Vitamin D Deficiency as a Risk Factor for Myocardial Ischemia
Abstract
1. Introduction
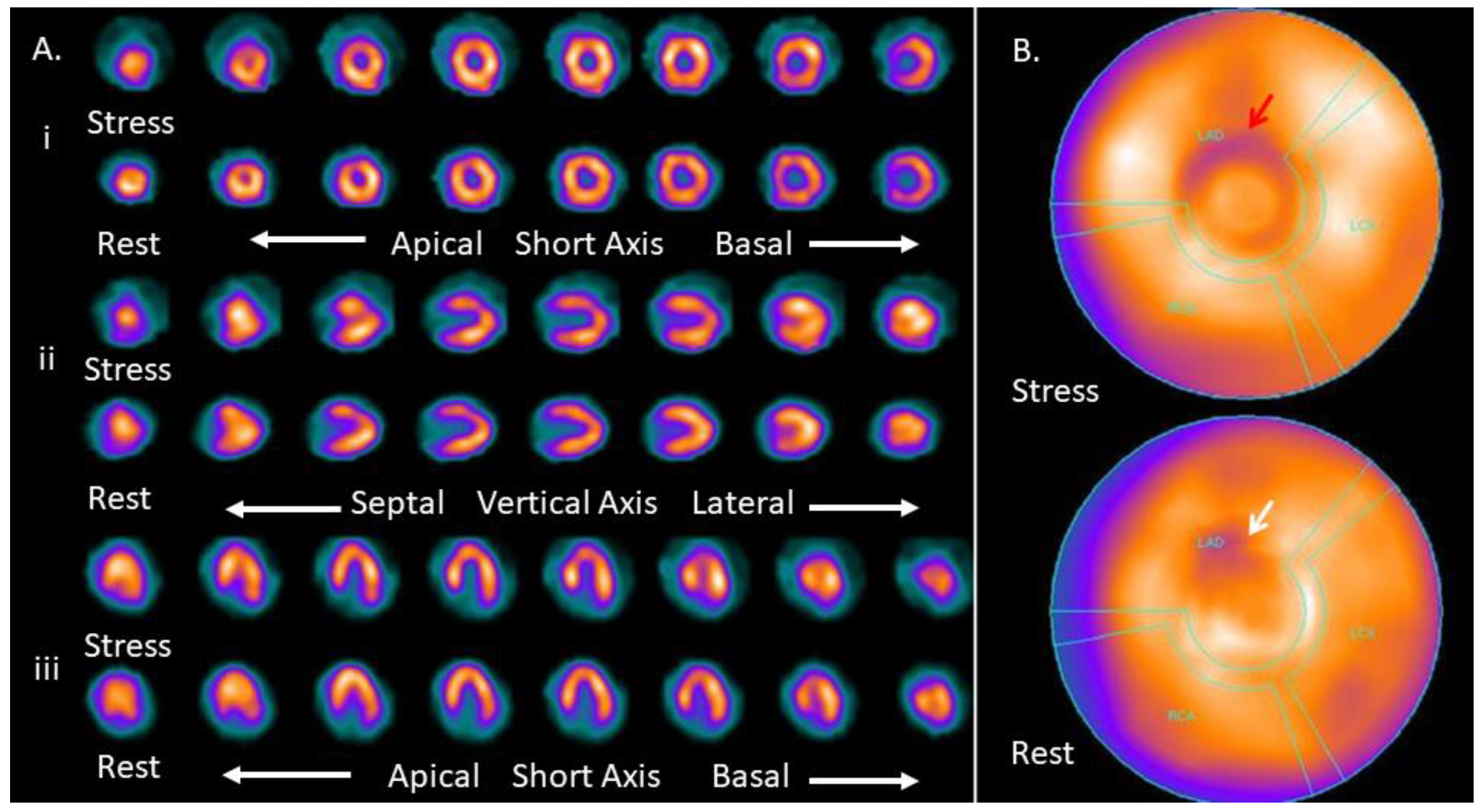
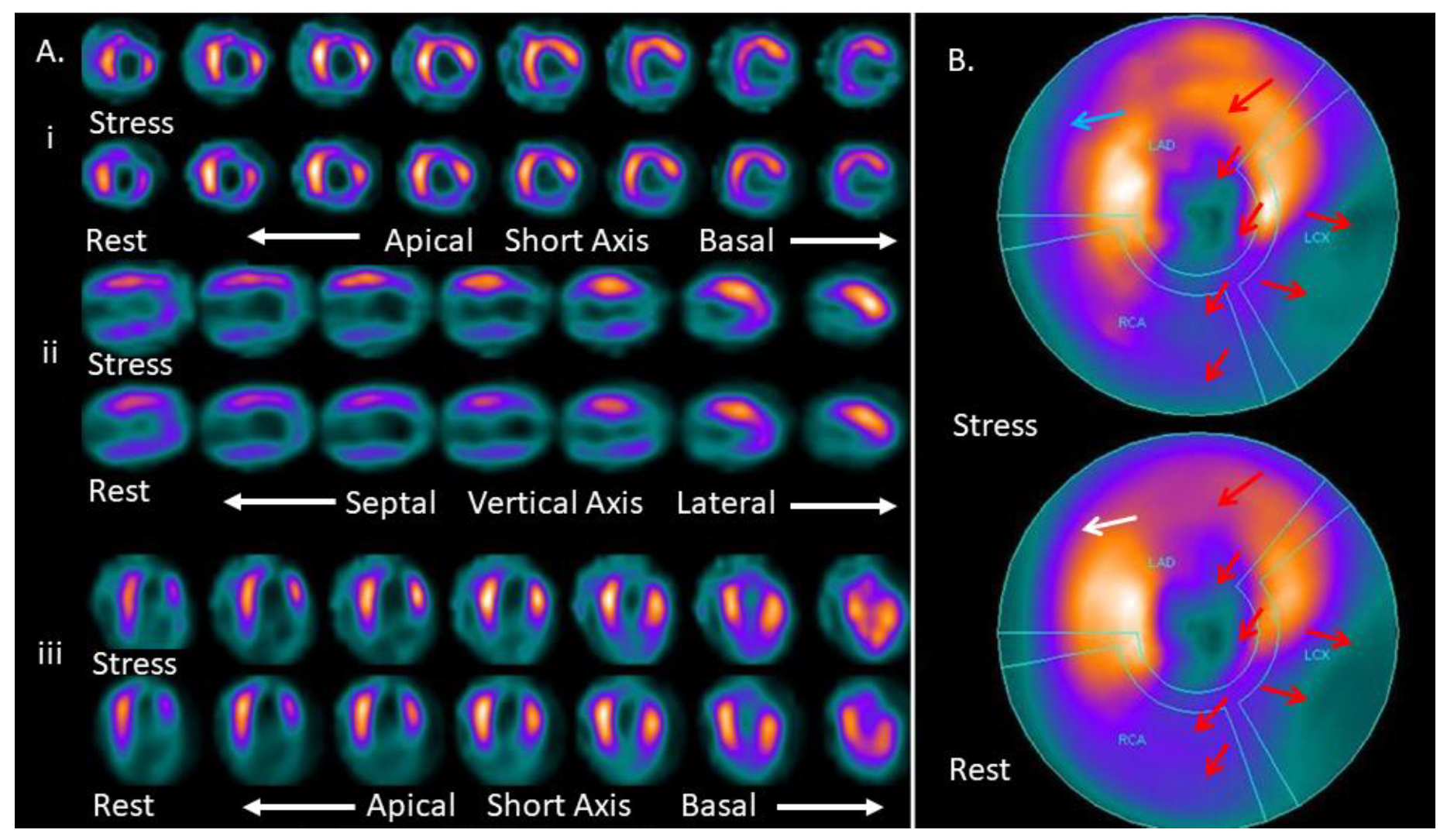
2. Materials and Methods
2.1. Participants and Procedures
2.2. Statistical Analysis
2.3. Ethics
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hung, C.L.; Chien, D.K.; Shih, S.C.; Chang, W.H. The feasibility and diagnostic accuracy by multiple cardiac biomarkers in emergency chest pain patients: A clinical analysis to compare 290 suspected acute coronary syndrome cases stratified by age and gender in Taiwan. BMC Cardiovasc. Disord. 2016, 16, 191. [Google Scholar] [CrossRef]
- Lim, W.Y.; Thevarajah, T.M.; Goh, B.T.; Khor, S.M. Paper microfluidic device for early diagnosis and prognosis of acute myocardial infarction via quantitative multiplex cardiac biomarker detection. Biosens. Bioelectron. 2019, 128, 176–185. [Google Scholar] [CrossRef] [PubMed]
- Carvajal-Zarrabal, O.; Hayward-Jones, P.M.; Nolasco-Hipolito, C.; Barradas-Dermitz, D.M.; Calderón-Garcidueñas, A.L.; López-Amador, N. Use of Cardiac Injury Markers in the Postmortem Diagnosis of Sudden Cardiac Death. J. Forensic Sci. 2017, 62, 1332–1335. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; O’Keefe, J.H.; Bell, D.; Hensrud, D.D.; Holick, M.F. Vitamin D deficiency an important, common, and easily treatable cardiovascular risk factor? J. Am. Coll. Cardiol. 2008, 52, 1949–1956. [Google Scholar] [CrossRef] [PubMed]
- Sioka, C.; Kyritsis, A.P.; Fotopoulos, A. Multiple sclerosis, osteoporosis, and vitamin D. J. Neurol. Sci. 2009, 287, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Sioka, C.; Papakonstantinou, S.; Markoula, S.; Gkartziou, F.; Georgiou, A.; Georgiou, I.; Pelidou, S.H.; Kyritsis, A.P.; Fotopoulos, A. Vitamin D receptor gene polymorphisms in multiple sclerosis patients in northwest Greece. J. Negat. Results Biomed. 2011, 10, 3. [Google Scholar] [CrossRef]
- Sioka, C.; Fotopoulos, A.; Georgiou, A.; Xourgia, X.; Papadopoulos, A.; Kalef-Ezra, J.A. Age at menarche, age at menopause and duration of fertility as risk factors for osteoporosis. Climacteric 2010, 13, 63–71. [Google Scholar] [CrossRef]
