Less Invasive Fixation of Acute Avulsions of the Achilles Tendon: A Technical Note
Abstract
:1. Introduction
2. Materials and Methods
2.1. Clinical Evaluation
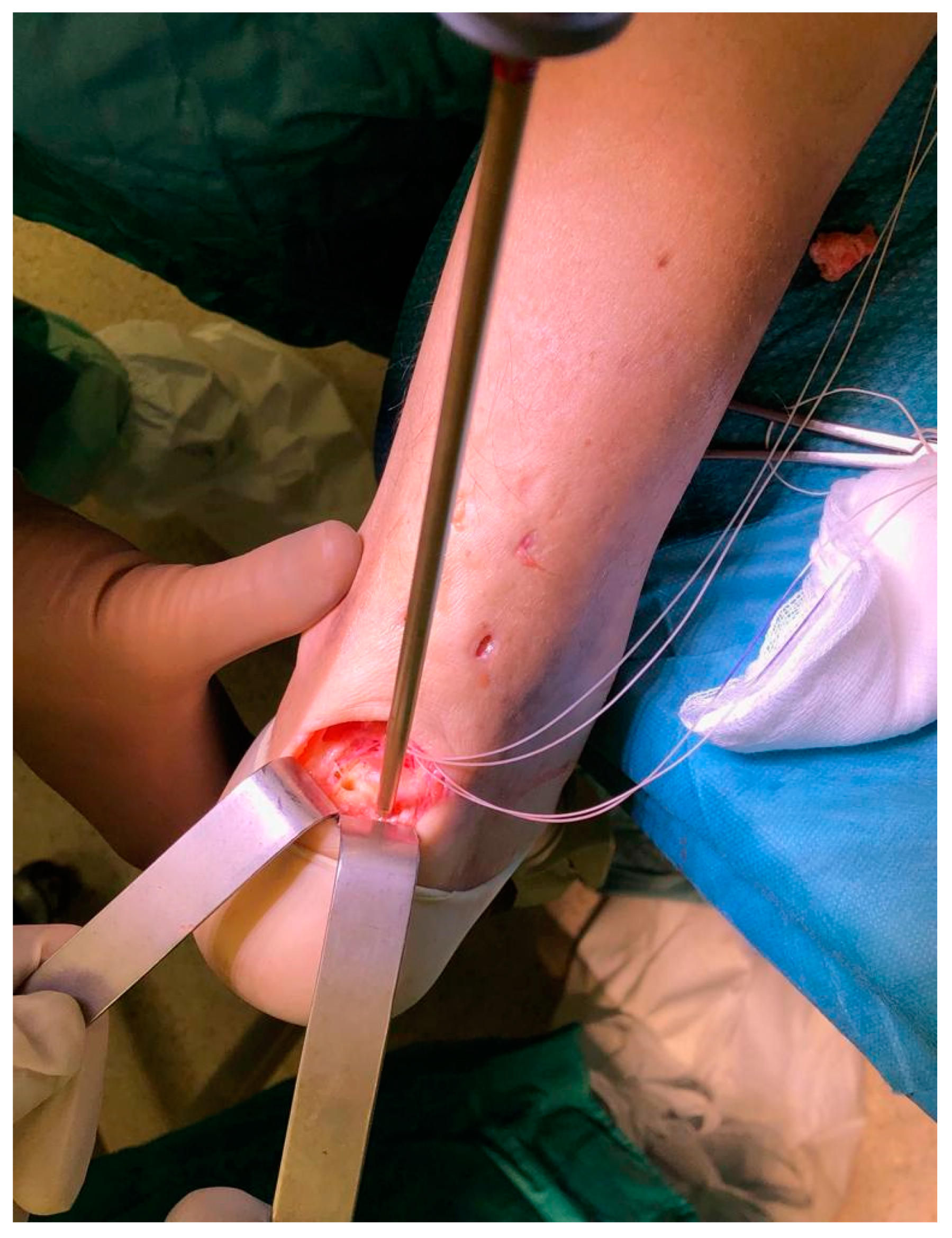
2.2. Technical Description
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Amlang, M.H.; Maffuli, N.; Longo, U.G.; Stübig, T.; Imrecke, J.; Hüfner, T. Surgical treatment of Achilles tendon rupture. Unfallchirurg 2010, 113, 712–720. [Google Scholar] [CrossRef] [PubMed]
- Longo, U.G.; Ronga, M.; Maffulli, N. Acute ruptures of the achilles tendon. Sports Med. Arthrosc. 2009, 17, 127–138. [Google Scholar] [CrossRef] [PubMed]
- Maffulli, N.; Longo, U.G.; Kadakia, A.; Spiezia, F. Achilles tendinopathy. Foot Ankle Surg. Off. J. Eur. Soc. Foot Ankle Surg. 2019, 26, 240–249. [Google Scholar] [CrossRef] [PubMed]
- Maffulli, N.; Margiotti, K.; Longo, U.G.; Loppini, M.; Fazio, V.M.; Denaro, V. The genetics of sports injuries and athletic performance. Muscles Ligaments Tendons J. 2013, 3, 173–189. [Google Scholar] [CrossRef] [Green Version]
- Işık, Ç.; Tahta, M. Primary repair of Achilles tendon avulsions: Presentation of a novel technique and its comparison with suture anchor repair. J. Orthop. Surg. 2017, 25. [Google Scholar] [CrossRef]
- Bibbo, C.A.R.; Davis, W.H.; Agnone, M. Repair of the Achilles tendon sleeve avulsion: Quantitative and functional evaluation of a transcalcaneal suture technique. Foot Ankle Int. 2003, 24, 539–544. [Google Scholar]
- Schipper, O.N.; Anderson, R.B.; Cohen, B.E. Outcomes After Primary Repair of Insertional Ruptures of the Achilles Tendon. Foot Ankle Int. 2018, 39, 664–668. [Google Scholar] [CrossRef]
- Stavenuiter, X.J.R.; Lubberts, B.; Prince, R.M.; Johnson, A.H.; DiGiovanni, C.W.; Guss, D. Postoperative Complications Following Repair of Acute Achilles Tendon Rupture. Foot Ankle Int. 2019, 40, 679–686. [Google Scholar] [CrossRef]
- Maffulli, N.; Longo, U.G.; Spiezia, F.; Denaro, V. Minimally invasive surgery for Achilles tendon pathologies. Open Access J. Sports Med. 2010, 1, 95–103. [Google Scholar] [CrossRef] [Green Version]
