Does Cement Augmentation of the Sacroiliac Screw Lead to Superior Biomechanical Results for Fixation of the Posterior Pelvic Ring? A Biomechanical Study
Abstract
:1. Introduction
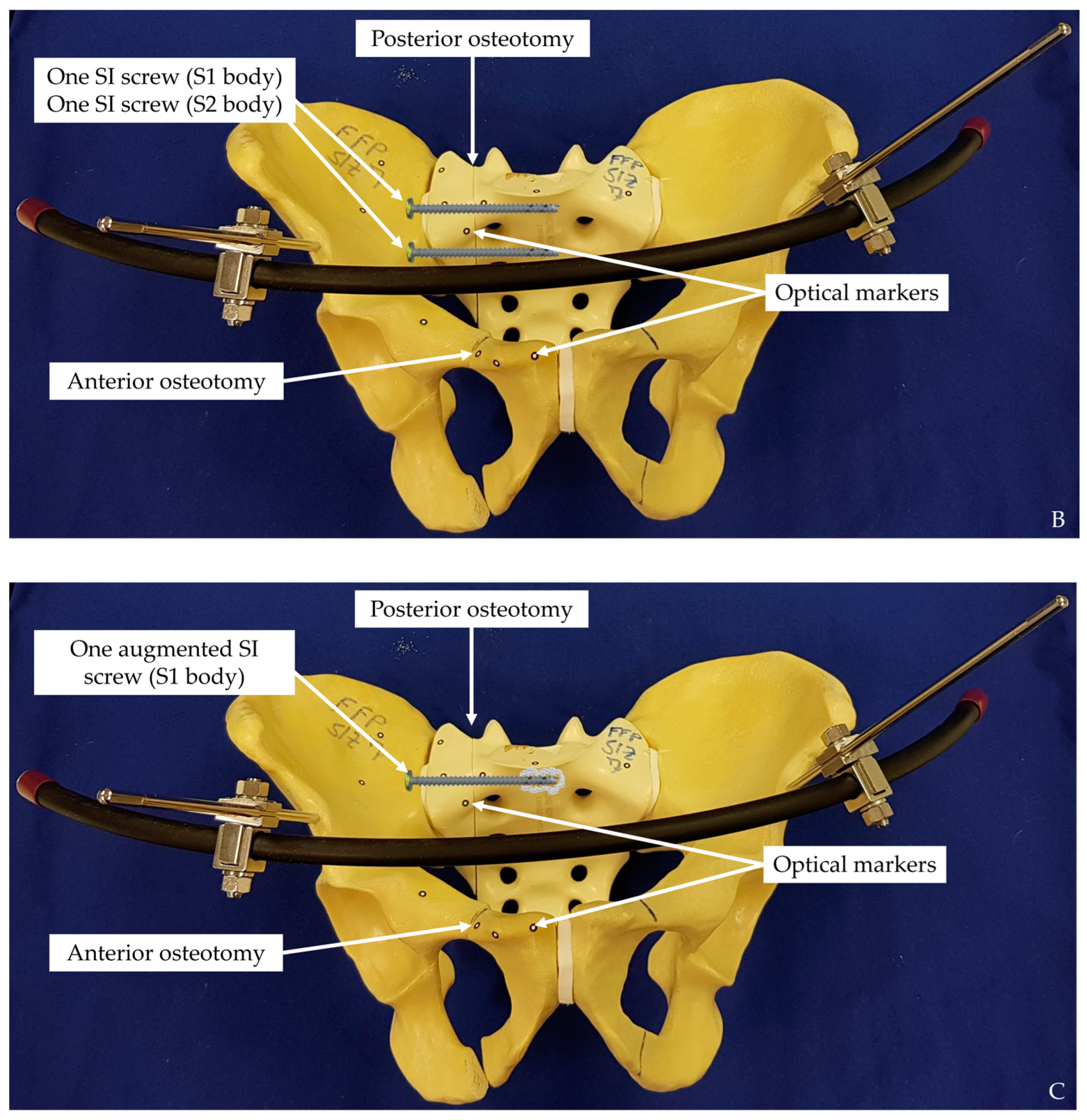
2. Materials and Methods
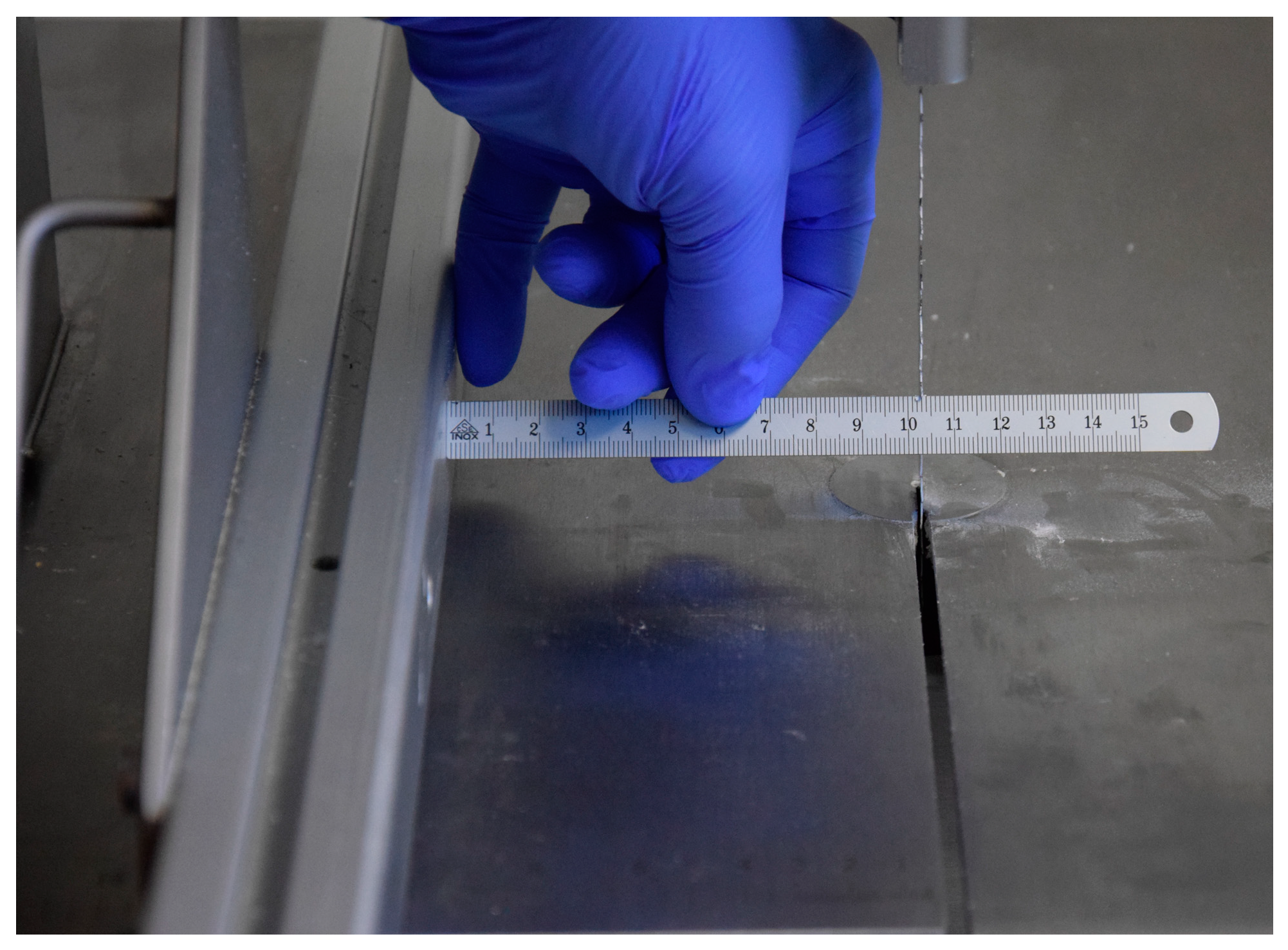
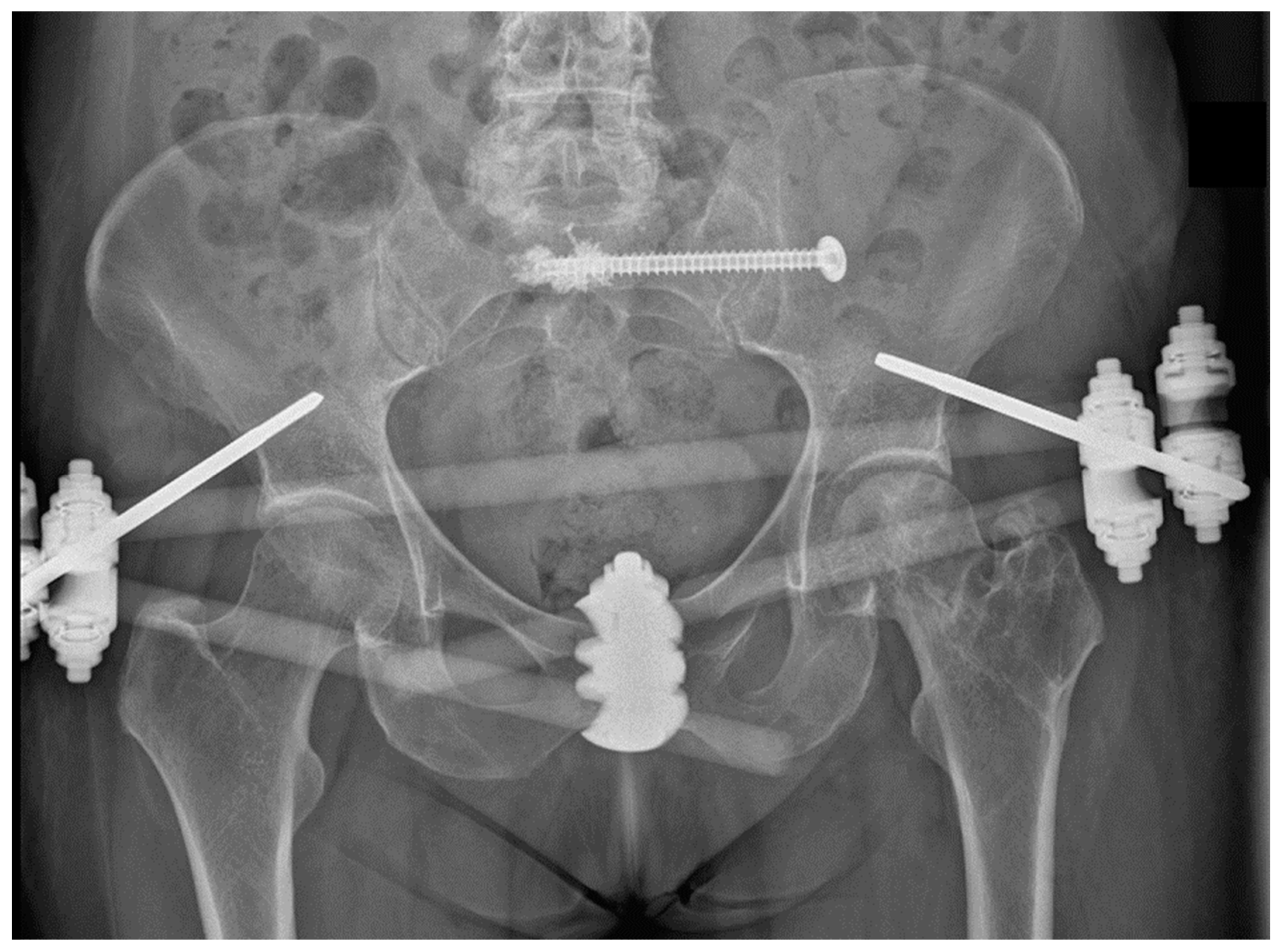
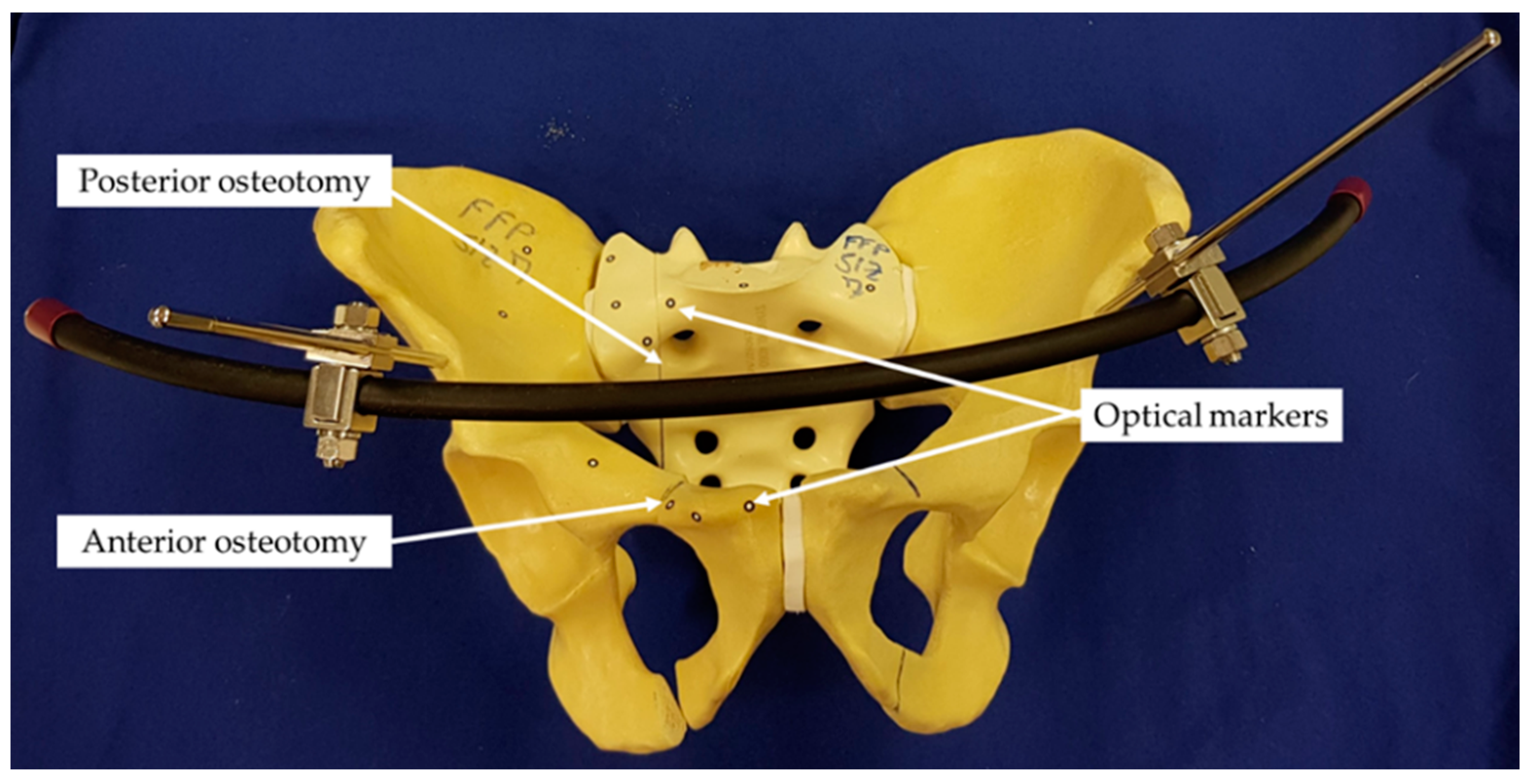
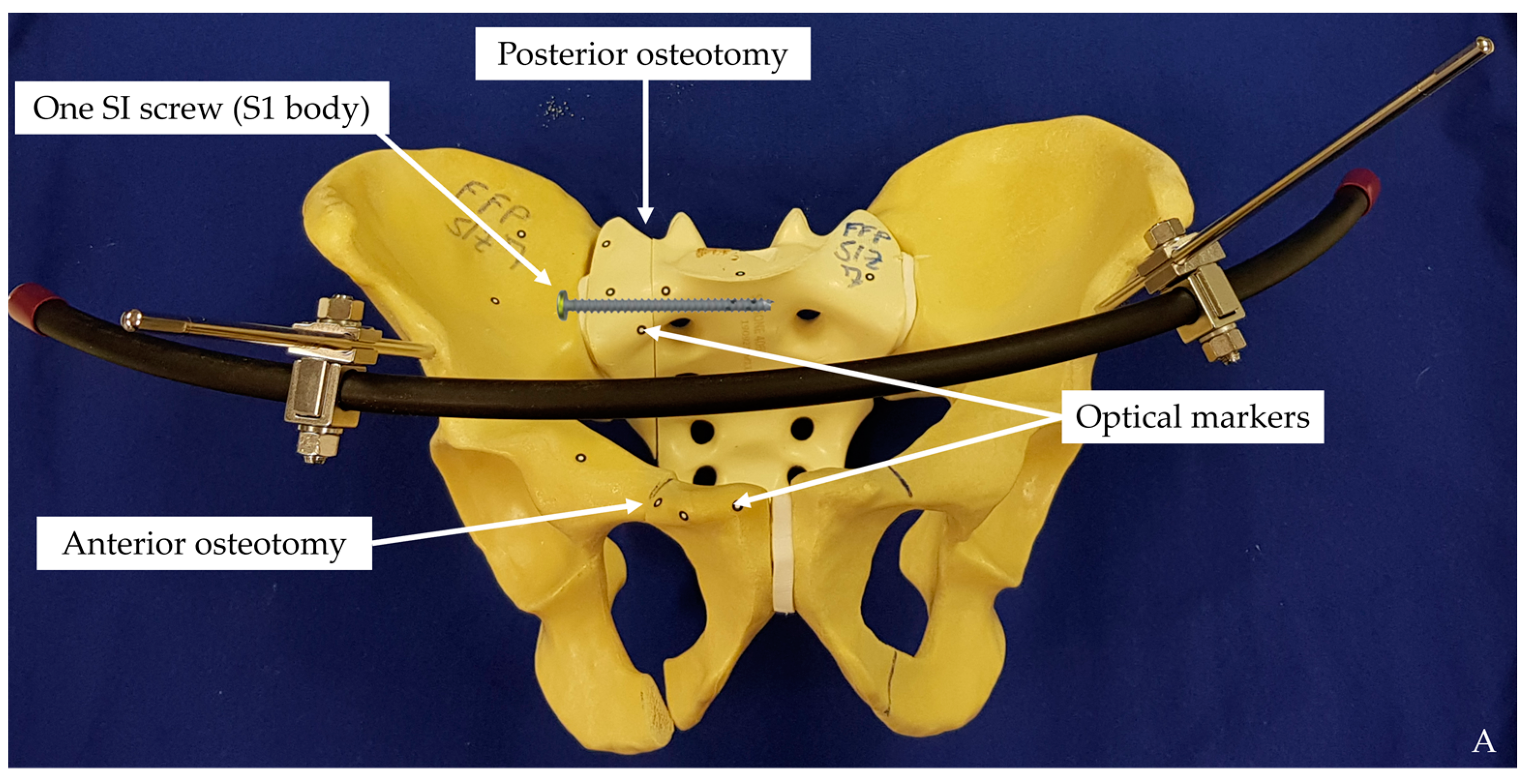
2.1. Biomechanical Testing
2.2. Data Acquisition and Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A



References
- Lodde, M.F.; Katthagen, J.C.; Riesenbeck, O.; Raschke, M.J.; Hartensuer, R. Trends in der operativen Therapie von Frakturen des Beckenrings: Eine bundesweite Analyse von OPS-Daten zwischen 2005 und 2017. Unfallchirurg 2020, 124, 373–381. [Google Scholar] [CrossRef] [PubMed]
- Keating, J.F.; Werier, J.; Blachut, P.; Broekhuyse, H.; Meek, R.N.; O’Brien, P.J. Early fixation of the vertically unstable pelvis: The role of iliosacral screw fixation of the posterior lesion. J. Orthop. Trauma 1999, 13, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Rommens, P.M.; Hofmann, A. Comprehensive classification of fragility fractures of the pelvic ring: Recommendations for surgical treatment. Injury 2013, 44, 1733–1744. [Google Scholar] [CrossRef]
- Letournel, E. Pelvic fractures. Injury 1979, 10, 145–148. [Google Scholar] [CrossRef]
- Letournel, E. Traitement chirurgical des traumatismes du bassin en dehors des fractures isolées du cotyle. Rev. Chir. Orthop. Reparatrice Appar. Mot. 1981, 67, 771–782. [Google Scholar]
