Does the Severity of Obstructive Sleep Apnea Have an Independent Impact on Systemic Inflammation?
Abstract
1. Introduction
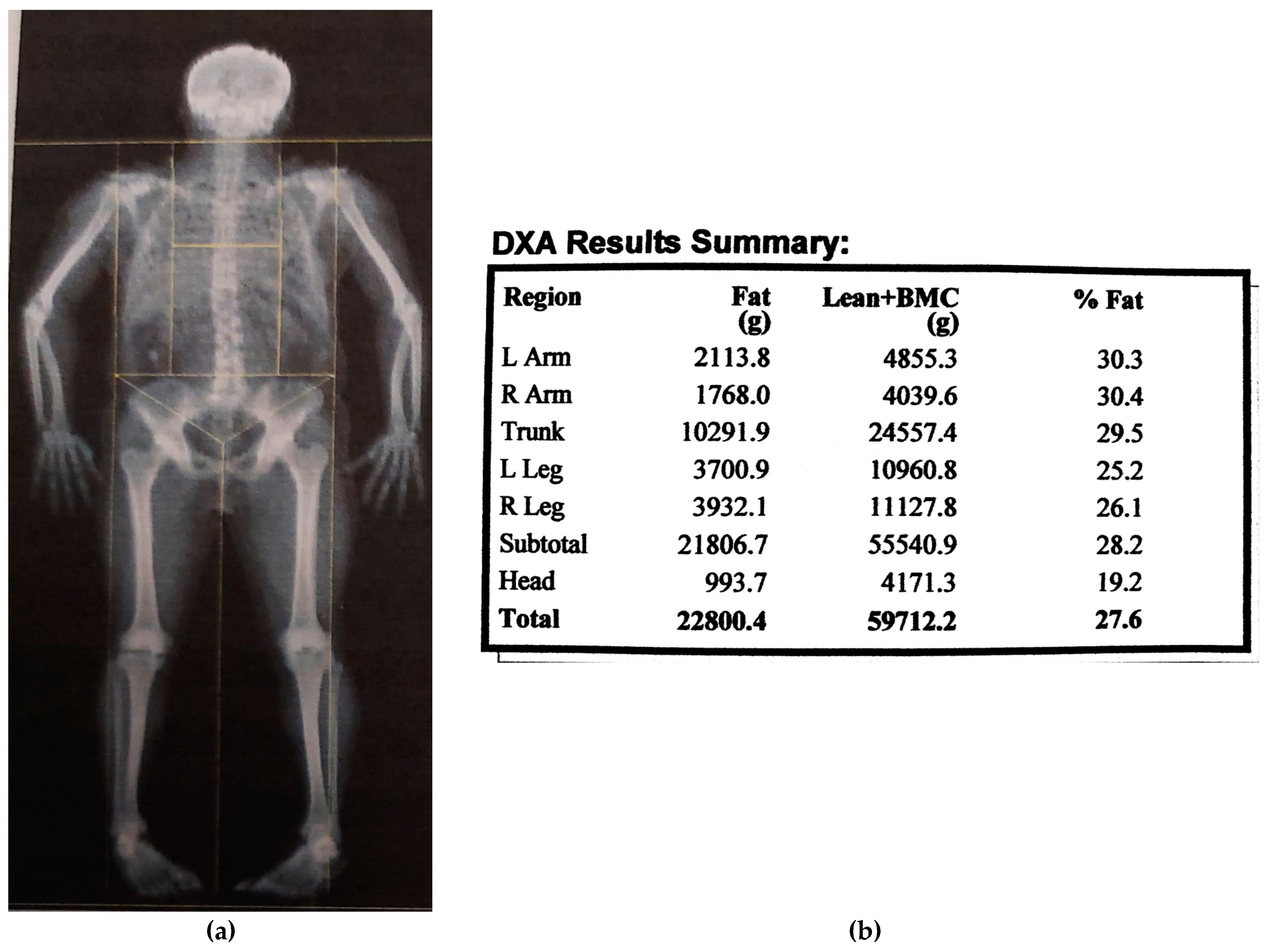
2. Materials and Methods
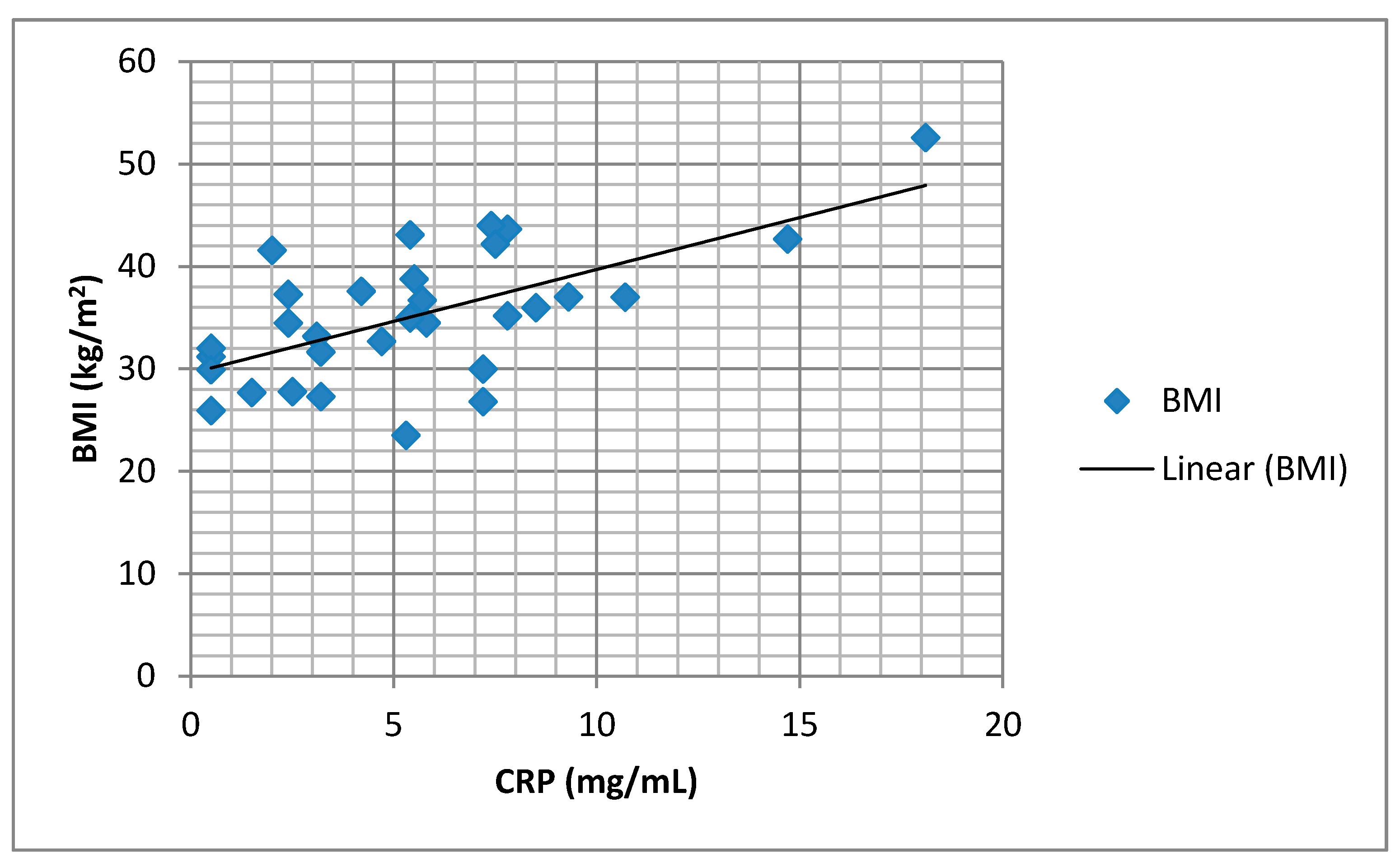
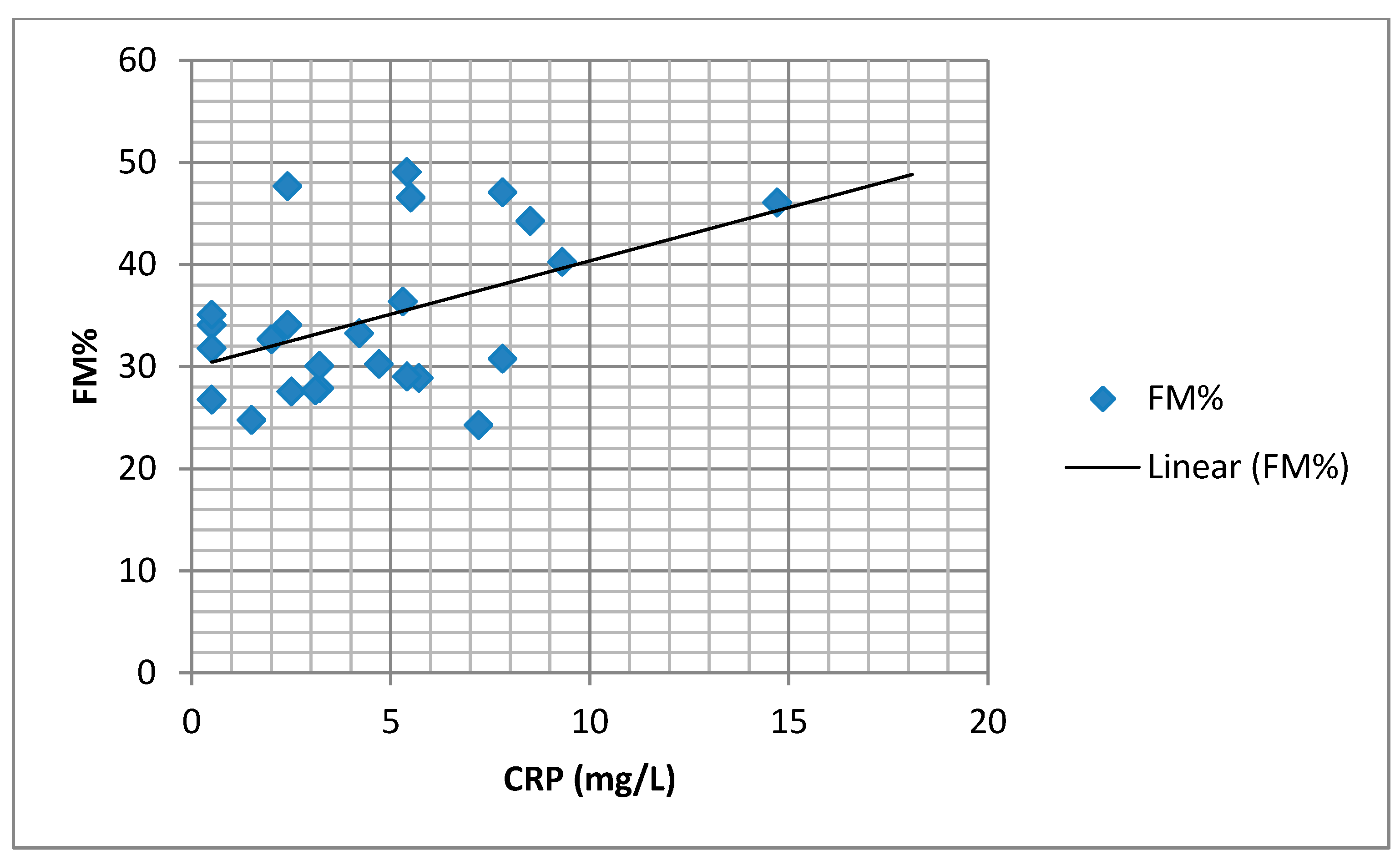
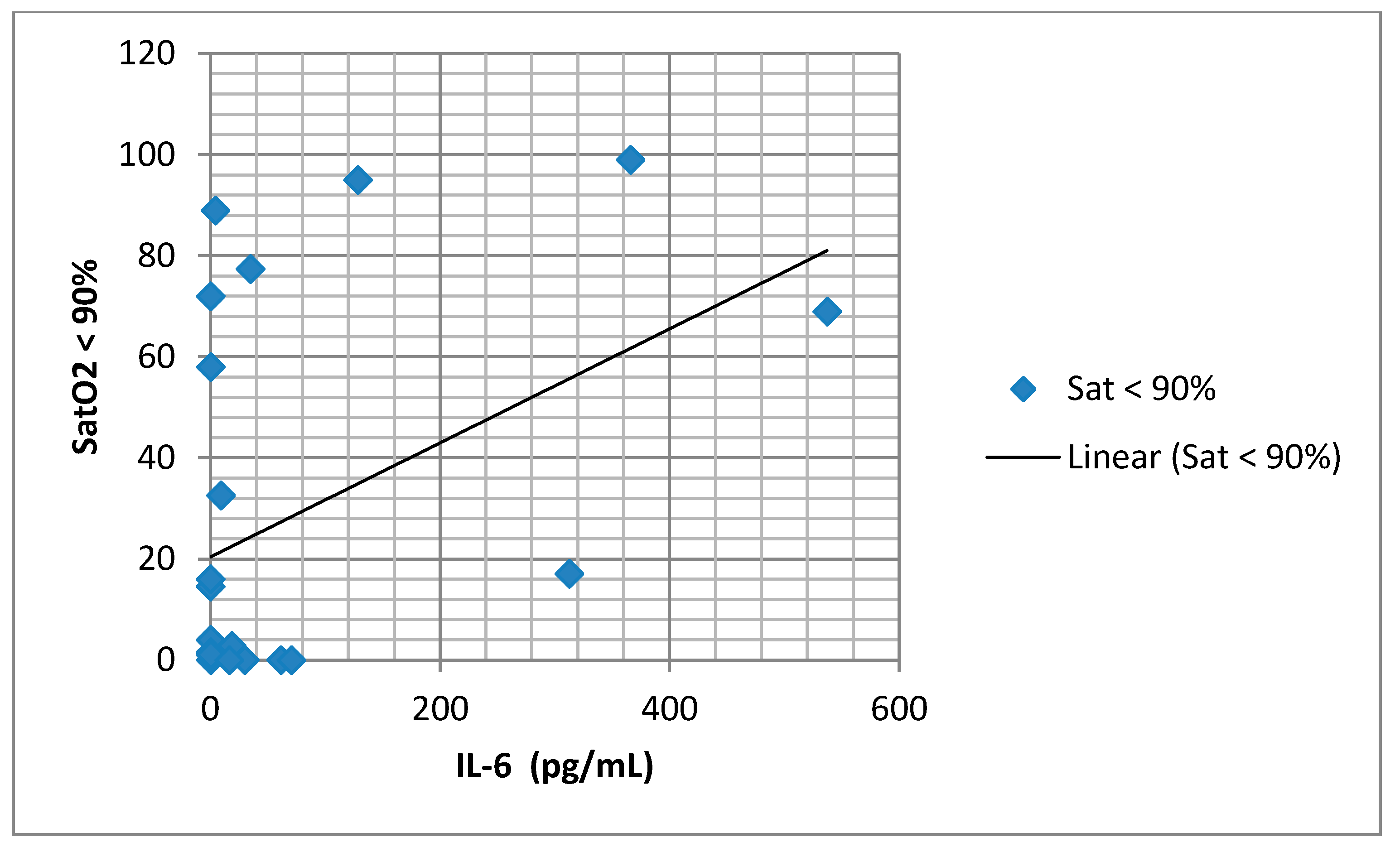
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stradling, J.R.; Chadwick, G.A.; Frew, A.J. Changes in ventilation and its components in normal subjects during sleep. Thorax 1985, 40, 364–370. [Google Scholar] [CrossRef]
- Feng, J.; Zhang, D.; Chen, B. Endothelial mechanisms of endothelial dysfunction in patients with obstructive sleep apnea. Sleep Breath. 2011, 16, 283–294. [Google Scholar] [CrossRef]
- Ryan, S.; Taylor, C.; McNicholas, W.T. Selective activation of inflammatory pathways by intermittent hypoxia in obstructive sleep apnea syndrome. Circulation 2005, 112, 2660–2667. [Google Scholar] [CrossRef]
- Kokturk, O.; Ciftci, T.U.; Mollarecep, E.; Ciftci, B. Elevated C-reactive protein levels and increased cardiovascular risk in pa-tients with obstructive sleep apnea syndrome. Int. Heart J. 2005, 46, 801–809. [Google Scholar] [CrossRef] [PubMed]
