COVID-19 and Pneumocystis jirovecii Pulmonary Coinfection—The First Case Confirmed through Autopsy
Abstract
1. Introduction
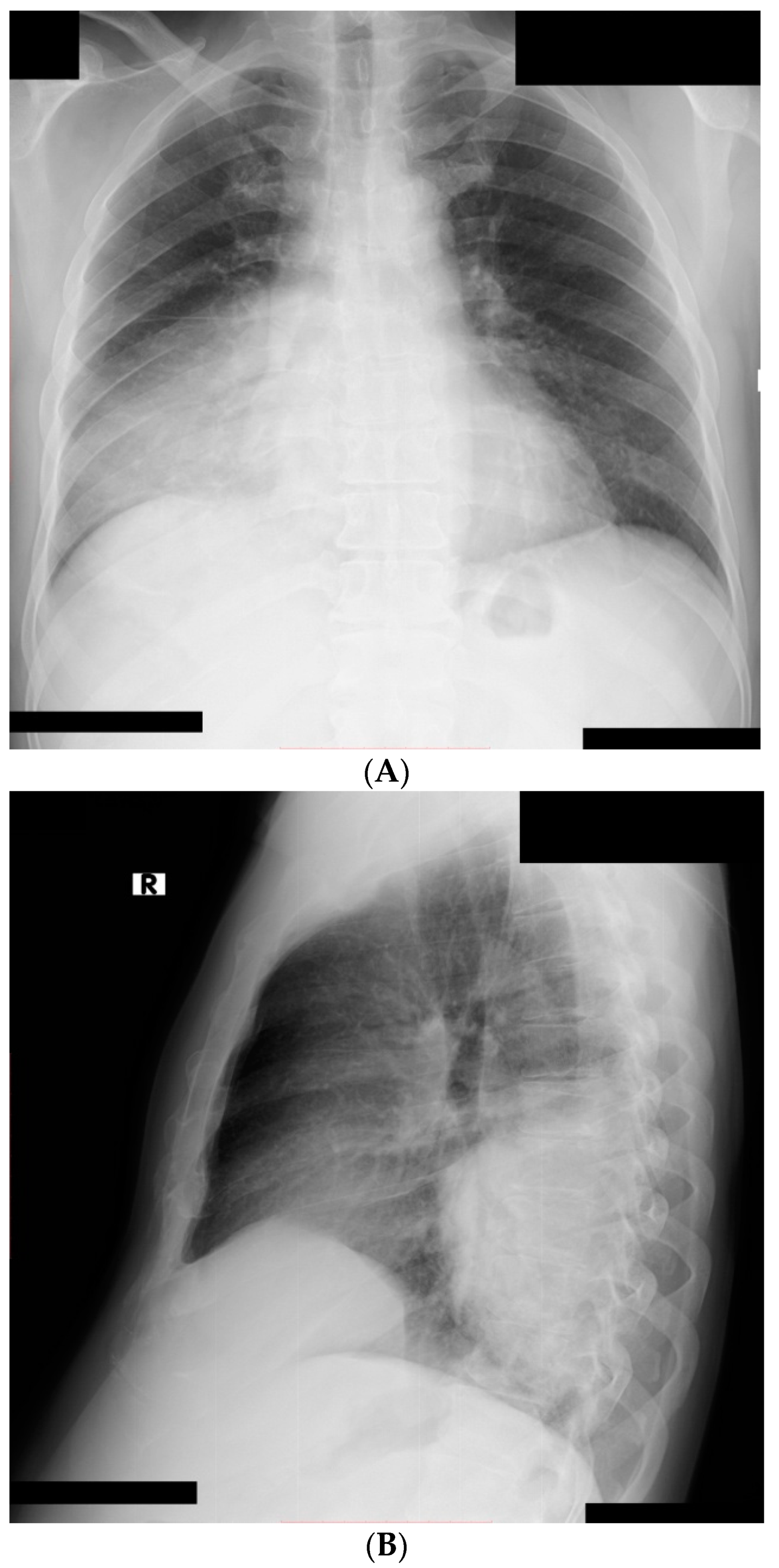
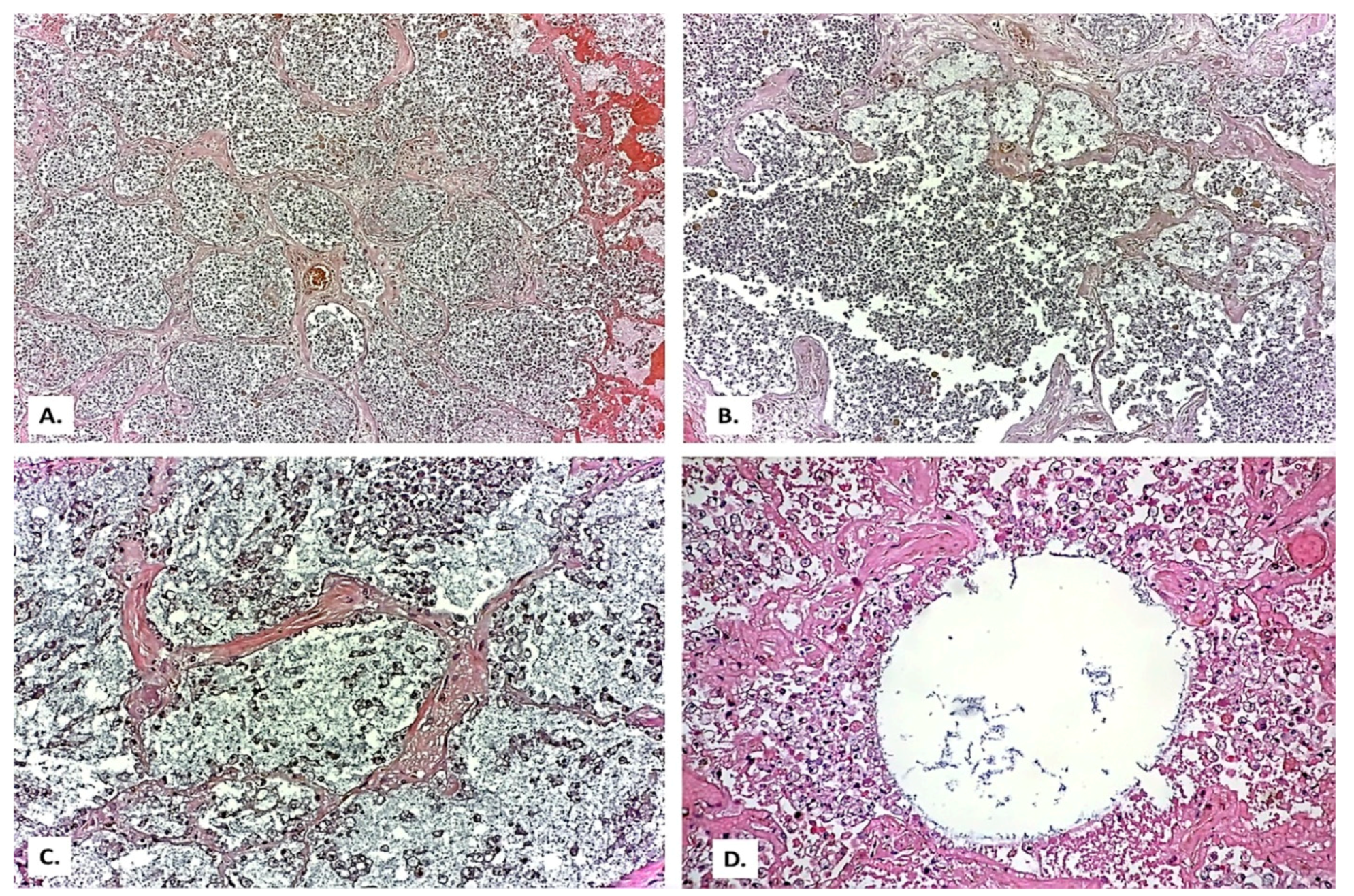
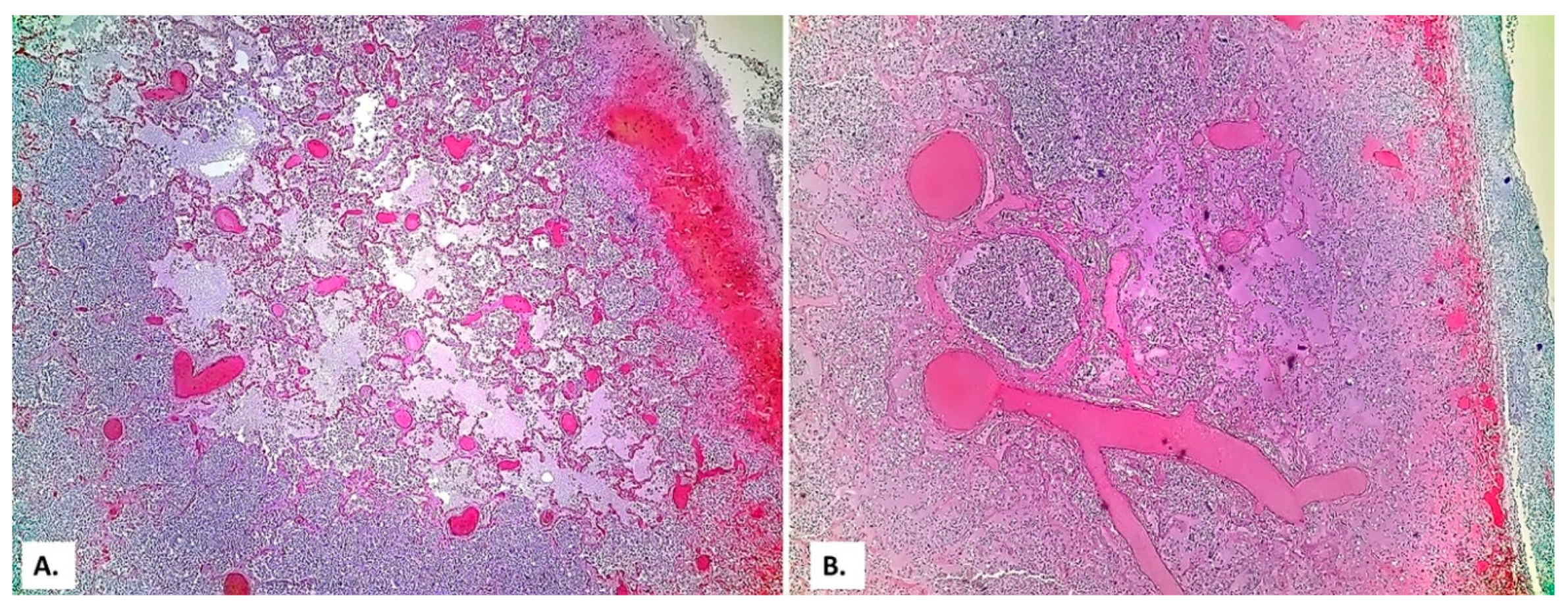
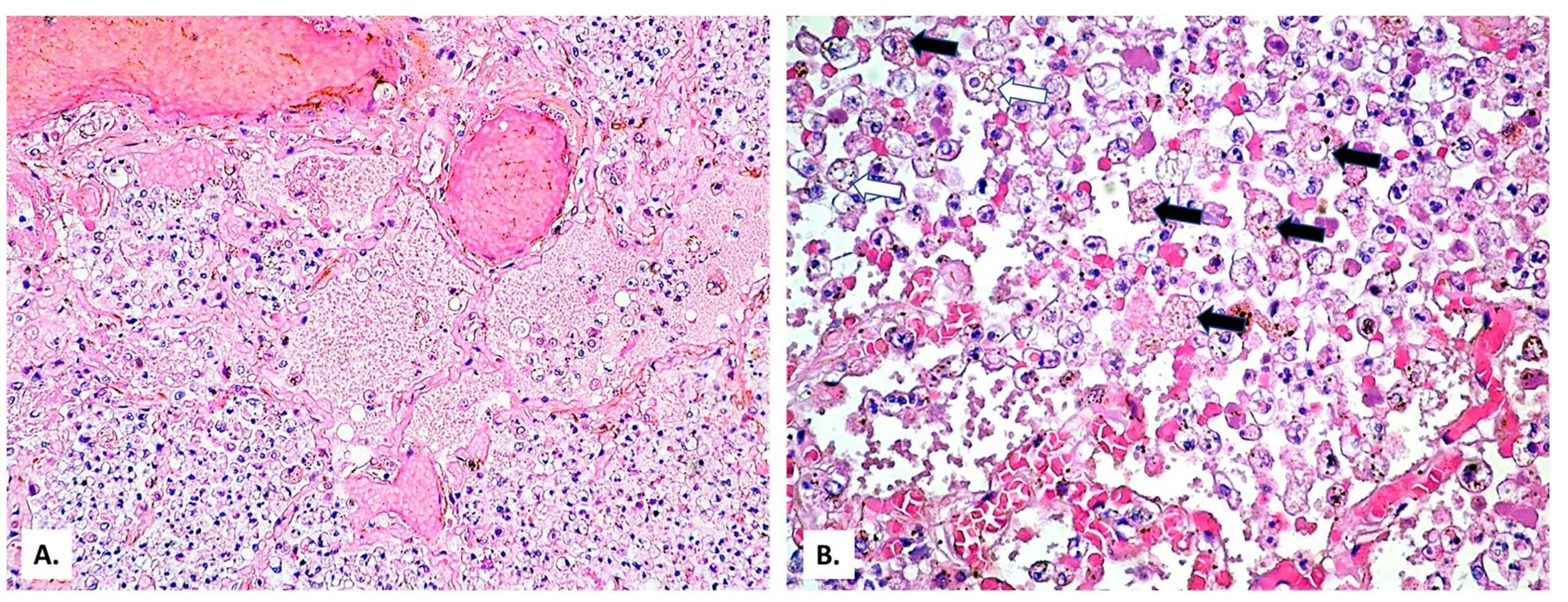
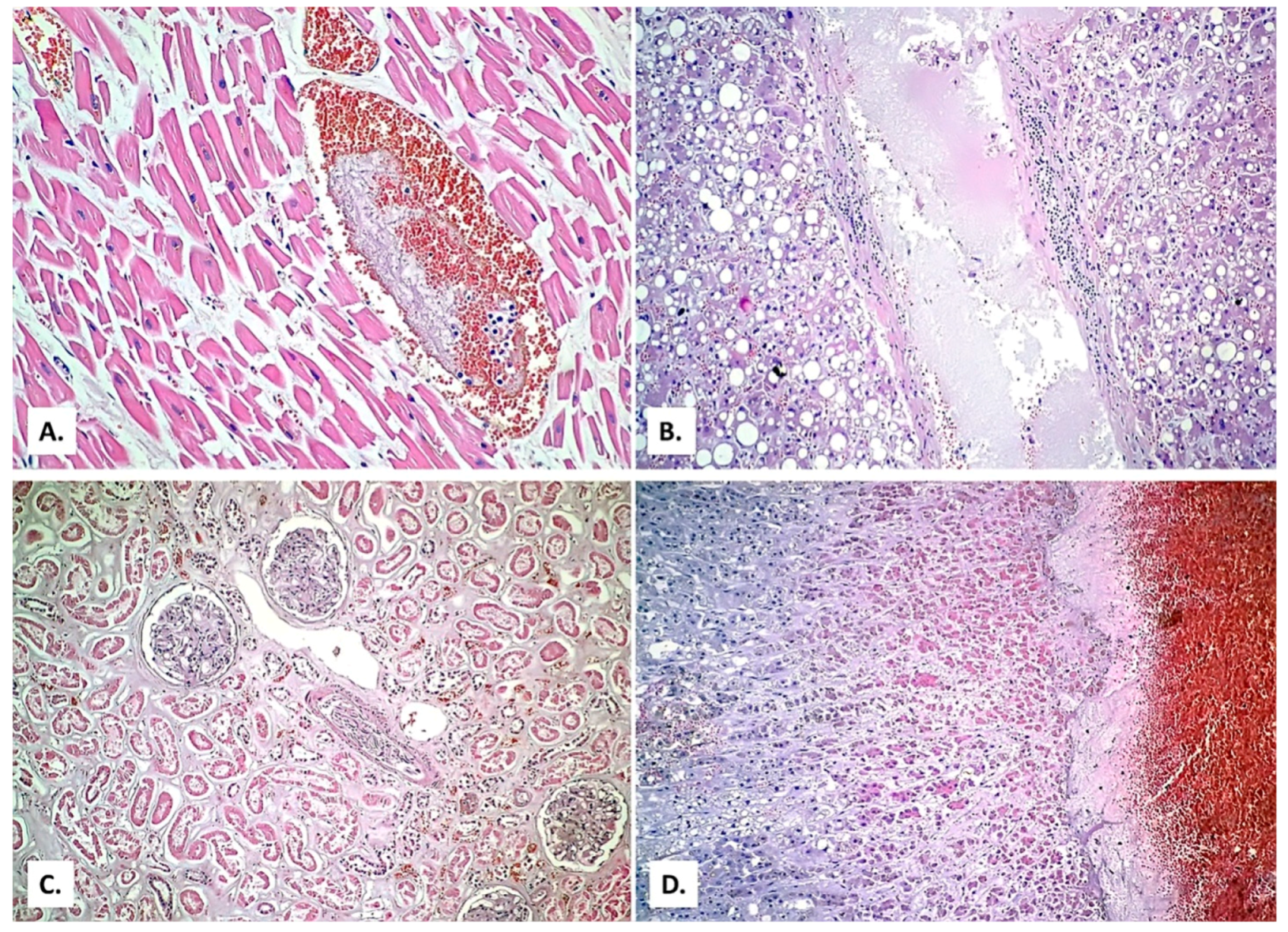
2. Case Presentation
3. Discussions
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jin, M.; Shi, N.; Wang, M.; Shi, C.; Lu, S.; Chang, Q.; Sha, S.; Lin, Y.; Chen, Y.; Zhou, H.; et al. CD45: A critical regulator in immune cells to predict severe and non-severe COVID-19 patients. Aging 2020, 12, 19867–19879. [Google Scholar] [CrossRef]
