Stress in the Volunteer Caregiver: Human-Centric Technology Can Support Both Caregivers and People with Dementia
Abstract
1. Introduction
2. Materials and Methods
2.1. Home-Based Caregivers
2.2. Professional Caregivers
2.3. Data Collection and Management
3. Results
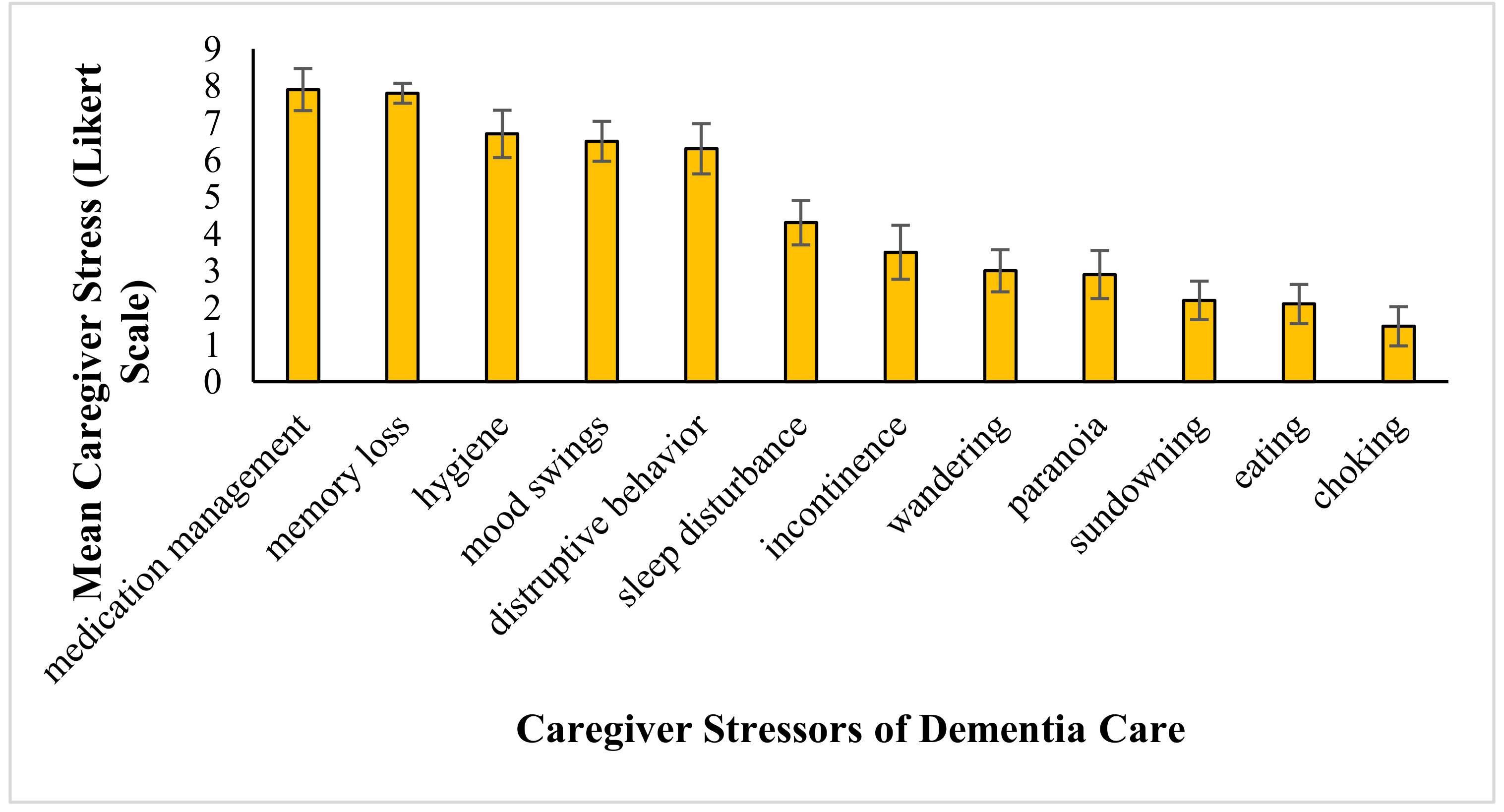
3.1. Drivers of Stress in the Home-Based Caregiver
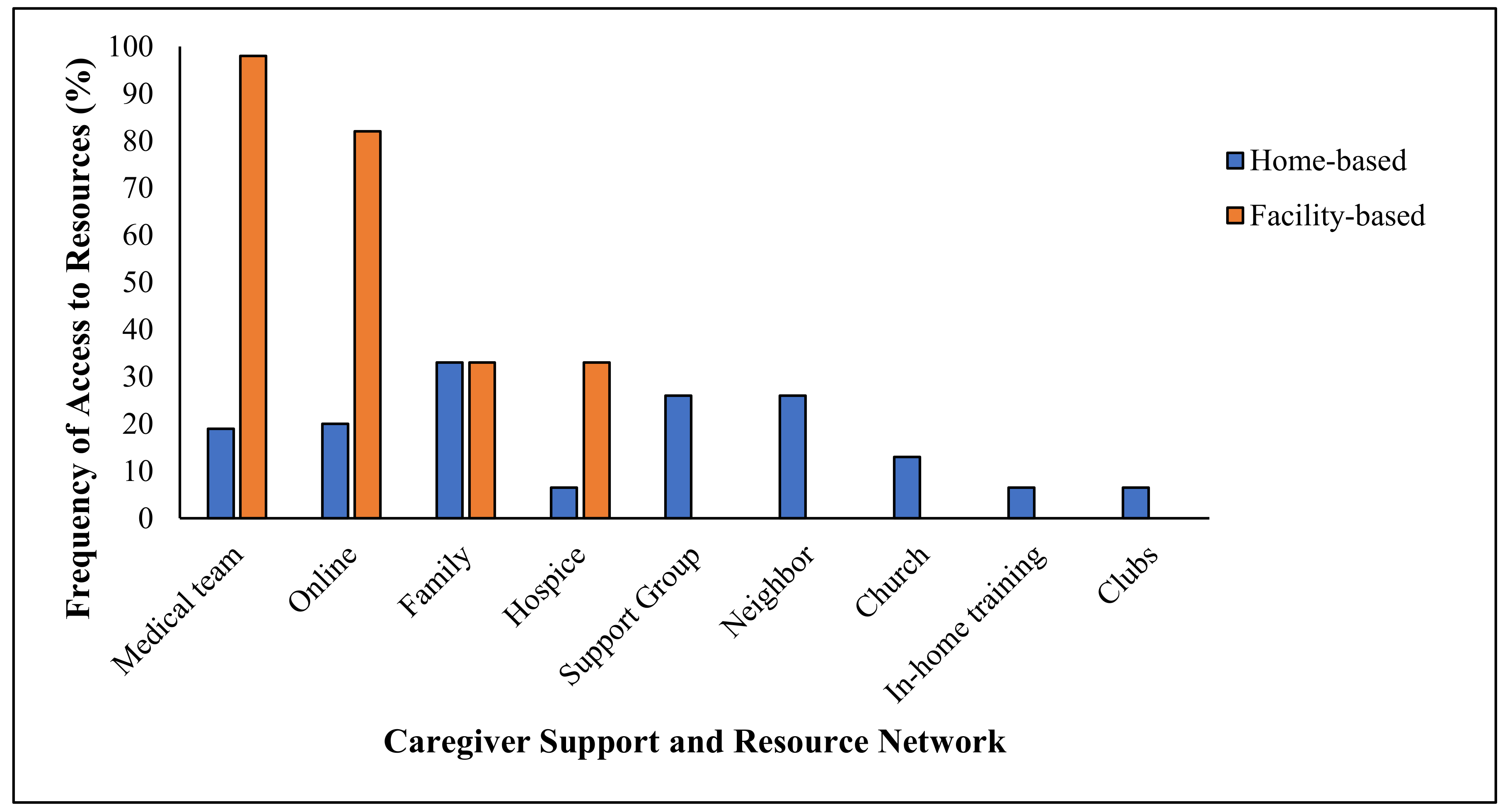
3.2. Resources for Caregivers
3.3. Triggers
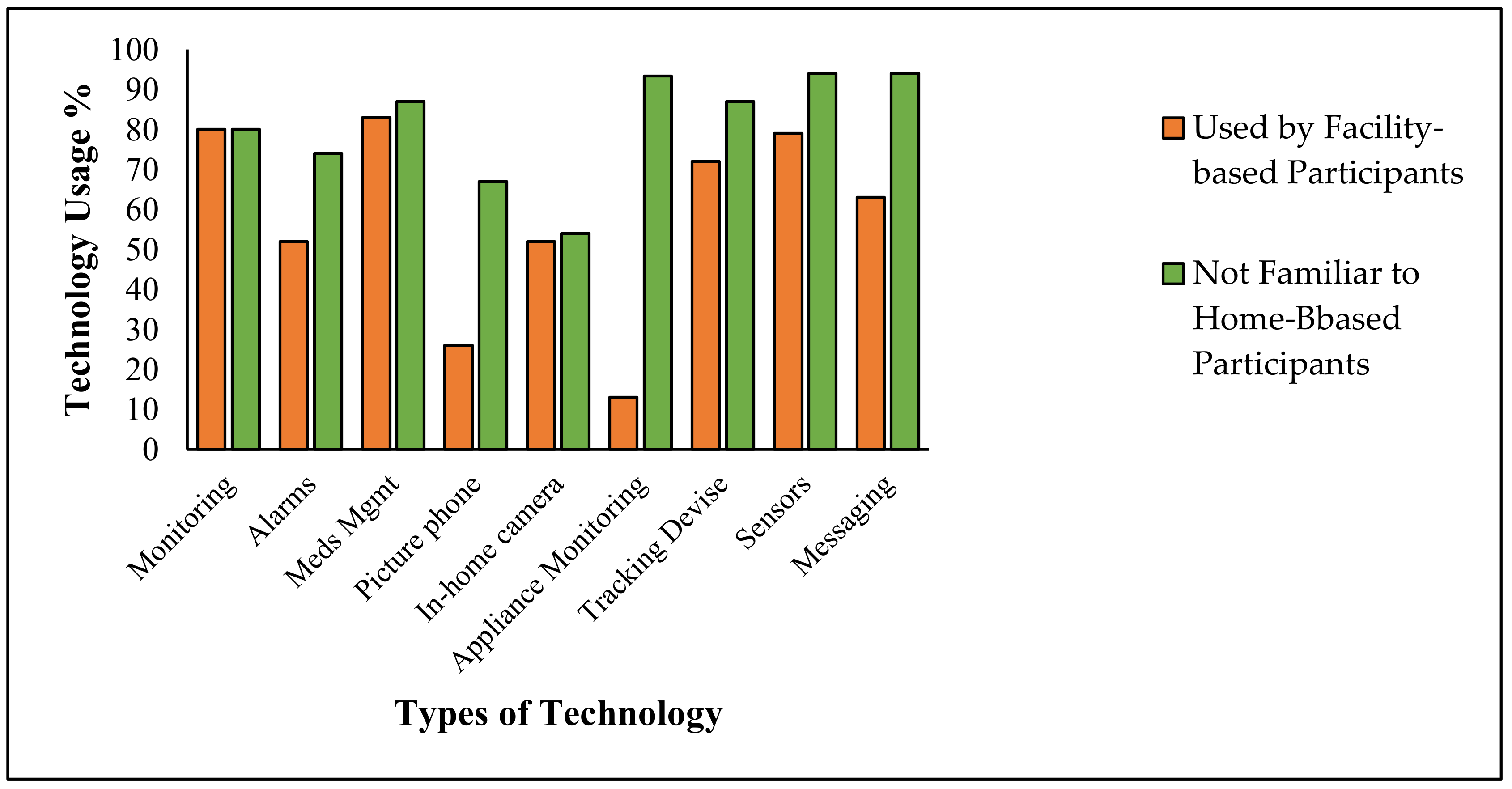
3.4. Awareness of Dementia-Based Technology
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
