Prediction of Judkins Left Catheter Size during Left Transradial Coronary Angiography by Simple Chest Radiographic and Echocardiographic Index
Abstract
:1. Introduction
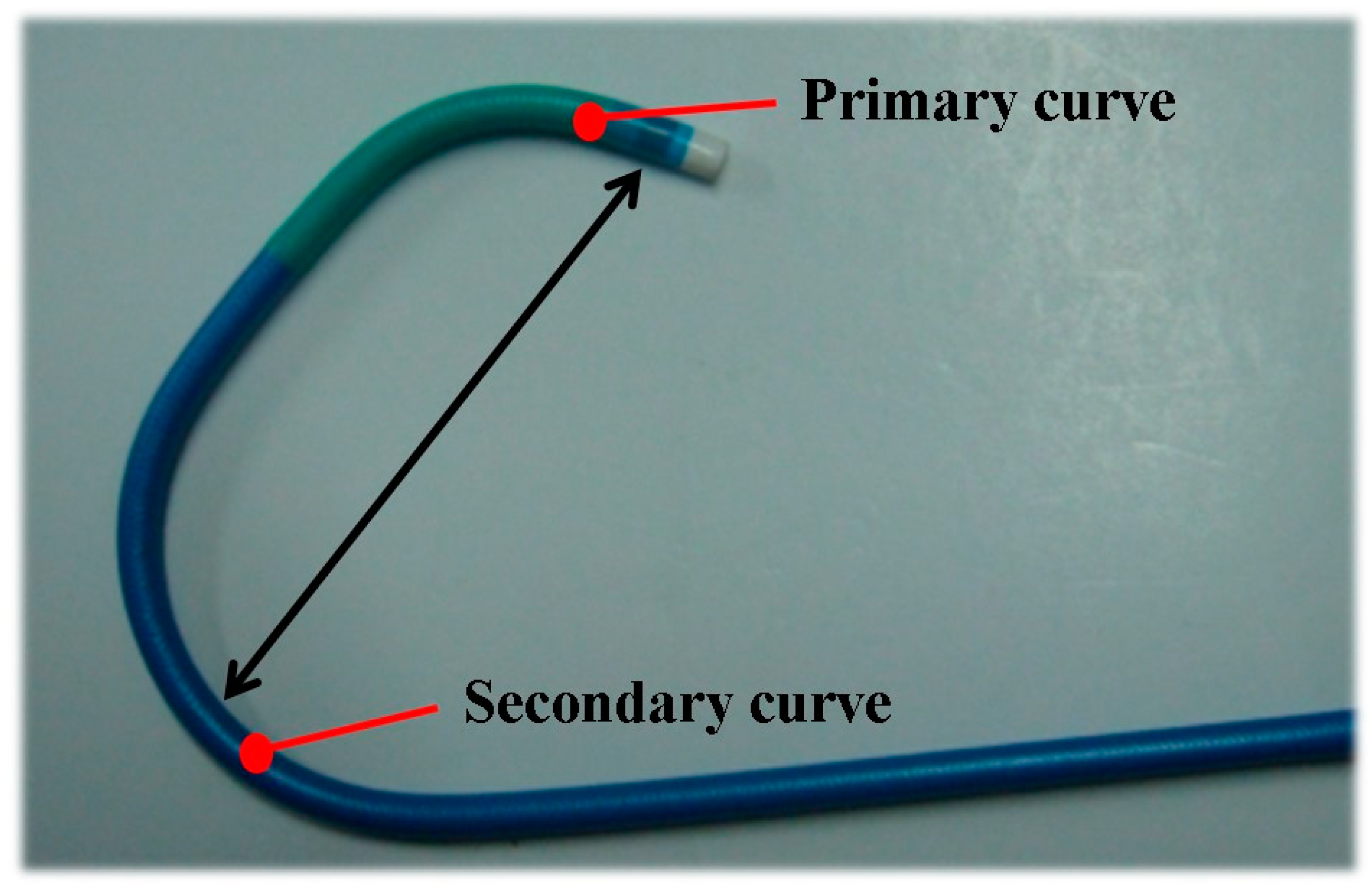
2. Methods
2.1. Study Population
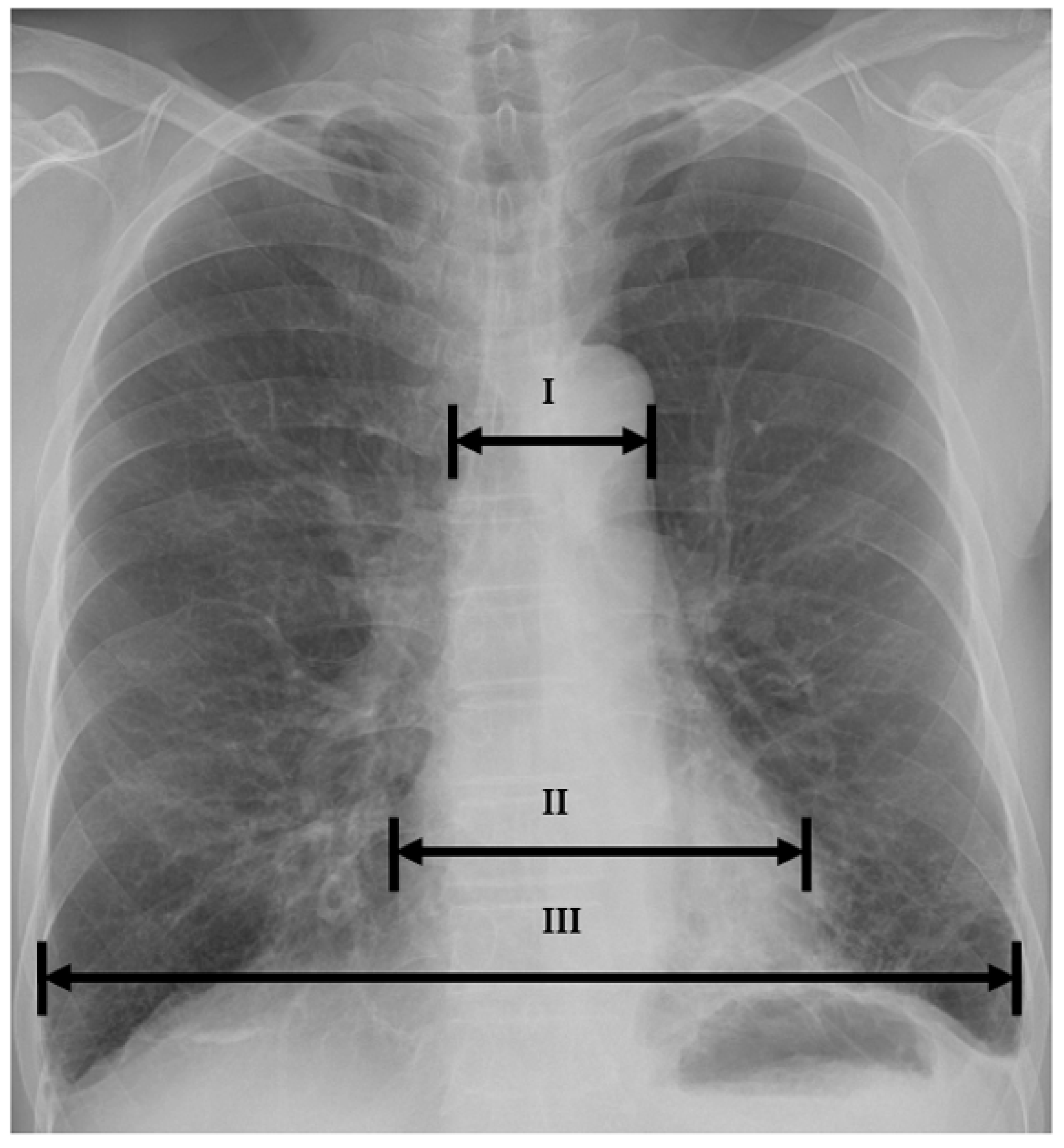
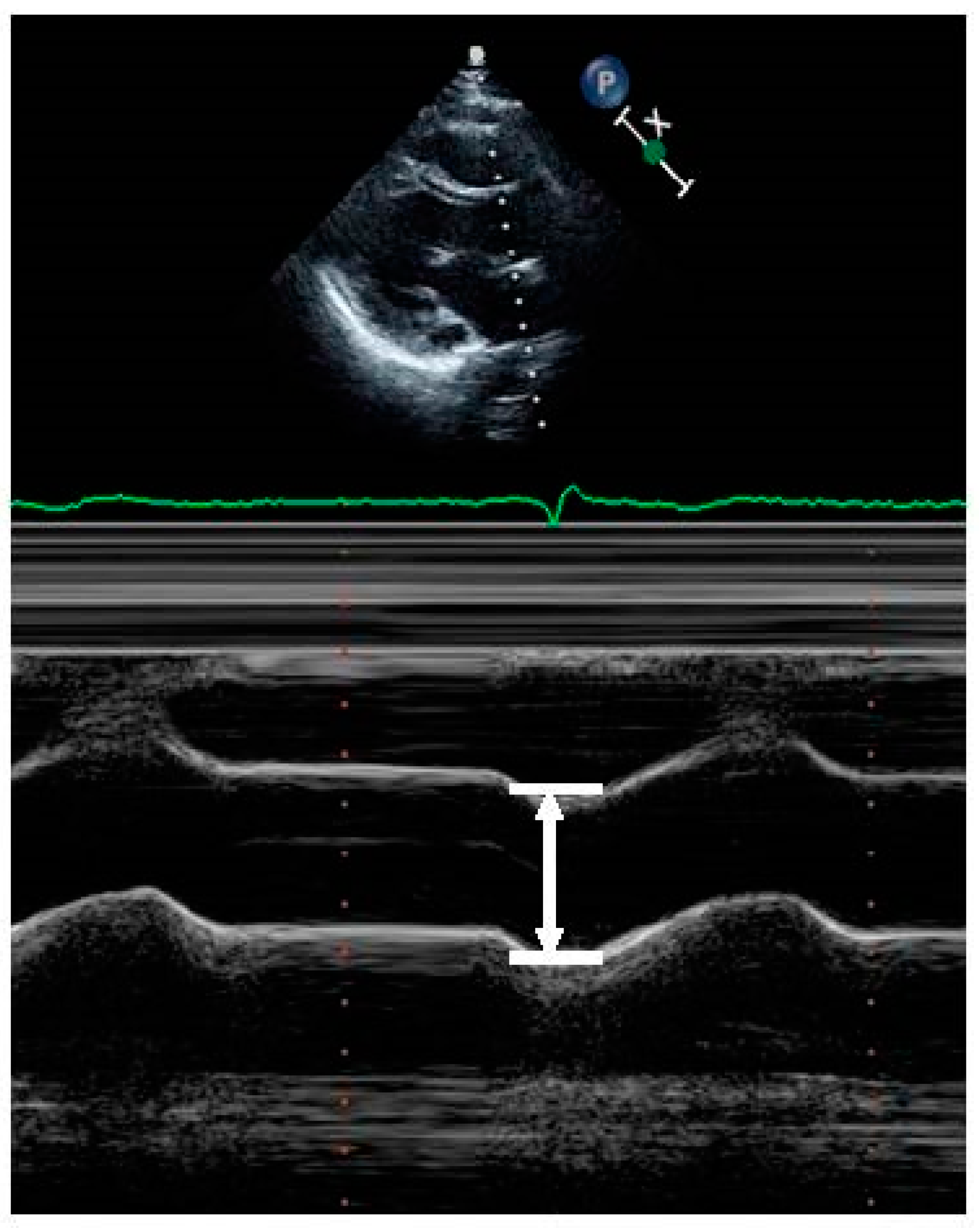
2.2. Data Collection
2.3. Statistical Analysis
2.4. Data Availability
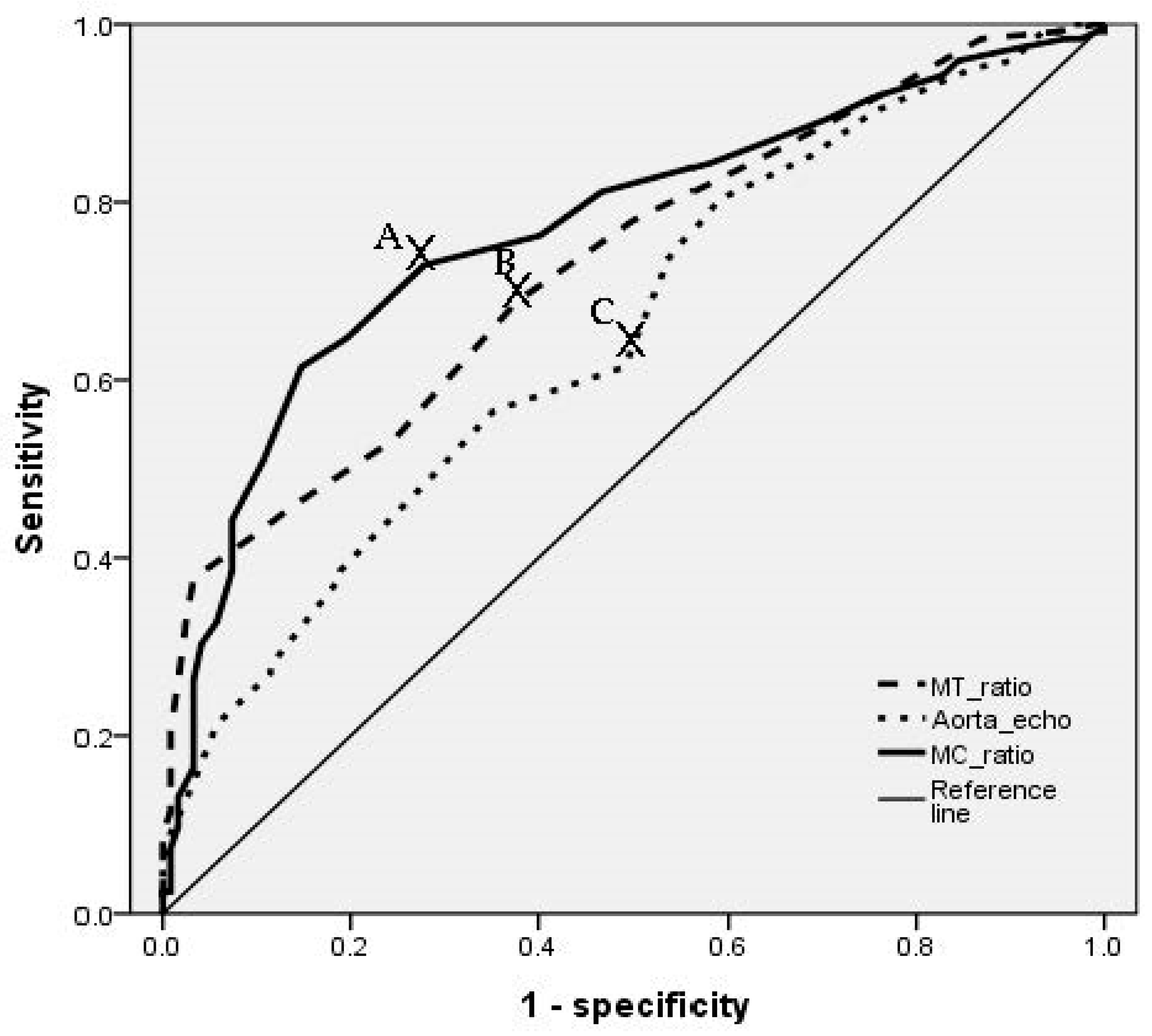
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Oudkerk, M.; Baert, A.L. Coronary Radiology, 2nd Revised ed.; 2009 edition; Springer: Berlin/Heidelberg, Germany, 2009; pp. 26–27. [Google Scholar]
- Badgett, R.G.; Mulrow, C.D.; Otto, P.M.; Ramírez, G. How well can the chest radiograph diagnose left ventricular dysfunction? J. Gen. Intern. Med. 1996, 11, 625–634. [Google Scholar] [CrossRef] [PubMed]
- Marnocha, K.; Maglinte, D.; Woods, J.; Goodman, M.; Peterson, P. Mediastinal-width/chest-width ratio in blunt chest trauma: A reappraisal. Am. J. Roentgenol. 1984, 142, 275–277. [Google Scholar] [CrossRef] [PubMed]
- Roman, M.J.; Devereux, R.B.; Kramer-Fox, R.; O’Loughlin, J. Two-dimensional echocardiographic aortic root dimensions in normal children and adults. Am. J. Cardiol. 1989, 64, 507–512. [Google Scholar] [CrossRef]
