Subclinical Changes in Cardiac Functional Parameters as Determined by Cardiovascular Magnetic Resonance (CMR) Imaging in Sleep Apnea and Snoring: Findings from UK Biobank
Abstract
1. Introduction
2. Materials and Methods
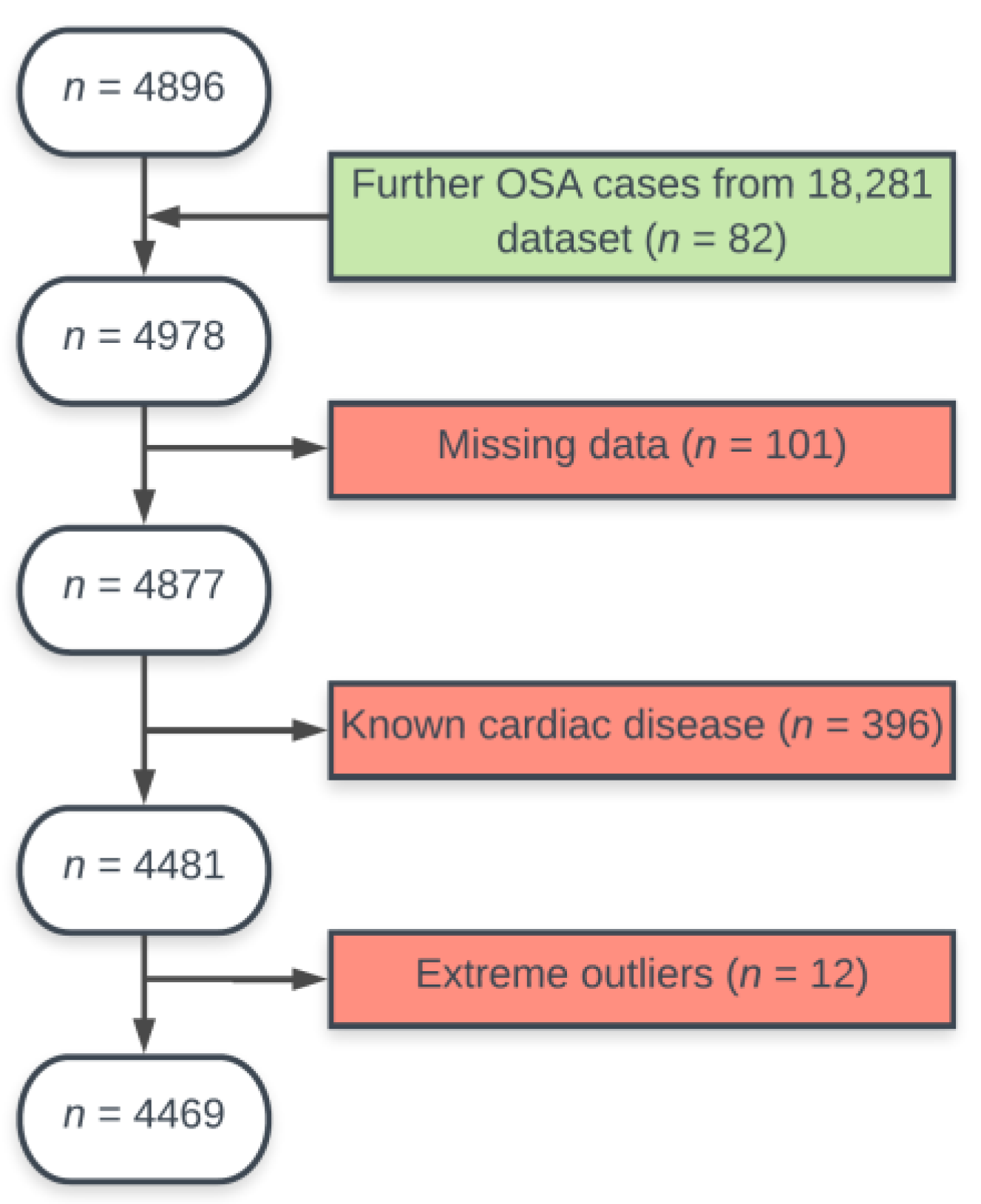
2.1. Study Sample
2.2. Assessment of OSA and Snoring
2.3. CMR Imaging and Evaluation
2.4. Covariates
2.5. Statistical Analysis
3. Results
3.1. Study Population
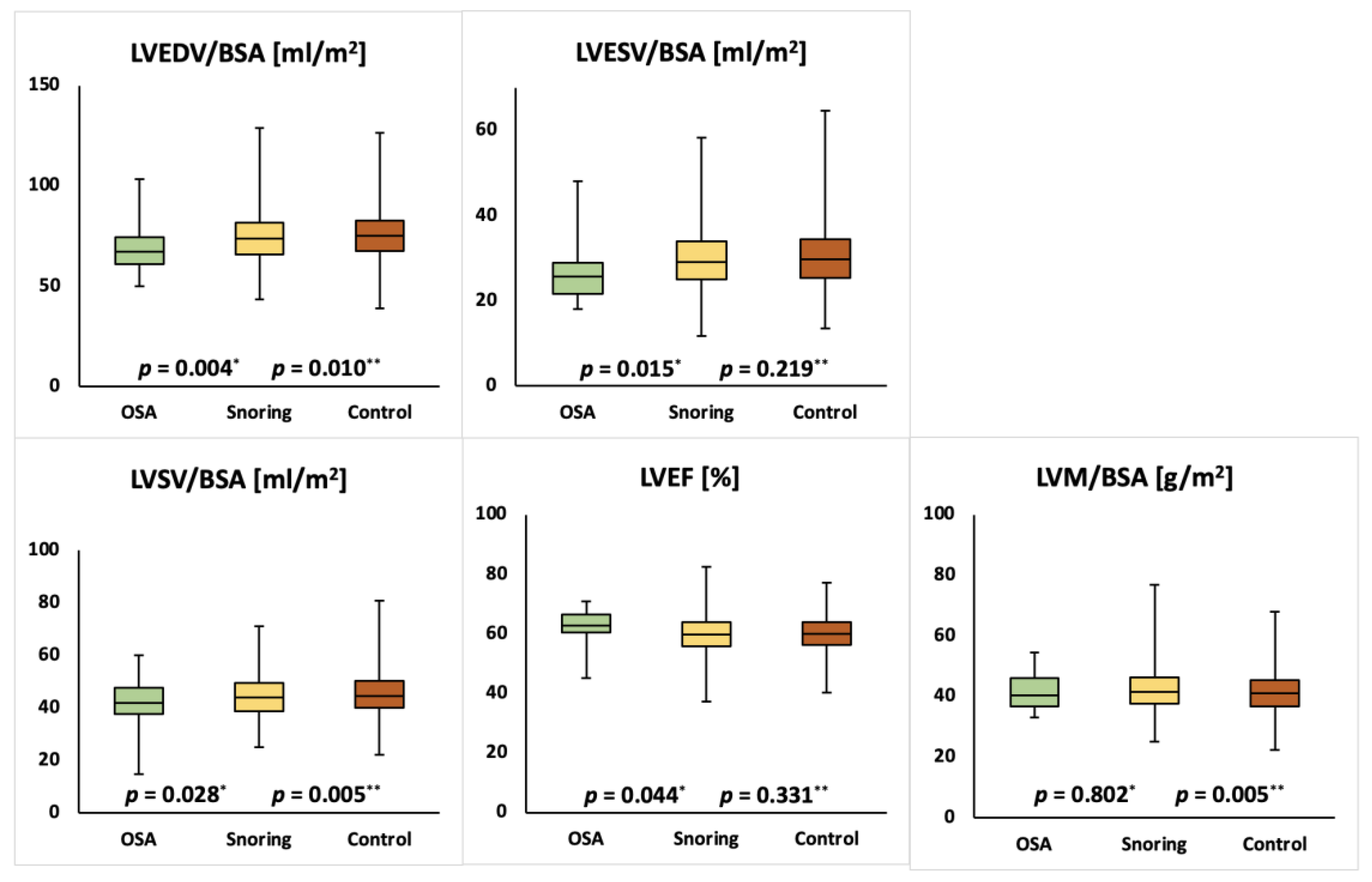
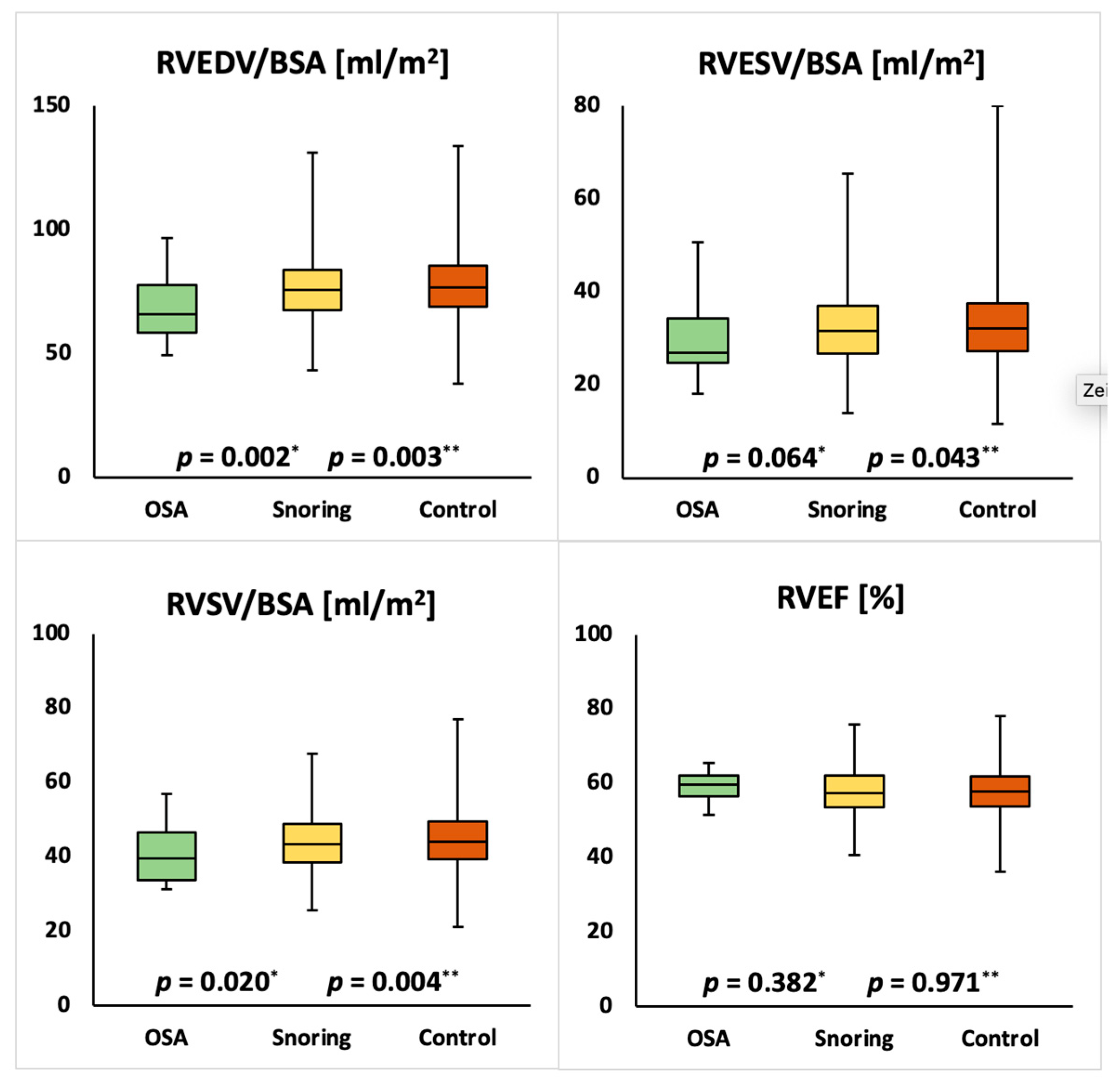
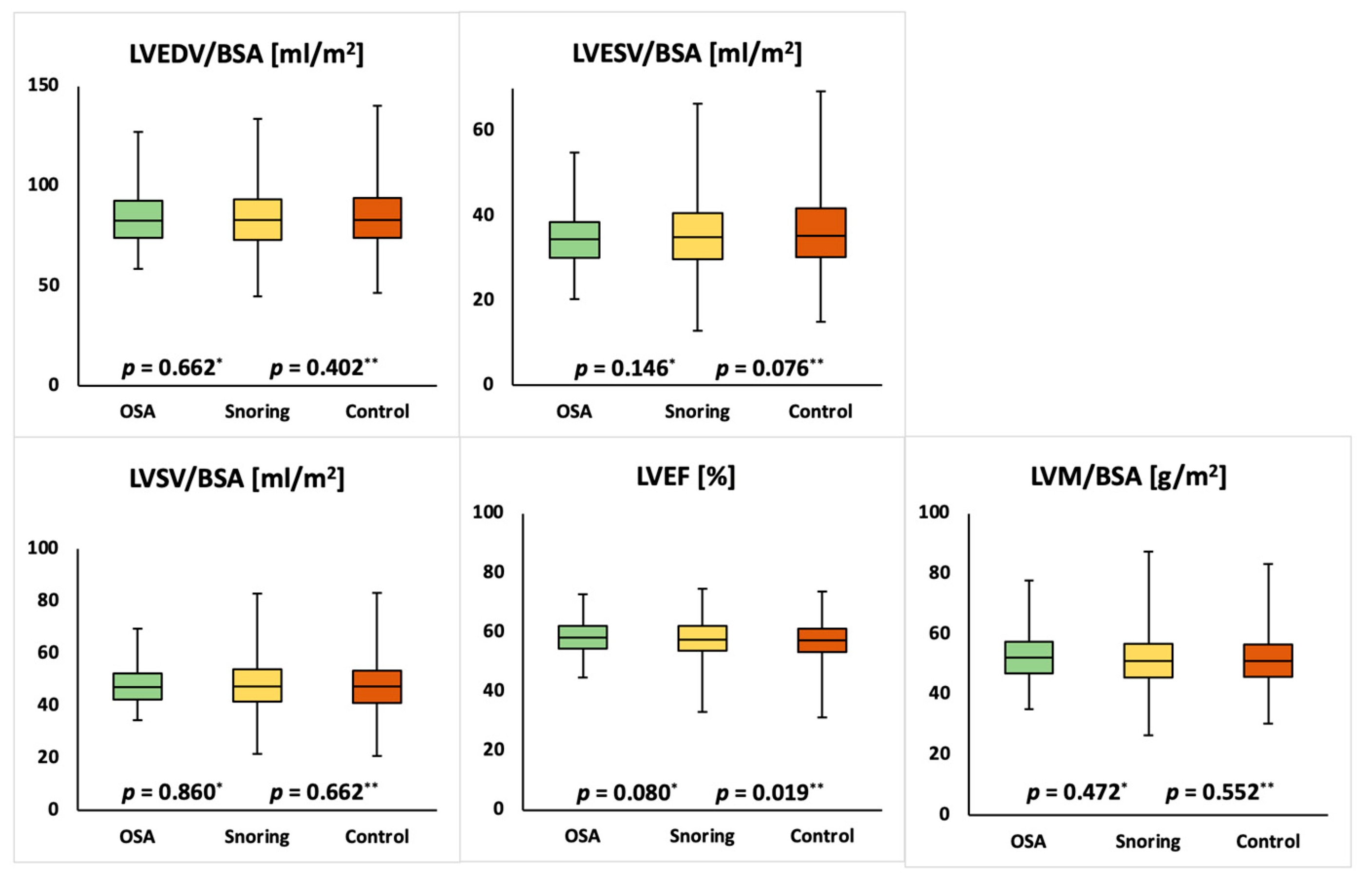
3.2. Left and Right Ventricular Parameters
3.3. Regression Analysis
4. Discussion
4.1. Limitations
4.2. Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Peppard, P.E.; Young, T.; Barnet, J.H.; Palta, M.; Hagen, E.W.; Hla, K.M. Increased Prevalence of Sleep-Disordered Breathing in Adults. Am. J. Epidemiol. 2013, 177, 1006–1014. [Google Scholar] [CrossRef]
- Benjafield, A.V.; Ayas, N.T.; Eastwood, P.R.; Heinzer, R.; Ip, M.S.; Morrell, M.J.; Nunez, C.M.; Patel, S.R.; Penzel, T.; Pépin, J.-L.; et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: A literature-based analysis. Lancet. Respir. Med. 2019, 7. [Google Scholar] [CrossRef]
- Mansukhani, M.P.; Wang, S.; Somers, V.K. Sleep, death, and the heart. Am. J. Physiol. Heart Circ. Physiol. 2015, 309, H739–H749. [Google Scholar] [CrossRef]
- Bliwise, D.L.; Nekich, J.C.; Dement, W.C. Relative validity of self-reported snoring as a symptom of sleep apnea in a sleep clinic population. Chest 1991, 99, 600–608. [Google Scholar] [CrossRef]
- Mansukhani, M.P.; Kara, T.; Caples, S.M.; Somers, V.K. Chemoreflexes, sleep apnea, and sympathetic dysregulation. Curr. Hypertens. Rep. 2014, 16, 476. [Google Scholar] [CrossRef] [PubMed]
