Effects of Immunonutrition on Comprehensive Complication Index in Patients Undergoing Pancreatoduodenectomy
Abstract
1. Introduction
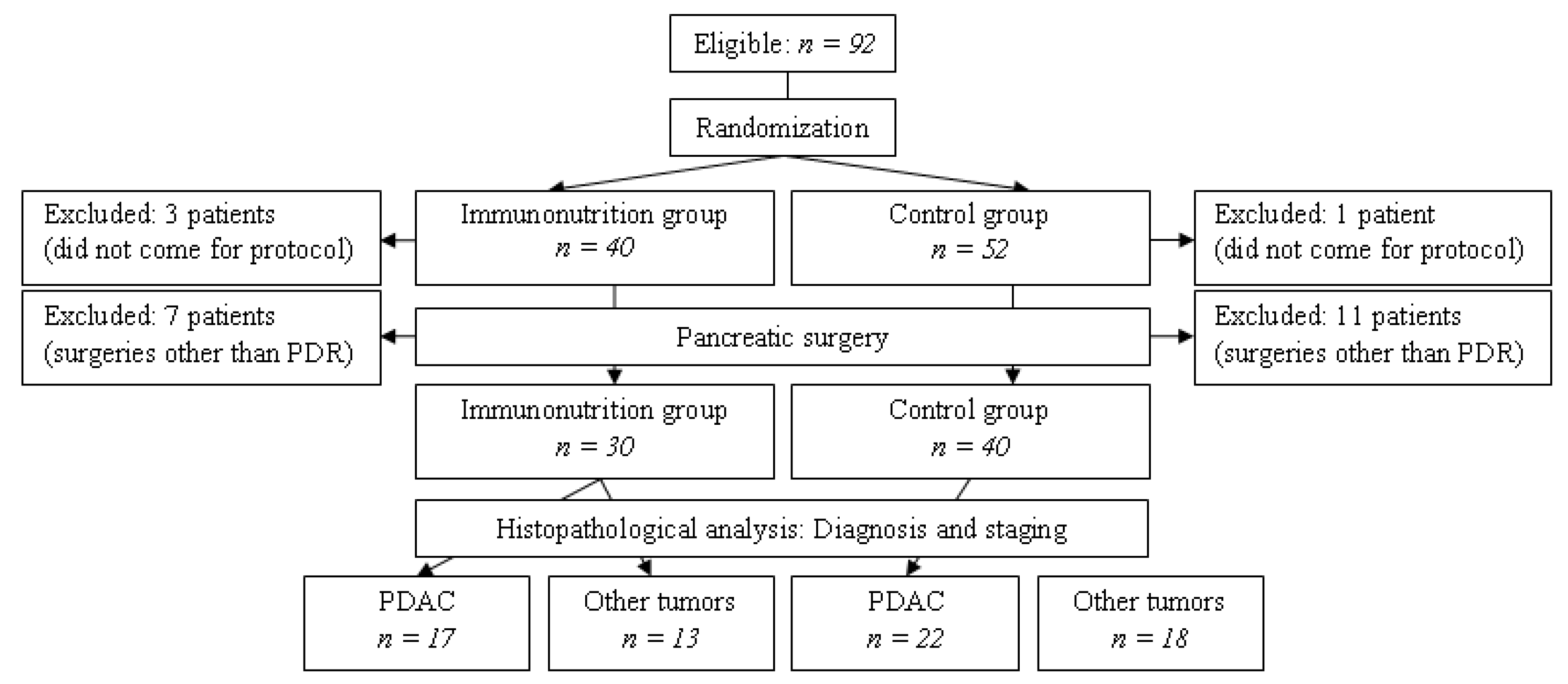
2. Materials and Methods
2.1. Patients and Data
- (1)
- The first (immunonutrition) group received 5 days of preoperative immunonutrition (L-arginine 6.04 g/day and polyunsaturated fat 4 g/day) in addition to the usual preoperative nutritional management;
- (2)
- The second (control) group received a routine preoperative nutritional management only.