- Campeau, L. Percutaneous radial artery approach for coronary angiography. Catheter. Cardiovasc. Diagn. 1989, 16, 3–7. [Google Scholar] [CrossRef] [PubMed]
- Kiemeneij, F.; Jan Laarman, G. Percutaneous transradial artery approach for coronary stent implantation. Catheter. Cardiovasc. Diagn. 1993, 30, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Choussat, R.; Black, A.; Bossi, I.; Fajadet, J.; Marco, J. Vascular complications and clinical outcome after coronary angioplasty with platelet IIb/IIIa receptor blockade. Comparison of transradial vs transfemoral arterial access. Eur. Heart J. 2000, 21, 662–667. [Google Scholar] [CrossRef] [PubMed]
- Agostoni, P.; Biondi-Zoccai, G.G.; De Benedictis, M.L. Radial versus femoral approach for percutaneous coronary diagnostic and interventional proceduresSystematic overview and meta-analysis of randomized trials. J. Am. Coll. Cardiol. 2004, 44, 349–356. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, E.H.; Kim, M.H.; Park, T.H. Feasibility of Transradial Coronary Angiography Using a Single Judkins Left Catheter. Korean Circ. J. 2005, 35, 253–257. [Google Scholar] [CrossRef] [Green Version]
- Judkins, M. Coronary Arteriography and Left Ventriculography: Judkins Technique; King, S.B., III, Douglas, J.S., Jr., Eds.; Coronary arteriography and angioplasty New York; McGraw-Hill Book Company: New York, NY, USA, 1985; pp. 182–238. [Google Scholar]
- Lai, V.; Tsang, W.K.; Chan, W.C.; Yeung, T.W. Diagnostic accuracy of mediastinal width measurement on posteroanterior and anteroposterior chest radiographs in the depiction of acute nontraumatic thoracic aortic dissection. Emerg. Radiol. 2012, 19, 309–315. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gundry, S.R.; Burney, R.E.; Mackenzie, J.R. Assessment of mediastinal widening associated with traumatic rupture of the aorta. J. Trauma 1983, 23, 293–299. [Google Scholar] [CrossRef] [PubMed]
| Switched Group (n = 122) | Control Group (n = 122) | p Value | |
|---|---|---|---|
| Age | 64.84 ± 9.4 | 64.45 ± 7.9 | 0.726 |
| Male | 102 (83.6%) | 101(82.8%) | >0.99 |
| Height (cm) | 161.9 ± 9.4 | 160.5 ± 13.1 | 0.182 |
| Weight (kg) | 64.6 ± 14.8 | 65.1 ± 11.5 | 0.769 |
| Hypertension | 100 (82.0%) | 86 (70.5%) | 0.050 |
