Implant Placement after Closure of Oroantral Communication by Sinus Bone Graft Using a Collagen Barrier Membrane in the Shape of a Pouch: A Case Report and Review of the Literature
Abstract
1. Introduction
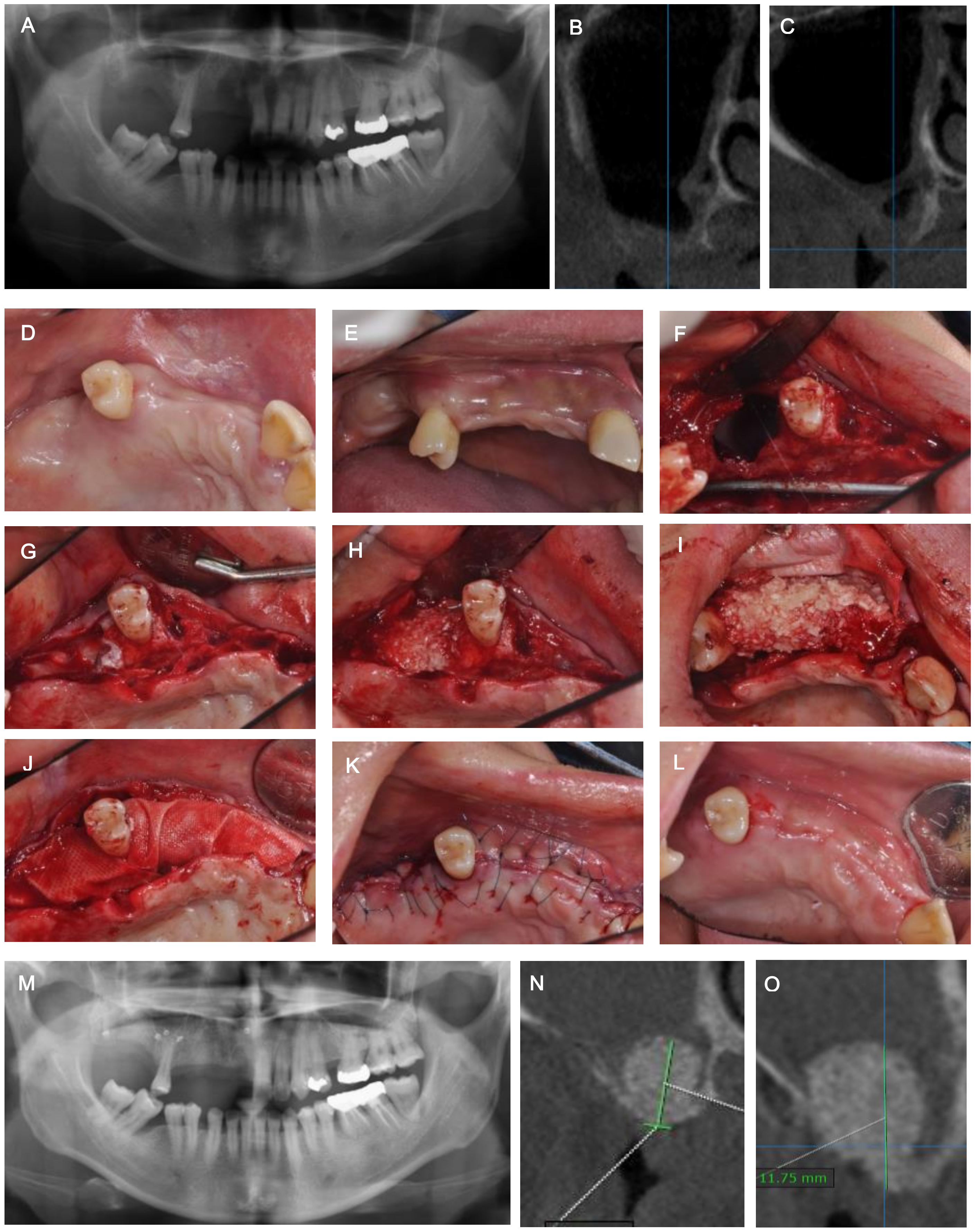
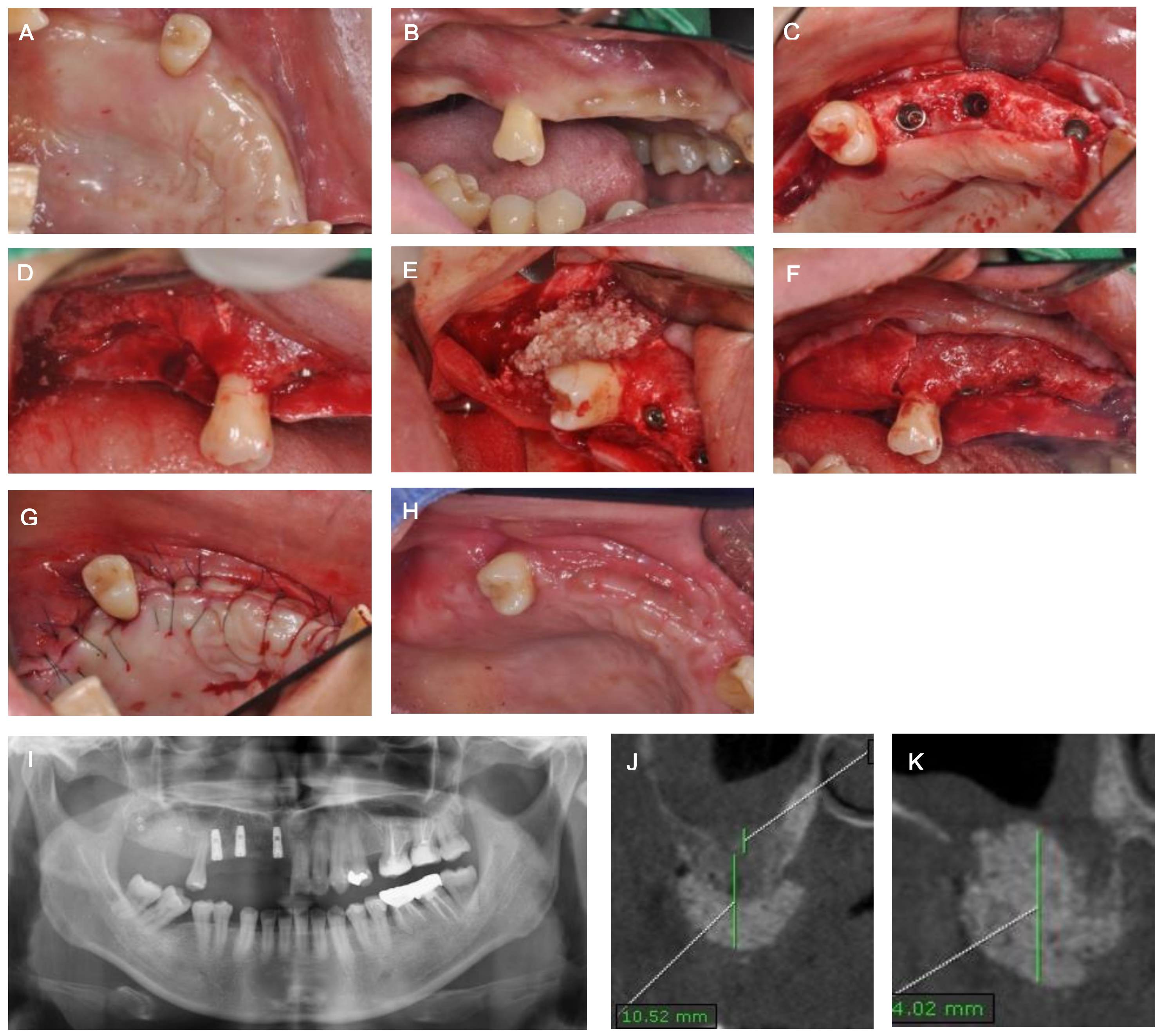
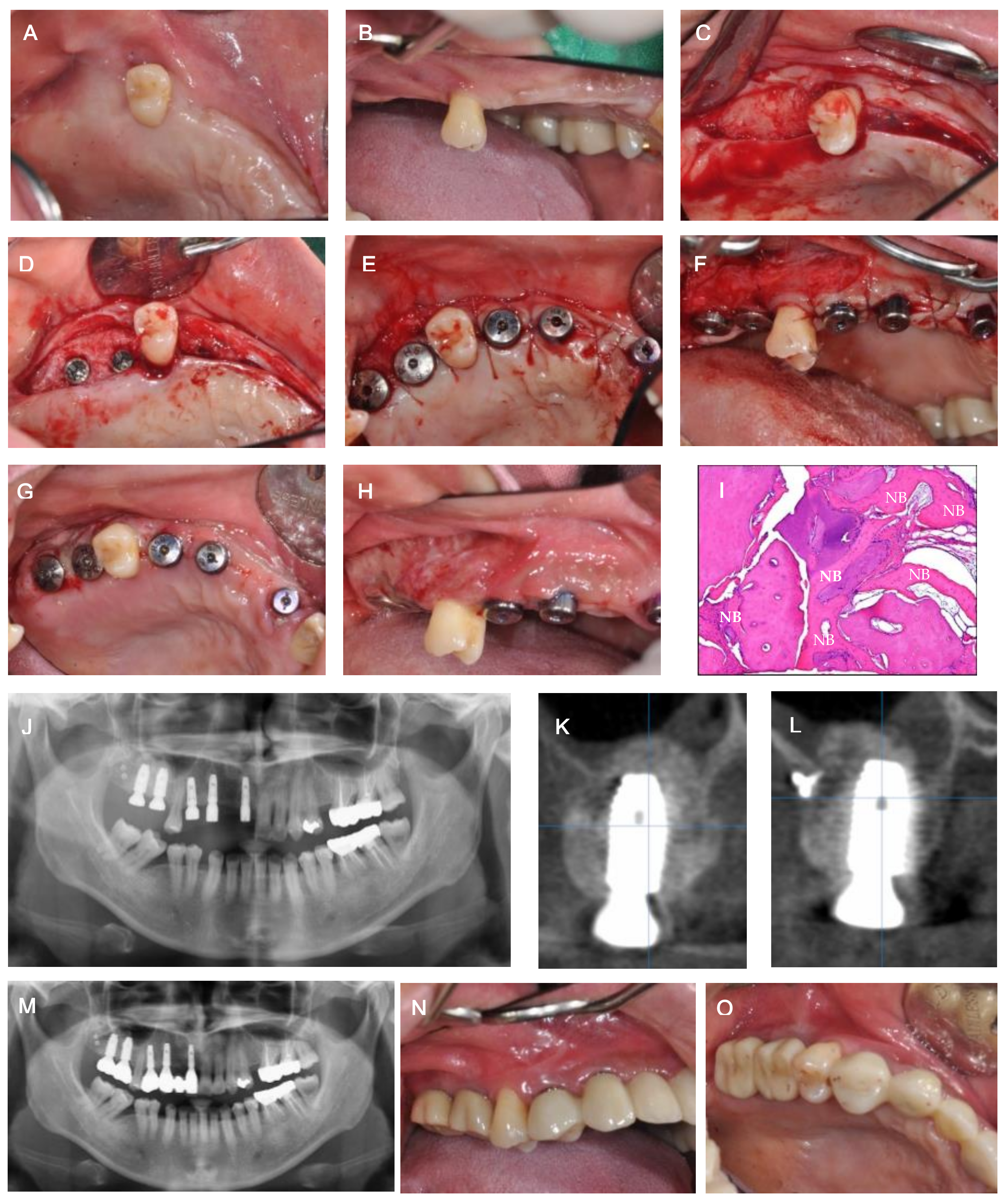
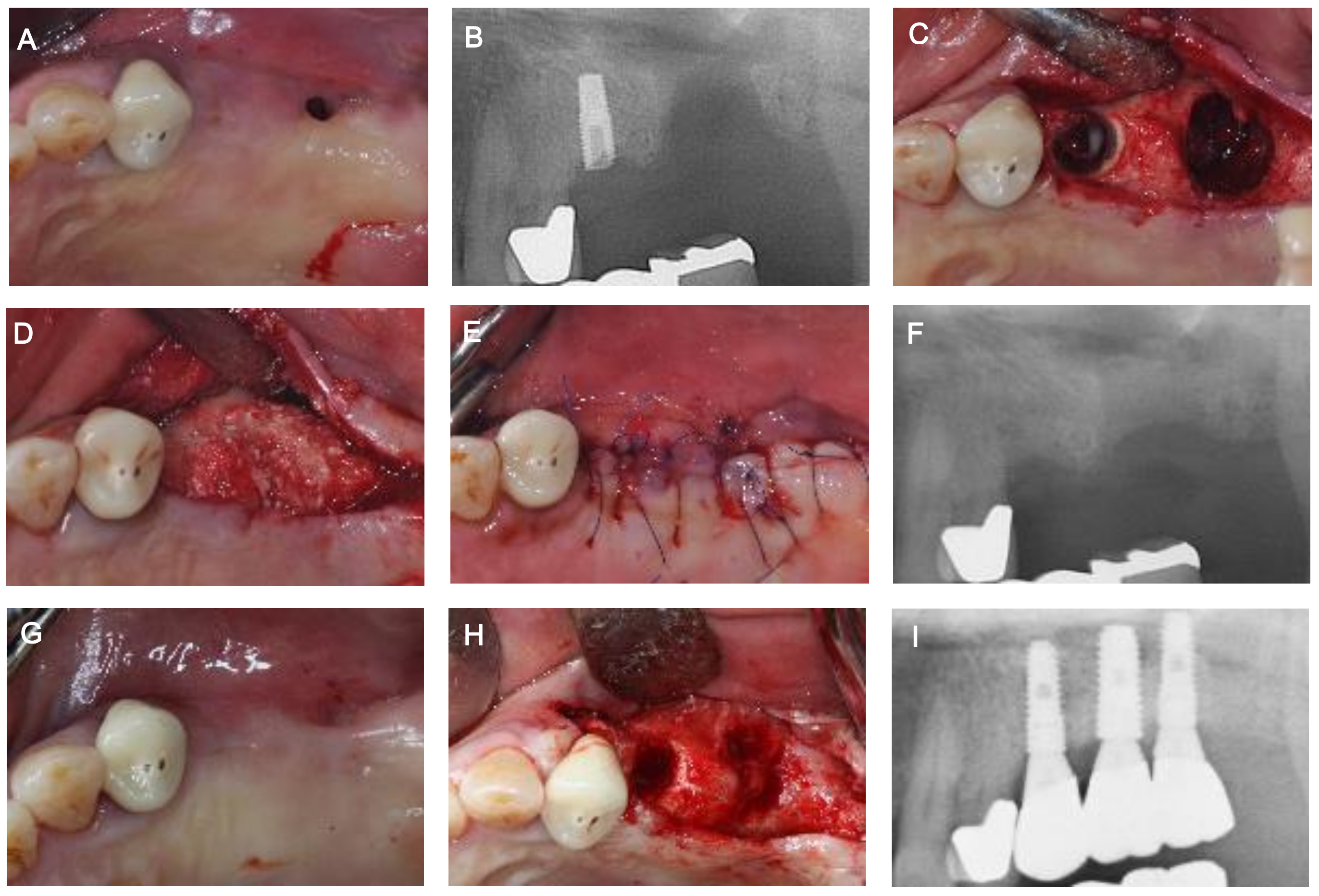
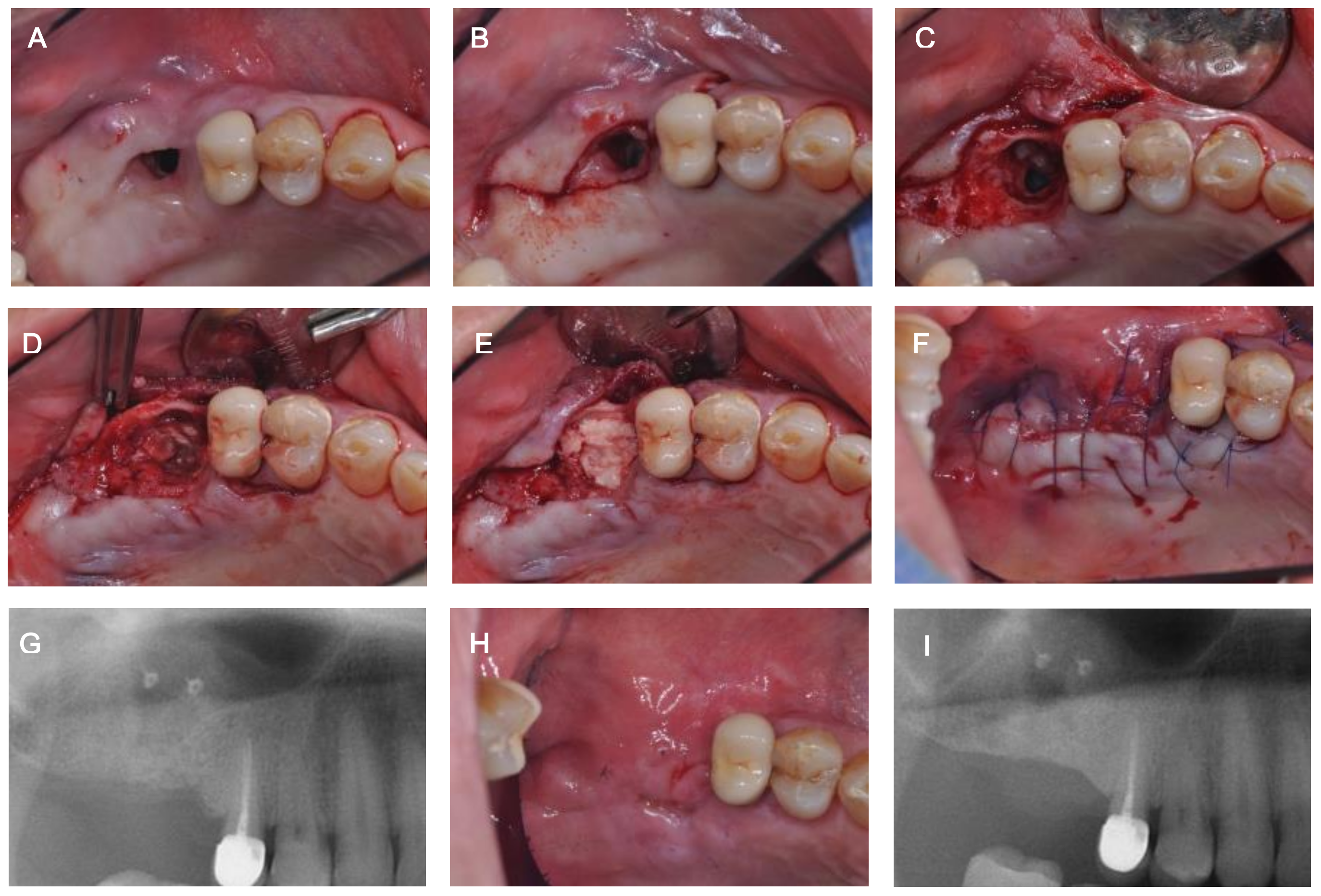
2. Case Description
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Logan, R.M.; Coates, E.A. Non-surgical management of an oro-antral fistula in a patient with HIV infection. Aust. Dent. J. 2003, 48, 255–258. [Google Scholar] [PubMed]
- Yalcın, S.; Öncü, B.; Emes, Y.; Atalay, B.; Aktas, I. Surgical treatment of oroantral fistulas: A clinical study of 23 Cases. J. Oral Maxillofac. Surg. 2011, 69, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Parvini, P.; Obreja, K.; Sader, R.; Becker, J.; Schwarz, F.; Salti, L. Decision-making in closure of oroantral communication and fistula. Int. J. Implant Dent. 2019, 5, 13. [Google Scholar] [CrossRef] [PubMed]
