Roles of JNK/Nrf2 Pathway on Hemin-Induced Heme Oxygenase-1 Activation in MCF-7 Human Breast Cancer Cells
Abstract
1. Introduction
2. Materials and Methods
2.1. Cells and Materials
2.2. Cell Viability Assay
2.3. Western Blot Analysis
2.4. Quantitative Real-Time Polymerase Chain Reaction
2.5. Isolation Extracts of Nuclear Fraction
2.6. Electrophoretic Mobility Shift Assay (EMSA)
2.7. Statistical Analysis
3. Results
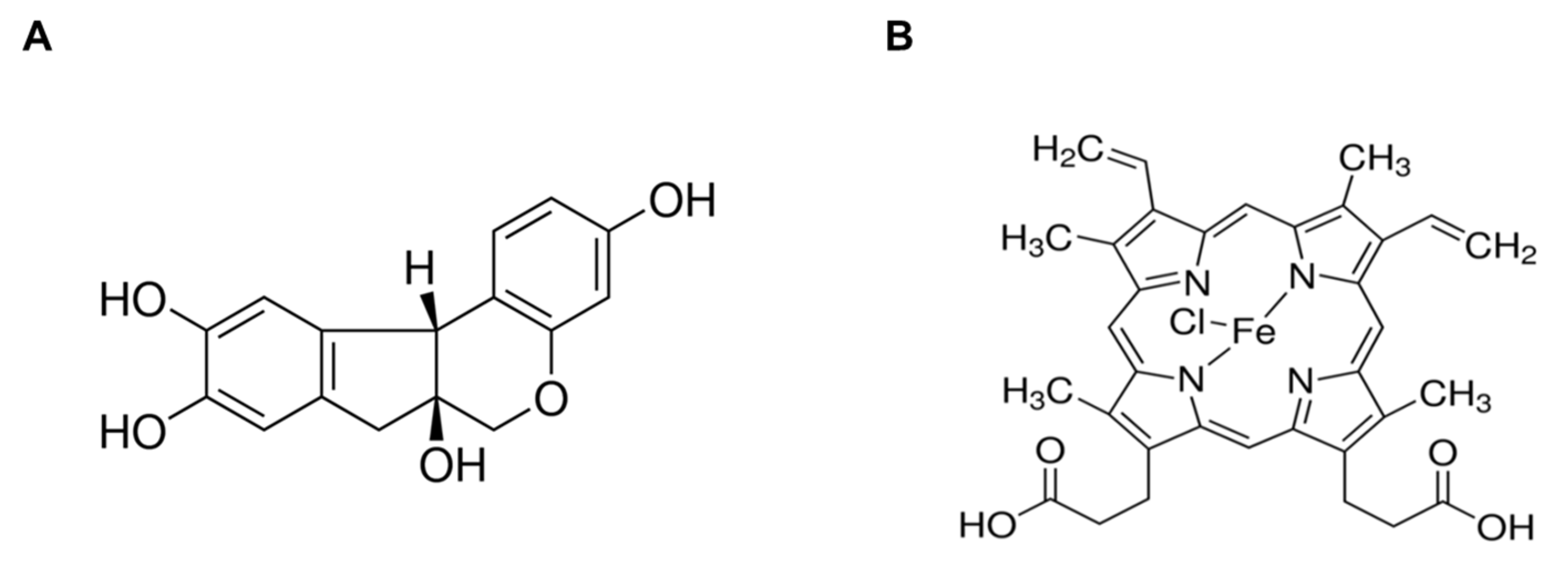
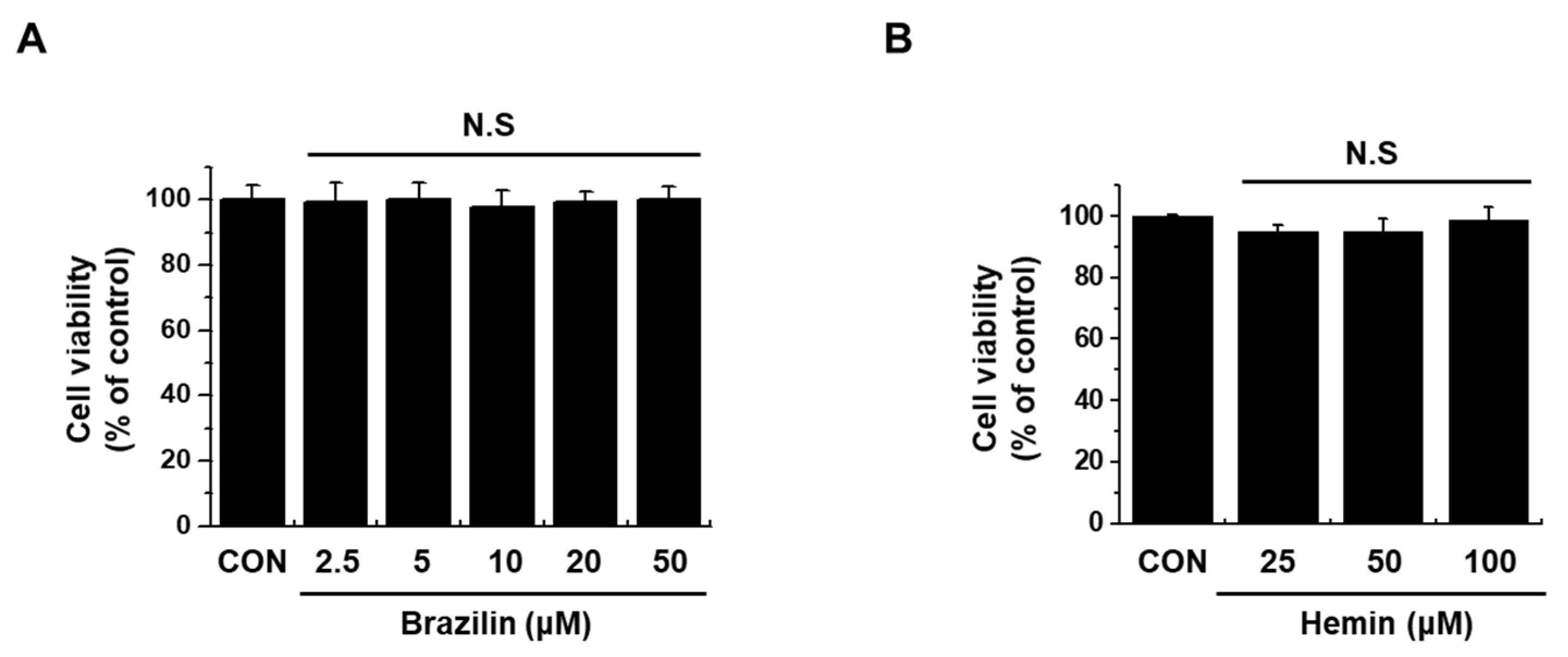
3.1. Endogenous Cytotoxicity of Brazilin and Hemin on MCF-7 Cells
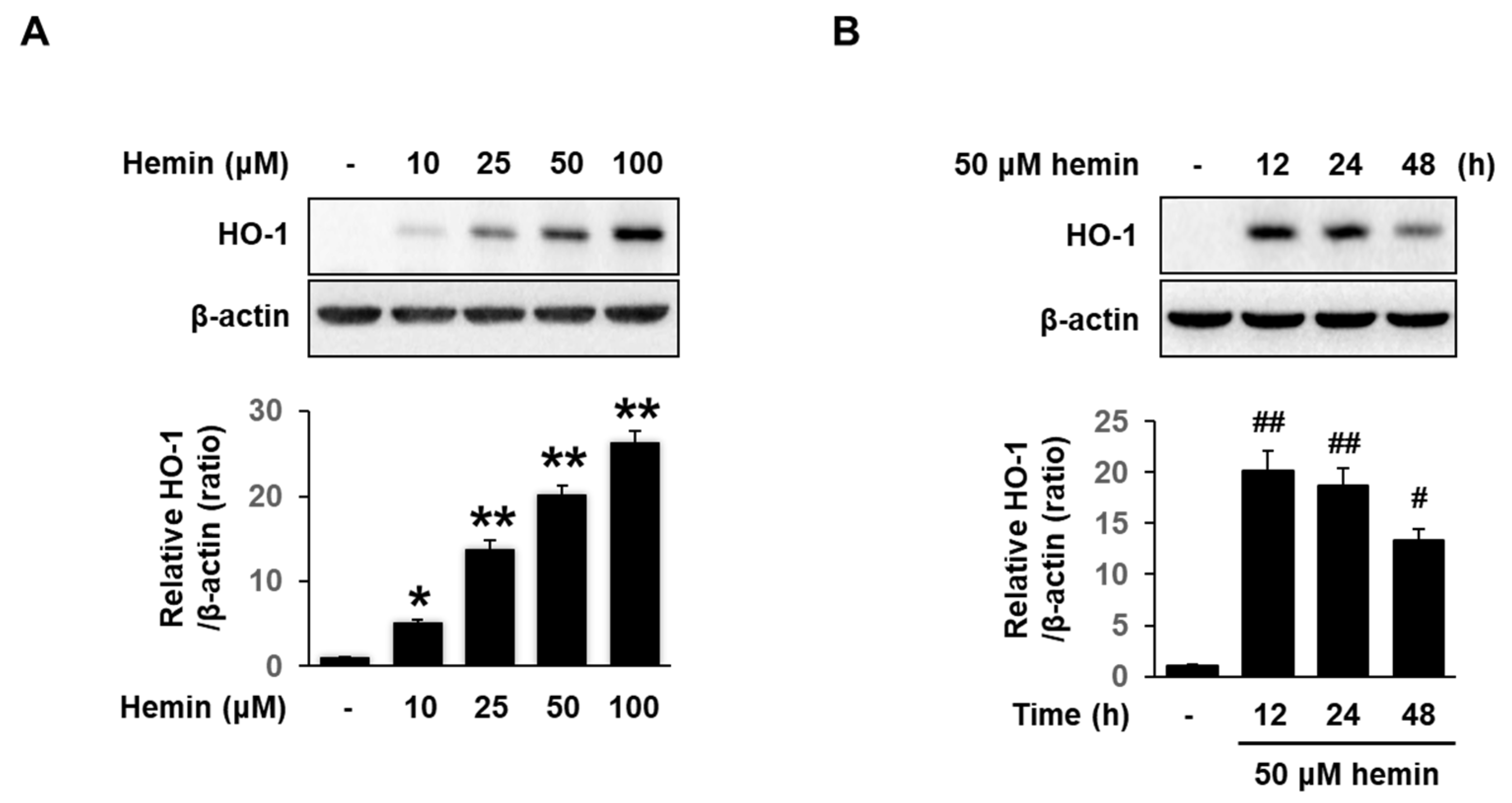
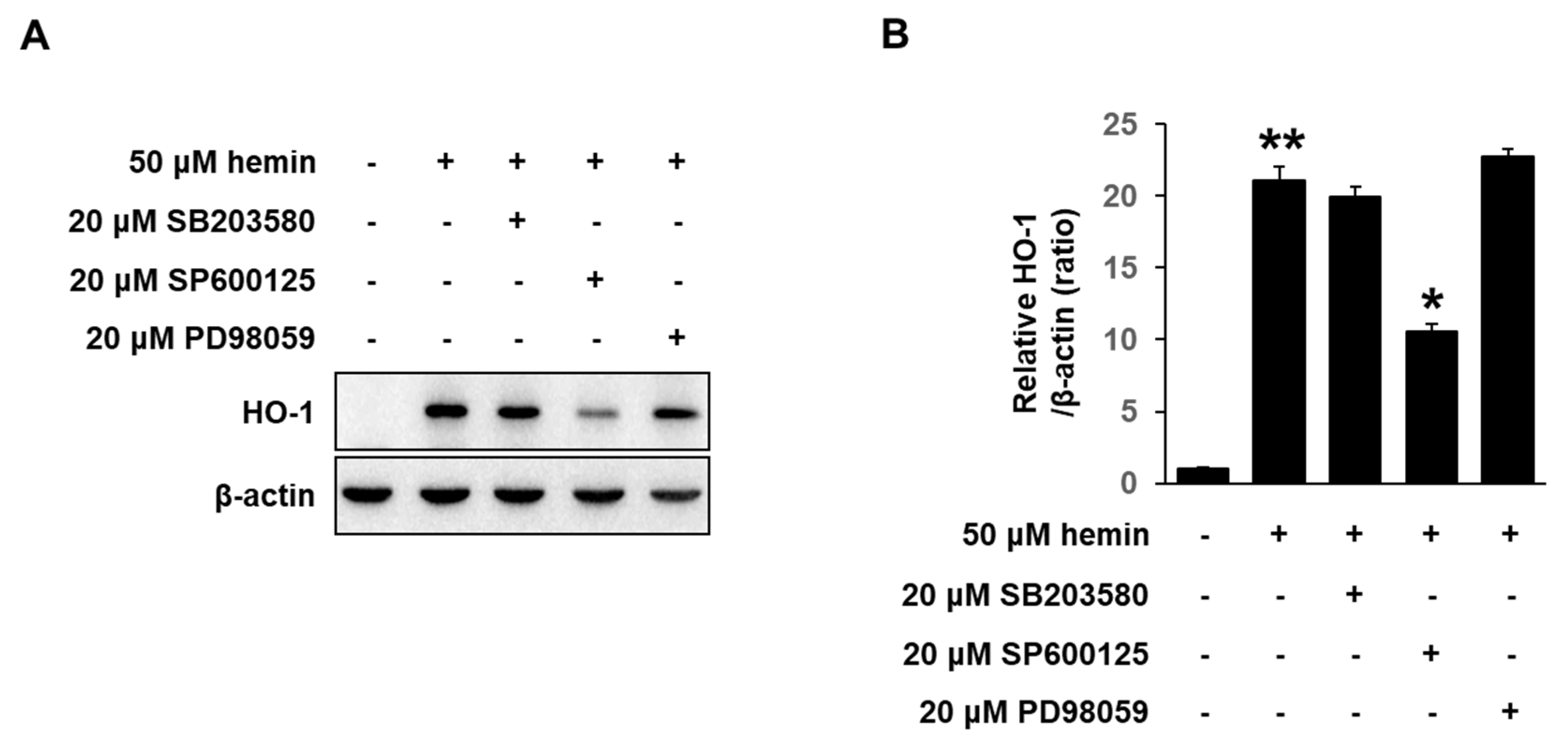
3.2. Effect of Hemin on HO-1 Expression in MCF-7 Cells
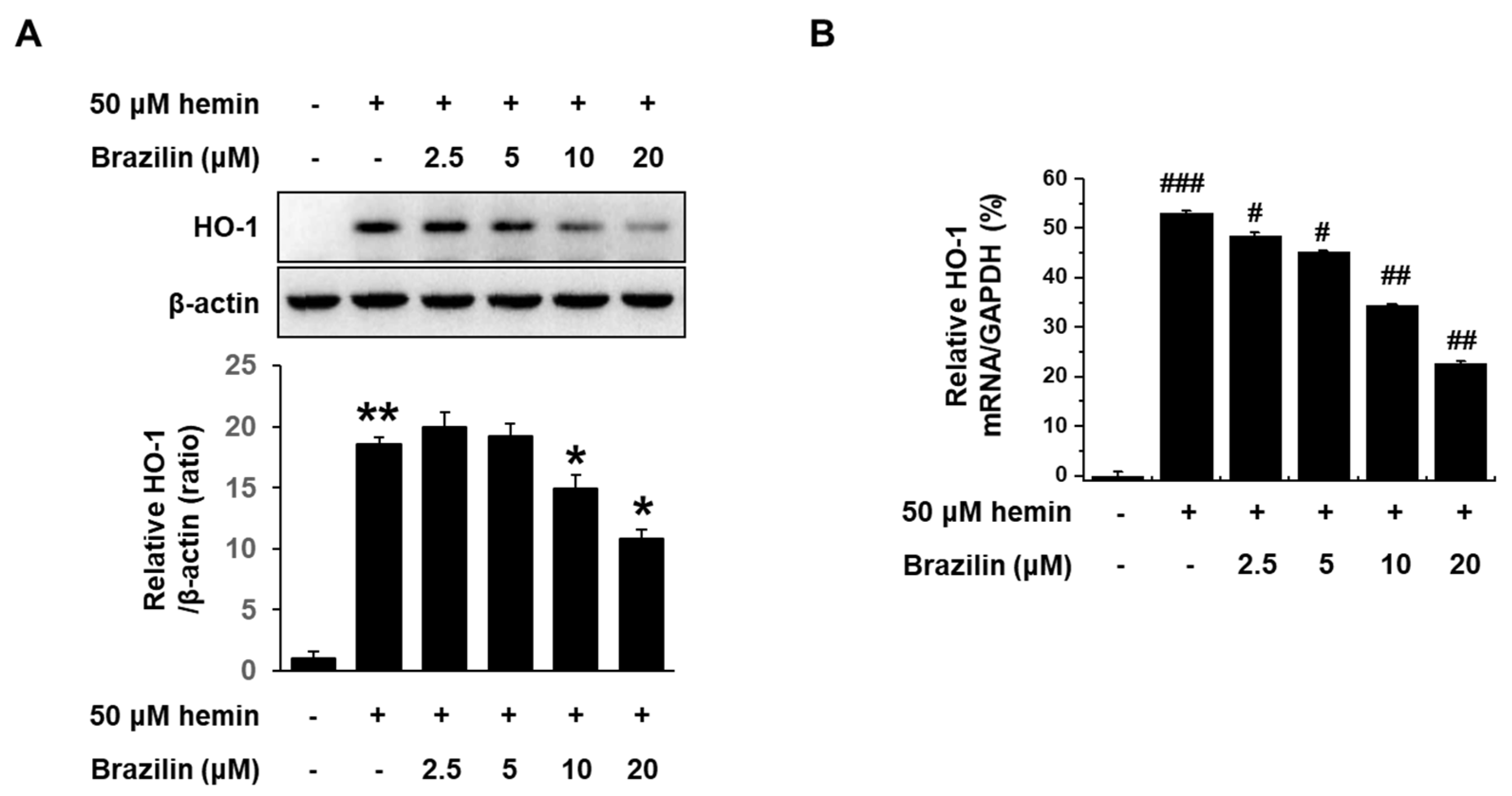
3.3. Effect of Brazilin on Hemin-Induced HO-1 Expression in MCF-7 Cells
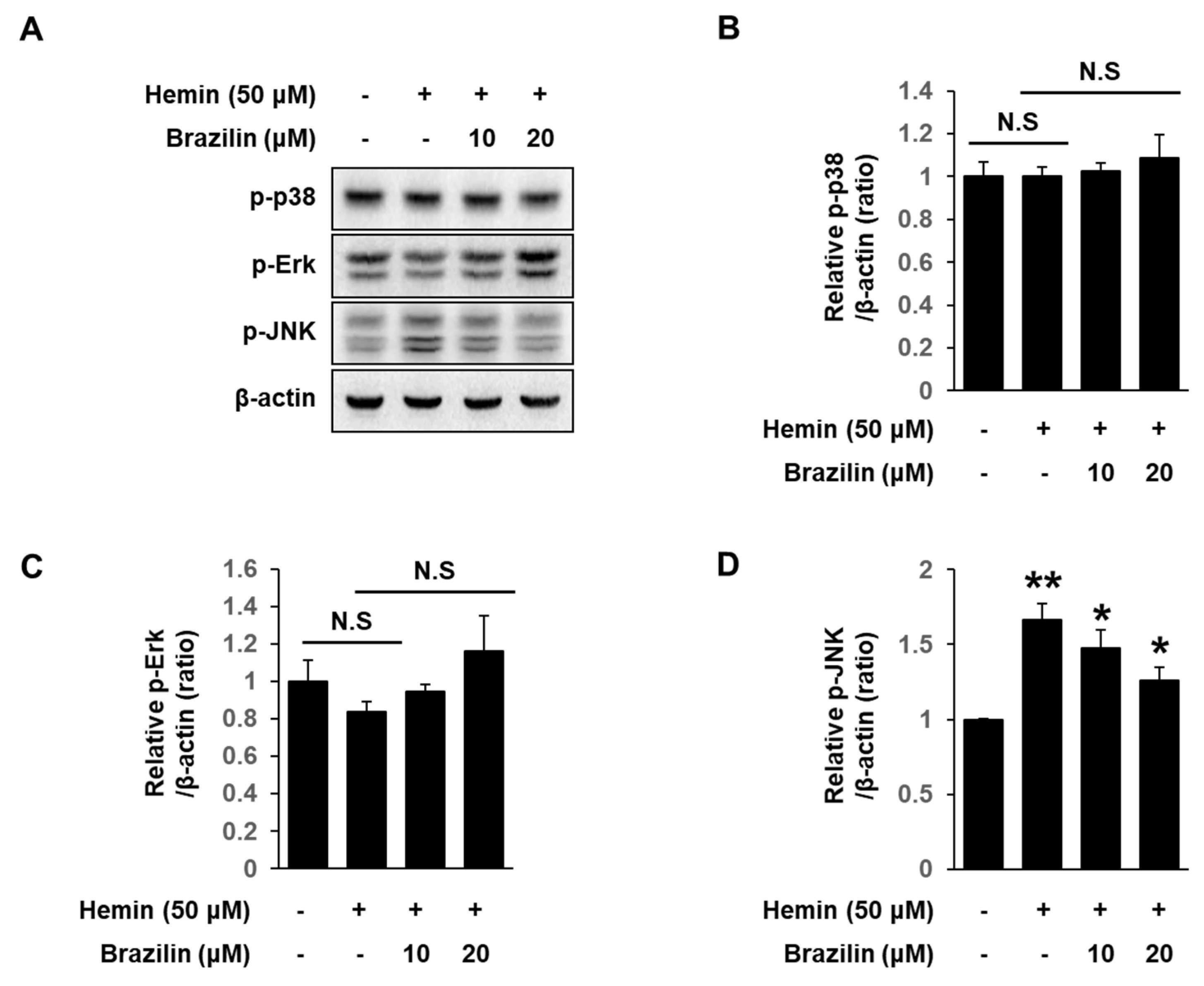
3.4. Effects of Hemin on MAPK Activation in MCF-7 Cells
3.5. Effects of Brazilin on Hemin-Induced JNK Activation in MCF-7 Cells
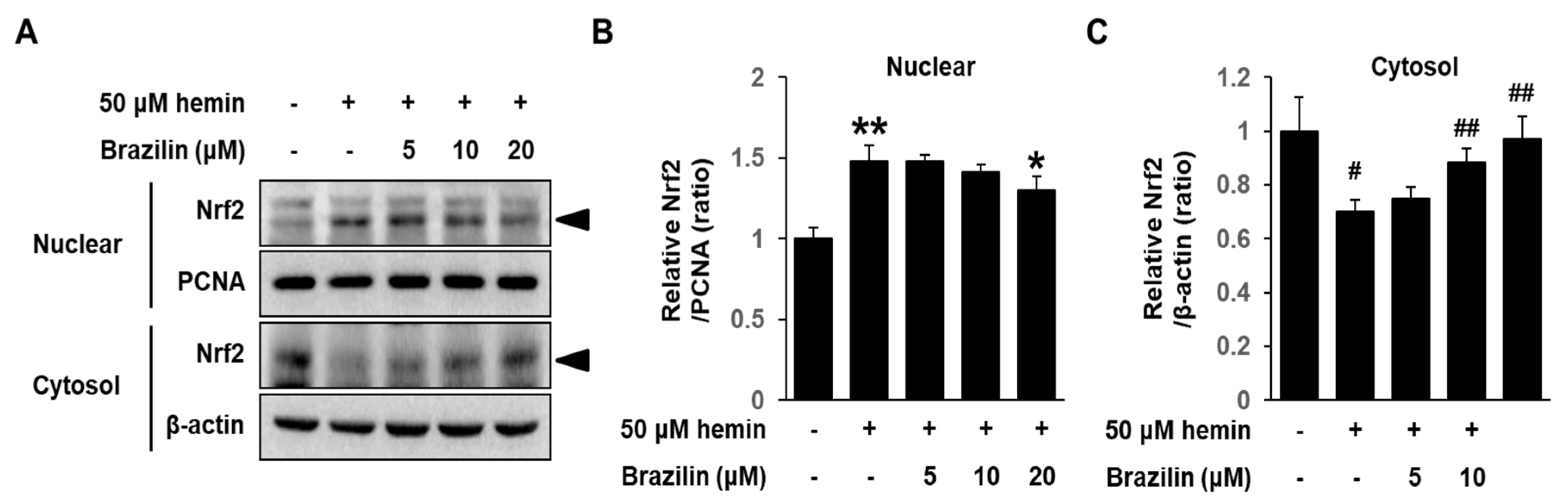
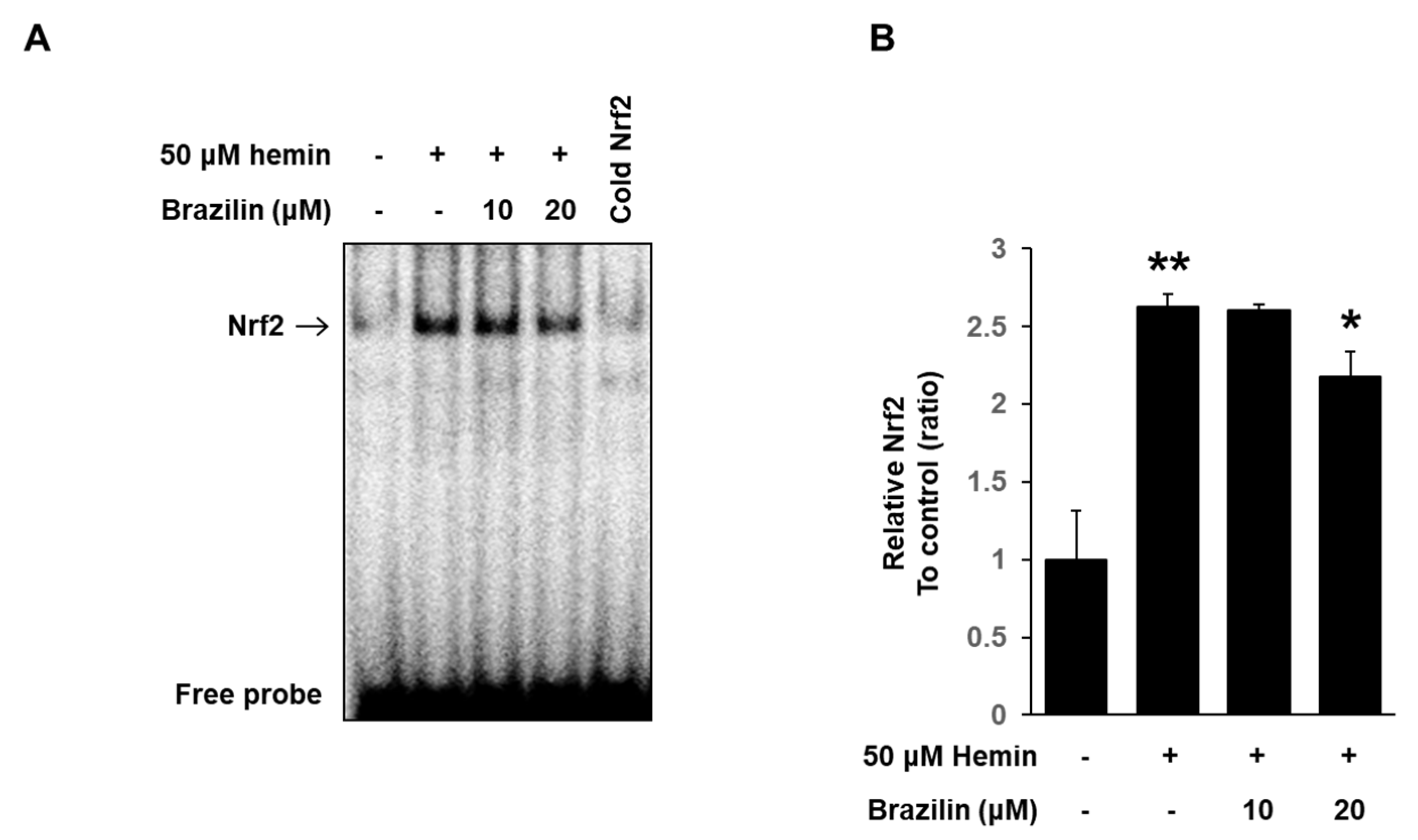
3.6. Effect of Brazilin on Hemin-Induced Nrf2 Activation in MCF-7 Cells
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Maines, M.D. Heme oxygenase: Function, multiplicity, regulatory mechanisms, and clinical applications. FASEB J. 1988, 2, 2557–2568. [Google Scholar] [CrossRef] [PubMed]
- Maines, M.D. The heme oxygenase system: A Regulator of Second Messenger Gases. Annu. Rev. Pharmacol. Toxicol. 1997, 37, 517–554. [Google Scholar] [CrossRef] [PubMed]
- Florczyk, U.M.; Jozkowicz, A.; Dulak, J. Biliverdin reductase: New features of an old enzyme and its potential therapeutic significance. Pharmacol. Rep. 2008, 60, 38–48. [Google Scholar] [PubMed]
- Clark, J.E.; Foresti, R.; Green, C.J.; Motterlini, R. Dynamics of heme oxygenase-1 expression and bilirubin production in cellular protection against oxidative stress. Biochem. J. 2000, 348, 615–619. [Google Scholar] [CrossRef]