- Sioka, C.; Bougias, C.; Papadopoulos, A.; Fotopoulos, A. Is osteoporosis in postmenopausal female patients related to previous pregnancies and/or miscarriages? Climacteric 2007, 10, 381–385. [Google Scholar] [CrossRef] [PubMed]
- Sioka, C.; Fotopoulos, A.; Papakonstantinou, S.; Georgiou, A.; Pelidou, S.H.; Kyritsis, A.P.; Kalef-Ezra, J.A. The effect of menarche age, parity and lactation on bone mineral density in premenopausal ambulatory multiple sclerosis patients. Mult. Scler. Relat. Disord. 2015, 4, 287–290. [Google Scholar] [CrossRef]
- Markoula, S.; Sioka, C.; Exarchopoulos, T.; Chatzistefanidis, D.; Kalef-Ezra, J.; Fotopoulos, A.; Kyritsis, A.P. Gender specific association of decreased bone mineral density in patients with epilepsy. Neurol. Neurochir. Pol. 2015, 49, 267–271. [Google Scholar] [CrossRef]
- Sioka, C.; Fotopoulos, A.; Georgiou, A.; Papakonstantinou, S.; Pelidou, S.H.; Kyritsis, A.P.; Kalef-Ezra, J.A. Body composition in ambulatory patients with multiple sclerosis. J. Clin. Densitom. 2011, 14, 465–470. [Google Scholar] [CrossRef]
- Sioka, C.; Papakonstantinou, S.; Fotopoulos, A.; Alamanos, Y.; Georgiou, A.; Tsouli, S.; Pelidou, S.H.; Kyritsis, A.P.; Kalef-Ezra, J. Bone mineral density in ambulatory patients with multiple sclerosis. Neurol. Sci. 2011, 32, 819–824. [Google Scholar] [CrossRef]
- Sioka, C.; Baldouma, A.; Papadopoulos, A.; Petrikis, P.; Batsi, C.; Kostadima, V.; Fotopoulos, A.; Kyritsis, A.P. Co-Existence of Depression, Low Bone Mineral Density, and Vitamin D Deficiency in Patients with Multiple Sclerosis. Psychiatr. Danub. 2021, 33, 201. [Google Scholar]
- Sioka, C.; Bougias, C.; Al-Bokharhli, J.; Fotopoulos, A. Smoking and alcohol use as risk factors for low bone mineral density. Rheumatol. Int. 2006, 27, 207–208. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, R.; Liu, Y.; Bai, L.; Liu, L.; He, L.; Deng, H.; Li, T.; Xu, S.; Chen, L.; et al. Associations between bone mineral density in different measurement locations and coronary artery disease: A cross-sectional study. Arch. Osteoporos 2021, 16, 100. [Google Scholar]
