Glycemia, Beta-Cell Function and Sensitivity to Insulin in Mildly to Critically Ill Covid-19 Patients
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ilias, I.; Zabuliene, L. Hyperglycemia and the novel Covid-19 infection: Possible pathophysiologic mechanisms. Med. Hypotheses 2020, 139, 109699. [Google Scholar] [CrossRef] [PubMed]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y.; et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef]
- Iacobellis, G.; Penaherrera, C.A.; Bermudez, L.E.; Bernal Mizrachi, E. Admission hyperglycemia and radiological findings of SARS-CoV2 in patients with and without diabetes. Diabetes Res. Clin. Pract. 2020, 164, 108185. [Google Scholar] [CrossRef] [PubMed]
- Ilias, I.; Jahaj, E.; Kokkoris, S.; Zervakis, D.; Temperikidis, P.; Magira, E.; Pratikaki, M.; Vassiliou, A.G.; Routsi, C.; Kotanidou, A.; et al. Clinical Study of Hyperglycemia and SARS-CoV-2 Infection in Intensive Care Unit Patients. In Vivo 2020, 34, 3029–3032. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.; Chen, X.; Cai, Y.; Xia, J.; Zhou, X.; Xu, S.; Huang, H.; Zhang, L.; Du, C.; Zhang, Y.; et al. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients with Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern. Med. 2020, e200994. [Google Scholar] [CrossRef]
- Chen, J.; Wu, C.; Wang, X.; Yu, J.; Sun, Z. The Impact of COVID-19 on Blood Glucose: A Systematic Review and Meta-Analysis. Front. Endocrinol. 2020, 11, 574541. [Google Scholar] [CrossRef]
- Carrasco-Sánchez, F.J.; López-Carmona, M.D.; Martínez-Marcos, F.J.; Pérez-Belmonte, L.M.; Hidalgo-Jiménez, A.; Buonaiuto, V.; Suárez Fernández, C.; Freire Castro, S.J.; Luordo, D.; Pesqueira Fontan, P.M.; et al. Admission hyperglycaemia as a predictor of mortality in patients hospitalized with COVID-19 regardless of diabetes status: Data from the Spanish SEMI-COVID-19 Registry. Ann. Med. 2021, 53, 103–116. [Google Scholar] [CrossRef]
- Ali Abdelhamid, Y.; Kar, P.; Finnis, M.E.; Phillips, L.K.; Plummer, M.P.; Shaw, J.E.; Horowitz, M.; Deane, A.M. Stress hyperglycaemia in critically ill patients and the subsequent risk of diabetes: A systematic review and meta-analysis. Crit. Care 2016, 20, 301. [Google Scholar] [CrossRef]