- Keyse, S.; A Applegate, L.; Tromvoukis, Y.; Tyrrell, R.M. Oxidant stress leads to transcriptional activation of the human heme oxygenase gene in cultured skin fibroblasts. Mol. Cell. Boil. 1990, 10, 4967–4969. [Google Scholar] [CrossRef]
- Rizzardini, M.; Terao, M.; Falciani, F.; Cantoni, L. Cytokine induction of heme oxygenase mRNA in mouse liver. Interleukin 1 transcriptionally activates the heme oxygenase gene. Biochem. J. 1993, 290, 343–347. [Google Scholar] [CrossRef]
- Cantoni, L.; Rossi, C.; Rizzardini, M.; Gadina, M.; Ghezzi, P. Interleukin-1 and tumour necrosis factor induce hepatic heme oxygenase. Feedback regulation by glucocorticoids. Biochem. J. 1991, 279, 891–894. [Google Scholar] [CrossRef]
- Lee, P.J.; Jiang, B.H.; Chin, B.Y. Hypoxia-inducible factor-1 mediates transcriptional activation of the heme oxygenase-1 gene in response to hypoxia. J. Biol. Chem. 1997, 272, 5375–5381. [Google Scholar] [CrossRef]
- Becker, J.C.; Fukui, H.; Imai, Y.; Sekikawa, A.; Kimura, T.; Yamagishi, H.; Yoshitake, N.; Pohle, T.; Domschke, W.; Fujimori, T. Colonic expression of heme oxygenase-1 is associated with a better long-term survival in patients with colorectal cancer. Scand. J. Gastroenterol. 2007, 42, 852–858. [Google Scholar] [CrossRef]
- Busserolles, J.; Megías, J.; Terencio, M.C.; Alcaraz, M.J. Heme oxygenase-1 inhibits apoptosis in Caco-2 cells via activation of Akt pathway. Int. J. Biochem. Cell Boil. 2006, 38, 1510–1517. [Google Scholar] [CrossRef]
- Willis, D.; Moore, A.R.; Frederick, R.; Willoughby, D. Heme oxygenase: A novel target for the modulation of inflammatory response. Nat. Med. 1996, 2, 87–90. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.J.; Alam, J.; Wiegand, G.W.; Choi, A.M. Overexpression of heme oxygenase-1 in human pulmonary epithelial cells results in cell growth arrest and increased resistance to hyperoxia. Proc. Natl. Acad. Sci. USA 1996, 93, 10393–10398. [Google Scholar] [CrossRef] [PubMed]
