Clinical Profile and Length of Hospital Stay in a Sample of Psychogeriatric Patients Referred to Consultation Liaison Psychiatric Unit
Abstract
1. Introduction
2. Material and Methods
2.1. Design
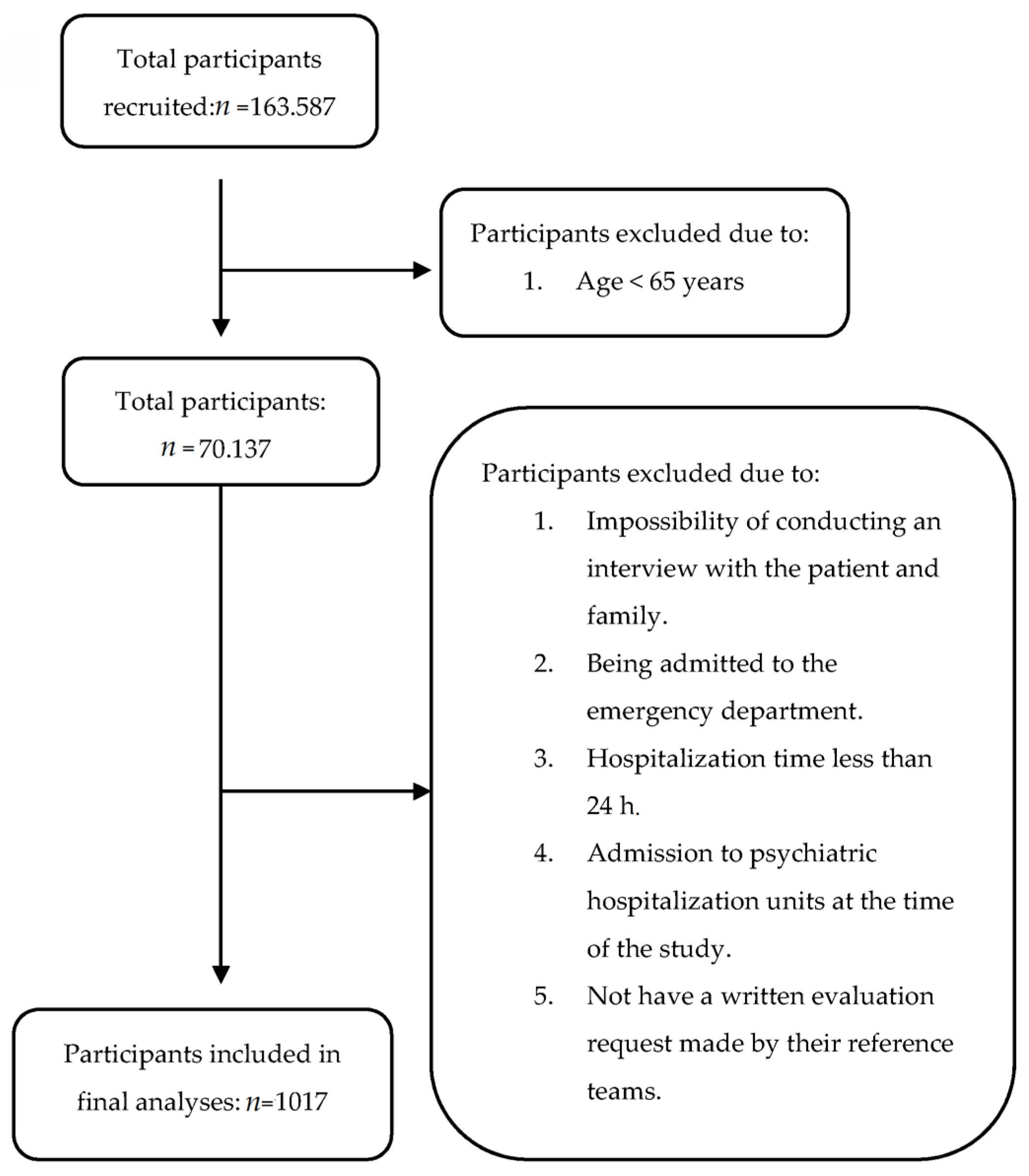
2.2. Patients
2.3. Data Sources and Procedure
2.4. Statistical Analyses
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Sowa, A.; Tobiasz-Adamczyk, B.; Topór-Mądry, R.; Poscia, A.; La Milia, D.I. Predictors of healthy ageing: Public health policy targets. BMC Health Serv. Res. 2016, 16, 441–453. [Google Scholar] [CrossRef]
- Filinson, R. “Living Well in Later Life”: An Overview of the National Service Framework for Older People in England. J. Aging Soc. Policy 2008, 20, 240–258. [Google Scholar] [CrossRef] [PubMed]
- Goh, A.M.; Westphal, A.; Daws, T.; Gascoigne-Cohen, S.; Hamilton, B.; Lautenschlager, N.T. A retrospective study of medical comorbidities in psychogeriatric patients. Psychogeriatrics 2015, 16, 12–19. [Google Scholar] [CrossRef]
- Yohannes, A.M.; Baldwin, R.C.; Connolly, M.J. Prevalence of depression and anxiety symptoms in elderly patients admitted in post-acute intermediate care. Int. J. Geriatr. Psychiatry 2008, 23, 1141–1147. [Google Scholar] [CrossRef]
- Marengoni, A.; Agüero-Torres, H.; Cossi, S.; Ghisla, M.K.; De Martinis, M.; Leonardi, R.; Fratiglioni, L. Poor mental and physical health differentially contributes to disability in hospitalized geriatric patients of different ages. Int. J. Geriatr. Psychiatry 2004, 19, 27–34. [Google Scholar] [CrossRef]
- Covinsky, K.E.; Palmer, R.M.; Fortinsky, R.H.; Counsell, S.R.; Stewart, A.L.; Rn, D.K.; Ma, C.J.B.; Landefeld, C.S. Loss of Independence in Activities of Daily Living in Older Adults Hospitalized with Medical Illnesses: Increased Vulnerability with Age. J. Am. Geriatr. Soc. 2003, 51, 451–458. [Google Scholar] [CrossRef]
- Gabayan, G.Z.; Sarkisian, C.A.; Liang, L.-J.; Sun, B.C. Predictors of Admission after Emergency Department Discharge in Older Adults. J. Am. Geriatr. Soc. 2015, 63, 39–45. [Google Scholar] [CrossRef]
- Anderson, D.; Holmes, J. Liaison psychiatry for older people—an overlooked opportunity. Age Ageing 2005, 34, 205–207. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Holmes, J.; Bentley, K.; Cameron, I. A UK survey of psychiatric services for older people in general hospitals. Int. J. Geriatr. Psychiatry 2003, 18, 716–721. [Google Scholar] [CrossRef] [PubMed]
