The Role of Hyaluronic Acid in Sport-Related Tendinopathies: A Narrative Review
Abstract
1. Introduction
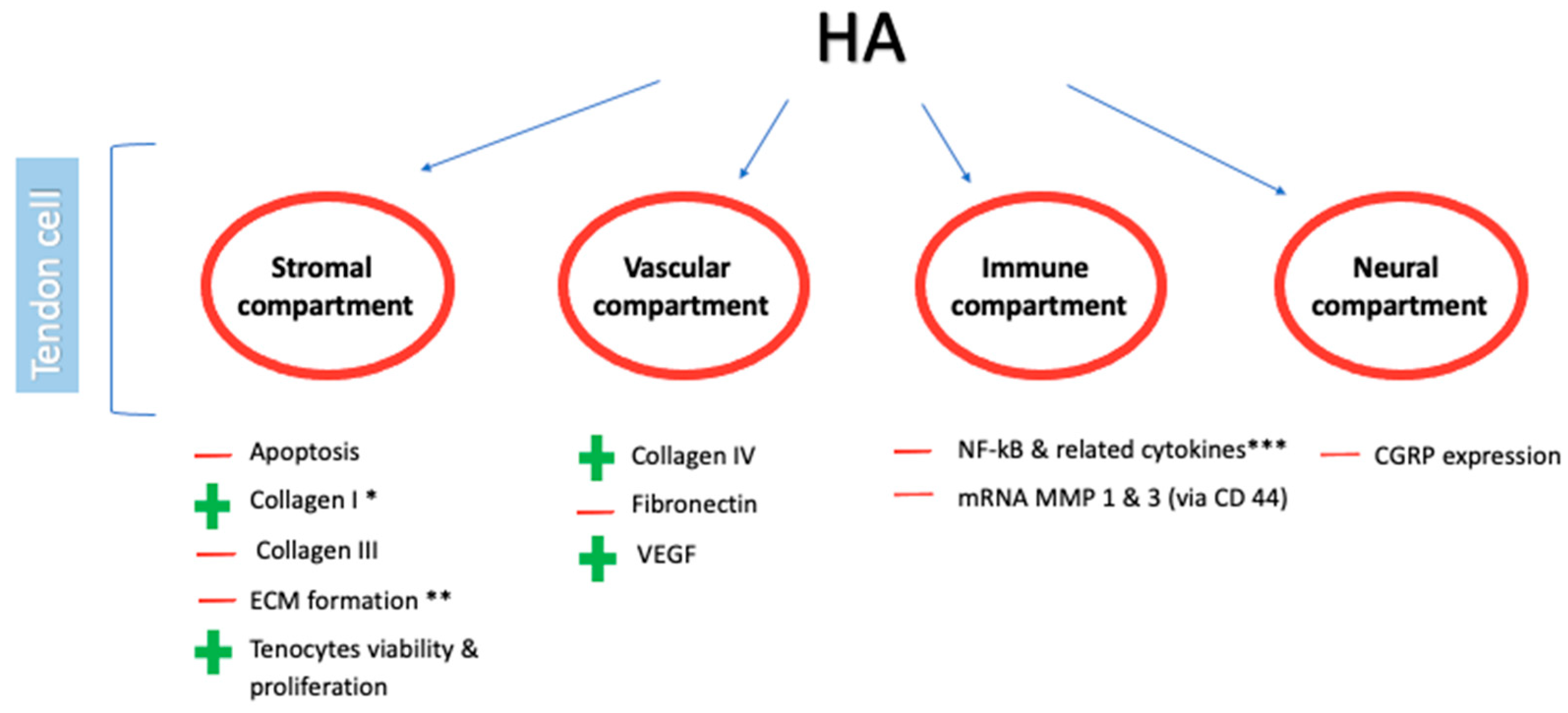
2. The Rationale of HA Use in the Management of Tendinopathies
2.1. Preclinical Studies
2.2. Clinical Studies
3. Clinical Implications of HA Injections in Sport-Related Tendinopathies
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Millar, N.L.; Silbernagel, K.G.; Thorborg, K.; Kirwan, P.D.; Galatz, L.M.; Abrams, G.D.; Murrell, G.A.C.; McInnes, I.B.; Rodeo, S.A. Tendinopathy. Nat. Rev. Dis. Primers 2021, 7, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Aicale, R.; Bisaccia, R.D.; Oliviero, A.; Oliva, F.; Maffulli, N. Current pharmacological approaches to the treatment of tendinopathy. Expert Opin. Pharmacother. 2020, 21, 1467–1477. [Google Scholar] [CrossRef] [PubMed]
- Macedo, C.S.; Tadiello, F.F.; Medeiros, L.T.; Antonelo, M.C.; Alves, M.A.; Mendonça, L.D. Physical therapy service delivered in the polyclinic during the Rio 2016 paralympic games. Phys. Ther. Sport 2019, 36, 62–67. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, C.; Fu, S.C.; Chua, E.; Hu, X.; Rolf, C.; Mattila, V.M.; Qin, L.; Yung, P.S.; Chan, K.M. Critical review on the socio-economic impact of tendinopathy. Asia-Pac. J. Sports Med. Arthrosc. Rehabil. Technol. 2016, 4, 9–20. [Google Scholar] [CrossRef]
- Ackermann, P.W.; Renström, P. Tendinopathy in sport. Sports Health 2012, 4, 193–201. [Google Scholar] [CrossRef]
- Gajhede-Knudsen, M.; Ekstrand, J.; Magnusson, H.; Maffulli, N. Recurrence of Achilles tendon injuries in elite male football players is more common after early return to play: An 11-year follow-up of the UEFA Champions League injury study. Br. J. Sports Med. 2013, 47, 763–768. [Google Scholar] [CrossRef]
- Lim, H.Y.; Wong, S.H. Effects of isometric, eccentric, or heavy slow resistance exercises on pain and function in individuals with patellar tendinopathy: A systematic review. Physiother. Res. Int. 2018, 23, e1721. [Google Scholar] [CrossRef]
- Beyer, R.; Kongsgaard, M.; Hougs Kjær, B.; Øhlenschlæger, T.; Kjær, M.; Magnusson, S.P. Heavy Slow Resistance Versus Eccentric Training as Treatment for Achilles Tendinopathy: A Randomized Controlled Trial. Am. J. Sports Med. 2015, 43, 1704–1711. [Google Scholar] [CrossRef]
- Dean, B.J.; Lostis, E.; Oakley, T.; Rombach, I.; Morrey, M.E.; Carr, A.J. The risks and benefits of glucocorticoid treatment for tendinopathy: A systematic review of the effects of local glucocorticoid on tendon. Semin. Arthritis Rheum. 2014, 43, 570–576. [Google Scholar] [CrossRef]
- Abate, M.; Salini, V.; Schiavone, C.; Andia, I. Clinical benefits and drawbacks of local corticosteroids injections in tendinopathies. Expert Opin. Drug Saf. 2017, 16, 341–349. [Google Scholar] [CrossRef]
- Nasiri, A.; Mohamadi Jahromi, L.S.; Vafaei, M.A.; Parvin, R.; Fakheri, M.S.; Sadeghi, S. Comparison of the Effectiveness of Ultrasound-Guided Prolotherapy in Supraspinatus Tendon with Ultrasound-Guided Corticosteroid Injection of Subacromial Subdeltoid Bursa in Rotator Cuff-Related Shoulder Pain: A Clinical Trial Study. Adv. Biomed. Res. 2021, 10, 12. [Google Scholar] [CrossRef]