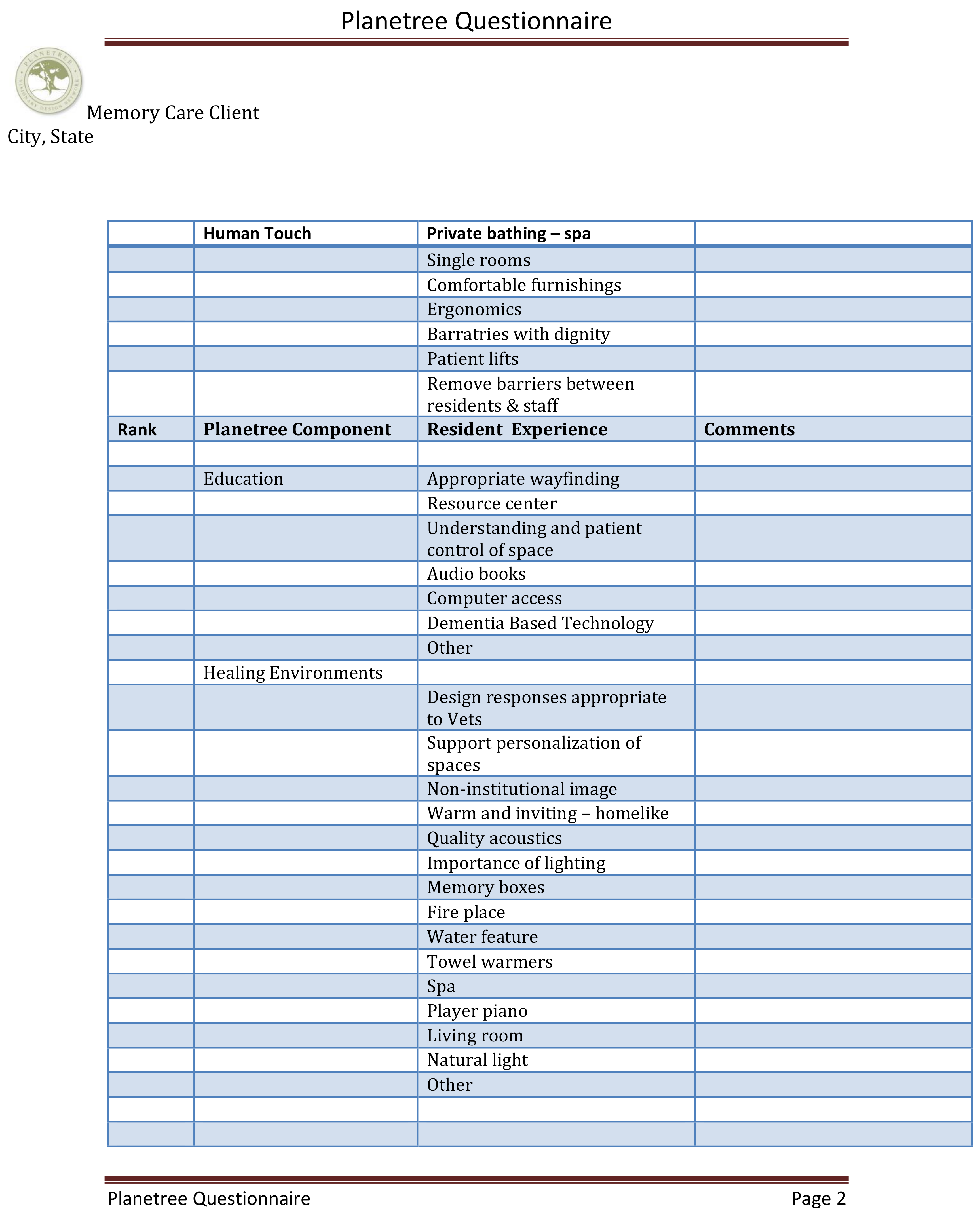
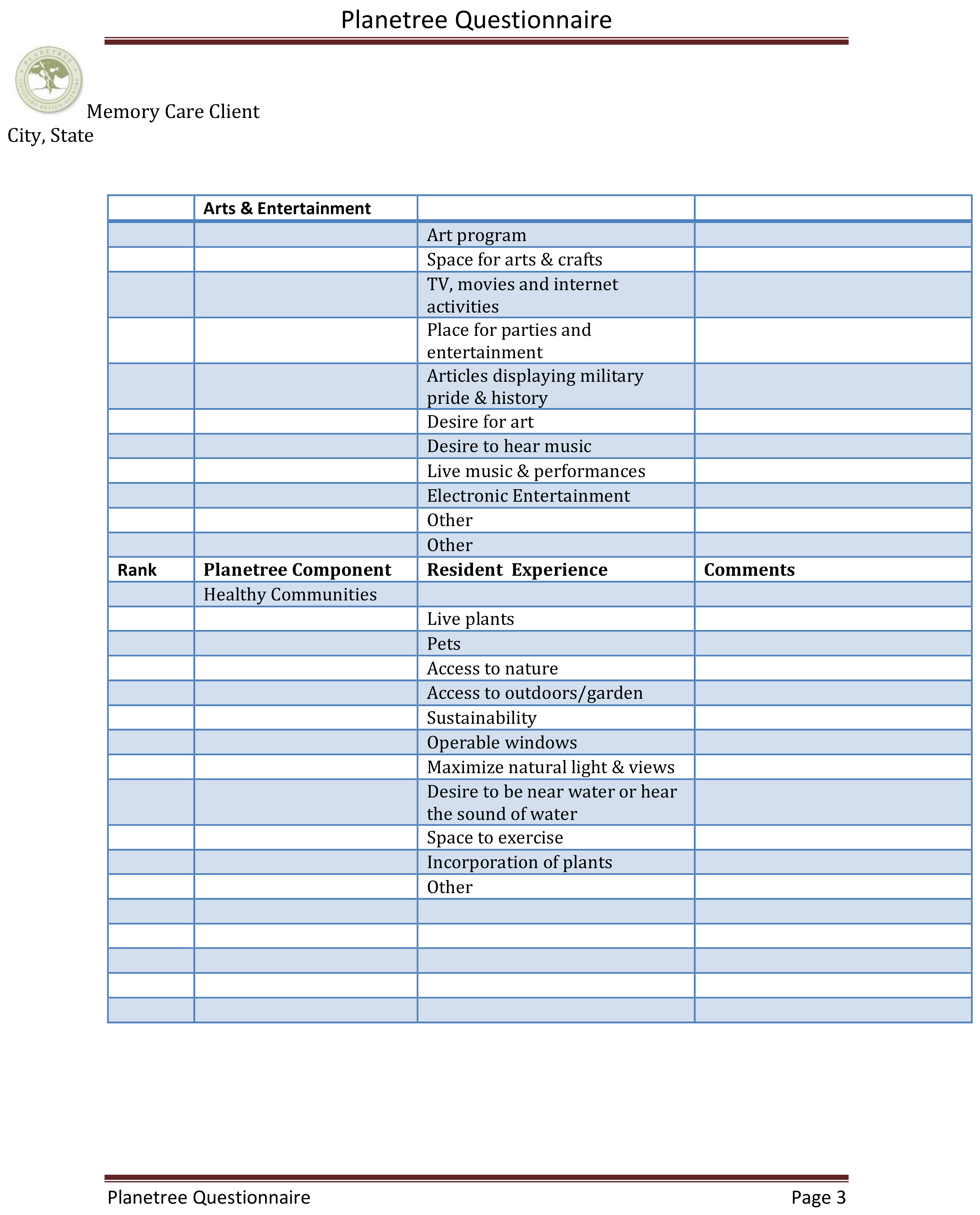
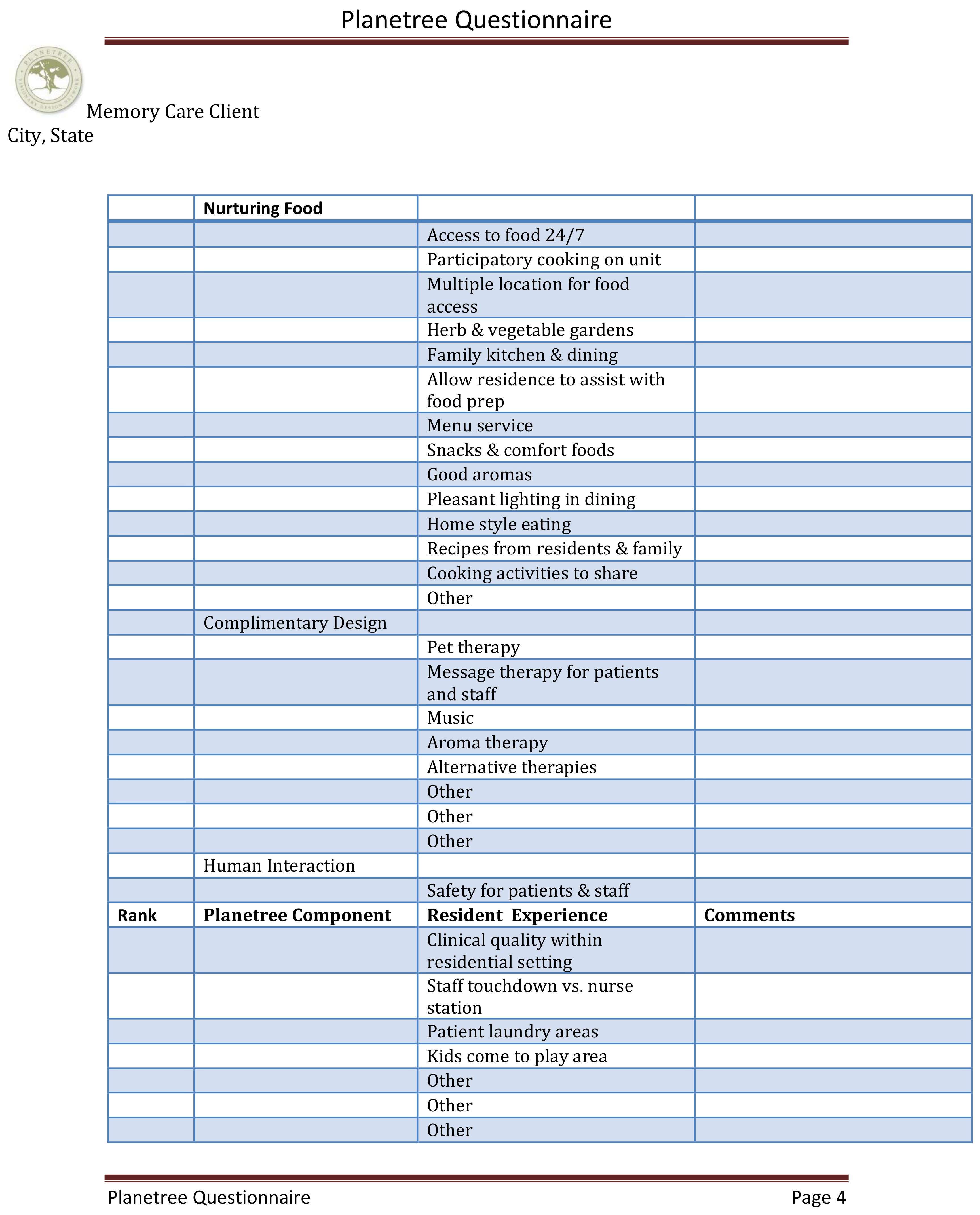
Appendix A
- Primary caregiver:
- Age
- Gender
- Care environment
- Who did you care for?
- Diagnosis:
- Symptoms:
- Med Mgmt.
- Memory Loss
- Personal Hygiene
- Mood Swings
- Disruptive Behavior
- Sleep Disturbance
- Incontinence
- Wandering
- Paranoia
- Sundowning
- Eating Problems
- Choking
- Other
- Most stressful dementia symptom? (Identify level of stress 1–10: 10 being the most stressful.)