- Ursavaş, A.; Karadağ, M.; Rodoplu, E.; Yilmaztepe, A.; Oral, H.B.; Gözü, R.O. Circulating ICAM-1 and VCAM-1 levels in pa-tients with obstructive sleep apnea syndrome. Respiration 2007, 74, 525–532. [Google Scholar] [CrossRef] [PubMed]
- Von Känel, R.; Loredo, J.; Ancoli-Israel, S.; Mills, P.; Natarajan, L.; Dimsdale, J. Association between polysomnographic measures of disrupted sleep and prothrombotic factors. Chest 2007, 131, 733–739. [Google Scholar] [CrossRef]
- Punjabi, N.M.; Beamer, B.A. C-reactive protein is associated with sleep disordered breathing independent of adiposity. Sleep 2007, 30, 29–34. [Google Scholar] [CrossRef] [PubMed]
- De la Pena Bravo, M.; Serpero, L.D.; Barcelo, A. Inflammatory proteins in patients with obstructive sleep apnea with and without daytime sleepiness. Sleep Breath. 2007, 11, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Minoguchi, K.; Tazaki, T.; Yokoe, T. Elevated production of tumor necrosis factor-α by monocytes in patients with obstructive sleep apnea syndrome. Chest 2004, 126, 1473–1479. [Google Scholar] [CrossRef] [PubMed]
- Roytblat, L.; Rachinsky, M.; Fisher, A.; Greemberg, L.; Shapira, Y.; Douvdevani, A. Raised interleukin-6 levels in obese patients. Obes. Res. 2000, 8, 673–675. [Google Scholar] [CrossRef] [PubMed]