- Cao, X. COVID-19: Immunopathology and its implications for therapy. Nat. Rev. Immunol. 2020, 20, 269–270. [Google Scholar] [CrossRef]
- Wiersinga, W.J.; Rhodes, A.; Cheng, A.C.; Peacock, S.J.; Prescott, H.C. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review. JAMA 2020, 324, 782–793. [Google Scholar] [CrossRef] [PubMed]
- Bhat, P.; Noval, M.; Doub, J.B.; Heil, E. Concurrent COVID-19 and Pneumocystis jirovecii pneumonia in a severely immunocompromised 25-year-old patient. Int. J. Infect. Dis. 2020, 99, 119–121. [Google Scholar] [CrossRef]
- Messina, F.A.; Marin, E.; Caceres, D.H.; Romero, M.; Depardo, R.; Priarone, M.M.; Rey, L.; Vázquez, M.; Verweij, P.E.; Chiller, T.M.; et al. Coronavirus Disease 2019 (COVID-19) in a Patient with Disseminated Histoplasmosis and HIV—A Case Report from Argentina and Literature Review. J. Fungi 2020, 6, 275. [Google Scholar] [CrossRef]
- Ma, L.; Cissé, O.H.; Kovacs, J.A. A Molecular Window into the Biology and Epidemiology of Pneumocystis spp. Clin. Microbiol. Rev. 2018, 31, e00009-18. [Google Scholar] [CrossRef] [PubMed]
- De Armas Rodríguez, Y.; Wissmann, G.; Müller, A.L.; Pederiva, M.A.; Brum, M.C.; Brackmann, R.L.; Capó de Paz, V.; Calderón, E.J. Pneumocystis jirovecii pneumonia in developing countries. Parasite 2011, 18, 219–228. [Google Scholar] [CrossRef]