Symptom Most Stressful Trigger Intervention Med Mgmt. Memory Loss Personal Hygiene Mood Swings Disruptive Behavior Sleep Disturbance Incontinence Wandering Paranoia Sundowning Eating Problems Choking Other - Were you prepared for this?
- How?
- What was the most difficult part of caregiving?
- What was your greatest concern/worry?
- What support resources did you access?
- Medical teams/doctors
- Online resources
- Family
- Friends
- Hospice
- Support groups
- Neighbors
- Church
- In-home training
- Clubs and organization
- Other
- Did you have in-home help or assistance?
- Family
- Neighbors
- Home health agency
- Professional medical team
- Hospice
- Church and volunteer organization
- Other
- Where did you find dementia support or caregiving advise?
- Family
- Neighbors
- Home health agency
- Professional medical team
- Hospice
- Church and volunteer organization
- Other
- Where did you find health care support?
- Family
- Neighbors
- Home health agency
- Professional medical team
- Hospice
- Church and volunteer organization
- Other
- What technology assistance have you used?
Technology Used Known about but Not Used Unknown Room Monitoring Alarms Medical management technology Picture phones In home cameras Appliance monitoring Tracking devises Body sensors Messaging devices Robotics Virtual reality entertainment Day clocks Music therapy Digital memory box Other - Were there financial concerns?
- Understand what care, services, equipment, drugs cost
- Insurance
- Forms
- Resources
- Was there an impact on your own health, well-being?
- What did you do for your own self-care?
- What kind of help did you need?
- What would you recommend for other caregivers?