- Andrich, S.; Haastert, B.; Neuhaus, E.; Neidert, K.; Arend, W.; Ohmann, C.; Grebe, J.; Vogt, A.; Jungbluth, P.; Thelen, S.; et al. Excess Mortality After Pelvic Fractures Among Older People. J. Bone Miner. Res. 2017, 32, 1789–1801. [Google Scholar] [CrossRef] [Green Version]
- Rommens, P.M.; Wagner, D.; Hofmann, A. Minimal Invasive Surgical Treatment of Fragility Fractures of the Pelvis. Chirurgia 2017, 112, 524–537. [Google Scholar] [CrossRef]
- Schmerwitz, I.U.; Jungebluth, P.; Lehmann, W.; Hockertz, T.J. Minimally invasive posterior locked compression plate osteosynthesis shows excellent results in elderly patients with fragility fractures of the pelvis. Eur. J. Trauma Emerg. Surg. 2021, 47, 37–45. [Google Scholar] [CrossRef]
- Hartensuer, R.; Lodde, M.F.; Keller, J.; Eveslage, M.; Stolberg-Stolberg, J.; Riesenbeck, O.; Raschke, M.J. Safety, Effect and Feasibility of Percutaneous SI-Screw with and without Augmentation-A 15-Year Retrospective Analysis on over 640 Screws. J. Clin. Med. 2020, 9, 2660. [Google Scholar] [CrossRef]
- Hartensuer, R.; Grüneweller, N.; Lodde, M.F.; Evers, J.; Riesenbeck, O.; Raschke, M. Die S2-Ala-Ilium-Schraube in der Beckentraumatologie. Z. Orthop. Unfall. 2020, 159, 522–532. [Google Scholar] [CrossRef]
- Osterhoff, G.; Ossendorf, C.; Wanner, G.A.; Simmen, H.-P.; Werner, C.M.L. Posterior screw fixation in rotationally unstable pelvic ring injuries. Injury 2011, 42, 992–996. [Google Scholar] [CrossRef] [PubMed]