- Maffulli, N.; Longo, U.G.; Oliva, F.; Ronga, M.; Denaro, V. Minimally invasive surgery of the achilles tendon. Orthop. Clin. N. Am. 2009, 40, 491–498. [Google Scholar] [CrossRef]
- Longo, U.G.; Ramamurthy, C.; Denaro, V.; Maffulli, N. Minimally invasive stripping for chronic Achilles tendinopathy. Disabil. Rehabil. 2008, 30, 1709–1713. [Google Scholar] [CrossRef] [PubMed]
- Longo, U.G.; Forriol, F.; Campi, S.; Maffulli, N.; Denaro, V. A biomechanical comparison of the primary stability of two minimally invasive techniques for repair of ruptured Achilles tendon. Knee Surg. Sports Traumatol. Arthrosc. 2012, 20, 1392–1397. [Google Scholar] [CrossRef] [PubMed]
- Maffulli, N.; Ajis, A.; Longo, U.G.; Denaro, V. Chronic rupture of tendo Achillis. Foot Ankle Clin. 2007, 12, 583–596. [Google Scholar] [CrossRef] [PubMed]
- Maffulli, N.; Longo, U.G.; Gougoulias, N.; Denaro, V. Ipsilateral free semitendinosus tendon graft transfer for reconstruction of chronic tears of the Achilles tendon. BMC Musculoskelet Disord. 2008, 9, 100. [Google Scholar] [CrossRef] [Green Version]
- Maffulli, N.; Spiezia, F.; Longo, U.G.; Denaro, V. Less-invasive reconstruction of chronic achilles tendon ruptures using a peroneus brevis tendon transfer. Am. J. Sports Med. 2010, 38, 2304–2312. [Google Scholar] [CrossRef]
- Maffulli, N.; Spiezia, F.; Testa, V.; Capasso, G.; Longo, U.G.; Denaro, V. Free gracilis tendon graft for reconstruction of chronic tears of the Achilles tendon. J. Bone Jt. Surg. Am. 2012, 94, 906–910. [Google Scholar] [CrossRef]
- Maffulli, N.; Del Buono, A.; Spiezia, F.; Maffulli, G.D.; Longo, U.G.; Denaro, V. Less-invasive semitendinosus tendon graft augmentation for the reconstruction of chronic tears of the Achilles tendon. Am. J. Sports Med. 2013, 41, 865–871. [Google Scholar] [CrossRef]
- Maffulli, N.; Loppini, M.; Longo, U.G.; Maffulli, G.D.; Denaro, V. Minimally invasive reconstruction of chronic achilles tendon ruptures using the ipsilateral free semitendinosus tendon graft and interference screw fixation. Am. J. Sports Med. 2013, 41, 1100–1107. [Google Scholar] [CrossRef]
