Age-Dependent Patient and Trauma Characteristics and Hospital Resource Requirements—Can Improvement Be Made? An Analysis from the German Trauma Registry
Abstract
:1. Introduction
2. Materials and Methods
2.1. The TraumaRegister DGU®
2.2. Statistical Analysis
3. Results
3.1. Patient Characterisitics
3.1.1. Sex Distribution
3.1.2. Preexisting Conditions
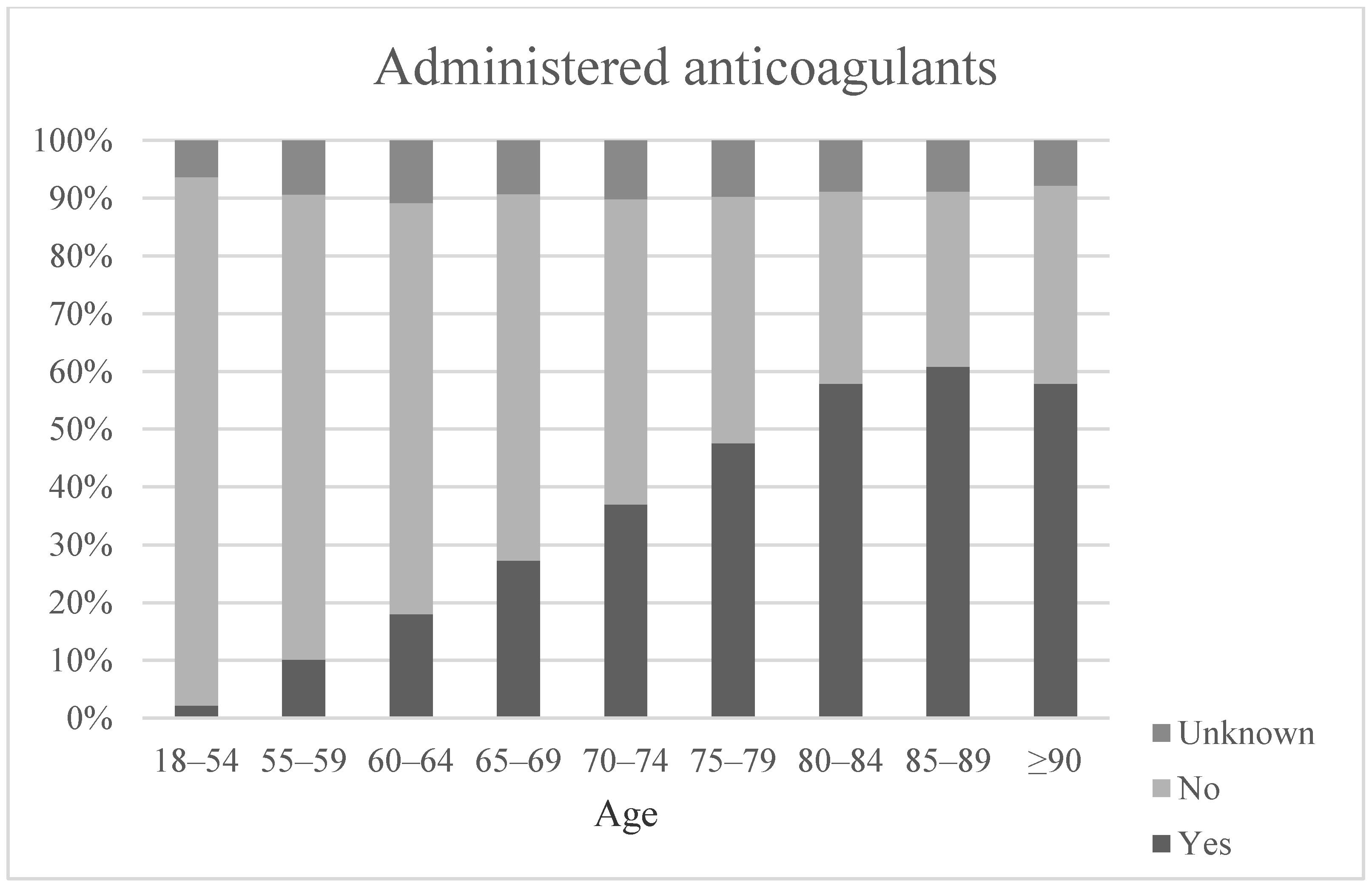
3.2. Trauma Characteristics
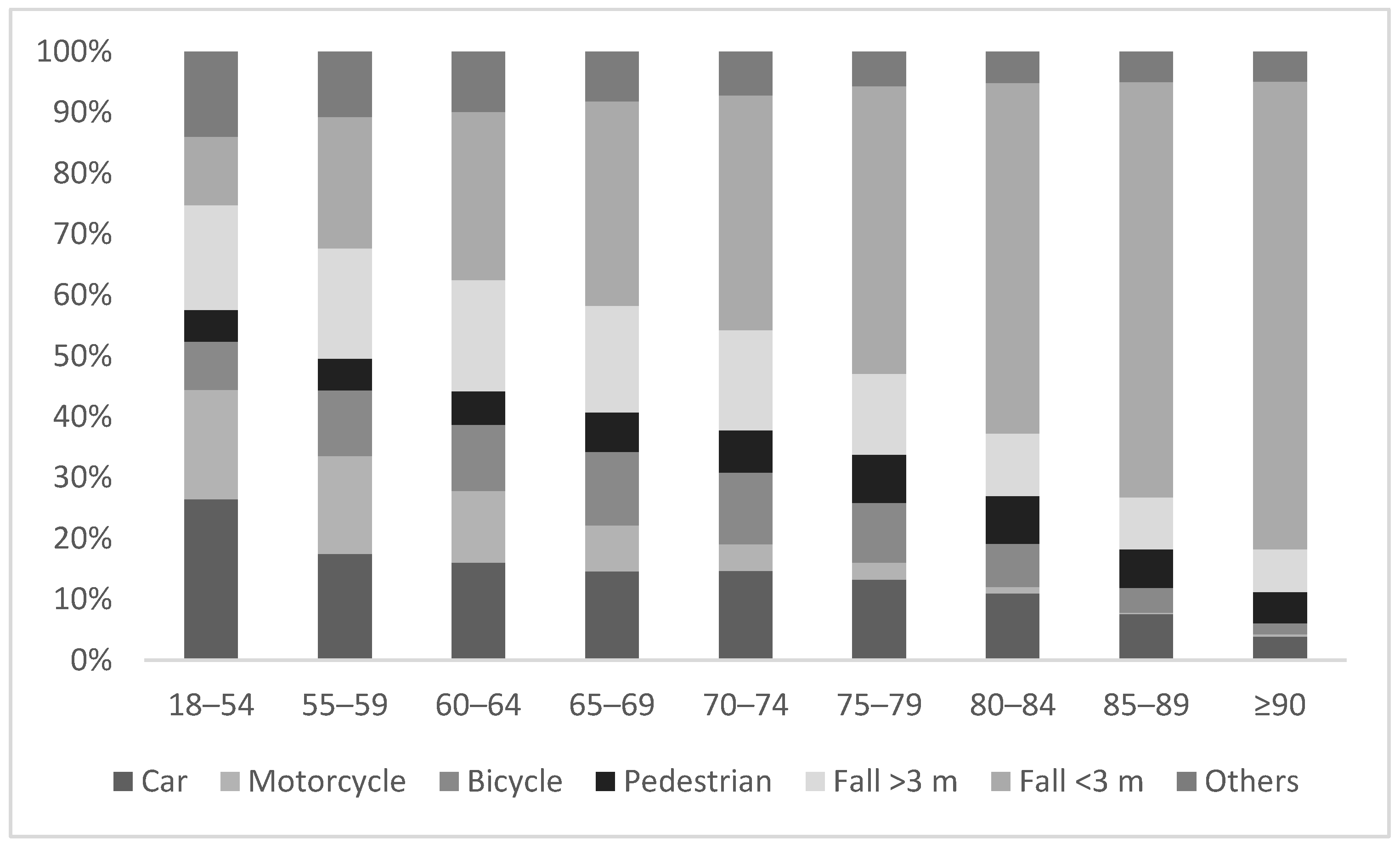
3.2.1. Trauma Mechanism
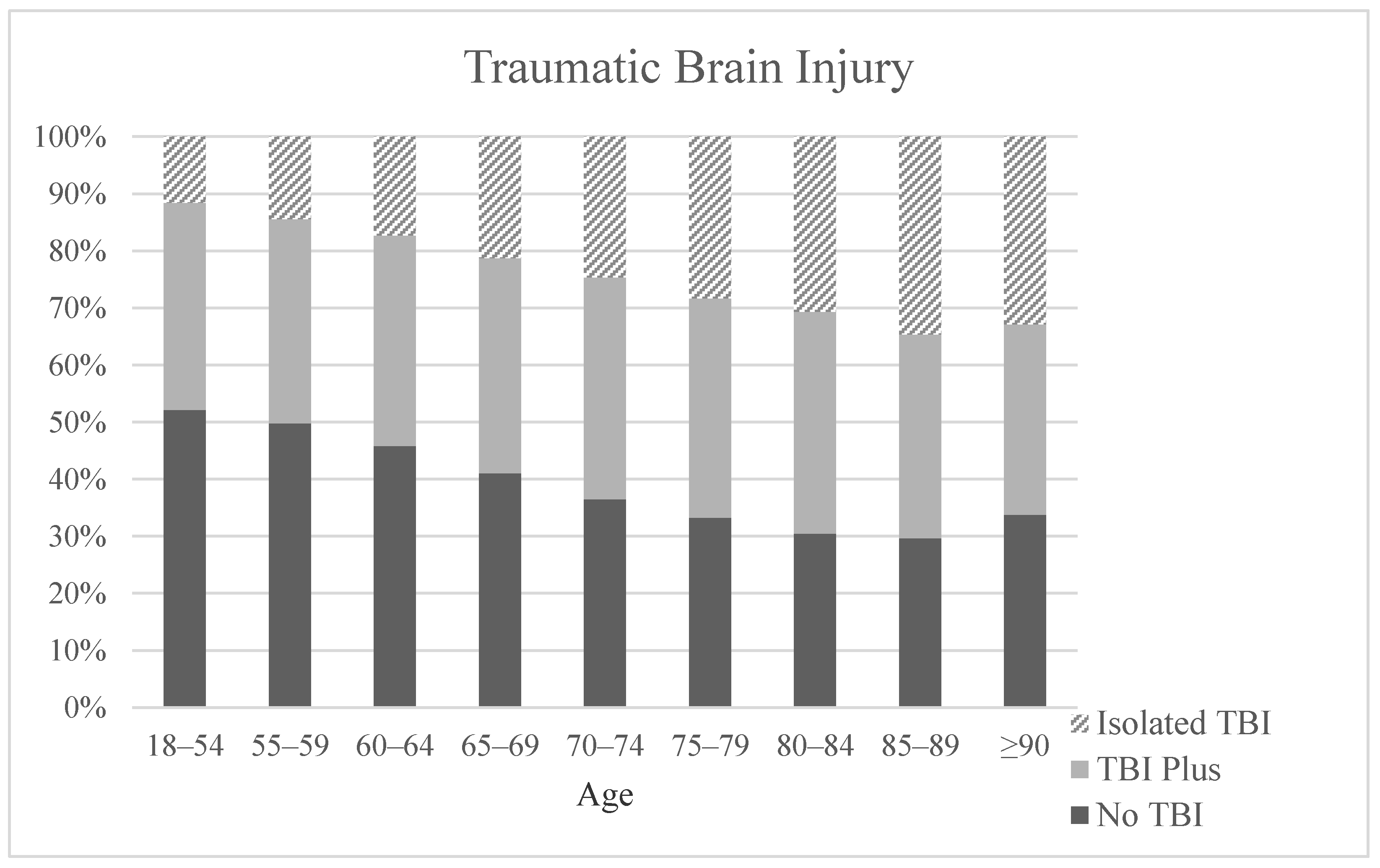
3.2.2. Injury Pattern
3.3. Allocation and Patients Triage
Admission
3.4. Diagnostics
3.5. Outcome
3.5.1. Length of Hospital Stay
