Use of an Insulation-Tipped Knife during Rigid Bronchoscopic Treatment of Benign Tracheobronchial Stenosis
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
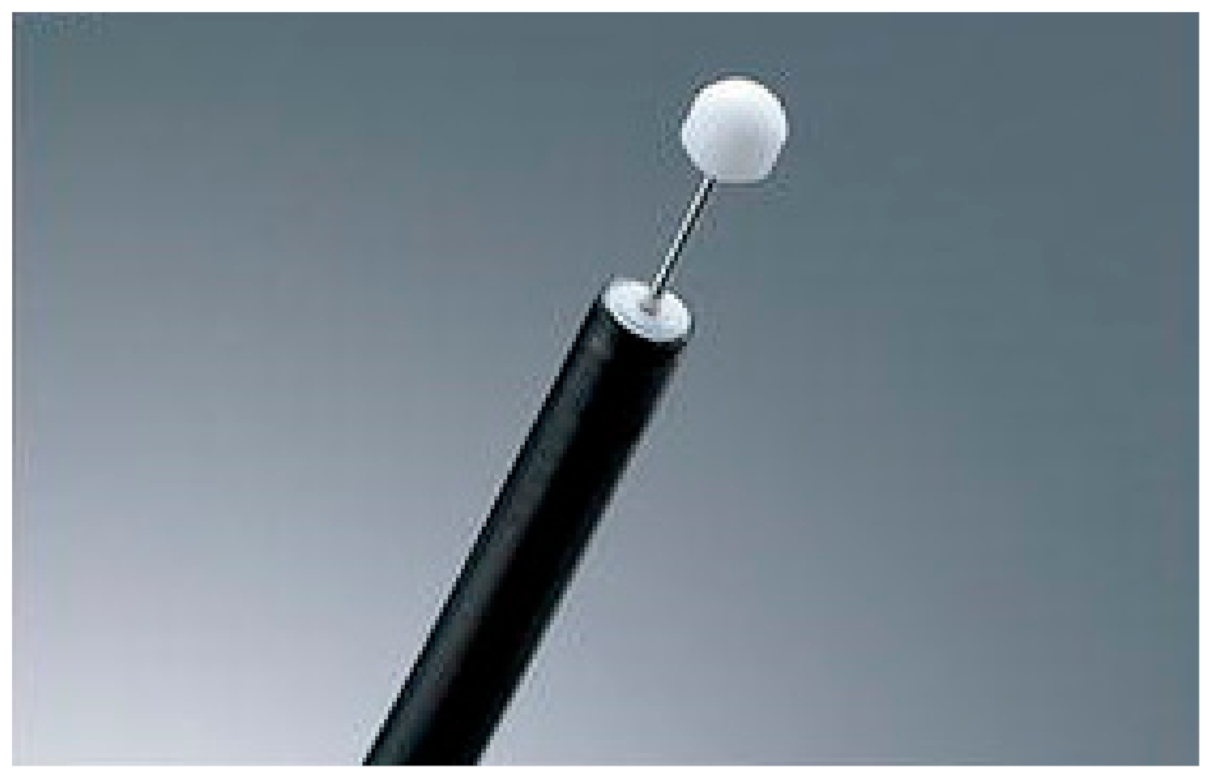
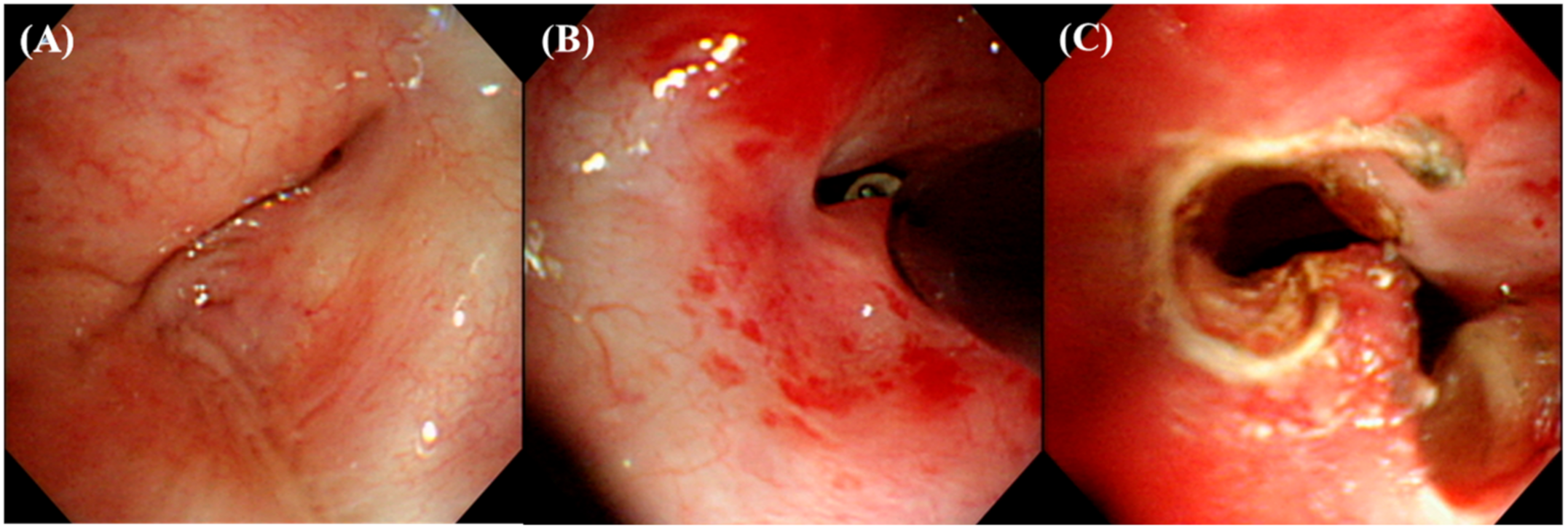
2.2. Airway Intervention Techniques
2.3. Airway Stents
2.4. Data Collection
2.5. Statistical Analysis
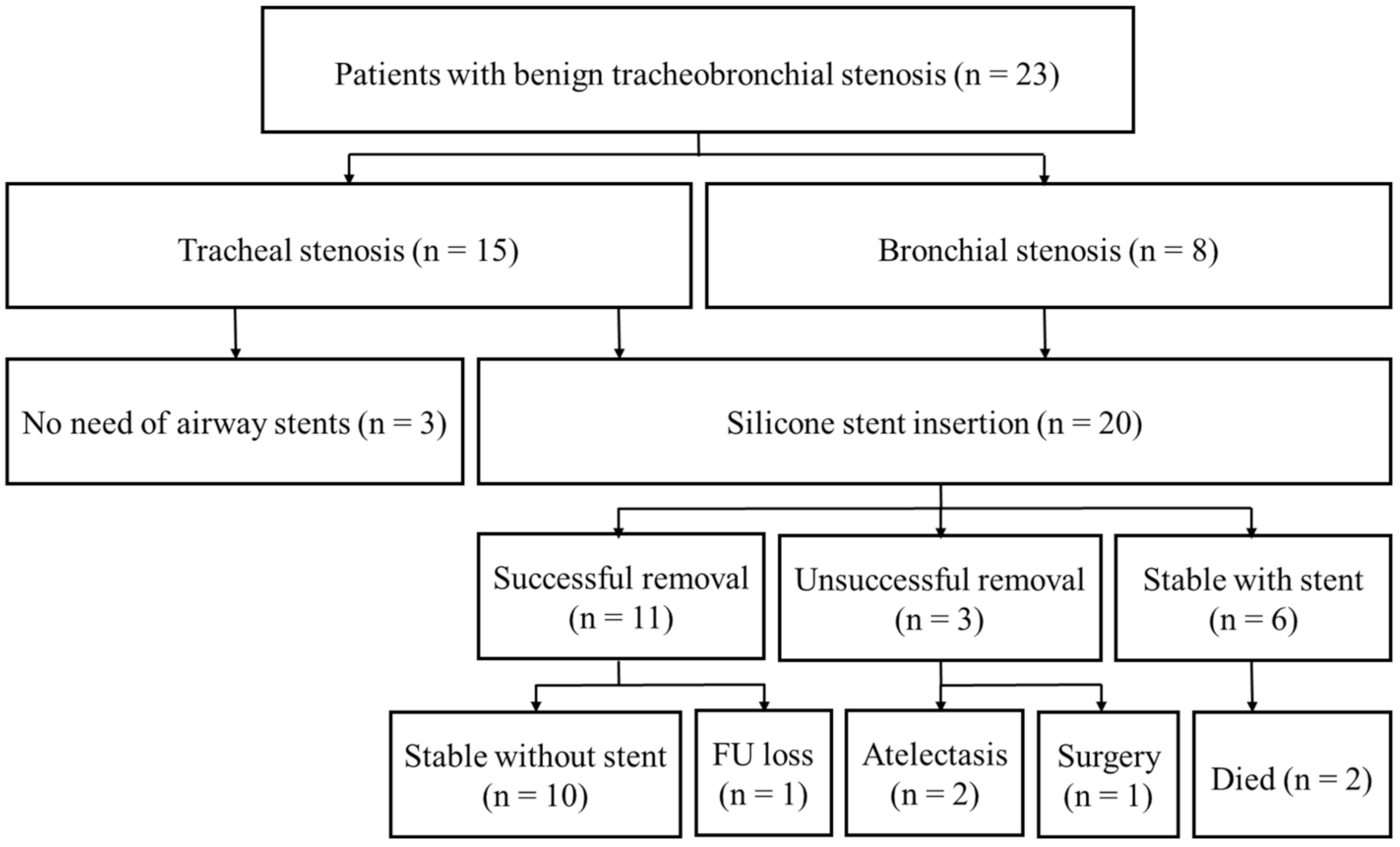
3. Results
3.1. Baseline Characteristics
3.2. Treatment Modalities
3.3. Treatment Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Puchalski, J.; Musani, A.I. Tracheobronchial Stenosis: Causes and advances in management. Clin. Chest Med. 2013, 34, 557–567. [Google Scholar] [CrossRef] [PubMed]
- Ryu, Y.J.; Kim, H.; Yu, C.M.; Choi, J.C.; Kwon, Y.S.; Kwon, O.J. Use of silicone stents for the management of post-tuberculosis tracheobronchial stenosis. Eur. Respir. J. 2006, 28, 1029–1035. [Google Scholar] [CrossRef] [PubMed]
- Rea, F.; Callegaro, D.; Loy, M.; Zuin, A.; Narne, S.; Gobbi, T.; Grapeggia, M.; Sartori, F. Benign tracheal and laryngotracheal stenosis: Surgical treatment and results. Eur. J. Cardio Thorac. Surg. 2002, 22, 352–356. [Google Scholar] [CrossRef]
- Wain, J.C. Postintubation tracheal stenosis. Chest Surg. Clin. N. Am. 2003, 13, 231–246. [Google Scholar] [CrossRef]
- Kim, H. Stenting therapy for stenosing airway disease. Respirology 1998, 3, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Galluccio, G.; Lucantoni, G.; Battistoni, P.; Paone, G.; Batzella, S.; Lucifora, V.; Dello Iacono, R. Interventional endoscopy in the management of benign tracheal stenoses: Definitive treatment at long-term follow-up. Eur. J. Cardio Thorac. Surg. 2009, 35, 429–433, Discussion 933–424. [Google Scholar] [CrossRef] [PubMed]