- Park, J.; Yoon, Y.E.; Kim, K.M.; Hwang, I.C.; Lee, W.; Cho, G.Y. Prognostic value of lower bone mineral density in predicting adverse cardiovascular disease in Asian women. Heart 2021, 7, 1040–1046. [Google Scholar] [CrossRef] [PubMed]
- Sioka, C.; Goudevenos, J.; Pappas, K.; Bougias, C.; Papadopoulos, A.; Grammatikopoulos, K.; Fotopoulos, A. Bone mineral density and coronary atherosclerosis. Calcif. Tissue. Int. 2007, 81, 333. [Google Scholar] [CrossRef] [PubMed]
- Ahmadi, N.; Mao, S.S.; Hajsadeghi, F.; Arnold, B.; Kiramijyan, S.; Gao, Y.; Flores, F.; Azen, S.; Budoff, M. The relation of low levels of bone mineral density with coronary artery calcium and mortality. Osteoporos. Int. 2018, 29, 1609–1616. [Google Scholar] [CrossRef]
- Wacker, M.; Holick, M.F. Sunlight and Vitamin D: A global perspective for health. Dermatoendocrinol 2013, 5, 51–108. [Google Scholar] [CrossRef] [PubMed]
- Mozos, I.; Marginean, O. Links between Vitamin D Deficiency and Cardiovascular Diseases. Biomed. Res. Int. 2015, 2015, 109275. [Google Scholar] [CrossRef]
- El Mokadem, M.; Boshra, H.; Abd El Hady, Y.; Abd El Hameed, A.S. Relationship of serum vitamin D deficiency with coronary artery disease severity using multislice CT coronary angiography. Clin. Investig. Arterioscler. 2021. [Google Scholar] [CrossRef]
- Ozer, P.K.; Emet, S.; Karaayvaz, E.B.; Elitok, A.; Bilge, A.K.; Adalet, K.; Oncul, A. Silent myocardial dysfunction in vitamin D deficiency. Arch. Med. Sci. Atheroscler. Dis. 2020, 5, e153–e162. [Google Scholar] [CrossRef] [PubMed]
- Saraste, A.; Knuuti, J. ESC 2019 guidelines for the diagnosis and management of chronic coronary syndromes: Recommendations for cardiovascular imaging. Herz 2020, 45, 409–420. [Google Scholar] [CrossRef]
- Sioka, C.; Nikas, D.; Tsoumani, A.; Kiortsis, D.N.; Fotopoulos, A.; Kostadima, V. Transient myocardial ischemia due to corticosteroid use in a patient with multiple sclerosis diagnosed with myocardial perfusion imaging. J. Nucl. Cardiol. 2020. [Google Scholar] [CrossRef]