- Lu, H.; Yang, H.; Shen, H.; Ye, G.; Lin, X.J. The clinical effect of tendon repair for tendon spontaneous rupture after corticosteroid injection in hands: A retrospective observational study. Medicine 2016, 95, e5145. [Google Scholar] [CrossRef] [PubMed]
- Petrella, R.J.; Cogliano, A.; Decaria, J.; Mohamed, N.; Lee, R. Management of Tennis Elbow with sodium hyaluronate periarticular injections. Sports Med. Arthrosc. Rehabil. Ther. Technol. 2010, 2, 4. [Google Scholar] [CrossRef] [PubMed]
- Muneta, T.; Koga, H.; Ju, Y.J.; Mochizuki, T.; Sekiya, I. Hyaluronan injection therapy for athletic patients with patellar tendinopathy. J. Orthop. Sci. 2012, 17, 425–431. [Google Scholar] [CrossRef] [PubMed]
- Fallacara, A.; Baldini, E.; Manfredini, S.; Vertuani, S. Hyaluronic Acid in the Third Millennium. Polymers 2018, 10, 701. [Google Scholar] [CrossRef]
- Pereira, H.; Sousa, D.A.; Cunha, A.; Andrade, R.; Espregueira-Mendes, J.; Oliveira, J.M.; Reis, R.L. Hyaluronic Acid. Adv. Exp. Med. Biol. 2018, 1059, 137–153. [Google Scholar] [CrossRef]
- Litwiniuk, M.; Krejner, A.; Speyrer, M.S.; Gauto, A.R.; Grzela, T. Hyaluronic Acid in Inflammation and Tissue Regeneration. Wounds 2016, 28, 78–88. [Google Scholar]
- Liu, L.; Liu, Y.; Li, J.; Du, G.; Chen, J. Microbial production of hyaluronic acid: Current state, challenges, and perspectives. Microb. Cell Fact. 2011, 10, 99. [Google Scholar] [CrossRef]
- Gupta, R.C.; Lall, R.; Srivastava, A.; Sinha, A. Hyaluronic Acid: Molecular Mechanisms and Therapeutic Trajectory. Front. Vet. Sci. 2019, 6, 192. [Google Scholar] [CrossRef]
- Neumann, A.; Schinzel, R.; Palm, D.; Riederer, P.; Münch, G. High molecular weight hyaluronic acid inhibits advanced glycation endproduct-induced NF-κB activation and cytokine expression. FEBS Lett. 1999, 453, 283–287. [Google Scholar] [CrossRef]
- Yamaguchi, T.; Ochiai, N.; Sasaki, Y.; Kijima, T.; Hashimoto, E.; Sasaki, Y.; Kenmoku, T.; Yamazaki, H.; Miyagi, M.; Ohtori, S.; et al. Efficacy of hyaluronic acid or steroid injections for the treatment of a rat model of rotator cuff injury. J. Orthop. Res. 2015, 33, 1861–1867. [Google Scholar] [CrossRef]
- Ozgenel, G.Y.; Etöz, A. Effects of repetitive injections of hyaluronic acid on peritendinous adhesions after flexor tendon repair: A preliminary randomized, placebo-controlled clinical trial. Ulus Travma Acil Cerrahi Derg 2012, 18, 11–17. [Google Scholar] [CrossRef]
- Halici, M.; Karaoglu, S.; Canoz, O.; Kabak, S.; Baktir, A. Sodium hyaluronate regulating angiogenesis during Achilles tendon healing. Knee Surg. Sports Traumatol. Arthrosc. 2004, 12, 562–567. [Google Scholar] [CrossRef]
- Akasaka, T.; Nishida, J.; Imaeda, T.; Shimamura, T.; Amadio, P.C.; An, K.N. Effect of hyaluronic acid on the excursion resistance of tendon graft: A biomechanical in vitro study in a modified human model. Clin. Biomech. 2006, 21, 810–815. [Google Scholar] [CrossRef] [PubMed]