References
- Ferraro, D.; Fiori, G. The Aging of the Baby Boomers: Demographics and Propagation of Tax Shocks. Am. Econ. J. Macroecon. 2020, 12, 167–193. [Google Scholar] [CrossRef]
- Hayashi, J.; Hayashi, J.; DeCherrie, L.; Ratner, E.; Boling, P.A. Workforce Development in Geriatric Home Care. Clin. Geriatr. Med. 2009, 25, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Kalambi, M.D. Caring for the Caregivers Through Healthy Human Resource Practices: The Caregivers. Int. J. Technol. Hum. Interact. 2020, 16, 1–7. [Google Scholar] [CrossRef]
- Flaherty, E.; Bartels, S.J. Addressing the Community-Based Geriatric Healthcare Workforce Shortage by Leveraging the Potential of Interprofessional Teams. J. Am. Geriatr. Soc. 2019, 67, S400–S408. [Google Scholar] [CrossRef]
- Edelstein, R.H.; Lacayo, A.J. Forecasting Seniors Housing Demand. In Seniors Housing; Anikeeff, M.A., Mueller, G.R., Eds.; Springer US: Boston, MA, USA, 1998; pp. 205–235. [Google Scholar] [CrossRef]
- Livingston, G.; Sommerlad, A.; Orgeta, V.; Costafreda, S.G.; Huntley, J.; Ames, D.; Ballard, P.C.; Banerjee, P.S.; Burns, P.A.; Cooper, C. Dementia prevention, intervention, and care. The Lancet 2017, 390, 2673–2734. [Google Scholar] [CrossRef]
- Gaugler, J.; Alzheimer’s Association. 2019 Alzheimer’s disease facts and figures. Alzheimers Dement. 2019, 15, 321–387. [Google Scholar] [CrossRef]
- Higgins, P.; Vyas, L. The policies, practices and predicaments of senior employment in Hong Kong and Singapore. Ageing Soc. 2018, 38, 1715–1739. [Google Scholar] [CrossRef]
- Alzheimer’s Association, A.S. 2018 Alzheimer’s disease facts and figures. Alzheimer’s Dement. 2018, 14, 367–429. [Google Scholar] [CrossRef]
- World Health Organization and Alzheimer’s Disease International, Dementia: A Public Health Priority. 2012. Available online: https://www.who.int/mental_health/publications/dementia_report_2012/en/ (accessed on 15 May 2020).
- Berenson, R.A.; Hammons, T.; Gans, D.N.; Zuckerman, S.; Merrell, K.; Underwood, W.S.; Williams, A.F. A House Is Not A Home: Keeping Patients At The Center Of Practice Redesign. Health Affairs 2008, 27, 1219–1230. [Google Scholar] [CrossRef]
- Karlsen, C.; Ludvigsen, M.S.; Moe, C.E.; Haraldstad, K.; Thygesen, E. Experiences of community-dwelling older adults with the use of telecare in home care services. JBI Database Syst. Rev. Implement. Rep. 2017, 15, 2913–2980. [Google Scholar] [CrossRef]
- Wan, T. A Pilot Study on Health-Related Quality of Life and Caregiving Burden of Caregivers. for Dementia: A Cross-sectional Report on the Pre-Test Assessment Results. JJ Geronto 2016, 2, 16. [Google Scholar]
- Ory, M.G.; Hoffman III, R.R.; Yee, J.L.; Tennstedt, S.; Schulz, R. Prevalence and Impact of Caregiving: A Detailed Comparison Between Dementia and Nondementia Caregivers. Gerontologist 1999, 39, 177–186. [Google Scholar] [CrossRef] [PubMed]
- Swinkels, J.; Tilburg, T.V.; Verbakel, E.; Broese van Groenou, M. Explaining the Gender Gap in the Caregiving Burden of Partner Caregivers. J. Gerontol. Ser. B-Psychol. Sci. Soc. Sci. 2019, 74, 309–317. [Google Scholar] [CrossRef]
- George, E.S.; Kecmanovic, M.; Meade, T.; Kolt, G.S. Psychological distress among carers and the moderating effects of social support. BMC Psychiatry 2020, 20, 9. [Google Scholar] [CrossRef]
- Polenick, C.A.; Struble, L.M.; Stanislawski, B.; Turnwald, M.; Broderick, B.; Gitlin, L.N.; Kales, H.C. I’ve learned to just go with the flow”: Family caregivers’ strategies for managing behavioral and psychological symptoms of dementia. Dement.-Int. J. Soc. Res. Pract. 2020, 19, 590–605. [Google Scholar] [CrossRef]
- Han, J.; Guo, G.F.; Hong, L. Impact of professionally facilitated peer support for family carers of people with dementia in a WeChat virtual community. J. Telemed. Telecare 2020, 9. [Google Scholar] [CrossRef]
- Gaugler, J.E.; Yu, F.; Krichbaum, K.; Wyman, J.F. Predictors of Nursing Home Admission for Persons with Dementia. Med. Care 2009, 47, 191–198. [Google Scholar] [CrossRef]
- Ministry of Health and Care Services. A More Dementia-Friendly Society in Demens Plan. 2020. Available online: https://www.regjeringen.no/contentassets/3bbec72c19a04af88fa78ffb02a203da/dementia_-plan_2020_long.pdf (accessed on 15 May 2020).