- Kotsalou, I.; Georgoulias, P.; Karydas, I.; Fourlis, S.; Sioka, C.; Zoumboulidis, A.; Demakopoulos, N. A rare case of myocardial infarction and ischemia in a cannabis-addicted patient. Clin. Nucl. Med. 2007, 32, 130–131. [Google Scholar] [CrossRef]
- Sioka, C.; Exarchopoulos, T.; Tasiou, I.; Tzima, E.; Fotou, N.; Capizzello, A.; Ragos, V.; Tsekeris, P.; Fotopoulos, A. Myocardial perfusion imaging with (99 m)Tc-tetrofosmin SPECT in breast cancer patients that received postoperative radiotherapy: A case-control study. Radiat. Oncol. 2011, 6, 151. [Google Scholar] [CrossRef] [PubMed]
- Fotopoulos, A.; Petrikis, P.; Iakovou, I.; Papadopoulos, A.; Sakelariou, K.; Gkika, E.; Lakkas, L.; Touzios, C.; Pappas, K.; Klaroudas, A.; et al. The impact of depression and anxiety in prognosis of patients undergoing myocardial perfusion imaging with 99mTc tetrofosmin SPECT for evaluation of possible myocardial ischemia. Nucl. Med. Rev. Cent. East. Eur. 2020, 23, 58–62. [Google Scholar] [CrossRef]
- Sioka, C.; Papadimitropoulos, K.; Michalis, L.; Pappas, K.; Lakkas, L.; Fotopoulos, A.; Dounousi, E. Myocardial ischemia with normal coronary angiography in a chronic kidney disease patient. Cardiol. J. 2019, 26, 620–621. [Google Scholar] [CrossRef]
- Giannopoulos, S.; Markoula, S.; Sioka, C.; Zouroudi, S.; Spiliotopoulou, M.; Naka, K.K.; Michalis, L.K.; Fotopoulos, A.; Kyritsis, A.P. Detecting myocardial Ischemia With (99m)Technetium-Tetrofosmin Myocardial Perfusion Imaging in Ischemic Stroke. Neurohospitalist 2017, 7, 164–168. [Google Scholar] [CrossRef] [PubMed]
- Iskandar, A.; Limone, B.; Parker, M.W.; Perugini, A.; Kim, H.; Jones, C.; Calamari, B.; Coleman, C.I.; Heller, G.V. Gender differences in the diagnostic accuracy of SPECT myocardial perfusion imaging: A bivariate meta-analysis. J. Nucl. Cardiol. 2013, 20, 53–63. [Google Scholar] [CrossRef] [PubMed]