- Jensen, A.V.; Baunbæk Egelund, G.; Bang Andersen, S.; Petersen, P.T.; Benfield, T.; Witzenrath, M.; Rohde, G.; Ravn, P.; Faurholt-Jepsen, D. The Glycemic Gap and 90-Day Mortality in Community-acquired Pneumonia. A Prospective Cohort Study. Ann. Am. Thorac. Soc. 2019, 16, 1518–1526. [Google Scholar] [CrossRef]
- Liao, W.I.; Lin, C.S.; Lee, C.H.; Wu, Y.C.; Chang, W.C.; Hsu, C.W.; Wang, J.C.; Tsai, S.H. An Elevated Glycemic Gap is Associated with Adverse Outcomes in Diabetic Patients with Acute Myocardial Infarction. Sci. Rep. 2016, 6, 27770. [Google Scholar] [CrossRef]
- Donagaon, S.; Dharmalingam, M. Association between Glycemic Gap and Adverse Outcomes in Critically Ill Patients with Diabetes. Indian J. Endocrinol. Metab. 2018, 22, 208–211. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.J.; Liao, W.I.; Tang, Z.C.; Wang, J.C.; Lee, C.H.; Chang, W.C.; Hsu, C.W.; Tang, S.E.; Tsai, S.H. Glycated hemoglobin A1c-based adjusted glycemic variables in patients with diabetes presenting with acute exacerbation of chronic obstructive pulmonary disease. Int. J. Chron. Obstruct. Pulmon. Dis. 2017, 12, 1923–1932. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wallace, T.M.; Levy, J.C.; Matthews, D.R. Use and abuse of HOMA modeling. Diabetes Care 2004, 27, 1487–1495. [Google Scholar] [CrossRef]
- Muniangi-Muhitu, H.; Akalestou, E.; Salem, V.; Misra, S.; Oliver, N.S.; Rutter, G.A. Covid-19 and Diabetes: A Complex Bidirectional Relationship. Front. Endocrinol. 2020, 11, 582936. [Google Scholar] [CrossRef]
- Lim, S.; Bae, J.H.; Kwon, H.S.; Nauck, M.A. COVID-19 and diabetes mellitus: From pathophysiology to clinical management. Nat. Rev. Endocrinol. 2020, 17, 1–20. [Google Scholar] [CrossRef]
- Bode, B.; Garrett, V.; Messler, J.; McFarland, R.; Crowe, J.; Booth, R.; Klonoff, D.C. Glycemic Characteristics and Clinical Outcomes of COVID-19 Patients Hospitalized in the United States. J. Diabetes Sci. Technol. 2020, 14, 813–821. [Google Scholar] [CrossRef] [PubMed]
- Bellaver, P.; Schaeffer, A.F.; Dullius, D.P.; Viana, M.V.; Leitão, C.B.; Rech, T.H. Association of multiple glycemic parameters at intensive care unit admission with mortality and clinical outcomes in critically ill patients. Sci. Rep. 2019, 9, 18498. [Google Scholar] [CrossRef] [PubMed]