- Eckardt, H.; Egger, A.; Hasler, R.M.; Zech, C.J.; Vach, W.; Suhm, N.; Morgenstern, M.; Saxer, F. Good functional outcome in patients suffering fragility fractures of the pelvis treated with percutaneous screw stabilisation: Assessment of complications and factors influencing failure. Injury 2017, 48, 2717–2723. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-W.; Oh, C.-W.; Oh, J.-K.; Kyung, H.-S.; Park, K.-H.; Yoon, S.-D.; Yoon, S.-H. The incidence of and factors affecting iliosacral screw loosening in pelvic ring injury. Arch. Orthop. Trauma Surg. 2016, 136, 921–927. [Google Scholar] [CrossRef]
- Wähnert, D.; Raschke, M.J.; Fuchs, T. Cement augmentation of the navigated iliosacral screw in the treatment of insufficiency fractures of the sacrum: A new method using modified implants. Int. Orthop. 2013, 37, 1147–1150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grüneweller, N.; Raschke, M.J.; Zderic, I.; Widmer, D.; Wähnert, D.; Gueorguiev, B.; Richards, R.G.; Fuchs, T.; Windolf, M. Biomechanical comparison of augmented versus non-augmented sacroiliac screws in a novel hemi-pelvis test model. J. Orthop. Res. 2017, 35, 1485–1493. [Google Scholar] [CrossRef]
- Osterhoff, G.; Dodd, A.E.; Unno, F.; Wong, A.; Amiri, S.; Lefaivre, K.A.; Guy, P. Cement Augmentation in Sacroiliac Screw Fixation Offers Modest Biomechanical Advantages in a Cadaver Model. Clin. Orthop. Relat. Res. 2016, 474, 2522–2530. [Google Scholar] [CrossRef] [Green Version]