- Vargas, S.L.; Hughes, W.T.; Santolaya, M.E.; Ulloa, A.V.; Ponce, C.A.; Cabrera, C.E.; Cumsille, F.; Gigliotti, F. Search for primary infection by Pneumocystis carinii in a cohort of normal, healthy infants. Clin. Infect. Dis. 2001, 32, 855–861. [Google Scholar] [CrossRef] [PubMed]
- Menon, A.A.; Berg, D.D.; Brea, E.J.; Deutsch, A.J.; Kidia, K.K.; Thurber, E.G.; Polsky, S.B.; Yeh, T.; Duskin, J.A.; Holliday, A.M.; et al. A Case of COVID-19 and Pneumocystis jirovecii Coinfection. Am. J. Respir. Crit. Care Med. 2020, 202, 136–138. [Google Scholar] [CrossRef]
- Coleman, H.; Snell, L.B.; Simons, R.; Douthwaite, S.T.; Lee, M.J. Coronavirus disease 2019 and Pneumocystis jirovecii pneumonia: A diagnostic dilemma in HIV. AIDS 2020, 34, 1258–1260. [Google Scholar] [CrossRef]
- Alanio, A.; Dellière, S.; Voicu, S.; Bretagne, S.; Mégarbane, B. The presence of Pneumocystis jirovecii in critically ill patients with COVID-19. J. Infect. 2020, S0163-4453(20)30694-0. [Google Scholar] [CrossRef]
- Choy, C.Y.; Wong, C.S. It’s not all about COVID-19: Pneumocystis pneumonia in the era of a respiratory outbreak. J. Int. AIDS Soc. 2020, 23, e25533. [Google Scholar] [CrossRef]
- Hughes, W.T. Pneumocystis Carinii. In Medical Microbiology, 4th ed.; Baron, S., Ed.; University of Texas Medical Branch at Galveston: Galveston, TX, USA, 1996; Chapter 85. Available online: https://www.ncbi.nlm.nih.gov/books/NBK8137/ (accessed on 1 December 2020).