- Parvini, P.; Obreja, K.; Sader, R.; Becker, J.; Schwarz, F.; Salti, L. Surgical options in oroantral fistula management: A narrative review. Int. J. Implant Dent. 2018, 4, 40. [Google Scholar] [CrossRef] [PubMed]
- Liversedge, R.L.; Wong, K. Use of the buccal fat pad in maxillary and sinus grafting of the severely atrophic maxilla preparatory to implant reconstruction of the partially or completely edentulous patient: Technical note. Int. J. Oral Maxillofac. Implant. 2002, 17, 424–428. [Google Scholar]
- Kraut, R.A.; Smith, R.V. Team approach for closure of oroantral and oronasal fistulae. Atlas Oral Maxillofac. Surg. Clin. N. Am. 2000, 8, 55–75. [Google Scholar] [CrossRef]
- Visscher, S.H.; Minnen, B.; Bos, R. Closure of oroantral communications: A review of the literature. J. Oral Maxillofac. Surg. 2010, 68, 1384–1391. [Google Scholar] [CrossRef] [PubMed]
- Nezafati, S.; Vafaii, A.; Ghojazadeh, M. Comparison of pedicled buccal fat pad flap with buccal flap for closure of oro-antral communication. Int. J. Oral Maxillofac. Surg. 2012, 41, 624–628. [Google Scholar] [CrossRef] [PubMed]
- Borgonovo, A.E.; Berardinelli, F.V.; Favale, M.; Maiorana, C. Surgical Options in Oro-antral Fistula Treatment. Open Dent. J. 2012, 6, 94–98. [Google Scholar] [CrossRef] [PubMed]
- Doobrow, J.H.; Leite, R.S.; Hirsch, H.Z. Concomitant oroantral communication repair and immediate implant placement: A five-year case report. Implant Dent. 2008, 17, 176–181. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.P.; Kwon, Y.S. Vestibuloplasty around dental implants using modified periosteal fenestration (mPF): Case series. Implantology 2020, 24, 22–30. [Google Scholar] [CrossRef]