- Moed, B.R.; Geer, B.L. S2 iliosacral screw fixation for disruptions of the posterior pelvic ring: A report of 49 cases. J. Orthop. Trauma 2006, 20, 378–383. [Google Scholar] [CrossRef] [PubMed]
- Osterhoff, G.; Ossendorf, C.; Wanner, G.A.; Simmen, H.-P.; Werner, C.M.L. Percutaneous iliosacral screw fixation in S1 and S2 for posterior pelvic ring injuries: Technique and perioperative complications. Arch. Orthop. Trauma Surg. 2011, 131, 809–813. [Google Scholar] [CrossRef] [Green Version]
- Mendel, T.; Noser, H.; Wohlrab, D.; Stock, K.; Radetzki, F. The lateral sacral triangle—A decision support for secure transverse sacroiliac screw insertion. Injury 2011, 42, 1164–1170. [Google Scholar] [CrossRef]
- Denis, F.; Davis, S.; Comfort, T. Sacral fractures: An important problem. Retrospective analysis of 236 cases. Clin. Orthop. Relat. Res. 1988, 227, 67–81. [Google Scholar] [CrossRef]
- Lodde, M.F.; Katthagen, J.C.; Schopper, C.O.; Zderic, I.; Richards, G.; Gueorguiev, B.; Raschke, M.J.; Hartensuer, R. Biomechanical Comparison of Five Fixation Techniques for Unstable Fragility Fractures of the Pelvic Ring. J. Clin. Med. 2021, 10, 2326. [Google Scholar] [CrossRef]
- Matta, J.M.; Tornetta, P. Internal fixation of unstable pelvic ring injuries. Clin. Orthop. Relat. Res. 1996, 129–140. [Google Scholar] [CrossRef]
- Routt, M.L.; Nork, S.E.; Mills, W.J. Percutaneous fixation of pelvic ring disruptions. Clin. Orthop. Relat. Res. 2000, 375, 15–29. [Google Scholar] [CrossRef] [PubMed]