- Gottlieb, D.J.; Yenokyan, G.; Newman, A.B.; O’Connor, G.T.; Punjabi, N.M.; Quan, S.F.; Redline, S.; Resnick, H.E.; Tong, E.K.; Diener-West, M.; et al. Prospective Study of Obstructive Sleep Apnea and Incident Coronary Heart Disease and Heart Failure. Circulation 2010, 122, 352–360. [Google Scholar] [CrossRef]
- Roca, G.Q.; Redline, S.; Claggett, B.; Bello, N.; Ballantyne, C.M.; Solomon, S.D.; Shah, A.M. Sex-Specific Association of Sleep Apnea Severity With Subclinical Myocardial Injury, Ventricular Hypertrophy, and Heart Failure Risk in a Community-Dwelling Cohort. Circulation 2015, 132, 1329–1337. [Google Scholar] [CrossRef]
- Drager, L.F.; Bortolotto, L.A.; Pedrosa, R.P.; Krieger, E.M.; Lorenzi-Filho, G. Left atrial diameter is independently associated with arterial stiffness in patients with obstructive sleep apnea: Potential implications for atrial fibrillation. Int. J. Cardiol. 2010, 144, 257–259. [Google Scholar] [CrossRef] [PubMed]
- Guilleminault, C.; Connolly, S.J.; Winkle, R.A. Cardiac arrhythmia and conduction disturbances during sleep in 400 patients with sleep apnea syndrome. Am. J. Cardiol. 1983, 52, 490–494. [Google Scholar] [CrossRef]
- Palomaki, H.; Partinen, M.; Erkinjuntti, T.; Kaste, M. Snoring, sleep apnea syndrome, and stroke. Neurology 1992, 42, 75–81. [Google Scholar] [PubMed]
- Parish, J.M.; Somers, V.K. Obstructive sleep apnea and cardiovascular disease. Mayo Clin. Proc. 2004, 79, 1036–1046. [Google Scholar] [CrossRef]
- Sanner, B.M.; Doberauer, C.; Konermann, M.; Sturm, A.; Zidek, W. Pulmonary hypertension in patients with obstructive sleep apnea syndrome. Arch. Intern. Med. 1997, 157, 2483–2487. [Google Scholar] [CrossRef] [PubMed]