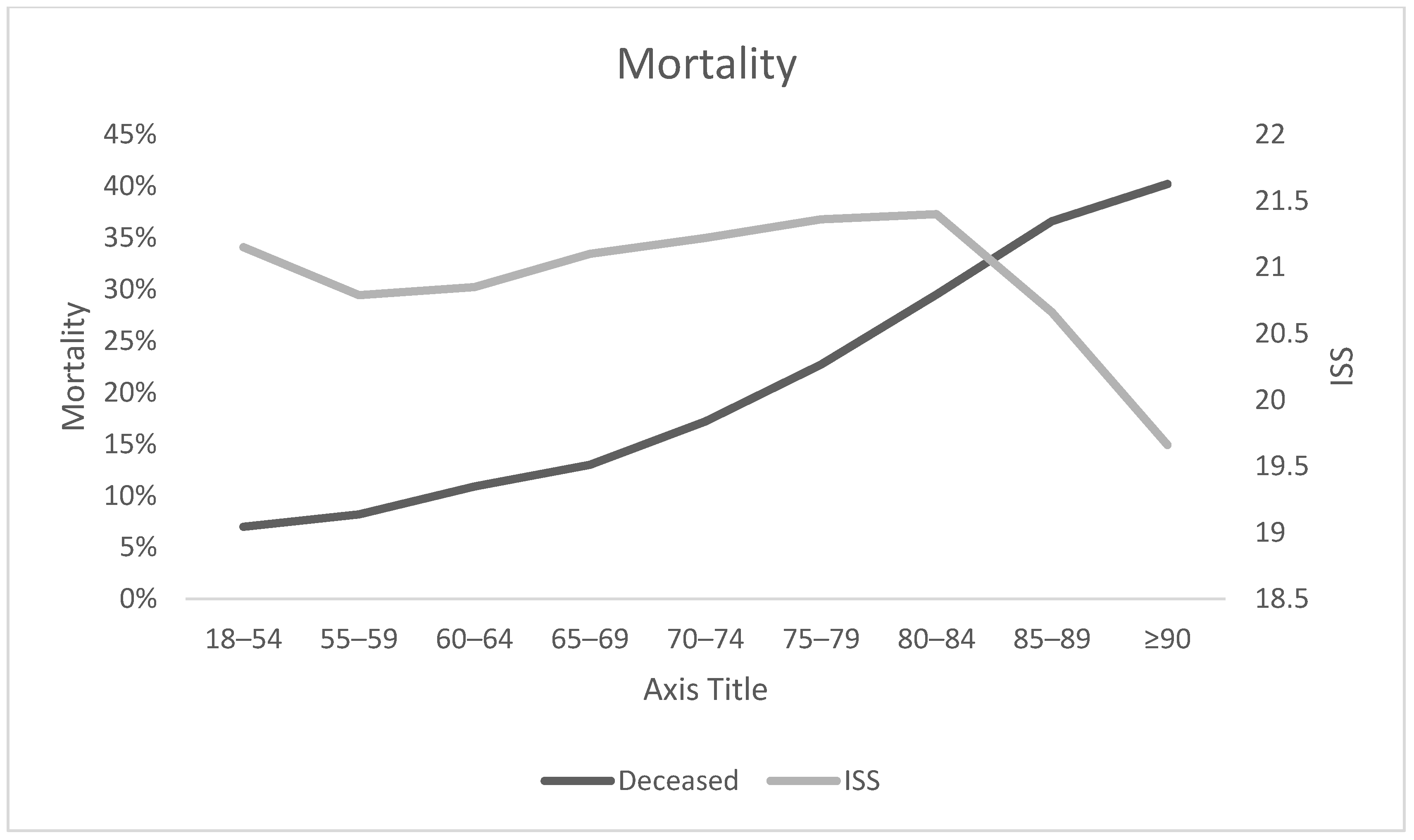
3.5.2. Mortality
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fuster, V. Changing Demographics: A New Approach to Global Health Care Due to the Aging Population. J. Am. Coll. Cardiol. 2017, 69, 3002–3005. [Google Scholar] [CrossRef]
- Statistisches Bundesamt Wiesbaden. Bevölkerung im Wandel; Statistisches Bundesamt Wiesbaden: Wiesbaden, Germany, 2019.
- Haustein, T.; Mischke, J.; Schönfeld, F.; Willand, I.; Theis, K. Older People in Germany and the EU; Federal Statistical Office: Wiesbaden, Germany, 2015.
- World Health Organization. Ageing and Health. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 16 September 2020).