- Zderic, I.; Wagner, D.; Schopper, C.; Lodde, M.; Richards, G.; Gueorguiev, B.; Rommens, P.; Acklin, Y.P. Screw-in-screw fixation of fragility sacrum fractures provides high stability without loosening-biomechanical evaluation of a new concept. J. Orthop. Res. 2020, 39, 761–770. [Google Scholar] [CrossRef]
- Shaw, J.A.; Mino, D.E.; Werner, F.W.; Murray, D.G. Posterior stabilization of pelvic fractures by use of threaded compression rods. Case reports and mechanical testing. Clin. Orthop. Relat. Res. 1985, 192, 240–254. [Google Scholar] [CrossRef]
- Oberkircher, L.; Masaeli, A.; Bliemel, C.; Debus, F.; Ruchholtz, S.; Krüger, A. Primary stability of three different iliosacral screw fixation techniques in osteoporotic cadaver specimens-a biomechanical investigation. Spine J. 2016, 16, 226–232. [Google Scholar] [CrossRef]
- Grechenig, S.; Gänsslen, A.; Gueorguiev, B.; Berner, A.; Müller, M.; Nerlich, M.; Schmitz, P. PMMA-augmented SI screw: A biomechanical analysis of stiffness and pull-out force in a matched paired human cadaveric model. Injury 2015, 46, S125–S128. [Google Scholar] [CrossRef]
- Van Zwienen, C.M.A.; van den Bosch, E.W.; Snijders, C.J.; Kleinrensink, G.J.; van Vugt, A.B. Biomechanical comparison of sacroiliac screw techniques for unstable pelvic ring fractures. J. Orthop. Trauma 2004, 18, 589–595. [Google Scholar] [CrossRef] [PubMed]
- Yinger, K.; Scalise, J.; Olson, S.A.; Bay, B.K.; Finkemeier, C.G. Biomechanical comparison of posterior pelvic ring fixation. J. Orthop. Trauma 2003, 17, 481–487. [Google Scholar] [CrossRef] [PubMed]