- Borrud, L.G.; Everhart, J.E.; Flegal, K.M.; Harris, T.; Looker, A.C.; Shepherd, J.A. Body compostion data for individuals eight years of age and older: US population, 1999–2004. National center for health statistics. Vital Health Stat. 2010, 11, 1–87. [Google Scholar]
- Nadeem, R.; Molnar, J.; Madbouly, E.; Nida, M.; Aggarwal, S.; Sajid, H.; Naseem, J.; Loomba, R. Serum inflammatory markers in obstructive sleep apnea: A meta-analysis. J. Clin. Sleep Med. 2013, 9, 1003–1012. [Google Scholar] [CrossRef]
- Guven, S.F.; Turkkani, M.H.; Ciftci, B.; Ciftci, T.U.; Erdogan, Y. The relationship between high-sensitivity C-reactive protein levels and the severity of obstructive sleep apnea. Sleep Breath. 2012, 16, 217–221. [Google Scholar] [CrossRef]
- Lee, L.-A.; Chen, N.-H.; Huang, C.-G.; Lin, S.-W.; Fang, T.-J.; Li, H.-Y. Patients with severe obstructive sleep apnea syndrome and elevated high-sensitivity C-reactive protein need priority treatment. Otolaryngol. Neck Surg. 2010, 143, 72–77. [Google Scholar] [CrossRef]
- Barceló, A.; Miralles, C.; Barbe, F.; Vila, M.; Pons, S.; Agustı, A.G.N. Abnormal lipid peroxidation in patients with sleep apnoea. Eur. Respir. J. 2000, 16, 644–647. [Google Scholar] [CrossRef]