2.2. Statistical Analysis
3. Results
3.1. Characteristics of Patients
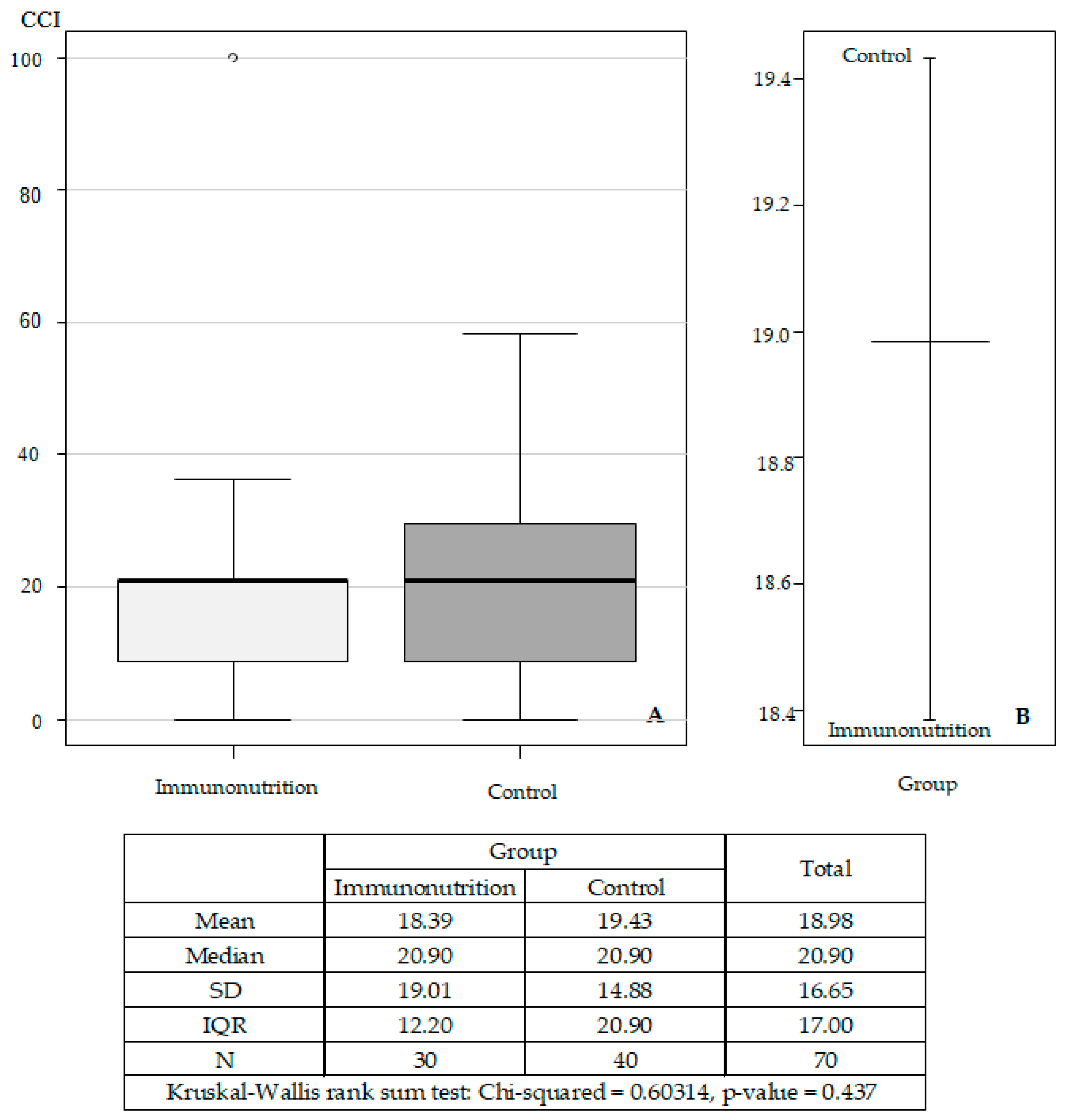
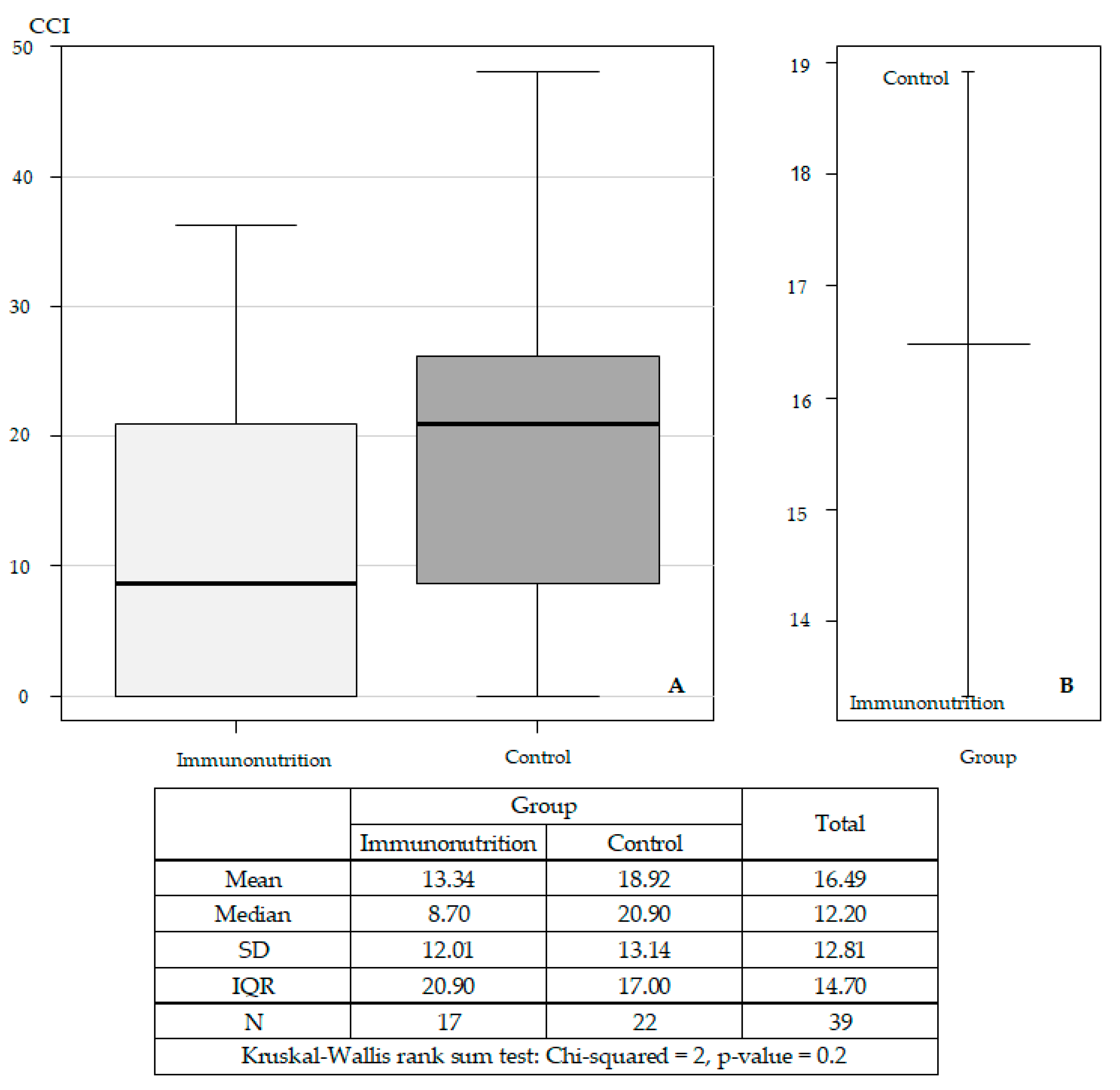
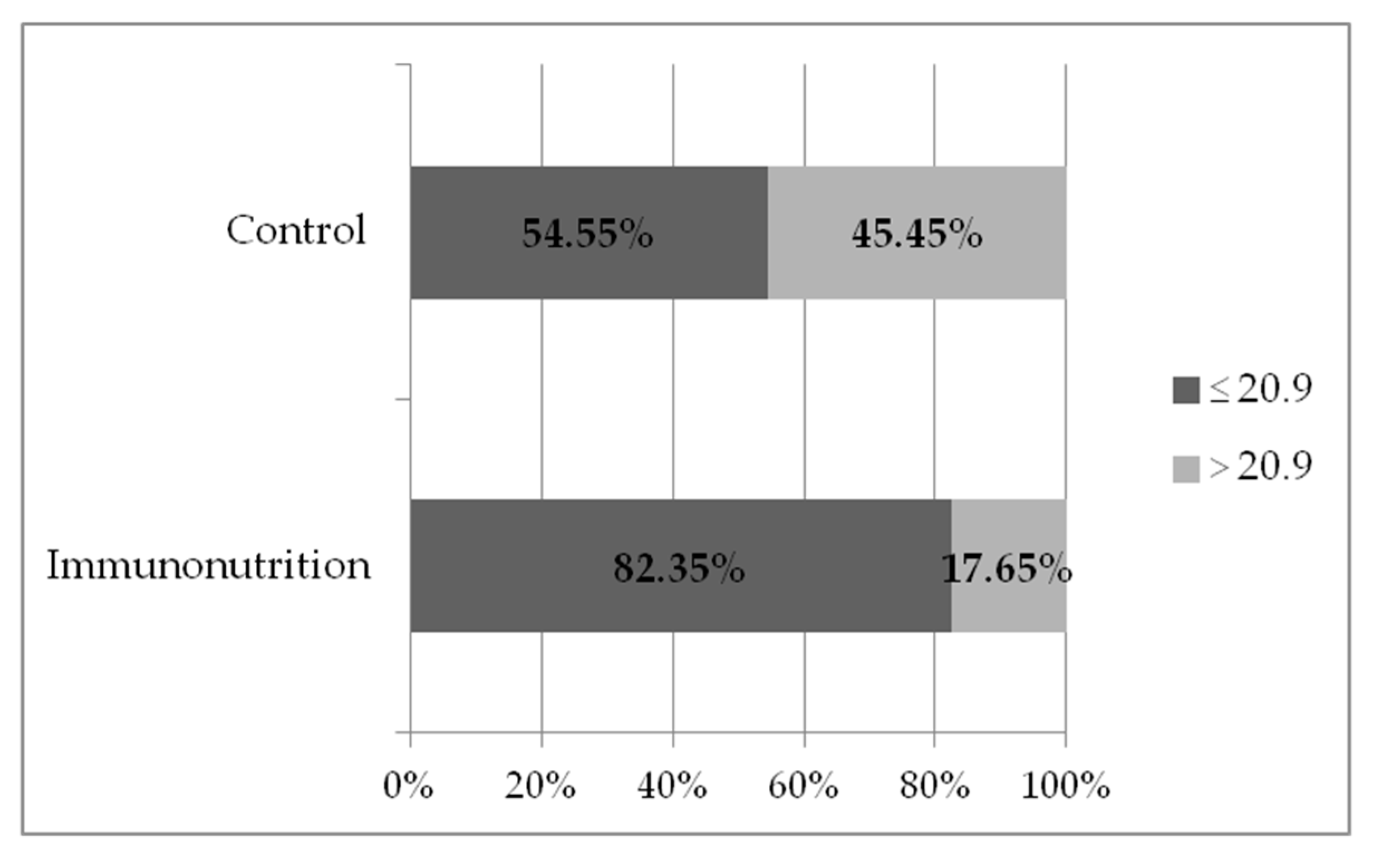
3.2. Surgical Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| PDAC | pancreatic ductal adenocarcinoma |
References
- Santilli, V.; Bernetti, A.; Mangone, M.; Paoloni, M. Clinical definition of sarcopenia. Clin. Cases Miner. Bone Metab. 2014, 11, 177–180. [Google Scholar] [CrossRef]
- Jourdan, C.; Petersen, A.K.; Gieger, C.; Döring, A.; Illig, T.; Wang-Sattler, R.; Meisinger, C.; Peters, A.; Adamski, J.; Prehn, C.; et al. Body fat free mass is associated with the serum metabolite profile in a population-based study. PLoS ONE 2012, 7, e40009. [Google Scholar] [CrossRef]
- Tomar, N.; De, R.K. Cross Talk Between the Metabolic and Immune Systems. Methods Mol. Biol. 2014, 1184, 13–21. [Google Scholar] [CrossRef]
- Braga, M.; Wischmeyer, P.E.; Drover, J.; Heyland, D.K. Clinical evidence for pharmaconutrition in major elective surgery. J. Parenter. Enter. Nutr. 2013, 37, S66–S72. [Google Scholar] [CrossRef]
- Gaudillière, B.; Fragiadakis, G.K.; Bruggner, R.V.; Nicolau, M.; Finck, R.; Tingle, M.; Silva, J.; Ganio, E.A.; Yeh, C.G.; Maloney, W.J.; et al. Clinical recovery from surgery correlates with single-cell immune signatures. Sci. Transl. Med. 2014, 6, 255ra131. [Google Scholar] [CrossRef]
- Alazawi, W.; Pirmadjid, N.; Lahiri, R.; Bhattacharya, S. Inflammatory and Immune Responses to Surgery and Their Clinical Impact. Ann. Surg. 2016, 264, 73–80. [Google Scholar] [CrossRef]
- Suzuki, D.; Furukawa, K.; Kimura, F.; Shimizu, H.; Yoshidome, H.; Ohtsuka, M.; Kato, A.; Yoshitomi, H.; Miyazaki, M. Effects of perioperative immunonutrition on cell-mediated immunity, T helper type 1 (Th1)/Th2 differentiation, and Th17 response after pancreaticoduodenectomy. Surgery 2010, 148, 573–581. [Google Scholar] [CrossRef]
- Hamza, N.; Darwish, A.; O’Reilly, D.A.; Denton, J.; Sheen, A.J.; Chang, D.; Sherlock, D.J.; Ammori, B.J. Perioperative Enteral Immunonutrition Modulates Systemic and Mucosal Immunity and the Inflammatory Response in Patients With Periampullary Cancer Scheduled for Pancreaticoduodenectomy: A Randomized Clinical Trial. Pancreas 2015, 44, 41–52. [Google Scholar] [CrossRef]
- Hübner, M.; Cerantola, Y.; Grass, F.; Bertrand, P.C.; Schäfer, M.; Demartines, N. Preoperative immunonutrition in patients at nutritional risk: Results of a double-blinded randomized clinical trial. Eur. J. Clin. Nutr. 2012, 66, 850–855. [Google Scholar] [CrossRef]
- Lassen, K.; Coolsen, M.M.; Slim, K.; Carli, F.; de Aguilar-Nascimento, J.E.; Schäfer, M.; Parks, R.W.; Fearon, K.C.; Lobo, D.N.; Demartines, N.; et al. Enhanced Recovery After Surgery (ERAS) Society, for Perioperative Care; European Society for Clinical nutrition and Metabolism (ESPEN); International Association for Surgical Metabolism and Nutrition (IASMEN): Guidelines for perioperative care for pancreaticoduodenectomy: Enhanced Recovery After Surgery (ERAS®) Society recommendations.ERAS® Society; European Society for Clinical Nutrition and Metabolism; International Association for Surgical Metabolism and Nutrition. Clin. Nutr. 2012, 31, M817–M830. [Google Scholar] [CrossRef]