- Sajkov, D.; McEvoy, R.D. Obstructive sleep apnea and pulmonary hypertension. Prog. Cardiovasc. Dis. 2009, 51, 363–370. [Google Scholar] [CrossRef] [PubMed]
- Sallach, S.M.; Peshock, R.M.; Reimold, S. Noninvasive cardiac imaging in pulmonary hypertension. Cardiol. Rev. 2007, 15, 97–101. [Google Scholar] [CrossRef]
- Sudlow, C.; Gallacher, J.; Allen, N.; Beral, V.; Burton, P.; Danesh, J.; Downey, P.; Elliott, P.; Green, J.; Landray, M.; et al. UK biobank: An open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med 2015, 12, e1001779. [Google Scholar] [CrossRef]
- Petersen, S.E.; Matthews, P.M.; Francis, J.M.; Robson, M.D.; Zemrak, F.; Boubertakh, R.; Young, A.A.; Hudson, S.; Weale, P.; Garratt, S.; et al. UK Biobank’s cardiovascular magnetic resonance protocol. J. Cardiovasc. Magn. Reson. 2016, 18, 8. [Google Scholar] [CrossRef]
- Petersen, S.E.; Aung, N.; Sanghvi, M.M.; Zemrak, F.; Fung, K.; Paiva, J.M.; Francis, J.M.; Khanji, M.Y.; Lukaschuk, E.; Lee, A.M.; et al. Reference ranges for cardiac structure and function using cardiovascular magnetic resonance (CMR) in Caucasians from the UK Biobank population cohort. J. Cardiovasc. Magn. Reson. 2017, 19, 18. [Google Scholar] [CrossRef] [PubMed]
- Sin, D.D.; Fitzgerald, F.; Parker, J.D.; Newton, G.; Floras, J.S.; Bradley, T.D. Risk factors for central and obstructive sleep apnea in 450 men and women with congestive heart failure. Am. J. Respir. Crit. Care Med. 1999, 160, 1101–1106. [Google Scholar] [CrossRef]
- Oldenburg, O.; Lamp, B.; Faber, L.; Teschler, H.; Horstkotte, D.; Topfer, V. Sleep-disordered breathing in patients with symptomatic heart failure: A contemporary study of prevalence in and characteristics of 700 patients. Eur. J. Heart Fail. 2007, 9, 251–257. [Google Scholar] [CrossRef]