- Sharma, S.; Mishra, H.K.; Sharma, H.; Goel, A.; Sreenivas, V.; Gulati, V.; Tahir, M. Obesity, and not obstructive sleep apnea, is responsible for increased serum hs-CRP levels in patients with sleep-disordered breathing in Delhi. Sleep Med. 2008, 9, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Guilleminault, C.; Kirisoglu, C.; Ohayon, M.M. C-Reactive Protein and Sleep-Disordered Breathing. Sleep 2004, 27, 1507–1517. [Google Scholar] [CrossRef] [PubMed]
- Ryan, S.; Nolan, G.M.; Hannigan, E.; Cunningham, S.; Taylor, C.; McNicholas, W.T. Cardiovascular risk markers in obstructive sleep apnoea syndrome and correlation with obesity. Thorax 2007, 62, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Imagawa, S.; Yamaguchi, Y.; Ogawa, K.; Obara, N.; Suzuki, N.; Yamamoto, M.; Nagasawa, T. Interleukin-6 and Tumor Necrosis Factor-α in Patients with Obstructive Sleep Apnea-Hypopnea Syndrome. Respiration 2004, 71, 24–29. [Google Scholar] [CrossRef]
- Alberti, A.; Sarchielli, P.; Gallinella, E.; Floridi, A.; Floridi, A.; Mazzotta, G.; Gallai, V. Plasma cytokine levels in patients with obstructive sleep apnea syndrome: A preliminary study. J. Sleep Res. 2003, 12, 305–311. [Google Scholar] [CrossRef]