- Verberne, H.J.; Acampa, W.; Anagnostopoulos, C.; Ballinger, J.; Bengel, F.; De Bondt, P.; Buechel, R.R.; Cuocolo, A.; van Eck-Smit, B.L.; Flotats, A.; et al. EANM procedural guidelines for radionuclide myocardial perfusion imaging with SPECT and SPECT/CT: 2015 revision. Eur. J. Nucl. Med. Mol. Imaging. 2015, 42, 1929–1940. [Google Scholar] [CrossRef] [PubMed]
- Fotopoulos, A.; Papadimitropoulos, K.; Papadopoulos, A.; Lakkas, L.; Spiliotopoulou, M.; Kotrotsios, T.D.; Pappas, K.; Notopoulos, A.; Sioka, C. Myocardial ischemia in female patients with rheumatoid arthritis assessed with single photon emission tomography-myocardial perfusion imaging. Nucl. Med. Rev. Cent. East. Eur. 2019, 22, 8–13. [Google Scholar] [PubMed]
- Michas, G.; Karvelas, G.; Trikas, A. Cardiovascular disease in Greece; the latest evidence on risk factors. Hellenic J. Cardiol. 2019, 60, 271–275. [Google Scholar] [CrossRef]
- Mangla, A.; Oliveros, E.; Williams, K.A., Sr.; Kalra, D.K. Cardiac Imaging in the Diagnosis of Coronary Artery Disease. Curr. Probl. Cardiol. 2017, 42, 316–366. [Google Scholar] [CrossRef]
- Jaarsma, C.; Leiner, T.; Bekkers, S.C.; Crijns, H.J.; Wildberger, J.E.; Nagel, E.; Nelemans, P.J.; Schalla, S. Diagnostic performance of noninvasive myocardial perfusion imaging using single-photon emission computed tomography, cardiac magnetic resonance, and positron emission tomography imaging for the detection of obstructive coronary artery disease: A meta-analysis. J. Am. Coll. Cardiol. 2012, 59, 1719–1728. [Google Scholar] [PubMed]
- Holick, M.F. High prevalence of vitamin D inadequacy and implications for health. Mayo. Clin. Proc. 2006, 81, 353–373. [Google Scholar] [CrossRef]
- Płudowski, P.; Grant, W.B.; Bhattoa, H.P.; Bayer, M.; Povoroznyuk, V.; Rudenka, E.; Ramanau, H.; Varbiro, S.; Rudenka, A.; Karczmarewicz, E.; et al. Vitamin D Status in Central Europe. Int. J. Endocrinol. 2014, 589587. [Google Scholar] [CrossRef] [PubMed]
- Manios, Y.; Moschonis, G.; Hulshof, T.; Bourhis, A.S.; Hull, G.L.J.; Dowling, K.G.; Kiely, M.E.; Cashman, K.D. Prevalence of vitamin D deficiency and insufficiency among schoolchildren in Greece: The role of sex, degree of urbanisation and seasonality. Br. J. Nutr. 2017, 118, 550–558. [Google Scholar] [CrossRef][Green Version]