- Li, G. Inpatient use of glucocorticoids may mediate the detrimental effect of new-onset hyperglycemia on COVID-19 severity. Diabetes Res. Clin. Pract. 2020, 168, 108441. [Google Scholar] [CrossRef]
- Inagaki, N.; Harashima, S.; Maruyama, N.; Kawaguchi, Y.; Goda, M.; Iijima, H. Efficacy and safety of canagliflozin in combination with insulin: A double-blind, randomized, placebo-controlled study in Japanese patients with type 2 diabetes mellitus. Cardiovasc. Diabetol. 2016, 15, 89. [Google Scholar] [CrossRef]
- Yang, T.; Lu, M.; Ma, L.; Zhou, Y.; Cui, Y. Efficacy and tolerability of canagliflozin as add-on to metformin in the treatment of type 2 diabetes mellitus: A meta-analysis. Eur. J. Clin. Pharmacol. 2015, 71, 1325–1332. [Google Scholar] [CrossRef]
- Monnier, L.; Colette, C.; Thuan, J.F.; Lapinski, H. Insulin secretion and sensitivity as determinants of HbA1c in type 2 diabetes. Eur. J. Clin. Investig. 2006, 36, 231–235. [Google Scholar] [CrossRef] [PubMed]
- Rubino, F.; Amiel, S.A.; Zimmet, P.; Alberti, G.; Bornstein, S.; Eckel, R.H.; Mingrone, G.; Boehm, B.; Cooper, M.E.; Chai, Z.; et al. New-Onset Diabetes in Covid-19. N. Engl. J. Med. 2020, 383, 789–790. [Google Scholar] [CrossRef] [PubMed]
| Group | Age (Years) | Gender (Men/Women) | BMI | APACHE II | SOFA | DEX (n) | Smoking | Comorbidities | Death |
|---|---|---|---|---|---|---|---|---|---|
| 1. Ward No Hx of diabetes (n = 75) | 56.3 ± 17.4 * | 50/25 | 25.7 ± 1.8 | N.A. | N.A. | 9 | 15 | Single: 23 More than one: 9 | 2 |
| 2. Ward Hx of diabetes (n = 10) | 59.3 ± 11.9 | 7/3 | 27.8 ± 5.3 | N.A. | N.A. | 1 | 2 | Single: 6 More than one: 4 | 0 |
| 3. ICU No Hx of diabetes (n = 60) | 62.9 ± 11.9 | 44/16 | 26.1 ± 2.4 | 13.7 ± 4.7 | 7.0 ± 2.8 | 36 | 17 | Single: 22 More than one: 12 | 17 |
| 4. ICU Hx of diabetes (n = 12) | 71.8 ± 10.8 | 11/1 | 27.1 ± 1.9 | 16.2 ± 6.1 | 7.4 ± 2.8 | 8 | 4 | Single: 5 More than one: 4 | 5 |
| Group | Glucose (mg/dL) | A1c (%) | GlyG (mg/dL) | Insulin (μU/mL) | C-Peptide (ng/mL) | HOMA2%Bins (%) | HOMA2%Bc-pept (%) | HOMA2%Sins (%) | HOMA2%Sc-pept (%) |
|---|---|---|---|---|---|---|---|---|---|
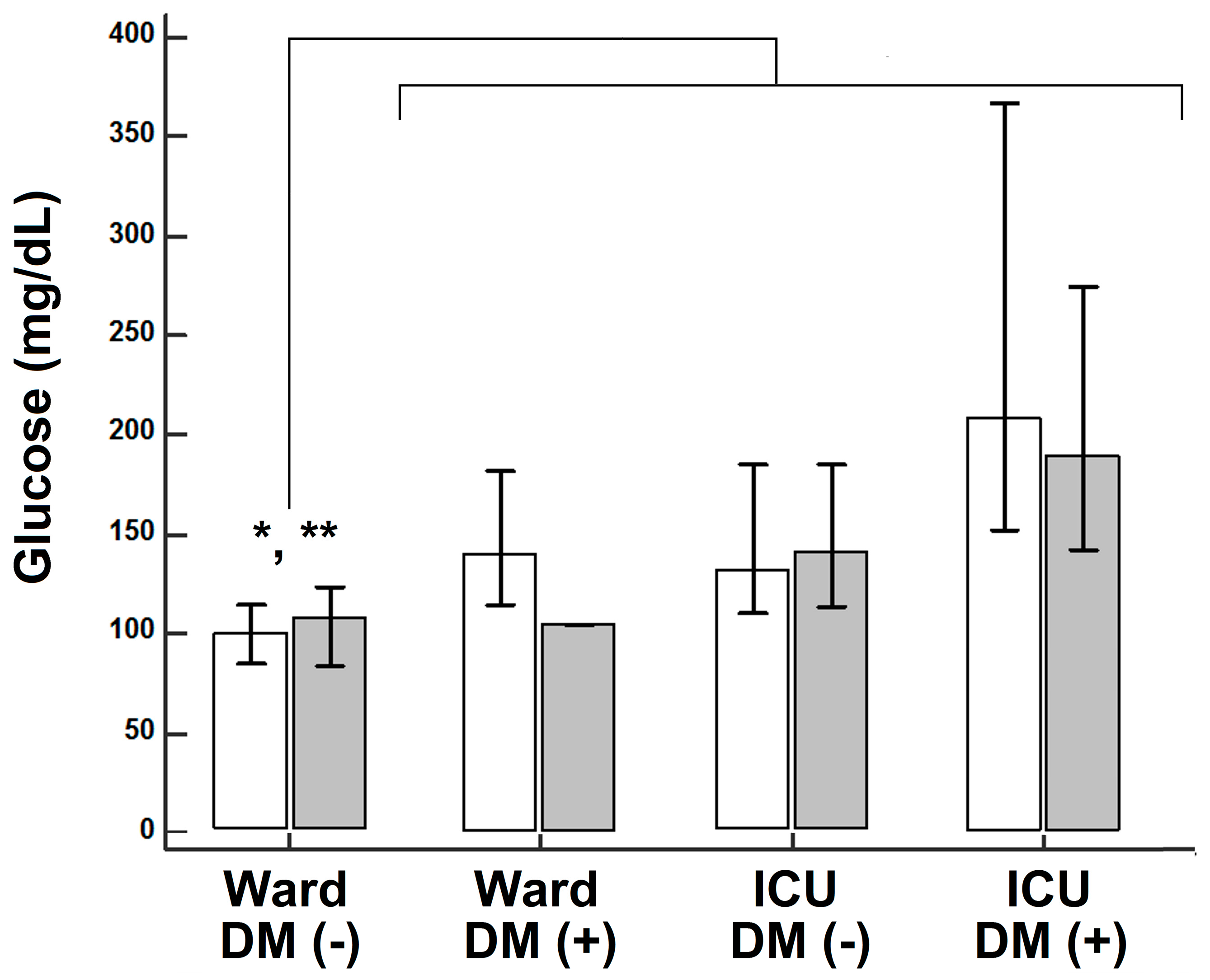
