–Wilk W | 0.915 | 0.907 | 0.923 | 0.926 |
| Shapiro–Wilk p | < 0.001 | <0 .001 | < 0.001 | <0 .001 |
| Predictor | Estimate (β) | SE | Z | p | Odds Ratio |
|---|---|---|---|---|---|
| POFT | 0.0517 | 0.0173 | 2.987 | 0.003 | 1.053 |
| Age | 0.0102 | 0.0343 | 0.297 | 0.766 | 1.010 |
| INS | −0.0150 | 0.1360 | −0.110 | 0.912 | 0.985 |
| BL | 0.0346 | 0.2928 | 0.118 | 0.906 | 1.035 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gurler, D.; Buyukceran, I. Is the Numbness after Knee Replacement a More Critical Complication Than Thought? A Detailed Analysis of Neuropathic Pain and Functional Outcomes. Medicina 2022, 58, 1369. https://doi.org/10.3390/medicina58101369
Gurler D, Buyukceran I. Is the Numbness after Knee Replacement a More Critical Complication Than Thought? A Detailed Analysis of Neuropathic Pain and Functional Outcomes. Medicina. 2022; 58(10):1369. https://doi.org/10.3390/medicina58101369
Chicago/Turabian StyleGurler, Deniz, and Ismail Buyukceran. 2022. "Is the Numbness after Knee Replacement a More Critical Complication Than Thought? A Detailed Analysis of Neuropathic Pain and Functional Outcomes" Medicina 58, no. 10: 1369. https://doi.org/10.3390/medicina58101369
APA StyleGurler, D., & Buyukceran, I. (2022). Is the Numbness after Knee Replacement a More Critical Complication Than Thought? A Detailed Analysis of Neuropathic Pain and Functional Outcomes. Medicina, 58(10), 1369. https://doi.org/10.3390/medicina58101369