- Hilger, J.; Friedel, A.; Herr, R.; Rausch, T.; Roos, F.; Wahl, D.A.; Pierroz, D.D.; Weber, P.; Hoffmann, K. A systematic review of vitamin D status in populations worldwide. Br. J. Nutr. 2014, 111, 23–45. [Google Scholar] [CrossRef]
- Pittas, A.G.; Chung, M.; Trikalinos, T.; Mitri, J.; Brendel, M.; Patel, K.; Lichtenstein, A.H.; Lau, J.; Balk, E.M. Systematic review: Vitamin D and cardiovascular outcomes. Ann. Intern. Med. 2010, 152, 307–314. [Google Scholar] [CrossRef]
- Kunadian, V.; Ford, G.A.; Bawamia, B.; Qiu, W.; Manson, J.E. Vitamin D deficiency and coronary artery disease: A review of the evidence. Am. Heart J. 2014, 167, 283–291. [Google Scholar] [CrossRef] [PubMed]
- Elamin, M.B.; Abu Elnour, N.O.; Elamin, K.B.; Fatourechi, M.M.; Alkatib, A.A.; Almandoz, J.P.; Liu, H.; Lane, M.A.; Mullan, R.J.; Hazem, A.; et al. Vitamin D and cardiovascular outcomes: A systematic review and meta-analysis. J. Clin. Endocrinol. Metab. 2011, 96, 1931–1942. [Google Scholar] [CrossRef]
- Norouzi, H.; Ziaie, N.; Saravi, M.; Norouzi, A.; Noei-Teymoordash, S.; Jokar-Darzi, F.; Norouzi, F.; Rajabi-Fumashi, M.; Zahedi-Tajrishi, F.; Norouzi, S. Association of vitamin D deficiency and premature coronary artery disease. Caspian J. Intern. Med. 2019, 10, 80–85. [Google Scholar] [PubMed]
- Aleksova, A.; Belfiore, R.; Carriere, C.; Kassem, S.; La Carrubba, S.; Barbati, G.; Sinagra, G. Vitamin D Deficiency in Patients with Acute Myocardial Infarction: An Italian Single-Center Study. Int. J. Vitam. Nutr. Res. 2015, 85, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Akter, K.; Khalilullah, I.; Saqueeb, S.N.; Islam, A.; Zaman, M.S.; Rahman, M.; Rokonujjaman, M.; Wadud, M.A.; Aziz, S.; Rahman, M.A.; et al. Level of Serum Vitamin D, To Which People Are at Risk of Developing Acute Myocardial Infarction in Bangladesh. Mymensingh Med. J. 2021, 30, 176–181. [Google Scholar]