- Dalar, L.; Karasulu, L.; Abul, Y.; Ozdemir, C.; Sokucu, S.N.; Tarhan, M.; Altin, S. Bronchoscopic Treatment in the Management of Benign Tracheal Stenosis: Choices for Simple and Complex Tracheal Stenosis. Ann. Thorac. Surg. 2016, 101, 1310–1317. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.W.; Choi, Y.S.; Kim, K.; Shim, Y.M.; Lee, K.S.; Kim, H.J.; Kim, J. Main Bronchial Reconstruction with Sparing of Pulmonary Parenchyma for Benign Diseases. J. Korean Med. Sci. 2006, 21, 1017–1020. [Google Scholar] [CrossRef] [PubMed]
- Ranu, H.; Madden, B.P. Endobronchial stenting in the management of large airway pathology. Postgrad. Med. J. 2009, 85, 682–687. [Google Scholar] [CrossRef] [PubMed]
- Wahidi, M.M.; Unroe, M.A.; Adlakha, N.; Beyea, M.; Shofer, S.L. The Use of Electrocautery as the Primary Ablation Modality for Malignant and Benign Airway Obstruction. J. Thorac. Oncol. 2011, 6, 1516–1520. [Google Scholar] [CrossRef] [PubMed]
- Colt, H.G.; Dumon, J.F. Airway stents. Present and future. Clin. Chest Med. 1995, 16, 465–478. [Google Scholar] [PubMed]
- Ryu, Y.J.; Kim, H.; Yu, C.M.; Choi, J.C.; Kwon, Y.S.; Kim, J.; Suh, S.W. Comparison of Natural and Dumon airway stents for the management of benign tracheobronchial stenoses. Respirology 2006, 11, 748–754. [Google Scholar] [CrossRef] [PubMed]
- Yoon, S.B.; Park, Y.W.; Cheon, M.J.; Koh, Y.M.; Park, S.; Kim, S.J.; Lee, S.H. Palliation of Postintubation Tracheal Stenosis Using Insulation-Tipped Diathermic Knife 2: A Case Report. Med. Princ. Pract. 2016, 25, 90–92. [Google Scholar] [CrossRef] [PubMed]