- Wutzler, S.; Lefering, R.; Laurer, H.L.; Walcher, F.; Wyen, H.; Marzi, I. Veränderungen in der alterstraumatologie: Eine analyse an 14.869 patienten aus dem Deutschen Traumaregister. Unfallchirurg 2008, 111, 592–598. [Google Scholar] [CrossRef]
- Hildebrand, F.; Pape, H.-C.; Horst, K.; Andruszkow, H.; Kobbe, P.; Simon, T.-P.; Marx, G.; Schürholz, T. Impact of age on the clinical outcomes of major trauma. Eur. J. Trauma Emerg. Surg. 2016, 42, 317–332. [Google Scholar] [CrossRef] [PubMed]
- Brown, C.V.; Rix, K.; Klein, A.L.; Ford, B.; Teixeira, P.G.; Aydelotte, J.; Coopwood, B.; Ali, S. A comprehensive investigation of comorbidities, mechanisms, injury patterns, and outcomes in geriatric blunt trauma patients. Am. Surg. 2016, 82, 1055–1062. [Google Scholar] [CrossRef] [PubMed]
- Kocuvan, S.; Brilej, D.; Stropnik, D.; Lefering, R.; Komadina, R. Evaluation of major trauma in elderly patients—A single trauma center analysis. Wien. Klin. Wochenschr. 2016, 128, 535–542. [Google Scholar] [CrossRef]
- Van der Sluis, C.K.; Klasen, H.J.; Eisma, W.H.; Duis, H.J.T. Major Trauma in Young and Old: What Is the Difference? J. Trauma Acute Care Surg. 1996, 40, 78–82. [Google Scholar] [CrossRef] [PubMed]
- Spering, C.; Lefering, R.; Bouillon, B.; Lehmann, W.; Von Eckardstein, K.; Dresing, K.; Sehmisch, S. It is time for a change in the management of elderly severely injured patients! An analysis of 126,015 patients from the TraumaRegister DGU®. Eur. J. Trauma Emerg. Surg. 2019, 46, 487–497. [Google Scholar] [CrossRef] [PubMed]
- Mende, A.; Riegel, A.-K.; Plümer, L.; Olotu, C.; Goetz, A.E.; Kiefmann, R. The determinants of perioperative outcome in frail older patients. Dtsch. Arztebl. Int. 2019, 116, 73–83. [Google Scholar] [CrossRef]
- Chen, C.-L.; Chen, C.-M.; Wang, C.-Y.; Ko, P.-W.; Chen, C.-H.; Hsieh, C.-P.; Chiu, H.-C. Frailty is Associated with an Increased Risk of Major Adverse Outcomes in Elderly Patients Following Surgical Treatment of Hip Fracture. Sci. Rep. 2019, 9, 19135. [Google Scholar] [CrossRef] [Green Version]
- Shamliyan, T.; Talley, K.M.C.; Ramakrishnan, R.; Kane, R.L. Association of frailty with survival: A systematic literature review. Ageing Res. Rev. 2013, 12, 719–736. [Google Scholar] [CrossRef]
- Sterling, D.A.; O’Connor, J.A.; Bonadies, J. Geriatric Falls: Injury Severity Is High and Disproportionate to Mechanism. J. Trauma Acute Care Surg. 2001, 50, 116–119. [Google Scholar] [CrossRef]
- Clegg, A.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in elderly people. Lancet 2013, 381, 752–762. [Google Scholar] [CrossRef] [Green Version]
- Peck, K.A.; Calvo, R.Y.; Schechter, M.S.; Sise, C.B.; Kahl, J.E.; Shackford, M.C.; Shackford, S.R.; Sise, M.J.; Blaskiewicz, D.J. The impact of preinjury anticoagulants and prescription antiplatelet agents on outcomes in older patients with traumatic brain injury. J. Trauma Acute Care Surg. 2014, 76, 431–436. [Google Scholar] [CrossRef]
- Peterer, L.; Ossendorf, C.; Jensen, K.O.; Osterhoff, G.; Mica, L.; Seifert, B.; Werner, C.M.L.; Simmen, H.-P.; Pape, H.-C.; Sprengel, K. Implementation of new standard operating procedures for geriatric trauma patients with multiple injuries: A single level I trauma centre study. BMC Geriatr. 2019, 19, 359. [Google Scholar] [CrossRef] [PubMed]
- Demetriades, D.; Sava, J.; Alo, K.; Newton, E.; Velmahos, G.C.; Murray, J.A.; Belzberg, H.; Asensio, J.A.; Berne, T.V. Old age as a criterion for trauma team activation. J. Trauma Inj. Infect. Crit. Care 2001, 51, 754–756. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.E.; Peetz, A.B. Evidence-Based Care of Geriatric Trauma Patients. Surg. Clin. 2017, 97, 1157–1174. [Google Scholar] [CrossRef] [PubMed]
- Deutsche Gesellschaft für Orthopädie und Unfallchirurgie; Traumaregister DGU®. 2020. Available online: www.traumaregister-dgu.de (accessed on 1 October 2020).