- Verdoia, M.; Schaffer, A.; Barbieri, L.; Di Giovine, G.; Marino, P.; Suryapranata, H.; De Luca, G. Novara Atherosclerosis Study Group (NAS). Impact of gender difference on vitamin D status and its relationship with the extent of coronary artery disease. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 464–470. [Google Scholar] [CrossRef]
- Davies, R.E.; Rier, J.D. Gender Disparities in CAD: Women and Ischemic Heart Disease. Curr. Atheroscler. Rep. 2018, 20, 51. [Google Scholar] [CrossRef]
- Waheed, N.; Elias-Smale, S.; Malas, W.; Maas, A.H.; Sedlak, T.L.; Tremmel, J.; Mehta, P.K. Sex differences in non-obstructive coronary artery disease. Cardiovasc. Res. 2020, 116, 829–840. [Google Scholar] [CrossRef]
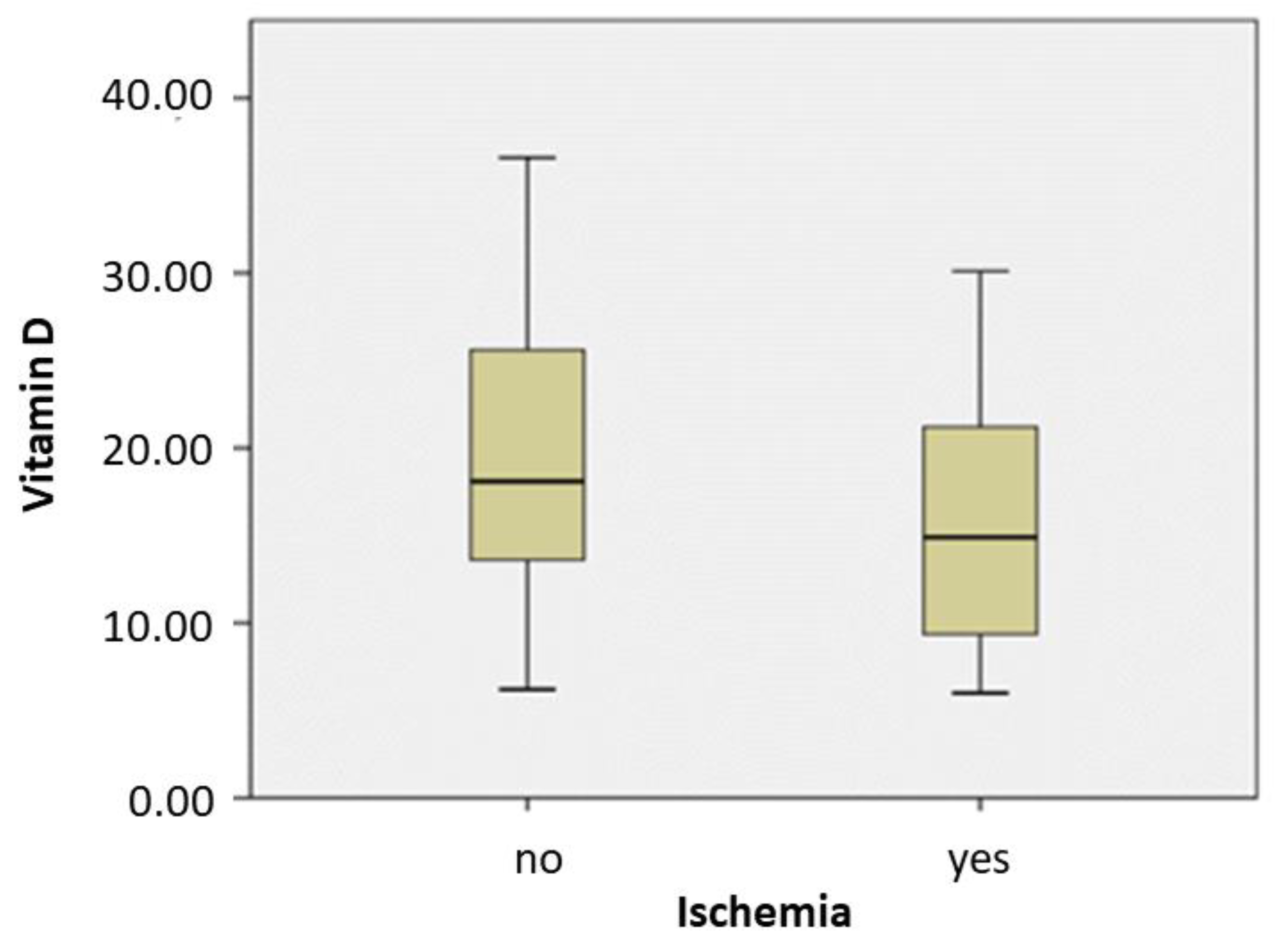
| Variable | Groups | Median (Minimum, Maximum) | p-Value (Mann-Whitney U-Test) |
|---|---|---|---|
| ischemia | No | 18.1 (6.2, 36.6) | 0.013 |
| Yes | 14.9 (6.0, 30.1) | ||
| gender | Male | 14.9 (6.0, 28.7) | 0.153 |
| Female | 17.4 (6.0, 36.6) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Batsi, C.; Gkika, E.; Astrakas, L.; Papadopoulos, A.; Iakovou, I.; Dogoritis, A.; Fotopoulos, A.; Sioka, C. Vitamin D Deficiency as a Risk Factor for Myocardial Ischemia. Medicina 2021, 57, 774. https://doi.org/10.3390/medicina57080774
Batsi C, Gkika E, Astrakas L, Papadopoulos A, Iakovou I, Dogoritis A, Fotopoulos A, Sioka C. Vitamin D Deficiency as a Risk Factor for Myocardial Ischemia. Medicina. 2021; 57(8):774. https://doi.org/10.3390/medicina57080774
Chicago/Turabian StyleBatsi, Christina, Evangelia Gkika, Loukas Astrakas, Athanassios Papadopoulos, Ioannis Iakovou, Alexandros Dogoritis, Andreas Fotopoulos, and Chrissa Sioka. 2021. "Vitamin D Deficiency as a Risk Factor for Myocardial Ischemia" Medicina 57, no. 8: 774. https://doi.org/10.3390/medicina57080774
APA StyleBatsi, C., Gkika, E., Astrakas, L., Papadopoulos, A., Iakovou, I., Dogoritis, A., Fotopoulos, A., & Sioka, C. (2021). Vitamin D Deficiency as a Risk Factor for Myocardial Ischemia. Medicina, 57(8), 774. https://doi.org/10.3390/medicina57080774