- Lee, C.H.; Khoo, S.M.; Tai, B.C.; Chong, E.Y.; Lau, C.; Than, Y.; Shi, D.X.; Lee, L.C.; Kailasam, A.; Low, A.F.; et al. Obstructive sleep apnea in patients admitted for acute myocardial infarction. Prevalence, predictors, and effect on microvascular perfusion. Chest 2009, 135, 1488–1495. [Google Scholar] [CrossRef]
- Dursunoglu, N.; Dursunoglu, D.; Kilic, M. Impact of obstructive sleep apnea on right ventricular global function: Sleep apnea and myocardial performance index. Respir. Int. Rev. Thorac. Dis. 2005, 72, 278–284. [Google Scholar] [CrossRef]
- Park, J.G.; Ramar, K.; Olson, E.J. Updates on definition, consequences, and management of obstructive sleep apnea. Mayo Clin. Proc. 2011, 86, 549–554. [Google Scholar] [CrossRef]
- Farre, N.; Otero, J.; Falcones, B.; Torres, M.; Jorba, I.; Gozal, D.; Almendros, I.; Farre, R.; Navajas, D. Intermittent Hypoxia Mimicking Sleep Apnea Increases Passive Stiffness of Myocardial Extracellular Matrix. A Multiscale Study. Front. Physiol. 2018, 9, 1143. [Google Scholar] [CrossRef] [PubMed]
- Laaban, J.P.; Pascal-Sebaoun, S.; Bloch, E.; Orvoen-Frija, E.; Oppert, J.M.; Huchon, G. Left ventricular systolic dysfunction in patients with obstructive sleep apnea syndrome. Chest 2002, 122, 1133–1138. [Google Scholar] [CrossRef] [PubMed]
- Heinzel, F.R.; Hohendanner, F.; Jin, G.; Sedej, S.; Edelmann, F. Myocardial Hypertrophy and Its Role in Heart Failure with Preserved Ejection Fraction. J. Appl. Physiol. 2015, 119, 1233–1242. [Google Scholar] [CrossRef] [PubMed]