- Deng, Y.-M.; Wu, B.J.; Witting, P.K.; Stocker, R. Probucol Protects Against Smooth Muscle Cell Proliferation by Upregulating Heme Oxygenase-1. Circulation 2004, 110, 1855–1860. [Google Scholar] [CrossRef] [PubMed]
- Brouard, S.; Otterbein, L.E.; Anrather, J.; Tobiasch, E.; Bach, F.H.; Choi, A.M.; Soares, M. Carbon Monoxide Generated by Heme Oxygenase 1 Suppresses Endothelial Cell Apoptosis. J. Exp. Med. 2000, 192, 1015–1026. [Google Scholar] [CrossRef] [PubMed]
- Goodman, A.I.; Choudhury, M.; Da Silva, J.-L.; Schwartzman, M.L.; Abraham, N.G. Overexpression of the Heme Oxygenase Gene in Renal Cell Carcinoma. Exp. Boil. Med. 1997, 214, 54–75. [Google Scholar] [CrossRef]
- Choi, B.-M.; Pae, H.-O.; Jeong, Y.-R.; Oh, G.-S.; Jun, C.-D.; Kim, B.-R.; Kim, Y.-M.; Chung, H.-T. Overexpression of heme oxygenase (HO)-1 renders jurkat T cells resistant to Fas-mediated apoptosis: Involvement of iron released by HO-1. Free Radic. Boil. Med. 2004, 36, 858–871. [Google Scholar] [CrossRef]
- Maines, M.D.; Abrahamsson, P.-A. Expression of heme oxygenase-1 (HSP32) in human prostate: Normal, hyperplastic, and tumor tissue distribution. Urology 1996, 47, 727–733. [Google Scholar] [CrossRef]
- Degese, M.S.; Mendizabal, J.E.; Gandini, N.A.; Gutkind, J.S.; Molinolo, A.; Hewitt, S.M.; Curino, A.C.; Coso, O.A.; Facchinetti, M.M. Expression of heme oxygenase-1 in non-small cell lung cancer (NSCLC) and its correlation with clinical data. Lung Cancer 2012, 77, 168–175. [Google Scholar] [CrossRef]
- Gandini, N.A.; Fermento, M.E.; Salomón, D.G.; Blasco, J.; Patel, V.; Gutkind, J.S.; Molinolo, A.A.; Facchinetti, M.M.; Curino, A.C. Nuclear localization of heme oxygenase-1 is associated with tumor progression of head and neck squamous cell carcinomas. Exp. Mol. Pathol. 2012, 93, 237–245. [Google Scholar] [CrossRef]