- Guan, H.; Chen, S.; Huang, Q. Effects of Enteral Immunonutrition in Patients Undergoing Pancreaticoduodenectomy: A Meta-Analysis of Randomized Controlled Trials. Ann. Nutr. Metab. 2019, 74, 53–61. [Google Scholar] [CrossRef]
- Miyauchi, Y.; Furukawa, K.; Suzuki, D.; Yoshitomi, H.; Takayashiki, T.; Kuboki, S.; Miyazaki, M.; Ohtsuka, M. Additional effect of perioperative, compared with preoperative, immunonutrition after pancreaticoduodenectomy: A randomized, controlled trial. Int. J. Surg. 2019, 61, 69–75. [Google Scholar] [CrossRef]
- Silvestri, S.; Franchello, A.; Deiro, G.; Galletti, R.; Cassine, D.; Campra, D.; Bonfanti, D.; De Carli, L.; Fop, F.; Fronda, G.R. Preoperative oral immunonutrition versus standard preoperative oral diet in well nourished patients undergoing pancreaticoduodenectomy. Int. J. Surg. 2016, 31, 93–99. [Google Scholar] [CrossRef]
- Gade, J.; Levring, T.; Hillingsø, J.; Hansen, C.P.; Andersen, J.R. The Effect of Preoperative Oral Immunonutrition on Complications and Length of Hospital Stay After Elective Surgery for Pancreatic Cancer—A Randomized Controlled Trial. Nutr. Cancer 2016, 68, 225–233. [Google Scholar] [CrossRef] [PubMed]
- Martin, R.C., 2nd; Agle, S.; Schlegel, M.; Hayat, T.; Scoggins, C.R.; McMasters, K.M.; Philips, P. Efficacy of preoperative immunonutrition in locally advanced pancreatic cancer undergoing irreversible electroporation (IRE). Eur. J. Surg. Oncol. 2017, 43, 772–779. [Google Scholar] [CrossRef] [PubMed]
- Adiamah, A.; Skořepa, P.; Weimann, A.; Lobo, D.N. The Impact of Preoperative Immune Modulating Nutrition on Outcomes in Patients Undergoing Surgery for Gastrointestinal Cancer: A Systematic Review and Meta-analysis. Ann. Surg. 2019, 270, 247–256. [Google Scholar] [CrossRef]
- Kim, T.H.; Suh, Y.S.; Huh, Y.J.; Son, Y.G.; Park, J.H.; Yang, J.Y.; Kong, S.H.; Ahn, H.S.; Lee, H.J.; Slankamenac, K.; et al. The comprehensive complication index (CCI) is a more sensitive complication index than the conventional Clavien-Dindo classification in radical gastric cancer surgery. Gastric Cancer 2018, 21, 171–181. [Google Scholar] [CrossRef]
- Cederholm, T.; Barazzoni, R.; Austin, P.; Ballmer, P.; Biolo, G.; Bischoff, S.C.; Compher, C.; Correia, I.; Higashiguchi, T.; Holst, M.; et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin. Nutr. 2017, 36, 49–64. [Google Scholar] [CrossRef]
- Baracos, V.; Kazemi-Bajestani, S.M. Clinical outcomes related to muscle mass in humans with cancer and catabolic illnesses. Int. J. Biochem. Cell Biol. 2013, 45, 2302–2308. [Google Scholar] [CrossRef]