- Park, D.Y.; Lee, W.P. Vestibuloplasty around teeth and dental implants using simplified periosteal fenestration (sPF): Case Reports. J. Kor. Dent. Assoc. 2020, 59, 20–27. [Google Scholar] [CrossRef]
- Proctor, B. Bone graft closure of large or persistent oro-maxillary fistula. Laryngoscope 1969, 79, 822. [Google Scholar] [CrossRef] [PubMed]
- Isler, S.C.; Demircan, S.; Cansiz, E. Closure of oroantral fistula using auricular cartilage: A new method to repair an oroantral fistula. Br. J. Oral Maxillofac. Surg. 2011, 49, e86–e87. [Google Scholar] [CrossRef] [PubMed]
- Scattarella, A.; Ballini, A.; Grassi, F.R.; Carbonara, A.; Ciccolella, F.; Dituri, A.; Nardi, G.M.; Cantore, S.; Pettini, F. Treatment of oroantral fistula with autologous bone graft and application of a non-reabsorbable membrane. Int. J. Med. Sci. 2010, 7, 267–271. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ogunsalu, C. A new surgical management for oro-antral communication: The resorbable guided tissue regeneration membrane-bone substitute sandwich technique. West Indian Med. J. 2005, 54, 261–263. [Google Scholar] [CrossRef] [PubMed]