- Tsai, M.-C.; Weng, H.-H.; Chou, S.-Y.; Tsai, C.-S.; Hung, T.-H.; Su, J.-A. One-Year Mortality of Elderly Inpatients with Delirium, Dementia, or Depression Seen by a Consultation-Liaison Service. J. Psychosom. Res. 2012, 53, 433–438. [Google Scholar] [CrossRef] [PubMed]
- González, M.; Martinez, G.; Calderón, J.; Villarroel, L.; Yuri, F.; Rojas, C.; Jeria, Á.; Valdivia, G.; Marín, P.P.; Carrasco, M. Impact of Delirium on Short-Term Mortality in Elderly Inpatients: A Prospective Cohort Study. J. Psychosom. Res. 2009, 50, 234–238. [Google Scholar] [CrossRef]
- Bronheim, H.; Fulop, G.; Kunkel, E.; Muskin, P.R.; Schindler, B.A.; Yates, W.R. The Academy of PsychosomaticMedicine practice guidelines for psychiatric consultation in the general medical setting. Psychosomatics 1998, 39, S8–S30. [Google Scholar] [CrossRef]
- Bourgeois, J.A.; Wegelin, J.A.; Servis, M.E.; Hales, R.E. Psychiatric Diagnoses of 901 Inpatients Seen by Consultation-Liaison Psychiatrists at an Academic Medical Center in a Managed Care Environment. J. Psychosom. Res. 2005, 46, 47–57. [Google Scholar] [CrossRef]
- Schellhorn, S.E.; Barnhill, J.W.; Raiteri, V.; Faso, V.L.; Ferrando, S.J. A comparison of psychiatric consultation between geriatric and non-geriatric medical inpatients. Int. J. Geriatr. Psychiatry 2009, 24, 1054–1061. [Google Scholar] [CrossRef]
- Wood, R.; Wand, A.P. The effectiveness of consultation-liaison psychiatry in the general hospital setting: A systematic review. J. Psychosom. Res. 2014, 76, 175–192. [Google Scholar] [CrossRef]
- Handrinos, D.; McKenzie, D.; Smith, G.C. Timing of Referral to a Consultation-Liaison Psychiatry Unit. J. Psychosom. Res. 1998, 39, 311–317. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. Int. J. Surg. 2014, 12, 1500–1524. [Google Scholar] [CrossRef] [PubMed]
- Tadros, G.; Salama, R.A.; Kingston, P.; Mustafa, N.; Johnson, E.; Pannell, R.; Hashmi, M. Impact of an integrated rapid response psychiatric liaison team on quality improvement and cost savings: The Birmingham RAID model. Psychiatry 2013, 37, 4–10. [Google Scholar] [CrossRef]
- CIE-10. Available online: http://eciemaps.mspsi.es/ecieMaps/browser/index_10_2008.html (accessed on 18 June 2016).