- Fornadi, K.; Lindner, A.; Czira, M.E.; Szentkiralyi, A.; Lazar, A.S.; Zoller, R.; Turanyi, C.Z.; Veber, O.; Novak, M.; Mucsi, I.; et al. Lack of association between objectively assessed sleep disorders and inflammatory markers among kidney transplant recipients. Int. Urol. Nephrol. 2011, 44, 607–617. [Google Scholar] [CrossRef] [PubMed]
- Sahlman, J.; Miettinen, K.; Peuhkurinen, K.; Seppä, J.; Peltonen, M.; Herder, C.; Punnonen, K.; Vanninen, E.; Gylling, H.; Partinen, M.; et al. The activation of the inflammatory cytokines in overweight patients with mild obstructive sleep apnoea. J. Sleep Res. 2009, 19, 341–348. [Google Scholar] [CrossRef]
- Vgontzas, A.N.; Papanicolaou, D.A.; Bixler, E.O.; Kales, A.; Tyson, K.; Chrousos, G.P. Elevation of Plasma Cytokines in Disorders of Excessive Daytime Sleepiness: Role of Sleep Disturbance and Obesity. J. Clin. Endocrinol. Metab. 1997, 82, 1313–1316. [Google Scholar] [CrossRef] [PubMed]
- Mehra, R.; Storfer-Isser, A.; Kirchner, H.L.; Johnson, N.; Jenny, N.; Tracy, R.P.; Redline, S. Soluble Interleukin 6 Receptor. Arch. Intern. Med. 2006, 166, 1725–1731. [Google Scholar] [CrossRef] [PubMed]