- Weimann, A.; Braga, M.; Carli, F.; Higashiguchi, T.; Hübner, M.; Klek, S.; Laviano, A.; Ljungqvist, O.; Lobo, D.N.; Martindale, R.; et al. ESPEN guideline: Clinical nutrition in surgery. Clin. Nutr. 2017, 36, 623–650. [Google Scholar] [CrossRef]
- Slankamenac, K.; Graf, R.; Barkun, J.; Puhan, M.A.; Clavien, P.A. The Comprehensive Complication Index. A Novel Continuous Scale to Measure Surgical Morbidity. Ann. Surg. 2013, 258, 1–7. [Google Scholar] [CrossRef]
- Burden, S.; Todd, C.; Hill, J.; Lal, S. Pre-operative nutrition support in patients undergoing gastrointestinal surgery. Cochrane Database Syst. Rev. 2012, 11, CD008879. [Google Scholar] [CrossRef]
- Hegazi, R.A.; Hustead, D.S.; Evans, D.C. Preoperative standard oral nutrition supplements vs immunonutrition: Results of a systematic review and meta-analysis. J. Am. Coll. Surg. 2014, 219, 1078–1087. [Google Scholar] [CrossRef]
- Reis, A.M.; Kabke, G.B.; Fruchtenicht, A.V.; Barreiro, T.D.; Moreira, L.F. Cost-effectiveness of perioperative immunonutrition in gastrointestinal oncologic surgery: A systematic review. Arq. Bras. Cir. Dig. 2016, 29, 121–125. [Google Scholar] [CrossRef]
- Klek, S.; Szybinski, P.; Szczepanek, K. Perioperative immunonutrition in surgical cancer patients: A summary of a decade of research. World J. Surg. 2014, 38, 803–812. [Google Scholar] [CrossRef]
- Wong, C.S.; Aly, E.H. The effects of enteral immunonutrition in upper gastrointestinal surgery: A systematic review and meta-analysis. Int. J. Surg. 2016, 29, 137–150. [Google Scholar] [CrossRef]
- Marimuthu, K.; Varadhan, K.K.; Ljungqvist, O.; Lobo, D.N. A meta-analysis of the effect of combinations of immune modulating nutrients on outcome in patients undergoing major open gastrointestinal surgery. Ann. Surg. 2012, 255, 1060–1068. [Google Scholar] [CrossRef]
- Mazaki, T.; Ishii, Y.; Murai, I. Immunoenhancing enteral and parenteral nutrition for gastrointestinal surgery: A multiple-treatments meta-analysis. Ann. Surg. 2015, 261, 662–669. [Google Scholar] [CrossRef]
- Yan, X.; Zhou, F.X.; Lan, T.; Xu, H.; Yang, X.X.; Xie, C.H.; Dai, J.; Fu, Z.M.; Gao, Y.; Chen, L.L. Optimal postoperative nutrition support for patients with gastrointestinal malignancy: A systematic review and meta-analysis. Clin. Nutr. 2017, 36, 710–721. [Google Scholar] [CrossRef]
- Song, G.M.; Tian, X.; Zhang, L.; Ou, Y.X.; Yi, L.J.; Shuai, T.; Zhou, J.G.; Zeng, Z.; Yang, H.L. Immunonutrition Support for Patients Undergoing Surgery for Gastrointestinal Malignancy: Preoperative, Postoperative, or Perioperative? A Bayesian Network Meta-Analysis of Randomized Controlled Trials. Medicine (Baltimore) 2015, 94, e1225. [Google Scholar] [CrossRef]
- Klek, S.; Sierzega, M.; Szybinski, P.; Szczepanek, K.; Scislo, L.; Walewska, E.; Kulig, J. The immunomodulating enteral nutrition in malnourished surgical patients—A prospective, randomized, double-blind clinical trial. Clin. Nutr. 2011, 30, 282–288. [Google Scholar] [CrossRef] [PubMed]