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; (DSM-5); American Psychiatric Association: Washington, DC, USA, 2013; p. 5. [Google Scholar]
- Leentjens, A.F.; Rundell, J.R.; Wolcott, D.L.; Guthrie, E.; Kathol, R.; Diefenbacher, A. Reprint of: Psychosomatic medicine and consultation-liaison psychiatry: Scope of practice, processes, and competencies for psychiatrists working in the field of CL psychiatry or psychosomatics. A consensus statement of the European Association of Consultation-Liaison Psychiatry and Psychosomatics (EACLPP) and the Academy of Psychosomatic Medicine (APM). J. Psychosom. Res. 2011, 70, 486–491. [Google Scholar] [CrossRef] [PubMed]
- Söllner, W.; Creed, F. European guidelines for training in consultation–liaison psychiatry and psychosomatics: Report of the EACLPP Workgroup on Training in Consultation–Liaison Psychiatry and Psychosomatics. J. Psychosom. Res. 2007, 62, 501–509. [Google Scholar] [CrossRef] [PubMed]
- Lobo, A.; Huyse, F.J.; Herzog, T.; Malt, U.F.; Opmeer, B.C. Eclw The ECLW collaborative study II: Patient Registration Form (PRF) instrument, training and reliability. J. Psychosom. Res. 1996, 40, 143–156. [Google Scholar] [CrossRef]
- Lyons, J.S.; Hammer, J.S.; Strain, J.J.; Fulop, G. The timing of psychiatric consultation in the general hospital and length of hospital stay. Gen. Hosp. Psychiatry 1986, 8, 159–162. [Google Scholar] [CrossRef]
- Benoit, K. Linear Regression Models with Logarithmic Transformations. London School of Economics. 2011. Available online: https://kenbenoit.net/assets/courses/ME104/logmodels2.pdf (accessed on 22 February 2021).
- World Medical Association. World medical association declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Sockalingam, S.; Alzahrani, A.; Meaney, C.; Styra, R.; Tan, A.; Hawa, R.; Abbey, S.E. Time to Consultation-Liaison Psychiatry Service Referral as a Predictor of Length of Stay. Psychosomatics 2016, 57, 264–272. [Google Scholar] [CrossRef] [PubMed]
- Kishi, Y.; Meller, W.H.; Kathol, R.G.; Swigart, S.E. Factors Affecting the Relationship Between the Timing of Psychiatric Consultation and General Hospital Length of Stay. J. Psychosom. Res. 2004, 45, 470–476. [Google Scholar] [CrossRef]
- Royal College of Psychiatrists. Who Cares Wins. Improving the Outcome for Older People Admitted to the General Hospital. Guidelines for the Development of Liaison Mental Health Services for Older People. Report of a Working group for the Faculty of Old Age Psychiatric 2005. Available online: http://www.rcpsych.ac.uk/college/faculty/oap/public/index.html (accessed on 10 March 2016).