- Yin, H.; Fang, J.; Liao, L.; Maeda, H.; Su, Q. Upregulation of heme oxygenase-1 in colorectal cancer patients with increased circulation carbon monoxide levels, potentially affects chemotherapeutic sensitivity. BMC Cancer 2014, 14, 436. [Google Scholar] [CrossRef]
- Tsai, J.-R.; Wang, H.-M.; Liu, P.-L.; Chen, Y.-H.; Yang, M.-C.; Chou, S.-H.; Cheng, Y.-J.; Yin, W.-H.; Chong, I.-W. High expression of heme oxygenase-1 is associated with tumor invasiveness and poor clinical outcome in non-small cell lung cancer patients. Cell. Oncol. 2012, 35, 461–471. [Google Scholar] [CrossRef] [PubMed]
- Yin, Y.; Liu, Q.; Wang, B.; Chen, G.; Xu, L.; Zhou, H. Expression and function of heme oxygenase-1 in human gastric cancer. Exp. Boil. Med. 2012, 237, 362–371. [Google Scholar] [CrossRef] [PubMed]
- Miyata, Y.; Kanda, S.; Mitsunari, K.; Asai, A.; Sakai, H. Heme oxygenase-1 expression is associated with tumor aggressiveness and outcomes in patients with bladder cancer: A correlation with smoking intensity. Transl. Res. 2014, 164, 468–476. [Google Scholar] [CrossRef] [PubMed]
- Noh, S.J.; Bae, J.S.; Jamiyandorj, U.; Park, H.S.; Kwon, K.; Jung, S.H.; Youn, H.J.; Lee, H.; Park, B.-H.; Chung, M.J.; et al. Expression of nerve growth factor and heme oxygenase-1 predict poor survival of breast carcinoma patients. BMC Cancer 2013, 13, 516. [Google Scholar] [CrossRef] [PubMed]
- Gandini, N.A.; Fermento, M.E.; Salomón, D.G.; Obiol, D.J.; Andrés, N.C.; Zenklusen, J.C.; Arévalo, J.; Blasco, J.; Romero, A.L.; Facchinetti, M.M.; et al. Heme oxygenase-1 expression in human gliomas and its correlation with poor prognosis in patients with astrocytoma. Tumor Boil. 2013, 35, 2803–2815. [Google Scholar] [CrossRef]
- Chau, L.-Y. Heme oxygenase-1: Emerging target of cancer therapy. J. Biomed. Sci. 2015, 22, 22. [Google Scholar] [CrossRef]