- de la Plaza Llamas, R.; Ramia Ángel, J.M.; Bellón, J.M.; Peralta, V.A.; Amador, C.G.; Marcano, A.L.; Velasco, A.M.; Sierra, B.G.; Vázquez, A.M. Clinical Validation of the Comprehensive Complication Index as a Measure of Postoperative Morbidity at a Surgical Department: A Prospective Study. Ann. Surg. 2018, 268, 838–844. [Google Scholar] [CrossRef] [PubMed]
- Slankamenac, K.; Nederlof, N.; Pessaux, P.; de Jonge, J.; Wijnhoven, B.P.L.; Breitenstein, S.; Oberkofler, C.E.; Graf, R.; Puhan, M.A.; Clavien, P.A. The comprehensive complication index: A novel and more sensitive endpoint for assessing outcome and reducing sample size in randomized controlled trials. Ann. Surg. 2014, 260, 757–763. [Google Scholar] [CrossRef]
- Poves, I.; Burdío, F.; Morató, O.; Iglesias, M.; Radosevic, A.; Ilzarbe, L.; Visa, L.; Grande, L. Comparison of Perioperative Outcomes Between Laparoscopic and Open Approach for Pancreatoduodenectomy: The PADULAP Randomized Controlled Trial. Ann. Surg. 2018, 268, 731–739. [Google Scholar] [CrossRef]
- Dumitra, S.; O’Leary, M.; Raoof, M.; Wakabayashi, M.; Dellinger, T.H.; Han, E.S.; Lee, S.J.; Lee, B. The Comprehensive Complication Index: A New Measure of the Burden of Complications After Hyperthermic Intraperitoneal Chemotherapy. Ann. Surg. Oncol. 2018, 25, 688–693. [Google Scholar] [CrossRef]
- Ying, H.; Dey, P.; Yao, W.; Kimmelman, A.C.; Draetta, G.F.; Maitra, A.; DePinho, R.A. Genetics and biology of pancreatic ductal adenocarcinoma. Genes Dev. 2016, 30, 355–385. [Google Scholar] [CrossRef]
- Inman, K.S.; Francis, A.A.; Murray, N.R. Complex role for the immune system in initiation and progression of pancreatic cancer. World J. Gastroenterol. 2014, 20, 11160–11181. [Google Scholar] [CrossRef]
- Holmer, R.; Goumas, F.A.; Waetzig, G.H.; Rose-John, S.; Kalthoff, H. Interleukin-6: A villain in the drama of pancreatic cancer development and progression. Hepatobiliary Pancreat Dis. Int. 2014, 13, 371–380. [Google Scholar] [CrossRef]

| Group | Immunonutrition | Control | Overall | Mann-Whitney | |||
|---|---|---|---|---|---|---|---|
| n = 30 | n = 40 | n = 70 | U test | ||||
| Statistics | Mean (SD) | Median (MAD) | Mean (SD) | Median (MAD) | Mean (SD) | Median (MAD) | U |
| p-Value | |||||||
| Effect Size R | |||||||
| Age (years) | 62.6 (10.5) | 61.5 (88.2) | 63.0 (8.7) | 61.5 (88.2) | 62.8 (9.43) | 61.5 (88.2) | U = 596.00 |
| p = 0.962 | |||||||
| r = −0.006 | |||||||
| Body mass index (kg/m²) | 26.8 (5.6) | 27.2 (5.3) | 26.9 (4.2) | 26. 5 (3.9) | 26.9 (4.79) | 26.6 (4.3) | U = 588.50 |
| p = 0.891 | |||||||
| r = −0.016 | |||||||
| Weight loss (kg) | 5.3 (6.8) | 0.0 (0.0) | 5.6 (7.3) | 1.6 (2.4) | 5.5 (7.04) | 0.0 (0.0) | U = 591.50 |
| p = 0.914 | |||||||
| r = −0.013 | |||||||
| Interleukin 6 (ng/L) | 4.4 (4.2) | 2.3 (0.4) | 5.6 (6.3) | 2.8 (1.2) | 5.0 (5.4) | 2.6 (0.9) | U = 359.00 |
| p = 0.582 | |||||||
| r = −0.073 | |||||||