- Punjabi, N.M. The epidemiology of adult obstructive sleep apnea. Proc. Am. Thorac. Soc. 2008, 5, 136–143. [Google Scholar] [CrossRef]
- Villaneuva, A.T.; Buchanan, P.R.; Yee, B.J.; Grunstein, R.R. Ethnicity and obstructive sleep apnoea. Sleep Med. Rev. 2005, 9, 419–436. [Google Scholar] [CrossRef]
- Akyol, S.; Cortuk, M.; Baykan, A.O.; Kiraz, K.; Borekci, A.; Seker, T.; Gur, M.; Cayli, M. Biventricular Myocardial Performance Is Impaired in Proportion to Severity of Obstructive Sleep Apnea. Tex. Heart Inst. J. 2016, 43, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Altintas, N.; Aslan, E.; Helvaci, A.; Malhotra, A. Relationship between obstructive sleep apnea severity index and left ventricular function and volume. Ann. Saudi Med. 2012, 32, 384–390. [Google Scholar] [CrossRef] [PubMed]
- Romero-Corral, A.; Somers, V.K.; Pellikka, P.A.; Olson, E.J.; Bailey, K.R.; Korinek, J.; Orban, M.; Sierra-Johnson, J.; Kato, M.; Amin, R.S.; et al. Decreased right and left ventricular myocardial performance in obstructive sleep apnea. Chest 2007, 132, 1863–1870. [Google Scholar] [CrossRef]
- Magalang, U.J.; Richards, K.; McCarthy, B.; Fathala, A.; Khan, M.; Parinandi, N.; Raman, S.V. Continuous positive airway pressure therapy reduces right ventricular volume in patients with obstructive sleep apnea: A cardiovascular magnetic resonance study. J. Clin. Sleep Med. 2009, 5, 110–114. [Google Scholar] [CrossRef] [PubMed]
- Sharma, B.; Neilan, T.G.; Kwong, R.Y.; Mandry, D.; Owens, R.L.; McSharry, D.; Bakker, J.P.; Malhotra, A. Evaluation of Right Ventricular Remodeling Using Cardiac Magnetic Resonance Imaging in Co-Existent Chronic Obstructive Pulmonary Disease and Obstructive Sleep Apnea. COPD 2013, 10, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Javaheri, S.; Sharma, R.K.; Wang, R.; Weng, J.; Rosen, B.D.; Bluemke, D.A.; Lima, J.A.; Redline, S. Association between Obstructive Sleep Apnea and Left Ventricular Structure by Age and Gender: The Multi-Ethnic Study of Atherosclerosis. Sleep 2016, 39, 523–529. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Unaffected (n = 2477) | Snoring (n = 1886) | p-Value * | OSA (n = 118) | p-Value ** |
|---|---|---|---|---|---|
| Female gender | 1153 (62.7%) | 815 (43.2%) | <0.001 | 24 (20.3%) | <0.0001 |
| Age (years) | 55.2 ± 7.7 | 55.1 ± 7.5 | 0.458 | 55.3 ± 7.3 | 0.914 |
| Height (cm) | 169 ± 9 | 171 ± 10 | <0.001 | 174 ± 9 | <0.001 |
| Weight (kg) | 72.6 ± 13.9 | 80.2 ± 15.0 | <0.001 | 93.6 ± 17.0 | <0.001 |
| BMI (kg/m²) | 25.7 ± 4.0 | 27.6 ± 4.3 | <0.001 | 31.3 ± 5.3 | <0.001 |
| Body surface area (m²) | 1.8 ± 0.2 | 1.9 ± 0.2 | <0.001 | 2.1 ± 0.2 | <0.001 |
| Systolic blood pressure (mmHg) | 135 ± 18 | 138 ± 17 | <0.001 | 140 ± 17 | 0.012 |
| Diastolic blood pressure (mmHg) | 78 ± 10 | 80 ± 10 | <0.001 | 80 ± 10 | 0.045 |
| Pulse rate (/s) | 70 ± 11 | 70 ± 11 | 0.038 | 71 ± 12 | 0.081 |
| Smoking Status | |||||
| Current | 95 (3.8%) | 90 (4.8%) | <0.001 | 7 (5.9%) | 0.097 |
| Never | 1570 (63.4%) | 1058 (56.1%) | 64 (54.2%) | ||
| Previous | 783 (31.6%) | 715 (37.9%) | 46 (39.0%) | ||
| Unknown | 29 (1.2%) | 23 (1.2%) | 1 (0.8%) | ||
| Daytime dozing | |||||
| Often | 38 (1.5%) | 55 (2.9%) | <0.001 | 6 (5.1%) | <0.001 |
| Sometimes | 423 (17.1%) | 435 (23.1%) | 39 (33.1%) | ||
| Never/rarely | 1990 (80.3%) | 1377 (73.0%) | 71 (60.2%) | ||
| No answer | 26 (1.0%) | 19 (1.0%) | 2 (1.7%) | ||