- Salis, O.; Bedir, A.; Ozdemir, T.; Okuyucu, A.; Alacam, H. The relationship between anticancer effect of metformin and the transcriptional regulation of certain genes (CHOP, CAV-1, HO-1, SGK-1 and Par-4) on MCF-7 cell line. Eur. Rev. Med. Pharmacol. Sci. 2014, 18, 1602–1609. [Google Scholar]
- Levenson, A.S.; Jordan, V.C. MCF-7: The first hormone-responsive breast cancer cell line. Cancer Res. 1997, 57, 3071–3078. [Google Scholar]
- Kao, J.; Salari, K.; Bocanegra, M.; Choi, Y.-L.; Girard, L.; Gandhi, J.; Kwei, K.A.; Hernandez-Boussard, T.; Wang, P.; Gazdar, A.F.; et al. Molecular Profiling of Breast Cancer Cell Lines Defines Relevant Tumor Models and Provides a Resource for Cancer Gene Discovery. PLoS ONE 2009, 4, e6146. [Google Scholar] [CrossRef]
- Lim, M.-Y.; Jeon, J.-H.; Jeong, E.-Y.; Lee, C.-H.; Lee, H.-S. Antimicrobial activity of 5-hydroxy-1,4-naphthoquinone isolated from Caesalpinia sappan toward intestinal bacteria. Food Chem. 2007, 100, 1254–1258. [Google Scholar] [CrossRef]
- Hikino, H.; Taguchi, T.; Fujimura, H.; Hiramatsu, Y. Antiinflammatory principles of Caesalpinia sappan wood and of Haematoxylon campechianum wood. Planta Med. 1977, 31, 214–220. [Google Scholar] [CrossRef] [PubMed]
- Bae, I.-K.; Min, H.-Y.; Han, A.-R.; Seo, E.-K.; Lee, S.K. Suppression of lipopolysaccharide-induced expression of inducible nitric oxide synthase by brazilin in RAW 264.7 macrophage cells. Eur. J. Pharmacol. 2005, 513, 237–242. [Google Scholar] [CrossRef] [PubMed]
- Moon, C.-K.; Park, K.-S.; Kim, S.-G.; Won, H.-S.; Chung, J.H. Brazilin protects cultured rat hepatocytes from BrCCl3-induced toxicity. Drug Chem. Toxicol. 1992, 15, 81–91. [Google Scholar] [CrossRef]