- Nishida, J.; Araki, S.; Akasaka, T.; Toba, T.; Shimamura, T.; Amadio, P.C.; An, K.N. Effect of hyaluronic acid on the excursion resistance of tendon grafts. A biomechanical study in a canine model in vitro. J. Bone Joint Surg. Br. 2004, 86, 918–924. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Oryan, A.; Moshiri, A.; Meimandiparizi, A.H. Effects of sodium-hyaluronate and glucosamine-chondroitin sulfate on remodeling stage of tenotomized superficial digital flexor tendon in rabbits: A clinical, histopathological, ultrastructural, and biomechanical study. Connect Tissue Res. 2011, 52, 329–339. [Google Scholar] [CrossRef] [PubMed]
- Kurt, B.; Ozaydin, I.; Sozmen, M.; Bilge, A.; Cihan, M.; Hamamci, E.; Aydin, U. Hyaluronic acid and synovial fluid in preventing adhesion formation after tenorrhaphy: An in vivo study on rabbit Achilles tendon. Ciênc. Rural 2018, 48, 1–7. [Google Scholar] [CrossRef]
- Wu, P.T.; Kuo, L.C.; Su, F.C.; Chen, S.Y.; Hsu, T.I.; Li, C.Y.; Tsai, K.J.; Jou, I.M. High-molecular-weight hyaluronic acid attenuated matrix metalloproteinase-1 and -3 expression via CD44 in tendinopathy. Sci. Rep. 2017, 7, 40840. [Google Scholar] [CrossRef]
- Yoshida, M.; Funasaki, H.; Kubota, M.; Marumo, K. Therapeutic effects of high molecular weight hyaluronan injections for tendinopathy in a rat model. J. Orthop. Sci. 2015, 20, 186–195. [Google Scholar] [CrossRef] [PubMed]
- Gallorini, M.; Berardi, A.C.; Berardocco, M.; Gissi, C.; Maffulli, N.; Cataldi, A.; Oliva, F. Hyaluronic acid increases tendon derived cell viability and proliferation in vitro: Comparative study of two different hyaluronic acid preparations by molecular weight. Muscles Ligaments Tendons J. 2017, 7, 208–214. [Google Scholar] [CrossRef]
- Nakamura, H.; Gotoh, M.; Kanazawa, T.; Ohta, K.; Nakamura, K.; Honda, H.; Ohzono, H.; Shimokobe, H.; Mitsui, Y.; Shirachi, I.; et al. Effects of corticos-teroids and hyaluronic acid on torn rotator cuff tendons in vitro and in rats. J. Orthop. Res. 2015, 33, 1523–1530. [Google Scholar] [CrossRef] [PubMed]
- Chou, W.Y.; Ko, J.Y.; Wang, F.S.; Huang, C.C.; Wong, T.; Wang, C.J.; Chang, H.E. Effect of sodium hyaluronate treatment on rotator cuff lesions without complete tears: A randomized, double-blind, placebo-controlled study. J. Shoulder Elbow Surg. 2010, 19, 557–563. [Google Scholar] [CrossRef] [PubMed]
- Ozgen, M.; Fırat, S.; Sarsan, A.; Topuz, O.; Ardıç, F.; Baydemir, C. Short- and long-term results of clinical effectiveness of sodium hyaluronate injection in supraspinatus tendinitis. Rheumatol. Int. 2012, 32, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Moghtaderi, A.; Sajadiyeh, S.; Khosrawi, S.; Dehghan, F.; Bateni, V. Effect of subacromial sodium hyaluronate injection on rotator cuff disease: A double-blind placebo-controlled clinical trial. Adv. Biomed. Res. 2013, 2, 89. [Google Scholar] [CrossRef] [PubMed]
- Meloni, F.; Milia, F.; Cavazzuti, M.; Doria, C.; Lisai, P.; Profili, S.; Meloni, G.B. Clinical evaluation of sodium hyaluronate in the treatment of patients with sopraspinatus tendinosis under echographic guide: Experimental study of periarticular injections. Eur. J. Radiol. 2008, 68, 170–173. [Google Scholar] [CrossRef] [PubMed]
- Merolla, G.; Bianchi, P.; Porcellini, G. Ultrasound-guided subacromial injections of sodium hyaluronate for the management of rotator cuff tendinopathy: A prospective comparative study with rehabilitation therapy. Musculoskelet. Surg. 2013, 97, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Tosun, H.B.; Gümüştaş, S.A.; Kom, M.; Uludağ, A.; Serbest, S.; Eröksüz, Y. The Effect of Sodium Hyaluronate plus Sodium Chondroitin Sulfate Solution on Peritendinous Adhesion and Tendon Healing: An Experimental Study. Balkan Med. J. 2016, 33, 258–266. [Google Scholar] [CrossRef]