- Zhao, W.; Zhong, Z.; Xie, X.; Yu, Q.; Liu, J. Relation Between Chest CT Findings and Clinical Conditions of Coronavirus Disease (COVID-19) Pneumonia: A Multicenter Study. Am. J. Roentgenol. 2020, 214, 1072–1077. [Google Scholar] [CrossRef]
- Corman, V.M.; Landt, O.; Kaiser, M.; Molenkamp, R.; Meijer, A.; Chu, K.W.A.; Bleicker, T.; Brünink, S.; Schneider, J.; Schmidt, M.L.; et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro. Surveill. 2020, 25, 2000045. [Google Scholar] [CrossRef]
- Schauwvlieghe, A.F.A.D.; Rijnders, B.J.A.; Philips, N.; Verwijs, R.; Vanderbeke, L.; Van Tienen, C.; Lagrou, K.; Verweij, P.E.; Van de Veerdonk, F.L.; Gommers, D.; et al. Dutch-Belgian Mycosis study group. Invasive aspergillosis in patients admitted to the intensive care unit with severe influenza: A retrospective cohort study. Lancet. Respir. Med. 2018, 6, 782–792. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Pemán, J.; Ruiz-Gaitán, A.; García-Vidal, C.; Salavert, M.; Ramírez, P.; Puchades, F.; García-Hita, M.; Alastruey-Izquierdo, A.; Quindós, G. Fungal co-infection in COVID-19 patients: Should we be concerned? Rev. Iberoam. Micol. 2020, 37, 41–46. [Google Scholar] [CrossRef] [PubMed]
- White, P.L.; Dhillon, R.; Cordey, A.; Hughes, H.; Faggani, F.; Soni, S.; Pandey, M.; Whitaker, H.; May, A.; Morgan, M.; et al. A national strategy to diagnose COVID-19 associated invasive fungal disease in the ICU. Clin. Infect. Dis. 2020, ciaa1298. [Google Scholar] [CrossRef] [PubMed]
- Cushion, M.T.; Linke, M.J.; Ashbaugh, A.; Sesterhenn, T.; Collins, M.S.; Lynch, K.; Brubaker, R.; Walzer, P.D. Echinocandin treatment of pneumocystis pneumonia in rodent models depletes cysts leaving trophic burdens that cannot transmit the infection. PLoS ONE 2010, 5, e8524. [Google Scholar] [CrossRef]
- Otieno-Odhiambo, P.; Wasserman, S.; Hoving, J.C. The Contribution of Host Cells to Pneumocystis Immunity: An Update. Pathogens 2019, 8, 52. [Google Scholar] [CrossRef]
- Thomas, C.F.; Limper, A.H. Pneumocystis pneumonia. N. Engl. J. Med. 2004, 350, 2487–2498. [Google Scholar] [CrossRef] [PubMed]
- Lowenstein, C.J.; Padalko, E. iNOS (NOS2) at a glance. J. Cell Sci. 2004, 117, 2865–2867. [Google Scholar] [CrossRef]
- Suess, C.; Hausmann, R. Gross and histopathological pulmonary findings in a COVID-19 associated death during self-isolation. Int. J. Legal Med. 2020, 134, 1285–1290. [Google Scholar] [CrossRef]
- Levi, M.; Thachil, J.; Iba, T.; Levy, J.H. Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet Haematol. 2020, 7, e438–e440. [Google Scholar] [CrossRef]
- Zhang, Q.; Raza, A.; Chan, V.; Minalyan, A.; Madara, J. Hamman-Rich Syndrome: A Diagnosis of Exclusion in the COVID-19 Pandemic. Cureus 2020, 12, e9866. [Google Scholar] [CrossRef] [PubMed]
- Álvarez-Troncoso, J.; Larrauri, M.Z.; Vega, M.D.M.; Vallano, R.G.; Peláez, E.P.; Rojas-Marcos, P.M.; Martín-Luengo, F.; Del Campo, P.L.; Gil, C.R.H.; Esteban, E.T. Case Report: COVID-19 with Bilateral Adrenal Hemorrhage. Am. J. Trop. Med. Hyg. 2020, 103, 1156–1157. [Google Scholar] [CrossRef] [PubMed]
- Frankel, M.; Feldman, I.; Levine, M.; Frank, Y.; Bogot, N.R.; Benjaminov, O.; Kurd, R.; Breuer, G.S.; Munter, G. Bilateral Adrenal Hemorrhage in Coronavirus Disease 2019 Patient: A Case Report. J. Clin. Endocrinol. Metab. 2020, 105, dgaa487. [Google Scholar] [CrossRef] [PubMed]
- Parekh, M.; Donuru, A.; Balasubramanya, R.; Kapur, S. Review of the Chest CT Differential Diagnosis of Ground-Glass Opacities in the COVID Era. Radiology 2020, 297, 202504. [Google Scholar] [CrossRef]