- Kosacka, M.; Piesiak, P.; Jankowska, R. Differences Between Overlap Syndrome and Severe Sleep Apnea Syndrome In BIA/ BIvA, Adiponectin Serum Levels and in Pro-Atherogenic Indices. Paripex Indian J. Res. 2012, 3, 175–179. [Google Scholar] [CrossRef]

| Examined Parameters X ±SD (min-max) | AHI < 15 | AHI ≥ 15 | p |
|---|---|---|---|
| Age (years) | 42.57 ± 13.63 | 52.44 ± 11.38 | 0.033 |
| AHI n (min-max) | 10.2 (5.1–14.8) | 24.3 (15.1–82) | <0.001 |
| ODI | 4.63 ± 7.06 (0–23.5) | 21.56 ± 14.45 | <0.001 |
| Mean SatO2 (%) (min/max) | 93.54 ± 2.90 (88–97) | 85.63 ± 12.52 (43–96) | 0.035 |
| Min SatO2 (%) (min/max) | 86.08 ± 4.80 (80–94) | 67.75 ± 13.26 (39–85) | <0.001 |
| SatO2 < 90% (%) (min/max) | 4.90 ± 10.04 (0–32.6) | 41.86 ± 38.43 (1–99) | 0.001 |
| BMI (kg/m2) | 32.29 ± 5.58 (23.5–42.2) | 36.55 ± 6.74 (26.8–52.6) | 0.156 |
| FM% | 31.97 ± 4.13 (26.8–40.3) | 34.25 ± 9.36 (24.3–49.1) | 0.234 |
| FMI (kg) | 31.68 ± 7.78 | 34.89 ± 9.64 | 0. 483 |
| FFM (kg) | 64.01 ± 12.14 | 59.0 ± 10.16 | 0.929 |
| FFMI | 20.80 ± 3.46 | 20.8 ± 4.12 | 0.172 |
| CentrFM (kg) | 16.84 ± 3.98 (11.28–23.11) | 17.87 ± 3.84 (12.52–26.50) | 0.51 |
| TNF-α(pg/mL) | 4.26 ± 3.92 (4–6–9.9) | 10.32 ± 2.32 | 0.929 |