- Taşkesen, A.; Ataoğlu, B.; Özer, M.; Demirkale, İ.; Turanli, S. Glucosamine-chondroitin sulphate accelerates tendon-to-bone healing in rabbits. Eklem Hastalik Cerrahisi 2015, 26, 77–83. [Google Scholar] [CrossRef]
- Tosun, H.B.; Gumustas, S.; Agir, I.; Uludag, A.; Serbest, S.; Pepele, D.; Ertem, K. Comparison of the effects of sodium hyaluronate-chondroitin sulphate and corticosteroid in the treatment of lateral epicondylitis: A prospective randomized trial. J. Orthop. Sci. 2015, 20, 837–843. [Google Scholar] [CrossRef]
- Lynen, N.; De Vroey, T.; Spiegel, I.; Van Ongeval, F.; Hendrickx, N.J.; Stassijns, G. Comparison of Peritendinous Hyaluronan Injections Versus Extracorporeal Shock Wave Therapy in the Treatment of Painful Achilles’ Tendinopathy: A Randomized Clinical Efficacy and Safety Study. Arch. Phys. Med. Rehabil. 2017, 98, 64–71. [Google Scholar] [CrossRef]
- Gervasi, M.; Barbieri, E.; Capparucci, I.; Annibalini, G.; Sisti, D.; Amatori, S.; Carrabs, V.; Valli, G.; Donati Zeppa, S.; Rocchi, M.B.L.; et al. Treatment of Achilles Tendinopathy in Recreational Runners with Peritendinous Hyaluronic Acid Injections: A Viscoelastometric, Functional, and Biochemical Pilot Study. J. Clin. Med. 2021, 10, 1397. [Google Scholar] [CrossRef]
- Scott, A.; Ashe, M.C. Common tendinopathies in the upper and lower extremities. Curr. Sports Med. Rep. 2006, 5, 233–241. [Google Scholar] [CrossRef]
- Alfredson, H.; Cook, J. A treatment algorithm for managing Achilles tendinopathy: New treatment options. Br. J. Sports Med. 2007, 41, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Ardern, C.L.; Glasgow, P.; Schneiders, A.; Witvrouw, E.; Clarsen, B.; Cools, A.; Gojanovic, B.; Griffin, S.; Khan, K.M.; Moksnes, H.; et al. 2016 Consensus statement on return to sport from the First World Congress in Sports Physical Therapy, Bern. Br. J. Sports Med. 2016, 50, 853–864. [Google Scholar] [CrossRef] [PubMed]
- Habets, B.; van den Broek, A.G.; Huisstede, B.M.A.; Backx, F.J.G.; van Cingel, R.E.H. Return to Sport in Athletes with Midportion Achilles Tendinopathy: A Qualitative Systematic Review Regarding Definitions and Criteria. Sports Med. 2018, 48, 705–723. [Google Scholar] [CrossRef] [PubMed]
| Author, Year | Study Design | Disease | Sample Size: Total; Group | Intervention | Outcome | Follow-Up | Main Results |
|---|---|---|---|---|---|---|---|
| Meloni, 2008 | Open-labeled prospective study | Supraspinatus tendinosis | 56 patients; LMW HA (28) Saline (28) | LMW HA group: 20 mg of LMW HA, with 2 mL of 1% lidocaine and 2 mL of 0.9% sodium chloride solution. Saline group: 4 mL of 0.9% sodium chloride solution, with 2 mL of 1% lidocaine. Timing: Both groups received 5 injections over the superior tendon surface (1-week interval) | Shoulder disability, ROM, VAS | 1, 3, 6, 12 months | In the LMW HA group, shoulder disability and pain improved for 25/28 patients at 1 and 3 months follow-up, 19/28 at 6 and 12 months follow-up; in the Saline group, shoulder disability and pain improved for 0/28 patients. In both groups ROM degrees were unchanged. |