| Cramer’s φ effect size p-value | |||||||
| Male gender % | 56.7% | 50.0% | 52.9% | Phi = 0.0661 | |||
| p = 0.7558 | |||||||
| Malnutrition % | 33.3% | 22.5% | 27.1% | Phi = 0.1206 | |||
| p = 0.4167 | |||||||
| Diagnosis PDAC % | 56.7% | 55.0% | 55.7% | Phi = 0.0166 | |||
| p = 1.000 | |||||||
| Clavien–Dindo Classification | Group | Total | ||||
|---|---|---|---|---|---|---|
| Immunonutrition | Control | |||||
| Grade | Count | % | Count | % | Count | % of Total |
| 0 | 6 | 20.0% | 7 | 17.5% | 13 | 18.6% |
| 1 | 10 | 33.3% | 15 | 37.5% | 25 | 35.7% |
| 2 | 10 | 33.3% | 9 | 22.5% | 19 | 27.1% |
| 3a | 2 | 6.7% | 1 | 2.5% | 3 | 4.3% |
| 3b | 1 | 3.3% | 7 | 17.5% | 8 | 11.4% |
| 4a | 0 | 0.0% | 1 | 2.5% | 1 | 1.4% |
| 5 | 1 | 3.3% | 0 | 0.0% | 1 | 1.4% |
| Total | 30 | 100.0% | 40 | 100.0% | 70 | 100.0% |
| Publication | Number of Patients | Patient Population | Study Design | Outcome Measures | Study Results |
|---|---|---|---|---|---|
| Miyauchi Y, 2019 [12] | 60 | Pancreato-duoden-ectomy | Prospective, randomised. Perioperative or preoperative immunonutrition. | Immune functions, rate of postoperative complications. | No significant differences between the groups. RR 0.76 [0.46–1.28] |
| Silvestri S, 2016 [13] | 54 | Pancreato-duoden-ectomy; patients without malnutrition | Case-control. Immunonutrition preoperatively. | Mortality, overall complication rate, rates of individual complications, length of hospitalisation. | Lower rate of infectious complications and shorter duration of hospitalisation in the immunonutrition group. RR 0.87 [0.56–1.36] |
| Suzuki D, 2010 [7] | 30 | Pancreato-duoden-ectomy | Randomised, three branches: perioperative immunonutrition, postoperative immunonutrition, control. | Immune functions; rate of infectious complications. | Statistically significant differences of immune functions and rates of infectious complications, RR 0.29 [0.08–1.05] in comparisons of perioperative immunonutrition vs. other groups. |
| Gade J, 2016 [14] | 35 | Pancreatic cancer | Randomised case-control. | Rate of postoperative complications, length of hospitalisation, changes of body weight and general clinical status. | No significant differences between the groups. RR 0.70 [0.51–0.95] |
| Martin RC, 2017 [15] | 71 | Pancreatic cancer | Randomised case-control. Preoperative immunonutrition. | Overall complication rate and rate of infectious complications, length of hospitalisation, risk of malnutrition postoperatively, serum albumin. | Lower rate of postoperative complications, RR 0.50 [0.24–1.05], shorter duration of hospitalisation, lower risk of malnutrition and less of a decrease of serum albumin in the immunonutrition group. |
| Hamza N, 2015 [8] | 37 | Periampular tumours | Randomised case-control. Perioperative immunonutrition. | Immune functions. | Statistically significant differences of immune functions in the immunonutrition group. RR 0.83 [0.32–2.15] |