| Diabetes mellitus | 89 (3.6%) | 101 (5.4%) | 0.005 | 18 (15.3%) | <0.001 |
| Parameter | Unaffected | Snoring | OSA | ||
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | p-Value * | Mean ± SD | p-Value ** | |
| LVMI (g/m2) | 41.4 ± 6.8 | 42.2 ± 6.8 | 0.005 | 41.7 ± 6.1 | 0.802 |
| LVEDVI (mL/m2) | 75.6 ± 11.7 | 74.3 ± 11.8 | 0.010 | 68.7 ± 11.9 | 0.004 |
| LVESVI (mL/m2) | 30.2 ± 6.9 | 29.9 ± 6.9 | 0.219 | 26.7 ± 7.3 | 0.015 |
| LVEF (%) | 60.2 ± 5.6 | 59.9 ± 5.8 | 0.331 | 62.6 ± 5.1 | 0.044 |
| LVSVI (mL/m2) | 45.4 ± 7.6 | 44.4 ± 7.7 | 0.005 | 41.9 ± 9.9 | 0.028 |
| RVEDVI (mL/m2) | 77.8 ± 12.6 | 76.1 ± 12.3 | 0.003 | 69.5 ± 13.1 | 0.002 |
| RVESVI (mL/m2) | 32.9 ± 8.1 | 32.2 ± 7.8 | 0.043 | 29.9 ± 8.4 | 0.064 |
| RVEF (%) | 57.9 ± 6.0 | 57.9 ± 5.9 | 0.971 | 59.0 ± 4.2 | 0.382 |
| RVSVI (mL/m2) | 44.8 ± 7.5 | 43.9 ± 7.3 | 0.004 | 41.2 ± 7.0 | 0.020 |
| Parameters | Unaffected | Snoring | OSA | ||
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | p-Value * | Mean ± SD | p-Value ** | |
| LVMI (g/m2) | 51.6 ± 8.5 | 51.8 ± 8.8 | 0.552 | 52.2 ± 8.2 | 0.472 |
| LVEDVI (mL/m2) | 84.4 ± 14.9 | 83.8 ± 14.6 | 0.402 | 83.7 ± 13.1 | 0.662 |
| LVESVI (mL/m2) | 36.2 ± 8.7 | 35.5 ± 8.6 | 0.076 | 34.8 ± 7.4 | 0.146 |
| LVEF (%) | 57.2 ± 6.2 | 57.8 ± 6.1 | 0.019 | 58.3 ± 5.3 | 0.080 |
| LVSVI (mL/m2) | 48.1 ± 9.3 | 48.3 ± 9.3 | 0.662 | 48.3 ± 8.0 | 0.860 |
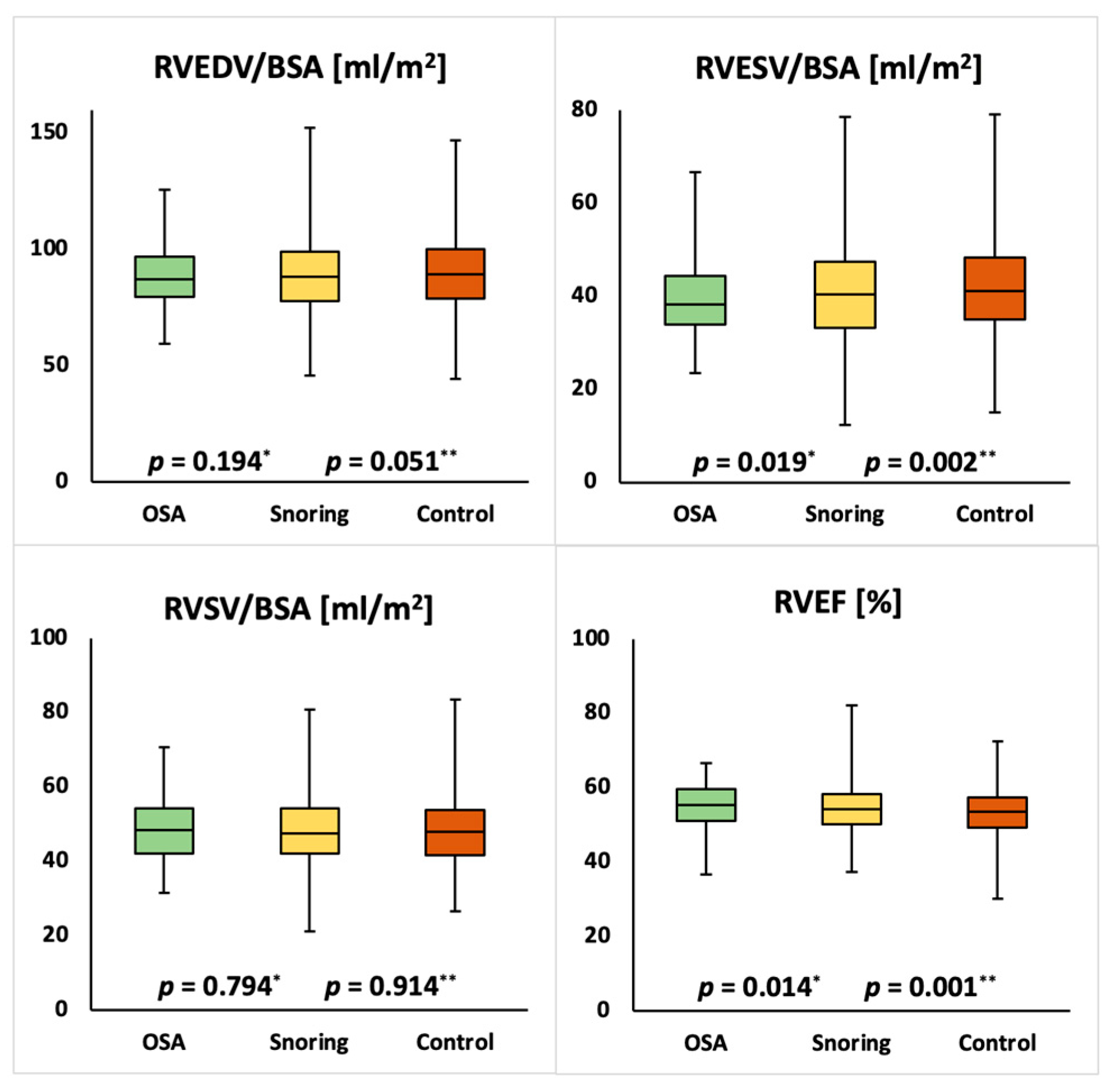
| RVEDVI (mL/m2) | 90.5 ± 15.9 | 89.1 ± 16.0 | 0.051 | 88.3 ± 13.1 | 0.194 |
| RVESVI (mL/m2) | 42.3 ± 10.3 | 40.7 ± 10.0 | 0.002 | 39.7 ± 8.5 | 0.019 |
| RVEF (%) | 53.5 ± 6.1 | 54.5 ± 6.1 | 0.001 | 55.1 ± 5.9 | 0.014 |