| Petrella, 2010 | Prospective randomized clinical trial | Lateral epicondylitis | 331 racquet sport athletes; HA (165) Saline (166) | HA group: 1.2 mL HA (1% HA in a phosphate buffered saline contained in a prefilled syringe); Saline group: 1.2 mL saline placebo. Timing: Both groups received 2 injections into the subcutaneous tissue and muscle 1 cm from the lateral epicondyle (1-week interval) | VAS-pain at rest and after grip testing | 14, 30, 90, 356 days | In the HA group, VAS-pain at rest and after grip testing were significantly better compared to Saline group from day 30 to each follow-up. |
| Muneta, 2012 | Retrospective study | Patellar tendinopathy | 50 athletes | 25 mg of hyaluronan (molecular weight 900,000 Da) in 2.5 mL (superpurified hyaluronate, Seikagaku Kogyo Co. Ltd., Tokyo, Japan) at the proximal interface between the posterior surface of the patellar tendon and the infrapatellar fat pad | Effectiveness *, safety | 25.7 months | From January 1999 to December 2006, 135 injections were performed with an average of 2 injections per case. 54% of the participants return to full athletic activities, while 40% were able to continue to participate in previous sporting activities. The rate of side effects from HA has been reported to be as low as 0.57% |
| Merolla, 2013 | Prospective non-randomized comparative study | RC tendinopathy | 48 patients; LMW HA (25) Physiotherapy (23) | LMW HA group: 12 mg/1.2 mL of STABHATM (Soft Tissue Adapted Biocompatible Hyaluronic Acid; SportVisTM, MDT Int’l SA, Switzerland) Physiotherapy group: active shoulder mobilization, soft tissue stretching and humeral head positioner and propeller muscles strengthening. Timing: LMW HA group received 2 injections over the superior tendon surface (2-week interval); physiotherapy group underwent 30 days of rehabilitation (3 sessions every week). | VAS, OSS, CMS, PGA | 2, 4, 12, 24 weeks | In the LMW HA group, a statistically significant reduction of pain and improvement of both CMS and OSS were found from baseline to the week 2, 4, and 12 (p < 0.05); in the Physiotherapy group, a statistically significant reduction of pain and improvement of both CMS and OSS were found at week 2 (p < 0.05) but not at week 4, 12 and 24 (p > 0.05). PGA scores showed good patient compliance with no serious adverse events registered. |
| Tosun, 2015 | Prospective randomized clinical trial | Lateral epicondylitis | 57 patients; HA + CS (25) Triamcinolone (32) | HA + CS group: 1 mL of an HA + CS combination (800 mg hyaluronate combined with 1 g chondroitin sulfate/50 mL; Ialuril, IBSA Farmaceutici Italia S.r.l, Italy) + 0.6 mL of prilocaine HCl (Citanest, AstraZeneca PLC, London, UK). Triamcinolone group: 1 mL of triamcinolone acetonide (40 mg/mL; Kenacort-A Retard, Bristol Meyers Squibb Pharmaceuticals, New York, NY, USA) + 0.6 mL of prilocaine HCl (Citanest). Timing: Both groups received one injection over an area under the external origin, immediately anterior and distal to the lateral epicondyle | PRTEE questionnaire and MCID and percentage changes in the PRTEE | 3, 6 months | Both groups improved mean pain and function scores at 3 and 6 months. HA + CS group showed a statistically significantly better mean function score and mean pain and function scores at 3 and 6 months, respectively, compared to triamcinolone group. HA + CS group showed clinically significant improvements at 3 and 6 months compared with triamcinolone group. |