- Amat, B.; Esselmann, A.; Reichle, G.; Rohde, H.J.; Westhoff, M.; Freitag, L. The electrosurgical knife in an optimized intermittent cutting mode for the endoscopic treatment of benign web-like tracheobronchial stenosis. Arch. Bronconeumol. 2012, 48, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Mori, G.; Nonaka, S.; Oda, I.; Abe, S.; Suzuki, H.; Yoshinaga, S.; Nakajima, T.; Saito, Y. Novel strategy of endoscopic submucosal dissection using an insulation-tipped knife for early gastric cancer: Near-side approach method. Endosc. Int. Open 2015, 3, E425–E431. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ernst, A.; Feller-Kopman, D.; Becker, H.D.; Mehta, A.C. Central Airway Obstruction. Am. J. Respir. Crit. Care Med. 2004, 169, 1278–1297. [Google Scholar] [CrossRef] [PubMed]
- McArdle, J.R.; Gildea, T.R.; Mehta, A.C. Balloon Bronchoplasty: Its indication, benefits, and complications. J. Bronchol. 2005, 12, 123–127. [Google Scholar] [CrossRef]
- Altinok, T.; Can, A. Management of Tracheobronchial Injuries. Eurasian J. Med. 2014, 46, 209–215. [Google Scholar] [CrossRef] [PubMed]
| Study Patients (n = 23) | ||
|---|---|---|
| Age (years) | 54.2 ± 14.8 | |
| Sex (male/female) | 9/14 (39.1%/60.9%) | |
| Comorbidities | Respiratory diseases | 8 (34.8%) |
| Chronic renal failure | 5 (21.7%) | |
| Diabetes mellitus | 5 (21.7%) | |
| Ischemic heart disease | 4 (17.4%) | |
| Hypertension | 4 (17.4%) | |
| Heart failure | 3 (13.0%) | |
| Chronic liver diseases | 3 (13.0%) | |
| Others * | 8 | |