- Proussaefs, P.; Lozada, J. The “Loma Linda Pouch”: A Technique for Repairing the Perforated Sinus Membrane. Int. J. Periodontics Restor. Dent. 2003, 23, 593–597. [Google Scholar]
- Testori, T.; Wallace, S.S.; Del Fabbro, M.; Taschieri, S.; Trisi, P.; Capelli, M.; Weinstein, R.L. Repair of large sinus membrane perforations using stabilized collagen barrier membranes: Surgical techniques with histologic and radiographic evidence of success. Int. J. Periodontics Restor. Dent. 2008, 28, 9–17. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baek, J.-H.; Kim, B.-O.; Lee, W.-P. Implant Placement after Closure of Oroantral Communication by Sinus Bone Graft Using a Collagen Barrier Membrane in the Shape of a Pouch: A Case Report and Review of the Literature. Medicina 2021, 57, 626. https://doi.org/10.3390/medicina57060626
Baek J-H, Kim B-O, Lee W-P. Implant Placement after Closure of Oroantral Communication by Sinus Bone Graft Using a Collagen Barrier Membrane in the Shape of a Pouch: A Case Report and Review of the Literature. Medicina. 2021; 57(6):626. https://doi.org/10.3390/medicina57060626
Chicago/Turabian StyleBaek, Jae-Ha, Byung-Ock Kim, and Won-Pyo Lee. 2021. "Implant Placement after Closure of Oroantral Communication by Sinus Bone Graft Using a Collagen Barrier Membrane in the Shape of a Pouch: A Case Report and Review of the Literature" Medicina 57, no. 6: 626. https://doi.org/10.3390/medicina57060626
APA StyleBaek, J.-H., Kim, B.-O., & Lee, W.-P. (2021). Implant Placement after Closure of Oroantral Communication by Sinus Bone Graft Using a Collagen Barrier Membrane in the Shape of a Pouch: A Case Report and Review of the Literature. Medicina, 57(6), 626. https://doi.org/10.3390/medicina57060626