- Huelat, B. Healing Environments What’s the Proof? Medezyn Books: Alexandria, VA, USA, 2007. [Google Scholar]
- Frampton, S.B.; Charmel, P.A. Putting Patients First: Best Practices in Patient-Centered Care; John Wiley & Sons: Hoboken, NJ, USA, 2009; Volume 38. [Google Scholar]
- Morley, J.E.J. The American Medical Directors Association: The State of the Journal. J. Am. Med. Dir. Assoc. 2012, 13, 571–573. [Google Scholar] [CrossRef]
- Gillespie, R.; Mullan, J.; Harrison, L. Managing medications: The role of informal caregivers of older adults and people living with dementia. A review of the literature. J. Clin. Nurs. 2014, 23, 3296–3308. [Google Scholar] [CrossRef]
- Naismith, S.L.; Rogers, N.L.; Hickie, I.B.; Mackenzie, J.; Norrie, L.M.; Lewis, S.J.G. Sleep Well, Think Well: Sleep-Wake Disturbance in Mild Cognitive Impairment. J. Geriatr. Psychiatry Neurol. 2010, 23, 123–130. [Google Scholar] [CrossRef]
- Bozoki, A.; Giordani, B.; Heidebrink, J.L.; Berent, S.; Foster, N.L. Mild Cognitive Impairments Predict Dementia in Nondemented Elderly Patients With Memory Loss. Arch. Neurol. 2001, 58, 411–416. [Google Scholar] [CrossRef] [PubMed]
- Rader, J.; Barrick, A.L.; Hoeffer, B.; Sloane, P.D.; McKenzie, D.; Talerico, K.A.; Glover, J.U. The Bathing Of Older Adults with Dementia: Easing the unnecessarily unpleasant aspects of assisted bathing. AJN Am. J. Nurs. 2006, 106, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Rheingold, H. The Virtual Community, Virtual Reality, Tools for Thought. In The Heart of the WELL; MIT Press: Boston, MA, USA, 2019. [Google Scholar]
- Stone, S. A Retrospective Evaluation of the Impact of the Planetree Patient-Centered Model of Care on Inpatient Quality Outcomes. Herd-Health Environ. Res. Des. J. 2008, 1, 55–69. [Google Scholar] [CrossRef] [PubMed]
- Bharucha, A.J.; Anand, V.; Forlizzi, J.; Dew, M.A.; Reynolds III, C.F.; Stevens, S.; Wactlar, H. Intelligent Assistive Technology Applications to Dementia Care: Current Capabilities, Limitations, and Future Challenges. Am. J. Geriatr. Psychiatry 2009, 17, 88–104. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.K.; Park, M. Effectiveness of person-centered care on people with dementia: A systematic review and meta-analysis. Clin. Interv. Aging 2017, 12, 381–397. [Google Scholar] [CrossRef] [PubMed]
- Dawson, A.; Bowes, A.; Kelly, F.; Velzke, K.; Ward, R. Evidence of what works to support and sustain care at home for people with dementia: A literature review with a systematic approach. BMC Geriatr. 2015, 15. [Google Scholar] [CrossRef]
- Constand, M.K.; MacDermid, J.C.; Dal Bello-Haas, V.; Law, M. Scoping review of patient-centered care approaches in healthcare. BMC Health Serv. Res. 2014, 14, 271. [Google Scholar] [CrossRef]
- Gilpin, L. The Planetree Model: Its Impact on Caring for Those With Dementia. Alzheimer’s Care Today 2006, 7, 273–277. [Google Scholar]
- Anåker, A.; Heylighen, A.; Nordin, S.; Elf, M. Design Quality in the Context of Healthcare Environments: A Scoping Review. HERD: Health Environ. Res. Des. J. 2017, 10, 136–150. [Google Scholar] [CrossRef]
- Hall, G.R. Progressively lowered stress threshold; A conceptual model for care of adults with Alzheimer’s disease. Arch. Psychiatr. Nurs. 1987, 1, 399–406. [Google Scholar]
- Wan, T. Convergence of Artificial Intelligence Research in Healthcare: Trends and Approaches Transactions of the SDPS. 2020. forthcoming. [Google Scholar] [CrossRef]

| Caregiver | Age | Gender | Relationship | Diagnosis | Care Environment |
|---|---|---|---|---|---|
| 1 | 82 | Male | Wife | Alzheimer’s | In-home with spouse |
| 2 | 69 | Female | Husband | Parkinson’s | In-home with spouse |
| 3 | 42 | Female | Friend | Trauma | Daycare in friend’s home |
| 4 | 60 | Female | Mother | Stroke | In-home with mother |
| 5 | 70 | Male | Wife | Brain tumor | In-home with spouse |
| 6 | 68 | Female | Husband | Alzheimer’s | In-home with spouse |
| 7 | 60 | Female | Mother | Parkinson’s | Daycare in mother’s home |
| 8 | 55 | Female | Mother-in-law | Parkinson’s | Daycare in mother’s home |
| 9 | 58 | Female | Father | Alzheimer’s | In-home care in caregiver’s home |
| 10 | 64 | Female | Husband | Alzheimer’s | In-home care with spouse |
| 11 | 76 | Female | Husband | Alzheimer’s | In-home care with spouse |
| 12 | 58 | Female | Mother | Alzheimer’s | Daycare in mother’s home |
| 13 | 83 | Female | Husband | Vascular dementia | In-home care with spouse |
| 14 | 74 | Female | Husband | PCA dementia | In-home care with spouse |
| 15 | 80 | Female | Husband | Dementia, COPD, diabetes | In-home care with spouse |
| Facility ID | Caregiving Team | Facility Environment | Region | Resident |
|---|---|---|---|---|
| A | Nurse Mgr, Program director, Env Services, Planetree coordinator, Admin, Physician | 2, 16-bedroom memory care households within hospital renovation | East Coast | 32 men |
| B | Nurse Mgr, Program director, Planetree coordinator, Admin, Physician | 2, 16-bedroom households, 1 memory care and 1 hospice, new construction, free standing facility | East Coast | 32 men |