- Gennarelli, T.A.; Wodzin, E. Abbreviated Injury Scale 2005: Update 2008; Russ Reeder: Redwood City, CA, USA, 2008. [Google Scholar]
- Daabiss, M. American Society of Anaesthesiologists physical status classification. Indian J. Anaesth. 2011, 55, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Bonne, S.; Schuerer, D.J.E. Trauma in the Older Adult: Epidemiology and Evolving Geriatric Trauma Principles. Clin. Geriatr. Med. 2013, 29, 137–150. [Google Scholar] [CrossRef]
- Con, J.; Friese, R.S.; Long, D.M.; Zangbar, B.; O’Keeffe, T.; Joseph, B.; Rhee, P.; Tang, A.L. Falls from ladders: Age matters more than height. J. Surg. Res. 2014, 191, 262–267. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gardner, R.C.; Dams-O’Connor, K.; Morrissey, M.R.; Manley, G.T. Geriatric Traumatic Brain Injury: Epidemiology, Outcomes, Knowledge Gaps, and Future Directions. J. Neurotrauma 2018, 35, 889–906. [Google Scholar] [CrossRef]
- Liener, U.C.; Becker, C.; Rapp, K. Weißbuch Alterstraumatologie; Deutschen Gesellschaft für Unfallchirurgie: Berlin, Germany, 2018. [Google Scholar]
- Stiell, I.G.; Wells, G.A.; Vandemheen, K.; Clement, C.; Lesiuk, H.; Laupacis, A.; McKnight, R.D.; Verbeek, R.; Brison, R.; Cass, D.; et al. The Canadian CT Head Rule for patients with minor head injury. Lancet 2001, 357, 1391–1396. [Google Scholar] [CrossRef]
- Bass, R.R.; Alcorta, R.L.; Beachley, M.; Chang, D.C. Undertriage of elderly trauma patients to state-designated trauma centers: The authors’ response. Arch. Surg. 2009, 144, 91. [Google Scholar] [CrossRef] [PubMed]
- Zhao, F.Z.; Wolf, S.E.; Nakonezny, P.A.; Minhajuddin, A.; Rhodes, R.L.; Paulk, M.E.; Phelan, H.A. Estimating geriatric mortality after injury using age, injury severity, and performance of a transfusion: The geriatric trauma outcome score. J. Palliat. Med. 2015, 18, 677–681. [Google Scholar] [CrossRef] [PubMed]
- Lefering, R.; Huber-Wagner, S.; Nienaber, U.; Maegele, M.; Bouillon, B. Update of the trauma risk adjustment model of the TraumaRegister DGUTM: The Revised Injury Severity Classification, version II. Crit. Care 2014, 18, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Age Group (Years) | 18–54 | 55–59 | 60–64 | 65–69 | 70–74 | 75–79 | 80–84 | 85–89 | ≥90 | All |
|---|---|---|---|---|---|---|---|---|---|---|
| Male | 77.4% | 75.9% | 75.4% | 71.3% | 65.8% | 60.6% | 54.9% | 45.4% | 32.1% | 70.3% |
| Female | 22.6% | 24.1% | 24.6% | 28.7% | 34.2% | 39.4% | 45.1% | 54.6% | 67.9% | 29.7% |
| Age Groups (Years) | 18–54 | 55–59 | 60–64 | 65–69 | 70–74 | 75–79 | 80–84 | 85–89 | ≥90 | All | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | 55,404 | 9734 | 8419 | 6856 | 8033 | 9830 | 7721 | 5418 | 2754 | 114,169 | |
| Body Regions, AIS ≥ 3 | Head | 37.1% | 38.8% | 43.0% | 48.1% | 53.3% | 57.2% | 60.0% | 62.6% | 58.6% | 44.5% |
| Thorax | 50.1% | 54.2% | 52.0% | 48.7% | 45.6% | 41.0% | 37.4% | 29.9% | 28.2% | 47.1% | |