| Diabetes mellitus | 56 (57.7%) | 41 (42.3%) | 0.067 |
| Dyslipidemia | 56 (52.3%) | 51 (47.7%) | 0.606 |
| Parameters | Switched Group (n = 122) | Control Group (n = 122) | p Value | |
|---|---|---|---|---|
| I | Cardio-thoracic ratio | 0.51 ± 0.08 | 0.51 ± 0.06 | 0.064 |
| Mediastinal-thoracic ratio | 0.27 ± 0.05 | 0.23 ± 0.03 | <0.001 | |
| Mediastinal-cardiac ratio | 0.50 ± 0.08 | 0.45 ± 0.05 | <0.001 | |
| II | Aortic root diameter (mm) | 34.94 ± 4.18 | 32.66 ± 3.99 | <0.001 |
| Value | SN | SP | AUC (95% CI) | OR (95% CI) | |
|---|---|---|---|---|---|
| Mediastinal-thoracic ratio | 0.23 | 0.689 | 0.562 | 0.730 (0.667–0.792) | 1.91 (1.040–3.480) |
| Mediastinal-cardiac ratio | 0.47 | 0.734 | 0.566 | 0.769(0.708–0.829) | 5.61(2.853–11.104) |
| Aortic root (mm) | 34 | 0.591 | 0.578 | 0.652 (0.583–0.720) | 2.24 (1.290–4.112) |
| Adjusted Odds Ratio (95% Confidence Interval) | p Value | |
|---|---|---|
| Mediastinal-cardiac ratio | 5.197 (2.608–10.355) | <0.001 |
| Mediastinal-thoracic ratio | 1.839 (0.967–3.497) | 0.063 |