| No. of comorbidities | 1.8 ± 1.44 | |
| Site of stenosis | Trachea | 15 (65.2%) |
| Main bronchus | 6 (26.1%) | |
| Right bronchus intermedius | 2 (8.7%) | |
| Reason of stenosis | PITS | 9 (39.1%) |
| PTTS | 6 (26.1%) | |
| Post-infectious | 7 (30.4%) | |
| Post-operative | 1 (4.3%) | |
| Nature of stenosis † | Simple | 3 (13.0%) |
| Complex | 20 (87.0%) | |
| Length of stenosis (mm) | 32.6 ± 12.4 | |
| Stent insertion | 20 (87.0%) | |
| Patients (n = 23) | |
|---|---|
| Acute complication | 2 (8.7%) |
| Treatment success * | 20 (87.0%) |
| Successful stent removal | 11/20 (55%) |
| Stable with stent | 6/20 (30%) |
| Surgical treatment | 1 (4.3%) |
| Death | 2 (8.7%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, J.-W.; Ko, Y.; Kim, C. Use of an Insulation-Tipped Knife during Rigid Bronchoscopic Treatment of Benign Tracheobronchial Stenosis. Medicina 2021, 57, 251. https://doi.org/10.3390/medicina57030251
Park J-W, Ko Y, Kim C. Use of an Insulation-Tipped Knife during Rigid Bronchoscopic Treatment of Benign Tracheobronchial Stenosis. Medicina. 2021; 57(3):251. https://doi.org/10.3390/medicina57030251
Chicago/Turabian StylePark, Ji-Won, Yousang Ko, and Changhwan Kim. 2021. "Use of an Insulation-Tipped Knife during Rigid Bronchoscopic Treatment of Benign Tracheobronchial Stenosis" Medicina 57, no. 3: 251. https://doi.org/10.3390/medicina57030251
APA StylePark, J.-W., Ko, Y., & Kim, C. (2021). Use of an Insulation-Tipped Knife during Rigid Bronchoscopic Treatment of Benign Tracheobronchial Stenosis. Medicina, 57(3), 251. https://doi.org/10.3390/medicina57030251