- Shi, H.; Han, X.; Jiang, N.; Cao, Y.; Alwalid, O.; Gu, J.; Fan, Y.; Zheng, C. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: A descriptive study. Lancet Infect. Dis. 2020, 20, 425–434. [Google Scholar] [CrossRef]
- Kovacs, J.A.; Masur, H. Evolving health effects of Pneumocystis: One hundred years of progress in diagnosis and treatment. JAMA 2009, 301, 2578–2585. [Google Scholar] [CrossRef] [PubMed]
- Kanne, J.P.; Yandow, D.R.; Meyer, C.A. Pneumocystis jiroveci pneumonia: High-resolution CT findings in patients with and without HIV infection. Am. J. Roentgenol. 2012, 198, W555–W561. [Google Scholar] [CrossRef] [PubMed]
- Nairz, M.; Bellmann-Weiler, R.; Ladstätter, M.; Schüllner, F.; Zimmermann, M.; Koller, A.-M.; Blunder, S.; Naschberger, H.; Kltoz, W.; Herold, M.; et al. Overcoming limitations in the availability of swabs systems used for SARS-CoV-2 laboratory diagnostics. Sci. Rep. 2021, 11, 2261. [Google Scholar] [CrossRef] [PubMed]
- Truong, J.; Ashurst, J.V. Pneumocystis Jiroveci Pneumonia; StatPearls Publishing: Treasure Island, FL, USA, 2020. Available online: https://www.ncbi.nlm.nih.gov/books/NBK482370/ (accessed on 1 December 2020).
- Matos, O.; Esteves, F. Laboratory diagnosis of Pneumocystis jirovecii pneumonia. In Microbiology of Respiratory System Infection; Kon, K., Rai, M., Eds.; Elsevier: Amsterdam, The Netherlands, 2016; pp. 185–210. [Google Scholar]
- Pennington, K.; Wilson, J.; Limper, A.H.; Escalante, P. Positive Pneumocystis jirovecii Sputum PCR Results with Negative Bronchoscopic PCR Results in Suspected Pneumocystis Pneumonia. Can. Respir. J. 2018, 2018, 6283935. [Google Scholar] [CrossRef] [PubMed]
- Medrano, F.J.; Montes-Cano, M.; Conde, M.; de la Horra, C.; Respaldiza, N.; Gasch, A.; Perez-Lozano, M.J.; Varela, J.M.; Calderon, E.J. Pneumocystis jirovecii in general population. Emerg. Infect. Dis. 2005, 11, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Mercier, T.; Aissaoui, N.; Gits-Muselli, M.; Hamane, S.; Prattes, J.; Kessler, H.H.; Mareković, I.; Pleško, S.; Steinmann, J.; Scharmann, U.; et al. Variable correlation between bronchoalveolar lavage fluid fungal load and serum-(1,3)-β-d-Glucan in patients with Pneumocystosis—A multicenter ECMM excellence center study. J. Fungi 2020, 6, 327. [Google Scholar] [CrossRef] [PubMed]
- Djawe, K.; Huang, L.; Daly, K.R.; Levin, L.; Koch, J.; Schwartzman, A.; Fong, S.; Roth, B.; Subramanian, A.; Grieco, K.; et al. Serum antibody levels to the Pneumocystis jirovecii major surface glycoprotein in the diagnosis of P. jirovecii pneumonia in HIV+ patients. PLoS ONE 2010, 5, e14259. [Google Scholar] [CrossRef]
- White, P.L.; Backx, M.; Barnes, R.A. Diagnosis and management of Pneumocystis jirovecii infection. Expert Rev. Anti. Infect. Ther. 2017, 15, 435–447. [Google Scholar] [CrossRef] [PubMed]
- Matos, O.; Tomás, A.L.; Antunes, F. Pneumocystis jirovecii and PcP. In Current Progress in Medical Mycology; Springer: Cham, Switzerland, 2017; pp. 215–254. [Google Scholar]
- Kovacs, J.A.; Gill, V.J.; Meshnick, S.; Masur, H. New insights into transmission, diagnosis, and drug treatment of Pneumocystis carinii pneumonia. J. Am. Med. Assoc. 2001, 286, 2450–2460. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Guidelines for prophylaxis against Pneumocystis carinii pneumonia for persons infected with human immunodeficiency virus. MMWR Morb Mortal Wkly Rep. 1989, 38, 1–9. [Google Scholar]
- Rubiano, C.; Tompkins, K.; Sellers, S.A.; Bramson, B.; Eron, J.; Parr, J.B.; Schranz, A.J. Pneumocystis and severe acute respiratory syndrome coronavirus 2 coinfection: A case report and review of an emerging diagnostic dilemma. Open Forum Infect. Dis. 2020, 8, ofaa633. [Google Scholar] [CrossRef]