- Ferrari, S.; Mattei, G.; Marchi, M.; Galeazzi, G.M.; Pingani, L. Is Consultation-Liaison Psychiatry ‘Getting Old’? How Psychiatry Referrals in the General Hospital Have Changed over 20 Years. Int. J. Environ. Res. Public Health 2020, 17, 7389. [Google Scholar] [CrossRef]
- Desan, P.H.; Zimbrean, P.C.; Weinstein, A.J.; Bozzo, J.E.; Sledge, W.H. Proactive Psychiatric Consultation Services Reduce Length of Stay for Admissions to an Inpatient Medical Team. J. Psychosom. Res. 2011, 52, 513–520. [Google Scholar] [CrossRef] [PubMed]
- Lewis, R.; Glasby, J. Delayed discharge from mental health hospitals: Results of an English postal survey. Health Soc. Care Community 2006, 14, 225–230. [Google Scholar] [CrossRef] [PubMed]
- Tulloch, A.D.; Fearon, P.; David, A.S. Length of Stay of General Psychiatric Inpatients in the United States: Systematic Review. Adm. Policy Ment. Heal. Ment. Health Serv. Res. 2010, 38, 155–168. [Google Scholar] [CrossRef]
- Chung, W.; Oh, S.-M.; Suh, T.; Lee, Y.M.; Oh, B.H.; Yoon, C.-W. Determinants of length of stay for psychiatric inpatients: Analysis of a national database covering the entire Korean elderly population. Health Policy 2010, 94, 120–128. [Google Scholar] [CrossRef]
- Anderson, D.; Nortcliffe, M.; Dechenne, S.; Wilson, K. The rising demand for consultation-liaison psychiatry for older people: Comparisons within Liverpool and the literature across time. Int. J. Geriatr. Psychiatry 2011, 26, 1231–1235. [Google Scholar] [CrossRef]
- Chen, K.Y.; Evans, R.; Larkins, S. Why are hospital doctors not referring to Consultation-Liaison Psychiatry?—A systemic review. BMC Psychiatry 2016, 16, 390. [Google Scholar] [CrossRef] [PubMed]
- Yamada, K.; Hosoda, M.; Nakashima, S.; Furuta, K.; Awata, S. Psychiatric diagnosis in the elderly referred to a consultation-liaison psychiatry service in a general geriatric hospital in Japan. Geriatr. Gerontol. Int. 2011, 12, 304–309. [Google Scholar] [CrossRef]
- Britton, A.M.; Luxenberg, J. Antipsychotics for delirium. Cochrane Database Syst. Rev. 2007, 18, CD005594. [Google Scholar] [CrossRef]
- Riviere, J.; Van Der Mast, R.C.; Vandenberghe, J.; Eede, F.V.D. Efficacy and Tolerability of Atypical Antipsychotics in the Treatment of Delirium: A Systematic Review of the Literature. Psychosomatics 2019, 60, 18–26. [Google Scholar] [CrossRef]
- Abad, V.C.; Guilleminault, C. Insomnia in Elderly Patients: Recommendations for Pharmacological Management. Drugs Aging 2018, 35, 791–817. [Google Scholar] [CrossRef]
- Burry, L.; Mehta, S.; Perreault, M.M.; Luxenberg, J.S.; Siddiqi, N.; Hutton, B.; Fergusson, D.A.; Bell, C.; Rose, L. Antipsychotics for treatment of delirium in hospitalized non-ICU patients. Cochrane Database Syst Rev. 2018, 6, CD005594. [Google Scholar] [CrossRef]
- Yunusa, I.; Alsumali, A.; Garba, A.E.; Regestein, Q.R.; Eguale, T. Assessment of Reported Comparative Effectiveness and Safety of Atypical Antipsychotics in the Treatment of Behavioral and Psychological Symptoms of Dementia: A Network Meta-analysis. JAMA Netw. Open 2019, 2, e190828. [Google Scholar] [CrossRef] [PubMed]