| C | Nurse Mgr, Program director, Planetree coordinator, Admin, Physician | 2, 16-bedroom households of free-standing new memory care | East Coast = | 32 women |
| D | Nurse Mgr, Program director, Eden Alternative director, Admin, Physician | 4, 14-bedroom households of memory care, free standing new construction | Rocky Mt | 56 men |
| E | Nurse Mgr, Program director, Planetree coordinator, Admin, Physician | 4, 14-bedroom households of memory care, free standing new construction | East Coast | 56 men |
| F | Nurse Mgr., Admin, Physician | 4, 16-bedroom households of memory care, free standing new construction | Midwest | 65 residents of mix men and women |
| G | Nurse Mgr., Admin, Physician | 2, 16-bedroom household of memory care within a CCRC new construction | Midwest | 34 residents of mix men and women |
| Class of Stress Relief | Example | Speaker |
|---|---|---|
| Resources | “Are there any resources that can help with the care, people, products, places? Don’t tell me to call X after the fact… I didn’t know that X even existed.” | Caregiver 8 |
| Information regarding disease progression | “What is it? “How to manage it? What are the symptoms and triggers? What happens next?” | Caregiver 6 |
| Empowerment | “If you are asking me to manage this illness, pay attention to me, I know what I am talking about, I live with it.” | Caregiver 2 |
| Knowledge of costs | “Why is the medical system so complex, I don’t understand the forms and especially what something cost until after they send a bill.” | Caregiver 4 |
| Training | “Help me understand how to use the equipment. Not just the use, but what do I do if something goes wrong?” | Caregiver 3 |
| Knowledge | “I wish I knew about hospice services much earlier. Social workers at the hospital could have discussed this with me when we had the dire diagnosis, right at the beginning. The promotion of hospice should be focused on hospice as a more patient-centered way of managing long-term health care, not just a place where you take your loved one to die. The big point for my wife was to reduce significantly the trips to the hospital.” | Caregiver 5 |
| Technology | PCC Benefit |
|---|---|
| Virtual Assistants | Virtual assistants such as smart devices (e.g., Amazon’s Alexa) allow a user to command or ask questions, such that the device then responds to the task. This technology, which can turn on lights and control climates, could address toileting and hygiene issues. Using artificial intelligence, the technology can “learn” to recognize voices and identify better ways to help. New programming could identify innovative purposes and functions. These technologies can lighten the caregiver burden. As these technologies move forward in development, human-centric qualities must be seamlessly integrated [33]. |
| Robots | Robotic technology is growing and promises meaningful solutions for dementia-based technology. Robotic vacuum cleaners use artificial intelligence to assist caregivers and provide entertainment for those who are wheelchair or bed bound [35]. |
| Virtual Reality | Early research has demonstrated a positive experience for those exposed to a virtual reality environment by recalling old memories, reducing aggression and improving their interaction with caregivers. VR has also proved useful in training the caregiver and providing entertainment without leaving the home [33,34]. |
| Music Technologies | The National Institute of Health has awarded $20M to support the first research project of the Sound Health initiative in order to explore the potential of music for treating a wide range of conditions, including dementia. “We hope that these in-depth studies of the science behind music’s influence and impact on the brain will bring real understanding of something we know anecdotally—that music is good for you!” [36]. |
| Internet of Things | Smart technology and the new wave of connected technology can help people with dementia live independently for longer. This new wave of connected technologies, nicknamed “the internet of things,” offers hope for dementia support. Connecting sensors with coordinated care that can collect and process data could help solve the problems of managing the disease and caring for the patient and caregiver [36,37]. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huelat, B.; Pochron, S.T. Stress in the Volunteer Caregiver: Human-Centric Technology Can Support Both Caregivers and People with Dementia. Medicina 2020, 56, 257. https://doi.org/10.3390/medicina56060257
Huelat B, Pochron ST. Stress in the Volunteer Caregiver: Human-Centric Technology Can Support Both Caregivers and People with Dementia. Medicina. 2020; 56(6):257. https://doi.org/10.3390/medicina56060257
Chicago/Turabian StyleHuelat, Barbara, and Sharon T. Pochron. 2020. "Stress in the Volunteer Caregiver: Human-Centric Technology Can Support Both Caregivers and People with Dementia" Medicina 56, no. 6: 257. https://doi.org/10.3390/medicina56060257
APA StyleHuelat, B., & Pochron, S. T. (2020). Stress in the Volunteer Caregiver: Human-Centric Technology Can Support Both Caregivers and People with Dementia. Medicina, 56(6), 257. https://doi.org/10.3390/medicina56060257