| Guan H *, 2019 [11] | 299 | Pancreato-duoden-ectomy | Meta-analysis; four randomised clinical trials included. | Immunonutrition decreases rate of infectious complications, RR 0.58 [0.37–0.92] and length of hospitalisation; no effect on the overall complication rate, RR 0.81 [0.62–1.05], rate of non-infectious complications, RR 0.94 [0.69, 1.28] and postoperative mortality. | |
| Hübner M, 2012 [9] | 152 | Gastro-intestinal surgery | Randomised case-control, preoperative immunonutrition, patients with malnutrition. | Rate of postoperative complications, infectious complications, length of hospitalisation. | No significant differences between the groups. RR 0.95 [0.76–1.19] |
| Burden S *, 2012 [22] | 1585 | Gastro-intestinal surgery | Meta-analysis; thirteen clinical trials included. | Immunonutrition decreases the overall complication rate, RR 0.67 [0.53–0.84], and rate of infectious complications. | |
| Hegazi RA *, 2014 [23] | 1456 | Gastro-intestinal surgery | Meta-analysis and systematic review; immunonutrition vs. standard nutritional management and immunonutrition vs. control (no nutritional management). 17 clinical trials included. | Immunonutrition and standard nutritional management decreases rate of infectious complications, OR 0.49 [0.29–0.83] and length of hospitalisation. No significant differences between immunonutrition and standard nutritional management. | |
| Reis AM *, 2016 [24] | Gastro-intestinal surgery | Systematic review; cost-effectiveness of immunonutrition. Six randomised clinical trials included. | Immunonutrition may reduce costs of treatment due to decreased rate of complications. | ||
| Klek S (a), 2014 [25] | 776 | Gastro-intestinal surgery | Randomised clinical trial; enteral and parenteral immunonutrition. Patients with or without malnutrition. | Rate of postoperative complications, length of hospitalisation. | No significant differences in patients without malnutrition. Statistically significant differences in patients with malnutrition when enteral immunonutrition is given, but no differences with parenteral immunonutrition. |
| Wong CS *, 2016 [26] | 2016 | Gastro-intestinal surgery | Systematic review; 19 randomised clinical trials included. | Immunonutrition decreases rate of infectious complications and length of hospitalisation; no effect on the overall complication rate and postoperative mortality. | |
| Marimuthu K *, 2012 [27] | 2496 | Gastro-intestinal surgery | Meta-analysis; 26 randomised clinical trials included. | Immunonutrition decreases rate of infectious complications, RR 0.64 [0.55–0.74] and length of hospitalisation; no effect on the overall non-infectious complication rate, RR 0.82 [0.71–0.95] and postoperative mortality. | |