| RVSVI (mL/m2) | 48.3 ± 9.1 | 48.4 ± 9.0 | 0.914 | 48.6 ± 8.3 | 0.794 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Curta, A.; Hetterich, H.; Schinner, R.; Lee, A.M.; Sommer, W.; Aung, N.; Sanghvi, M.M.; Fung, K.; Lukaschuk, E.; Cooper, J.A.; et al. Subclinical Changes in Cardiac Functional Parameters as Determined by Cardiovascular Magnetic Resonance (CMR) Imaging in Sleep Apnea and Snoring: Findings from UK Biobank. Medicina 2021, 57, 555. https://doi.org/10.3390/medicina57060555
Curta A, Hetterich H, Schinner R, Lee AM, Sommer W, Aung N, Sanghvi MM, Fung K, Lukaschuk E, Cooper JA, et al. Subclinical Changes in Cardiac Functional Parameters as Determined by Cardiovascular Magnetic Resonance (CMR) Imaging in Sleep Apnea and Snoring: Findings from UK Biobank. Medicina. 2021; 57(6):555. https://doi.org/10.3390/medicina57060555
Chicago/Turabian StyleCurta, Adrian, Holger Hetterich, Regina Schinner, Aaron M. Lee, Wieland Sommer, Nay Aung, Mihir M. Sanghvi, Kenneth Fung, Elena Lukaschuk, Jackie A. Cooper, and et al. 2021. "Subclinical Changes in Cardiac Functional Parameters as Determined by Cardiovascular Magnetic Resonance (CMR) Imaging in Sleep Apnea and Snoring: Findings from UK Biobank" Medicina 57, no. 6: 555. https://doi.org/10.3390/medicina57060555
APA StyleCurta, A., Hetterich, H., Schinner, R., Lee, A. M., Sommer, W., Aung, N., Sanghvi, M. M., Fung, K., Lukaschuk, E., Cooper, J. A., Paiva, J. M., Carapella, V., Neubauer, S., Piechnik, S. K., & Petersen, S. E. (2021). Subclinical Changes in Cardiac Functional Parameters as Determined by Cardiovascular Magnetic Resonance (CMR) Imaging in Sleep Apnea and Snoring: Findings from UK Biobank. Medicina, 57(6), 555. https://doi.org/10.3390/medicina57060555