| Clinical Picture | Imaging Diagnosis | Laboratory Diagnosis | Treatment | Clinical Evolution | |
|---|---|---|---|---|---|
| Male patient, 25-year-old [4]. Comorbidities: HIV (new diagnosis) | Profound hypoxemia | Chest X-ray: large right pneumothorax and extensive interstitial disease. Chest CT: apical cystic changes, diffuse ground-glass opacities, dense consolidation, and pneumothorax. | Nasopharyngeal SARS-CoV-2 PCR: positive. HIV serology: positive. Pneumocystis antigen (bronchial aspirate): positive. | Intubated. Trimethoprim-sulfamethoxazole, prednisone, and remdesivir. | Improved clinically, extubated 21 days later. |
| Female patient, 83-year-old [9]. Comorbidities: asthma, valvulopathy, ulcerative colitis. | Fever (39.3 °C), malaise, headache, dry cough, and dyspnea (SpO2 86%) | Chest CT: diffuse bilateral ground-glass opacities and small nodular foci of consolidation. | Leukocytosis, lymphocytopenia. Nasopharyngeal SARS-CoV-2 PCR: positive. HIV serology: nonreactive. Pneumocystis PCR (tracheal aspirate): positive. β-d-glucan elevated (305 pg/mL). | Intubated. Trimethoprim-sulfamethoxazole. | Improved clinically, extubated 7 days later. |
| Male patient, 55-year-old [10]. Comorbidities: controlled HIV and asthma. | Fever, cough, and hypoxia | Chest CT: Extensive subpleural and para-mediastinal cystic changes, subpleural ground-glass changes bilaterally. | Nose and throat SARS-CoV-2 PCR (day 2): negative. Throat SARS-CoV-2 PCR (day 7): positive. Pneumocystis PCR (sputum): positive. | High-flow oxygen, no intubation. Cotrimoxazole, prednisolone. | Improved clinically, discharged on day 14. |
| Male patient, 36-year-old [44] | Shortness of breath, fever (38.7 °C), nausea, and diarrhea for 3 weeks | Chest X-ray: diffuse hazy pulmonary opacifications. Chest CT: ground-glass alveolar airspace disease. | Lymphocytopenia Oropharyngeal SARS-CoV-2 PCR: positive. Pneumocystis PCR (bronchial alveolar lavage): positive. β-d-glucan elevated (>500 pg/mL). | Intubated, started with remdesivir and antibiotics. Trimethoprim-sulfamethoxazole, prednisone, remdesivir, and COVID-19 convalescent plasma. | Cardiac arrest 26 days later. No autopsy. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeican, I.I.; Inișca, P.; Gheban, D.; Tăbăran, F.; Aluaș, M.; Trombitas, V.; Cristea, V.; Crivii, C.; Junie, L.M.; Albu, S. COVID-19 and Pneumocystis jirovecii Pulmonary Coinfection—The First Case Confirmed through Autopsy. Medicina 2021, 57, 302. https://doi.org/10.3390/medicina57040302
Jeican II, Inișca P, Gheban D, Tăbăran F, Aluaș M, Trombitas V, Cristea V, Crivii C, Junie LM, Albu S. COVID-19 and Pneumocystis jirovecii Pulmonary Coinfection—The First Case Confirmed through Autopsy. Medicina. 2021; 57(4):302. https://doi.org/10.3390/medicina57040302
Chicago/Turabian StyleJeican, Ionuț Isaia, Patricia Inișca, Dan Gheban, Flaviu Tăbăran, Maria Aluaș, Veronica Trombitas, Victor Cristea, Carmen Crivii, Lia Monica Junie, and Silviu Albu. 2021. "COVID-19 and Pneumocystis jirovecii Pulmonary Coinfection—The First Case Confirmed through Autopsy" Medicina 57, no. 4: 302. https://doi.org/10.3390/medicina57040302
APA StyleJeican, I. I., Inișca, P., Gheban, D., Tăbăran, F., Aluaș, M., Trombitas, V., Cristea, V., Crivii, C., Junie, L. M., & Albu, S. (2021). COVID-19 and Pneumocystis jirovecii Pulmonary Coinfection—The First Case Confirmed through Autopsy. Medicina, 57(4), 302. https://doi.org/10.3390/medicina57040302