- Acklin, Y.P.; Zderic, I.; Richards, R.G.; Schmitz, P.; Gueorguiev, B.; Grechenig, S. Biomechanical investigation of four different fixation techniques in sacrum Denis type II fracture with low bone mineral density. J. Orthop. Res. 2018, 36, 1624–1629. [Google Scholar] [CrossRef]
- Cavalcanti Kußmaul, A.; Greiner, A.; Kammerlander, C.; Zeckey, C.; Woiczinski, M.; Thorwächter, C.; Gennen, C.; Kleber, C.; Böcker, W.; Becker, C.A. Biomechanical comparison of minimally invasive treatment options for Type C unstable fractures of the pelvic ring. Orthop. Traumatol. Surg. Res. 2020, 106, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Wagner, D.; Kamer, L.; Sawaguchi, T.; Noser, H.; Uesugi, M.; Baranowski, A.; Gruszka, D.; Rommens, P.M. Space available for trans-sacral implants to treat fractures of the pelvis assessed by virtual implant positioning. Arch. Orthop. Trauma Surg. 2019, 139, 1385–1391. [Google Scholar] [CrossRef]
- Griffin, D.R.; Starr, A.J.; Reinert, C.M.; Jones, A.L.; Whitlock, S. Vertically unstable pelvic fractures fixed with percutaneous iliosacral screws: Does posterior injury pattern predict fixation failure? J. Orthop. Trauma 2006, 20, S30–S36, discussion S36. [Google Scholar] [CrossRef] [PubMed]
- Elfar, J.; Menorca, R.M.G.; Reed, J.D.; Stanbury, S. Composite bone models in orthopaedic surgery research and education. J. Am. Acad. Orthop. Surg. 2014, 22, 111–120. [Google Scholar] [CrossRef] [Green Version]
- O’Neill, F.; Condon, F.; McGloughlin, T.; Lenehan, B.; Coffey, C.; Walsh, M. Validity of synthetic bone as a substitute for osteoporotic cadaveric femoral heads in mechanical testing: A biomechanical study. Bone Jt. Res. 2012, 1, 50–55. [Google Scholar] [CrossRef]