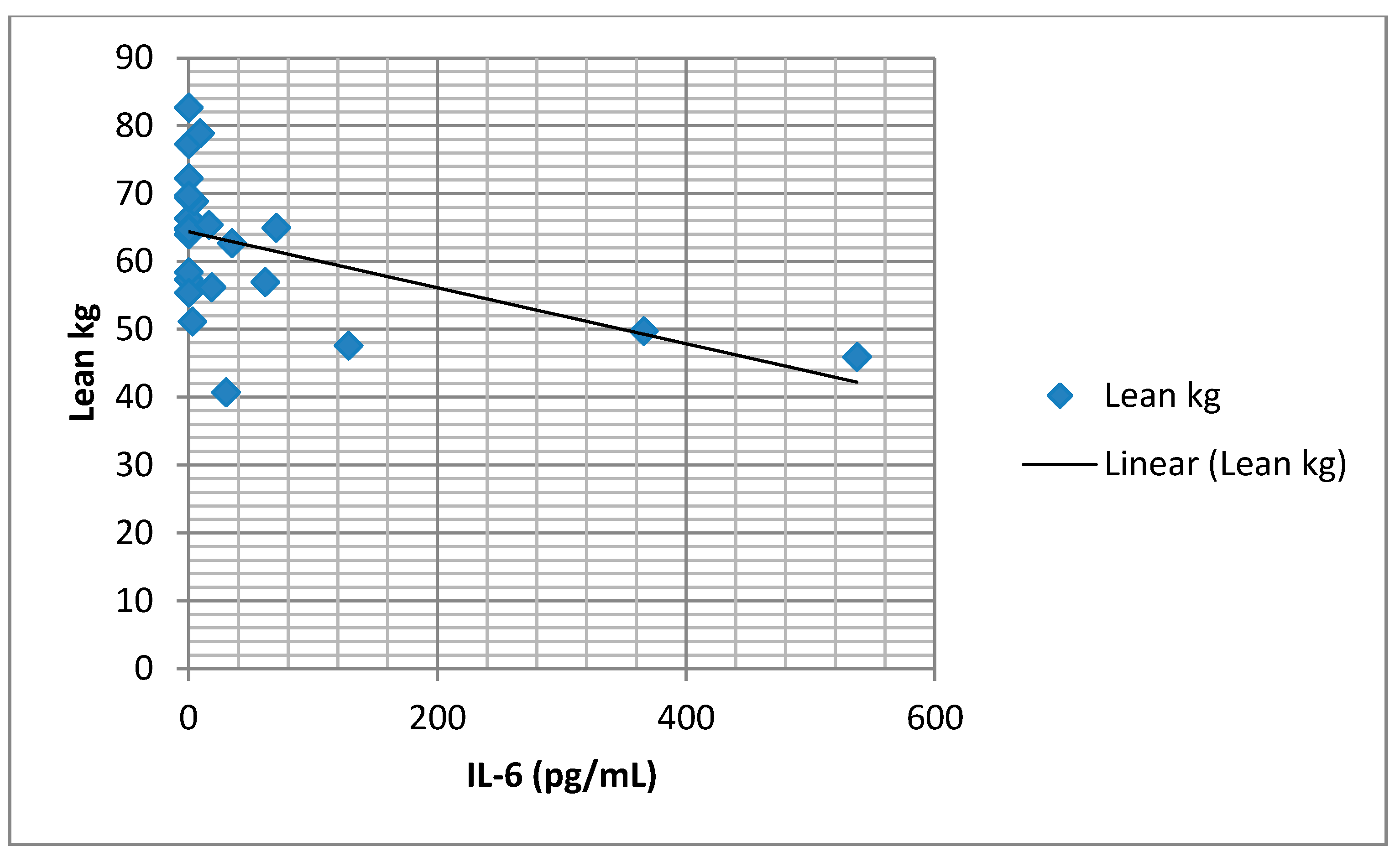
| IL-6 (pg/mL) | 38.41 ± 12.5 (0–333) | 65.17 ± 21.90 (0–537) | 0.964 |
| CRP (mg/L) | 4.52 ± 3.40(0.5–10.7) | 6.2 ± 4.43 (0.5–18.1) | 0.261 |
| Risk Factors Examined | Univariate | |
|---|---|---|
| # B (95%CI) | p | |
| Age | 0.089 (−0.021–0.199) | 0.109 |
| Gender | 2.646 (−0.536–5.828) | 0.100 |
| AHI | 0.021 (−0.031–0.072) | 0.419 |
| ODI | 0.047 (−0.008–0.101) | 0.09 |
| Mean SatO2 | −0.076 (−0.239–0.086) | 0.342 |
| MinSatO2 | −0.157 (−0.262–−0.053) | 0.005 * |
| SatO2 < 90% | 0.033 (−0.019–0.084) | 0.202 |
| BMI | 0.396 (0.212–0.579) | 0.015 * |
| FM% | 0.194 (0.028–0.36) | 0.051 |
| FMkg | 0.131 (−0.021–0.284) | 0.154 |
| CentrFM | 0.137 (−0.231–0.504) | 0.939 |
| FFM | −0.096 (−0.218–0.27) | 0.078 |
| FFMI | 0.141 (−0.415–0.697) | 0.083 |
| Risk Factors Examined | Multivariate R2 | |
|---|---|---|
| B (95%CI) | p | |
| minSatO2 | −0.017 (−0.215–0.182) | 0.808 |
| BMI | 0.534 (−1.836–2.903) | 0.525 |
| FM% | 1.306 (1.935–4.547) | 0.290 |
| FMI | −3.015 (−11.3–5.27) | 0.331 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suša, R.; Ćupurdija, V.; Novković, L.; Ratinac, M.; Janković, S.; Đoković, D.; Jovanović, J.; Pantić, K.; Simović, S.; Bazić-Sretenović, D.; et