- Kim, S.-G.; Kim, Y.-M.; Khil, L.-Y.; Jeon, S.-D.; So, D.-S.; Moon, C.-H.; Moon, C.-K. Brazilin inhibits activities of protein kinase C and insulin receptor serine kinase in rat liver. Arch. Pharmacal. Res. 1998, 21, 140–146. [Google Scholar] [CrossRef]
- Kim, S.-H.; Lyu, H.-N.; Kim, Y.S.; Jeon, Y.H.; Kim, W.; Kim, S.; Lim, J.-K.; Lee, H.W.; Baek, N.-I.; Choi, K.-Y.; et al. Brazilin Isolated from Caesalpinia sappan Suppresses Nuclear Envelope Reassembly by Inhibiting Barrier-to-Autointegration Factor Phosphorylation. J. Pharmacol. Exp. Ther. 2014, 352, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.-Y.; Lee, M.-K.; Kim, G.-S.; Noh, H.-J.; Lee, M.-H. Brazilin Inhibits Growth and Induces Apoptosis in Human Glioblastoma Cells. Molecules 2013, 18, 2449–2457. [Google Scholar] [CrossRef] [PubMed]
- Hellman, L.; Fried, M. Electrophoretic mobility shift assay (EMSA) for detecting protein–nucleic acid interactions. Nat. Protoc. 2007, 2, 1849–1861. [Google Scholar] [CrossRef] [PubMed]
- Foresti, R.; Hoque, M.; Bains, S.; Green, C.J.; Motterlini, R. Heme and nitric oxide: Synergism in the modulation of the endothelial heme oxygenase-1 pathway. Biochem. J. 2003, 372, 381–390. [Google Scholar] [CrossRef]
- Ndisang, J.F.; Wu, L.; Zhao, W.; Wang, R. Induction of heme oxygenase-1 and stimulation of cGMP production by hemin in aortic tissues from hypertensive rats. Blood 2003, 101, 3893–3900. [Google Scholar] [CrossRef]
- Abate, A.; Yang, G.; Wong, R.J.; Schroder, H.; Stevenson, D.K.; Dennery, P.A. Apigenin decreases hemin-mediated heme oxygenase-1 induction. Free Radic. Biol. Med. 2005, 39, 711–718. [Google Scholar] [CrossRef]
- Ryter, S.W.; Xi, S.; Hartsfield, C.L.; Choi, A.M.K. Mitogen Activated Protein Kinase (MAPK) Pathway Regulates Heme Oxygenase-1 Gene Expression by Hypoxia in Vascular Cells. Antioxid. Redox Signal. 2002, 4, 587–592. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.-Y.; Hsiao, W.-C.; Huang, C.-J.; Kao, C.-F.; Hsu, G.