- Wähnert, D.; Hoffmeier, K.L.; Klos, K.; Stolarczyk, Y.; Fröber, R.; Hofmann, G.O.; Mückley, T. Biomechanical characterization of an osteoporotic artificial bone model for the distal femur. J. Biomater. Appl. 2012, 26, 565–579. [Google Scholar] [CrossRef]
- Reed, J.D.; Stanbury, S.J.; Menorca, R.M.; Elfar, J.C. The emerging utility of composite bone models in biomechanical studies of the hand and upper extremity. J. Hand Surg. Am. 2013, 38, 583–587. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tabaie, S.A.; Bledsoe, J.G.; Moed, B.R. Biomechanical comparison of standard iliosacral screw fixation to transsacral locked screw fixation in a type C zone II pelvic fracture model. J. Orthop. Trauma 2013, 27, 521–526. [Google Scholar] [CrossRef]
- Pohlemann, T.; Culemann, U.; Tscherne, H. Vergleichende biomechanische Untersuchungen zur internen Stabilisierung der transforaminalen Sakrumfraktur. Orthopade 1992, 21, 413–421. [Google Scholar] [PubMed]

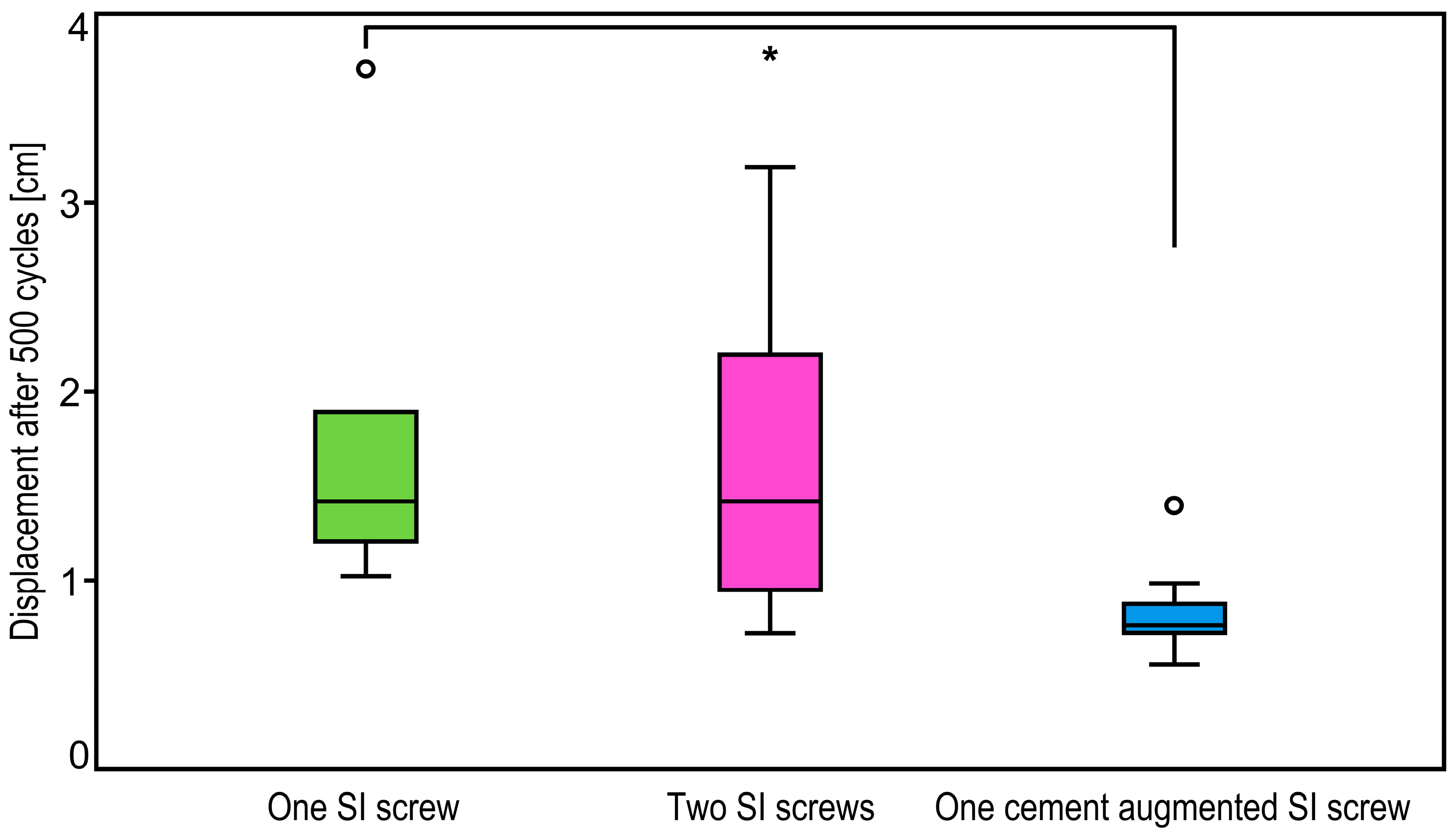
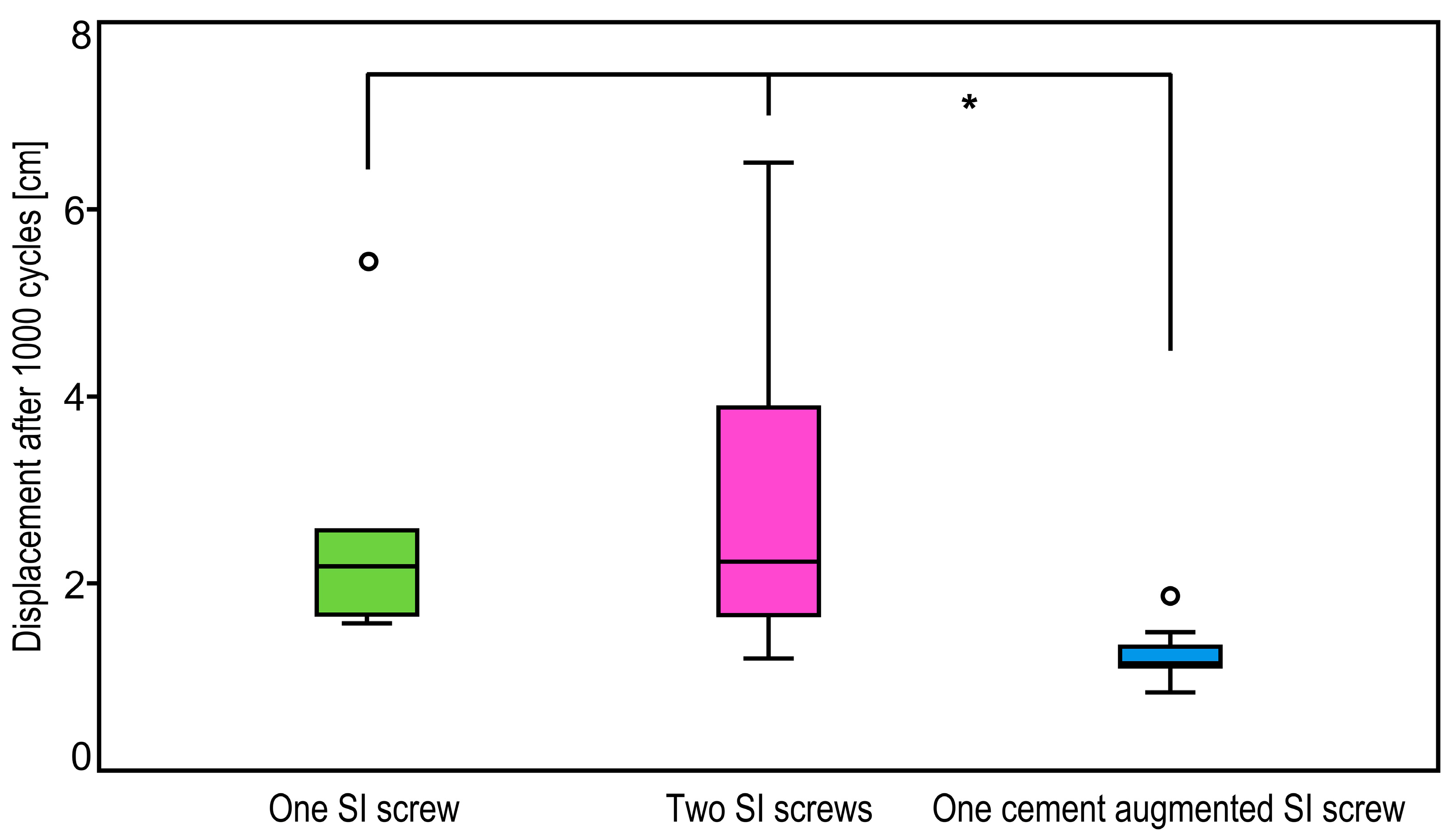
| Cycles | Pairwise Group Comparisons | p-Value |
|---|---|---|
| 500 | One SI screw vs. two SI screws | 0.99 |
| One SI screw vs. one cement augmented SI screw | 0.04 | |
| Two SI screws vs. one cement augmented SI screw | 0.08 | |
| 1000 | One SI screw vs. two SI screws | 0.99 |
| One SI screw vs. one cement augmented SI screw | 0.04 | |