- Basciotta, M.; Zhou, W.; Ngo, L.; Donnino, M.; Marcantonio, E.R.; Herzig, S.J. Antipsychotics and the Risk of Mortality or Cardiopulmonary Arrest in Hospitalized Adults. J. Am. Geriatr. Soc. 2019, 68, 544–550. [Google Scholar] [CrossRef] [PubMed]
- Diefenbacher, A.; Strain, J.J. Consultation-liaison psychiatry: Stability and change over a 10-year-period. Gen. Hosp. Psychiatry 2002, 24, 249–256. [Google Scholar] [CrossRef]
- Leigh, H. The function of consultation-liaison Psychiatriy. In Handbook of Consultation-Liaison Psychiatry; Leigh, H., Streltzer, J., Eds.; Springer: New York, NY, USA, 2015; pp. 11–14. [Google Scholar]
- O’Sullivan, R.; Inouye, S.K.; Meagher, D. Delirium and depression: Inter-relationship and clinical overlap in elderly people. Lancet Psychiatry 2014, 1, 303–311. [Google Scholar] [CrossRef]
| Youngest-Old N = 518 | Oldest-Old N = 499 | Total N = 1017 | p Value | ||
|---|---|---|---|---|---|
| Gender | Male | 297 (59%) | 206 (41%) | 503 (100%) | p < 0.001 ** |
| Female | 221 (43%) | 293 (57%) | 514 (100%) | p < 0.001 ** | |
| Medical Diagnosis | General Medicine | 183 (55%) | 152 (45%) | 335 (100%) | NS |
| Medical Subspecialties † | 203 (48%) | 216 (52%) | 419 (100%) | NS | |
| Neurology | 48 (62%) | 30 (38%) | 78 (100%) | NS | |
| Psychiatry | 29 (59%) | 20 (41%) | 49 (100%) | NS | |
| Surgery ‡ | 55 (40%) | 81 (60%) | 136 (100%) | p = 0.08 | |
| Previous Psychiatric Diagnosis | Yes | 227 (45%) | 277 (55%) | 504 (100%) | p < 0.001 ** |
| No | 291 (57%) | 222 (43%) | 513 (100%) | p < 0.001 ** | |
| Physical Disability | Autonomous | 293 (56%) | 234 (44%) | 527 (100%) | p = 0.02 * |
| Needs Assistance | 225 (46%) | 265 (54%) | 490 (100%) | p = 0.02 * |
| Youngest-Old N = 518 | Oldest-Old N = 499 | Total N = 1017 | p Value | ||
|---|---|---|---|---|---|
| Referring Service | General Medicine | 156 (53%) | 141 (47%) | 297 (100%) | NS |
| Medical Subspecialties † | 184 (60%) | 124 (40%) | 308 (100%) | p < 0.001 ** | |
| Surgery ‡ | 124 (39%) | 204 (62%) | 328 (100%) | p < 0.001 ** | |
| Neurology | 54 (64%) | 30 (36%) | 84 (100%) | p = 0.01 * | |
| Psychiatric Diagnosis Referring Service | Anxiety Disorder | 60 (61%) | 38 (39%) | 98 (100%) | p = 0.032 * |
| Mood Disorder | 187 (50%) | 185 (50%) | 372 (100%) | NS | |
| Neurocognitive Disorder § | 124 (40%) | 187 (60%) | 311 (100%) | p < 0.001 ** | |
| Substance Dependence | 57 (83%) | 12 (17%) | 69 (100%) | p < 0.001 ** | |
| Psychosis | 13 (43%) | 17 (57%) | 30 (100%) | NS | |
| Personality Disorder | 6 (50%) | 6 (50%) | 12 (100%) | NS | |
| Adaptive Disorder | 55 (60%) | 36 (40%) | 91 (100%) | NS | |
| Suicide Attempt | 16 (47%) | 18 (53%) | 34 (100%) | NS | |
| Psychiatric Diagnosis CLP Unit | Anxiety Disorder | 19 (53%) | 17 (47%) | 36 (100%) | NS |
| Mood Disorder | 101 (61%) | 65 (39%) | 166 (100%) | p = 0.005 ** | |
| Neurocognitive Disorder | 182 (41%) | 264 (60%) | 446 (100%) | p < 0.001 ** | |
| Substance Dependence | 56 (82%) | 12 (18%) | 68 (100%) | p < 0.001 ** | |
| Psychosis | 23 (52%) | 21 (48%) | 44 (100%) | NS | |
| Adaptive Disorder | 98 (54%) | 85 (46%) | 183 (100%) | NS | |
| Personality/Somatoform Disorder | 13 (62%) | 8 (38%) | 21 (100%) | NS | |