- Carmont, M.R.; Maffulli, N. Modified percutaneous repair of ruptured Achilles tendon. Knee Surg. Sports Traumatol. Arthrosc. 2008, 16, 199–203. [Google Scholar] [CrossRef]
- Maffulli, N.; Longo, U.G.; Testa, V.; Oliva, F.; Capasso, G.; Denaro, V. Italian translation of the VISA-A score for tendinopathy of the main body of the Achilles tendon. Disabil. Rehabil. 2008, 30, 1635–1639. [Google Scholar] [CrossRef]
- Carmont, M.R.; Silbernagel, K.G.; Nilsson-Helander, K.; Mei-Dan, O.; Karlsson, J.; Maffulli, N. Cross cultural adaptation of the Achilles tendon Total Rupture Score with reliability, validity and responsiveness evaluation. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 1356–1360. [Google Scholar] [CrossRef] [PubMed]
- Maffulli, N.; Longo, U.G.; Spiezia, F.; Denaro, V. Free hamstrings tendon transfer and interference screw fixation for less invasive reconstruction of chronic avulsions of the Achilles tendon. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 269–273. [Google Scholar] [CrossRef] [PubMed]
- Longo, U.G.; Petrillo, S.; Maffulli, N.; Denaro, V. Acute achilles tendon rupture in athletes. Foot Ankle Clin. 2013, 18, 319–338. [Google Scholar] [CrossRef] [PubMed]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Longo, U.G.; Candela, V.; Berton, A.; Di Naro, C.; Stelitano, G.; Maffulli, N.; Denaro, V. Less Invasive Fixation of Acute Avulsions of the Achilles Tendon: A Technical Note. Medicina 2020, 56, 715. https://doi.org/10.3390/medicina56120715
Longo UG, Candela V, Berton A, Di Naro C, Stelitano G, Maffulli N, Denaro V. Less Invasive Fixation of Acute Avulsions of the Achilles Tendon: A Technical Note. Medicina. 2020; 56(12):715. https://doi.org/10.3390/medicina56120715
Chicago/Turabian StyleLongo, Umile Giuseppe, Vincenzo Candela, Alessandra Berton, Calogero Di Naro, Giovanna Stelitano, Nicola Maffulli, and Vincenzo Denaro. 2020. "Less Invasive Fixation of Acute Avulsions of the Achilles Tendon: A Technical Note" Medicina 56, no. 12: 715. https://doi.org/10.3390/medicina56120715