-S.W. Heme oxygenase-1 induction by the ROS–JNK pathway plays a role in aluminum-induced anemia. J. Inorg. Biochem. 2013, 128, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Gong, P.; Stewart, D.; Hu, B.; Li, N.; Cook, J.; Nel, A.; Alam, J. Activation of the Mouse Heme Oxygenase-1 Gene by 15-Deoxy-Δ12,14-Prostaglandin J2 Is Mediated by the Stress Response Elements and Transcription Factor Nrf2. Antioxid. Redox Signal. 2002, 4, 249–257. [Google Scholar] [CrossRef] [PubMed]
- Lang, D.; Reuter, S.; Buzescu, T.; August, C.; Heidenreich, S. Heme-induced heme oxygenase-1 (HO-1) in human monocytes inhibits apoptosis despite caspase-3 up-regulation. Int. Immunol. 2004, 17, 155–165. [Google Scholar] [CrossRef][Green Version]
- Chen, G.G.; Liu, Z.; Vlantis, A.; Tse, G.; Leung, B.; Van Hasselt, C. Heme oxygenase-1 protects against apoptosis induced by tumor necrosis factor-α and cycloheximide in papillary thyroid carcinoma cells. J. Cell. Biochem. 2004, 92, 1246–1256. [Google Scholar] [CrossRef]
- Chiang, S.-K.; Chen, S.-E.; Chang, L.-C. A Dual Role of Heme Oxygenase-1 in Cancer Cells. Int. J. Mol. Sci. 2018, 20, 39. [Google Scholar] [CrossRef]
- Gonzales, S.; A Erario, M.; Tomaro, M.L. Heme oxygenase-1 induction and dependent increase in ferritin. A protective antioxidant stratagem in hemin-treated rat brain. Dev. Neurosci. 2002, 24, 61–168. [Google Scholar]
- Ciaffaglione, V.; Intagliata, S.; Pittalà, V.; Marrazzo, A.; Sorrenti, V.; Vanella, L.; Rescifina, A.; Floresta, G.; Sultan, A.; Greish, K.; et al. New Arylethanolimidazole Derivatives as HO-1 Inhibitors with Cytotoxicity against MCF-7 Breast Cancer Cells. Int. J. Mol. Sci. 2020, 21, 1923. [Google Scholar] [CrossRef]
- Sorrenti, V.; Raffaele, M.; Vanella, L.; Acquaviva, R.; Salerno, L.; Pittalà, V.; Intagliata, S.; Di Giacomo, C. Protective Effects of Caffeic Acid Phenethyl Ester (CAPE) and Novel Cape Analogue as Inducers of Heme Oxygenase-1 in Streptozotocin-Induced Type 1 Diabetic Rats. Int. J. Mol. Sci. 2019, 20, 2441. [Google Scholar] [CrossRef]