al. Does the Severity of Obstructive Sleep Apnea Have an Independent Impact on Systemic Inflammation? Medicina 2021, 57, 292. https://doi.org/10.3390/medicina57030292
Suša R, Ćupurdija V, Novković L, Ratinac M, Janković S, Đoković D, Jovanović J, Pantić K, Simović S, Bazić-Sretenović D, et al. Does the Severity of Obstructive Sleep Apnea Have an Independent Impact on Systemic Inflammation? Medicina. 2021; 57(3):292. https://doi.org/10.3390/medicina57030292
Chicago/Turabian StyleSuša, Romana, Vojislav Ćupurdija, Ljiljana Novković, Miloš Ratinac, Slobodan Janković, Danijela Đoković, Jovan Jovanović, Katarina Pantić, Stefan Simović, Danijela Bazić-Sretenović, and et al. 2021. "Does the Severity of Obstructive Sleep Apnea Have an Independent Impact on Systemic Inflammation?" Medicina 57, no. 3: 292. https://doi.org/10.3390/medicina57030292
APA StyleSuša, R., Ćupurdija, V., Novković, L., Ratinac, M., Janković, S., Đoković, D., Jovanović, J., Pantić, K., Simović, S., Bazić-Sretenović, D., & Čekerevac, I. (2021). Does the Severity of Obstructive Sleep Apnea Have an Independent Impact on Systemic Inflammation? Medicina, 57(3), 292. https://doi.org/10.3390/medicina57030292