| Lynen, 2016 | Multinational, prospective, randomized controlled, blinded-observer trial. | Achilles’ tendinopathy | 59 patients; HA (29) ESWT (30) | HA group: 40 mg/2 mL + 10 mg mannitol, OSTENIL® TENDONa ESWT group: piezo-electric ESWT device (PiezoSon 100 plusb) with standardized parameters (10 mm penetration depth, 94°aperture angle, 4 Hz pulse frequency, 1500 pulses per application) with an intensity levels set to 14 and 15 Timing: HA group received 2 injections peritendinously at the midportion of Achilles’ tendon (1-week interval); ESWT group: 3 sessions at weekly intervals. | VAS, VISA-A, safety | 1, 2 **, 4 ***, 12 ***, 24 *** weeks | In the HA group, percent change in pain (VAS) and VISA-A scores were statistically significant at 1, 3, 6 months compared to ESWT. No serious adverse events was reported. |
| Gervasi, 2021 | Pilot study | Achilles’ tendinopathy | 8 male runners | Three injections of 2–1000 kDa HA in 2 mL, (RegenFlex T&M, Regenyal Laboratories SRL, Italy), one each 15-day | Pain (Likert-scale 0–5), biochemical markers, MVIC, viscoelastic properties such as tone [frequency of oscillation (Hz)] and siffness) through handheld myotonometer, safety | 0, 15, 30, 45 days | Pain, MVIC, tone, and stiffness were significantly different between healthy and injured tendon during all over time. A reduction of IL1-β and MMP-3 level and pain plus an amelioration of tone, stiffness and MVIC was reached in the injured tendon among the visits. No adverse event was reported. |
| level of pain |
| level of functional recovery |
| muscular strength |
| range of motion |
| endurance |
| medical advice |
| psychosocial factors |
| anatomical/physiological properties |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Crimaldi, S.; Liguori, S.; Tamburrino, P.; Moretti, A.; Paoletta, M.; Toro, G.; Iolascon, G. The Role of Hyaluronic Acid in Sport-Related Tendinopathies: A Narrative Review. Medicina 2021, 57, 1088. https://doi.org/10.3390/medicina57101088
Crimaldi S, Liguori S, Tamburrino P, Moretti A, Paoletta M, Toro G, Iolascon G. The Role of Hyaluronic Acid in Sport-Related Tendinopathies: A Narrative Review. Medicina. 2021; 57(10):1088. https://doi.org/10.3390/medicina57101088
Chicago/Turabian StyleCrimaldi, Sergio, Sara Liguori, Pasquale Tamburrino, Antimo Moretti, Marco Paoletta, Giuseppe Toro, and Giovanni Iolascon. 2021. "The Role of Hyaluronic Acid in Sport-Related Tendinopathies: A Narrative Review" Medicina 57, no. 10: 1088. https://doi.org/10.3390/medicina57101088
APA StyleCrimaldi, S., Liguori, S., Tamburrino, P., Moretti, A., Paoletta, M., Toro, G., & Iolascon, G. (2021). The Role of Hyaluronic Acid in Sport-Related Tendinopathies: A Narrative Review. Medicina, 57(10), 1088. https://doi.org/10.3390/medicina57101088