- Podkalicka, P.; Mucha, O.; Kruczek, S.; Biela, A.; Andrysiak, K.; Stępniewski, J.; Mikulski, M.; Gałęzowski, M.; Sitarz, K.; Brzózka, K.; et al. Synthetically Lethal Interactions of Heme Oxygenase-1 and Fumarate Hydratase Genes. Biomolecules 2020, 10, 143. [Google Scholar] [CrossRef]
- Muñoz-Sánchez, J.; Chánez-Cárdenas, M.E. A Review on Hemeoxygenase-2: Focus on Cellular Protection and Oxygen Response. Oxidative Med. Cell. Longev. 2014, 2014, 1–16. [Google Scholar] [CrossRef]
- Jang, H.Y. Brazilin Has Anticancer Activity through HO-1 Pathway in MCF-7 Human Breast Cancer Cells. Master’s Thesis, Graduated School Chonbuk National University, Jeonju, Korea, 22 February 2017. [Google Scholar]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jang, H.-Y.; Hong, O.-Y.; Chung, E.-Y.; Park, K.-H.; Kim, J.-S. Roles of JNK/Nrf2 Pathway on Hemin-Induced Heme Oxygenase-1 Activation in MCF-7 Human Breast Cancer Cells. Medicina 2020, 56, 268. https://doi.org/10.3390/medicina56060268
Jang H-Y, Hong O-Y, Chung E-Y, Park K-H, Kim J-S. Roles of JNK/Nrf2 Pathway on Hemin-Induced Heme Oxygenase-1 Activation in MCF-7 Human Breast Cancer Cells. Medicina. 2020; 56(6):268. https://doi.org/10.3390/medicina56060268
Chicago/Turabian StyleJang, Hye-Yeon, On-Yu Hong, Eun-Yong Chung, Kwang-Hyun Park, and Jong-Suk Kim. 2020. "Roles of JNK/Nrf2 Pathway on Hemin-Induced Heme Oxygenase-1 Activation in MCF-7 Human Breast Cancer Cells" Medicina 56, no. 6: 268. https://doi.org/10.3390/medicina56060268
APA StyleJang, H.-Y., Hong, O.-Y., Chung, E.-Y., Park, K.-H., & Kim, J.-S. (2020). Roles of JNK/Nrf2 Pathway on Hemin-Induced Heme Oxygenase-1 Activation in MCF-7 Human Breast Cancer Cells. Medicina, 56(6), 268. https://doi.org/10.3390/medicina56060268