| Two SI screws vs. one cement augmented SI screw | 0.02 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lodde, M.F.; Katthagen, J.C.; Schopper, C.O.; Zderic, I.; Richards, R.G.; Gueorguiev, B.; Raschke, M.J.; Hartensuer, R. Does Cement Augmentation of the Sacroiliac Screw Lead to Superior Biomechanical Results for Fixation of the Posterior Pelvic Ring? A Biomechanical Study. Medicina 2021, 57, 1368. https://doi.org/10.3390/medicina57121368
Lodde MF, Katthagen JC, Schopper CO, Zderic I, Richards RG, Gueorguiev B, Raschke MJ, Hartensuer R. Does Cement Augmentation of the Sacroiliac Screw Lead to Superior Biomechanical Results for Fixation of the Posterior Pelvic Ring? A Biomechanical Study. Medicina. 2021; 57(12):1368. https://doi.org/10.3390/medicina57121368
Chicago/Turabian StyleLodde, Moritz F., J. Christoph Katthagen, Clemens O. Schopper, Ivan Zderic, R. Geoff Richards, Boyko Gueorguiev, Michael J. Raschke, and René Hartensuer. 2021. "Does Cement Augmentation of the Sacroiliac Screw Lead to Superior Biomechanical Results for Fixation of the Posterior Pelvic Ring? A Biomechanical Study" Medicina 57, no. 12: 1368. https://doi.org/10.3390/medicina57121368
APA StyleLodde, M. F., Katthagen, J. C., Schopper, C. O., Zderic, I., Richards, R. G., Gueorguiev, B., Raschke, M. J., & Hartensuer, R. (2021). Does Cement Augmentation of the Sacroiliac Screw Lead to Superior Biomechanical Results for Fixation of the Posterior Pelvic Ring? A Biomechanical Study. Medicina, 57(12), 1368. https://doi.org/10.3390/medicina57121368