| 1. Ward No Hx of diabetes (n = 75) | 101 (84/116) * | 5.8 (5.3/6.2) | −14.1 (−38.0/+0.4) | 9.4 (5.9/23.8) | 2.5 (1.6/4.6) | 105.2 ± 63.2 | 128.4 ± 73.7 | 87.9 (47.6/122.4) | 54.0 (35.1/86.2) |
| 2. Ward Hx of diabetes (n = 10) | 136 (113/171) | 7.4 (6.1/11.0) | -5.6 (−29.9/+5.4) | 16.6 (14.9/18.4) | 3.7 (2.8/4.7) | 89.0 ± 84.5 | 100.4 ± 116.5 | 41.9 (39.3/46.9) | 25.5 (19.5/29.8) |
| 3. ICU No Hx of diabetes (n = 60) | 138 (110/184) | 5.8 (5.4/7.1) | +5.7 ** (−10.1/+22.0) | 8.4 (2.8/16.8) | 2.9 (1.5/5.9) | 76.9 ± 63.2+ | 109.9 ± 80.6 | 64.4 (37.8/99.8) | 40.9 (16.8/78.3) |
| 4. ICU Hx of diabetes (n = 12) | 192 (149/275) | 6.1 (5.4/6.5) | +30.2 (+5.5/+74.5) | 16.7 (13.6/19.8) | 3.4 (1.8/4.4) | 44.0 ± 19.0+ | 59.6 ± 65.3 | 37.0 (32.8/50.3) | 27.0 (24.1/124.1) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ilias, I.; Diamantopoulos, A.; Pratikaki, M.; Botoula, E.; Jahaj, E.; Athanasiou, N.; Tsipilis, S.; Zacharis, A.; Vassiliou, A.G.; Vassiliadi, D.A.; et al. Glycemia, Beta-Cell Function and Sensitivity to Insulin in Mildly to Critically Ill Covid-19 Patients. Medicina 2021, 57, 68. https://doi.org/10.3390/medicina57010068
Ilias I, Diamantopoulos A, Pratikaki M, Botoula E, Jahaj E, Athanasiou N, Tsipilis S, Zacharis A, Vassiliou AG, Vassiliadi DA, et al. Glycemia, Beta-Cell Function and Sensitivity to Insulin in Mildly to Critically Ill Covid-19 Patients. Medicina. 2021; 57(1):68. https://doi.org/10.3390/medicina57010068
Chicago/Turabian StyleIlias, Ioannis, Aristidis Diamantopoulos, Maria Pratikaki, Efthymia Botoula, Edison Jahaj, Nikolaos Athanasiou, Stamatios Tsipilis, Alexandros Zacharis, Alice G. Vassiliou, Dimitra A. Vassiliadi, and et al. 2021. "Glycemia, Beta-Cell Function and Sensitivity to Insulin in Mildly to Critically Ill Covid-19 Patients" Medicina 57, no. 1: 68. https://doi.org/10.3390/medicina57010068
APA StyleIlias, I., Diamantopoulos, A., Pratikaki, M., Botoula, E., Jahaj, E., Athanasiou, N., Tsipilis, S., Zacharis, A., Vassiliou, A. G., Vassiliadi, D. A., Kotanidou, A., Tsagarakis, S., & Dimopoulou, I. (2021). Glycemia, Beta-Cell Function and Sensitivity to Insulin in Mildly to Critically Ill Covid-19 Patients. Medicina, 57(1), 68. https://doi.org/10.3390/medicina57010068