| Abdomen | 15.5% | 11.4% | 10.0% | 8.9% | 7.0% | 6.2% | 4.8% | 3.5% | 3.1% | 11.4% | |
| Extremities | 33.6% | 27.5% | 25.8% | 23.6% | 21.8% | 21.4% | 22.0% | 24.6% | 28.4% | 28.7% | |
| ISS | 21.15 (11.6) | 20.79 (11.1) | 20.85 (10.7) | 21.10 (10.9) | 21.22 (10.9) | 21.36 (10.9) | 21.40 (11.1) | 20.66 (10.9) | 19.66 (10.6) | 21.07 (11.2) |
| Age Group (Years) | 18–54 | 55–59 | 60–64 | 65–69 | 70–74 | 75–79 | 80–84 | 85–89 | ≥90 |
|---|---|---|---|---|---|---|---|---|---|
| WBCT | 84.5% | 82.1% | 81.7% | 78.7% | 76.1% | 72.6% | 67.8% | 60.6% | 52.5% |
| CCT | 91.8% | 91.6% | 91.8% | 91.9% | 91.5% | 91.5% | 89.9% | 87.1% | 81.7% |
| Age Group | Survivor | Non-Survivor | ||
|---|---|---|---|---|
| n | Median/Mean (SD) | n | Median/Mean (SD) | |
| 18–54 | 47,547 | 14/19.4 (19.2) | 3567 | 2/5.9 (11.8) |
| 55–59 | 8270 | 15/20.3 (20.1) | 734 | 3/7.9 (12.3) |
| 60–64 | 6897 | 15/20.6 (19) | 844 | 3/8.2 (14.1) |
| 65–69 | 5527 | 16/20.7 (18.8) | 825 | 4/8.6 (14.8) |
| 70–74 | 6132 | 16/21.1 (18.6) | 1276 | 4/8.2 (12.5) |
| 75–79 | 6978 | 16/20.5 (17.2) | 2050 | 3/8.5 (12.7) |
| 80–84 | 5051 | 16/19.6 (15.1) | 2112 | 3/8 (11.8) |
| 85–89 | 3213 | 14/17.6 (14.1) | 1854 | 3/7.4 (10.2) |
| ≥90 | 1563 | 12/14.7 (10.4) | 1051 | 3/6.4 (12.2) |
| ALL | 91178 | 15/19.7 (18.6) | 14313 | 3/7.4 (12.2) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ziegenhain, F.; Scherer, J.; Kalbas, Y.; Neuhaus, V.; Lefering, R.; Teuben, M.; Sprengel, K.; Pape, H.-C.; Jensen, K.O.; The TraumaRegister DGU. Age-Dependent Patient and Trauma Characteristics and Hospital Resource Requirements—Can Improvement Be Made? An Analysis from the German Trauma Registry. Medicina 2021, 57, 330. https://doi.org/10.3390/medicina57040330
Ziegenhain F, Scherer J, Kalbas Y, Neuhaus V, Lefering R, Teuben M, Sprengel K, Pape H-C, Jensen KO, The TraumaRegister DGU. Age-Dependent Patient and Trauma Characteristics and Hospital Resource Requirements—Can Improvement Be Made? An Analysis from the German Trauma Registry. Medicina. 2021; 57(4):330. https://doi.org/10.3390/medicina57040330
Chicago/Turabian StyleZiegenhain, Franziska, Julian Scherer, Yannik Kalbas, Valentin Neuhaus, Rolf Lefering, Michel Teuben, Kai Sprengel, Hans-Christoph Pape, Kai Oliver Jensen, and The TraumaRegister DGU. 2021. "Age-Dependent Patient and Trauma Characteristics and Hospital Resource Requirements—Can Improvement Be Made? An Analysis from the German Trauma Registry" Medicina 57, no. 4: 330. https://doi.org/10.3390/medicina57040330
APA StyleZiegenhain, F., Scherer, J., Kalbas, Y., Neuhaus, V., Lefering, R., Teuben, M., Sprengel, K., Pape, H.-C., Jensen, K. O., & The TraumaRegister DGU. (2021). Age-Dependent Patient and Trauma Characteristics and Hospital Resource Requirements—Can Improvement Be Made? An Analysis from the German Trauma Registry. Medicina, 57(4), 330. https://doi.org/10.3390/medicina57040330