| Aortic root (mm) | 2.115 (1.144–3.912) | 0.017 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, S.-S.; Park, B.-W.; Bang, D.-W.; Lee, M.-H.; Hyon, M.-S.; Lee, S.-S. Prediction of Judkins Left Catheter Size during Left Transradial Coronary Angiography by Simple Chest Radiographic and Echocardiographic Index. Medicina 2021, 57, 1124. https://doi.org/10.3390/medicina57101124
Kwon S-S, Park B-W, Bang D-W, Lee M-H, Hyon M-S, Lee S-S. Prediction of Judkins Left Catheter Size during Left Transradial Coronary Angiography by Simple Chest Radiographic and Echocardiographic Index. Medicina. 2021; 57(10):1124. https://doi.org/10.3390/medicina57101124
Chicago/Turabian StyleKwon, Seong-Soon, Byoung-Won Park, Duk-Won Bang, Min-Ho Lee, Min-Su Hyon, and Seong-Soo Lee. 2021. "Prediction of Judkins Left Catheter Size during Left Transradial Coronary Angiography by Simple Chest Radiographic and Echocardiographic Index" Medicina 57, no. 10: 1124. https://doi.org/10.3390/medicina57101124
APA StyleKwon, S.-S., Park, B.-W., Bang, D.-W., Lee, M.-H., Hyon, M.-S., & Lee, S.-S. (2021). Prediction of Judkins Left Catheter Size during Left Transradial Coronary Angiography by Simple Chest Radiographic and Echocardiographic Index. Medicina, 57(10), 1124. https://doi.org/10.3390/medicina57101124