| Mazaki T *, 2015 [28] | 7572 | Gastro-intestinal surgery | Meta-analysis. Comparison of enteral and parenteral immunonutrition, enteral and parenteral standard nutritional management. 74 clinical trials included. | Enteral immunonutrition is the most effective in decreasing overall complication rate, OR 0.75 [0.58–0.95], postoperative mortality, rates of wound infections, intraabdominal abscess and sepsis. Parenteral immunonutrition is the most effective in decreasing rates of pneumonia and urinary tract infections. The worst outcomes are obtained with standard parenteral nutritional management. | |
| Yan X *, 2016 [29] | 3854 | Gastro-intestinal cancers | Meta-analysis; 30 randomised clinical trials included. | Enteral immunonutrition decreases rates of infectious, RR 0.69 [0.48–0.98] and non-infectious complications, RR 0.72 [0.61–0.84], length of hospitalisation. | |
| Song GM *, 2015 [30] | Gastro-intestinal cancers | Meta-analysis, systematic review; 27 randomised clinical trials included. | Immunonutrition pre-, peri- or postoperatively decreases rate of infectious complications, RR 0.58 [0.43–0.78]. Besides, perioperative immunonutrition decreases rate of non-infectious complications, perioperative or postoperative immunonutrition decreases length of hospitalisation. | ||
| Adiamah A *, 2019 [16] | 1387 | Gastro-intestinal cancers | Meta-analysis, systematic review; 16 randomised clinical trials included. | Immunonutrition decreases rate of infectious complications, OR 0.52 [0.38, 0.71] and length of hospitalisation, no effect on the rate of non-infectious complications, OR 0.98 [0.73, 1.33] and postoperative mortality. | |
| Klek S (b), 2010 [31] | 305 | Gastro-intestinal cancers | Randomised clinical trial. Postoperative immunonutrition, patients with malnutrition. | Rate of postoperative complications, length of hospitalisation, postoperative mortality. | Immunonutrition decreases rate of infectious complications, OR 0.84 [0.42–1.69] and overall complication rate, OR 0.67 [0.35–1.27], length of hospitalisation and postoperative mortality. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tumas, J.; Jasiūnas, E.; Strupas, K.; Šileikis, A. Effects of Immunonutrition on Comprehensive Complication Index in Patients Undergoing Pancreatoduodenectomy. Medicina 2020, 56, 52. https://doi.org/10.3390/medicina56020052
Tumas J, Jasiūnas E, Strupas K, Šileikis A. Effects of Immunonutrition on Comprehensive Complication Index in Patients Undergoing Pancreatoduodenectomy. Medicina. 2020; 56(2):52. https://doi.org/10.3390/medicina56020052
Chicago/Turabian StyleTumas, Jaroslav, Eugenijus Jasiūnas, Kęstutis Strupas, and Audrius Šileikis. 2020. "Effects of Immunonutrition on Comprehensive Complication Index in Patients Undergoing Pancreatoduodenectomy" Medicina 56, no. 2: 52. https://doi.org/10.3390/medicina56020052
APA StyleTumas, J., Jasiūnas, E., Strupas, K., & Šileikis, A. (2020). Effects of Immunonutrition on Comprehensive Complication Index in Patients Undergoing Pancreatoduodenectomy. Medicina, 56(2), 52. https://doi.org/10.3390/medicina56020052