| No Diagnosis | 26 (49%) | 27 (51%) | 53 (100%) | NS |
| Youngest-Old N = 518 | Oldest-Old N = 499 | Total N = 1017 | p-Value | ||
|---|---|---|---|---|---|
| Pharmacological Prescription by CLP Unit | Antidepressant | 166 (56%) | 132 (44%) | 298 (100%) | NS |
| Antipsychotic | 184 (43%) | 245 (57%) | 429 (100%) | p < 0.001 ** | |
| Mood Stabilizer | 12 (63%) | 7 (37%) | 19 (100%) | NS | |
| Benzodiazepine | 68 (67%) | 33 (33%) | 101 (100%) | p = 0.001 ** | |
| No Prescription | 88 (52%) | 82 (48%) | 170 (100%) | NS | |
| Number of Visits by CLP Unit | 1 | 196 (58%) | 139 (42%) | 335 (100%) | p = 0.001 ** |
| 2–3 | 226 (46%) | 264 (54%) | 490 (100%) | p = 0.003 ** | |
| 4–7 | 74 (49%) | 78 (51%) | 152 (100%) | NS | |
| >7 | 22 (55%) | 18 (45%) | 40 (100%) | NS | |
| Discharge Disposition | Nursing Home | 56 (42%) | 76 (58%) | 132 (100%) | p = 0.036 * |
| Home | 438 (53%) | 396 (47%) | 834 (100%) | p = 0.031 * | |
| Death | 16 (44%) | 20 (56%) | 36 (100%) | NS | |
| Others | 8 (53%) | 7 (47%) | 15 (100%) | NS |
| Step | b (95% CI) | SE | P | |
|---|---|---|---|---|
| 1 | Gender | −0.03 (−0.11, 0.04) | 0.04 | 0.4 |
| Geriatric Group † | −0.09 (−0.16, −0.01) | 0.04 | 0.02 * | |
| 2 | Gender | −0.03 (−0.10, 0.04) | 0.04 | 0.3 |
| Geriatric Group † | −0.11 (−0.18, −0.04) | 0.04 | <0.001 ** | |
| History of Previous Psychiatric Diagnosis ‡ | −0.16 (−0.23, −0.09) | 0.04 | <0.001 ** | |
| Physical Disability § | 0.15 (0.08, 0.22) | 0.04 | <0.001 ** | |
| 3 | Gender | −0.02 (−0.07, 0.03) | 0.03 | 0.5 |
| Geriatric Group † | −0.06 (−0.11, −0.01) | 0.03 | 0.01 * | |
| History of Previous Psychiatric Diagnosis ‡ | −0.06 (−0.11, −0.01) | 0.03 | 0.03 * | |
| Physical Disability § | 0.07 (0.02, 0.12) | 0.03 | <0.001 ** | |
| Log Time to Consultation-Liaison Psychiatry Service (days) | 0.58 (0.53, 0.63) | 0.03 | <0.001 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barra, B.J.; Varela, L.F.; Maldonado, J.R.; Calvo, P.; Bastidas, A.; Sánchez, R.; Pintor, L. Clinical Profile and Length of Hospital Stay in a Sample of Psychogeriatric Patients Referred to Consultation Liaison Psychiatric Unit. Medicina 2021, 57, 256. https://doi.org/10.3390/medicina57030256
Barra BJ, Varela LF, Maldonado JR, Calvo P, Bastidas A, Sánchez R, Pintor L. Clinical Profile and Length of Hospital Stay in a Sample of Psychogeriatric Patients Referred to Consultation Liaison Psychiatric Unit. Medicina. 2021; 57(3):256. https://doi.org/10.3390/medicina57030256
Chicago/Turabian StyleBarra, Bernardo J., Luis F. Varela, José R. Maldonado, Pilar Calvo, Anna Bastidas, Roberto Sánchez, and Luis Pintor. 2021. "Clinical Profile and Length of Hospital Stay in a Sample of Psychogeriatric Patients Referred to Consultation Liaison Psychiatric Unit" Medicina 57, no. 3: 256. https://doi.org/10.3390/medicina57030256
APA StyleBarra, B. J., Varela, L. F., Maldonado, J. R., Calvo, P., Bastidas, A., Sánchez, R., & Pintor, L. (2021). Clinical Profile and Length of Hospital Stay in a Sample of Psychogeriatric Patients Referred to Consultation Liaison Psychiatric Unit. Medicina, 57(3), 256. https://doi.org/10.3390/medicina57030256







