Comparative Study between Full-Endoscopic Discectomy and Microendoscopic Discectomy for the Treatment of Lumbar Disc Herniation
Abstract
1. Introduction
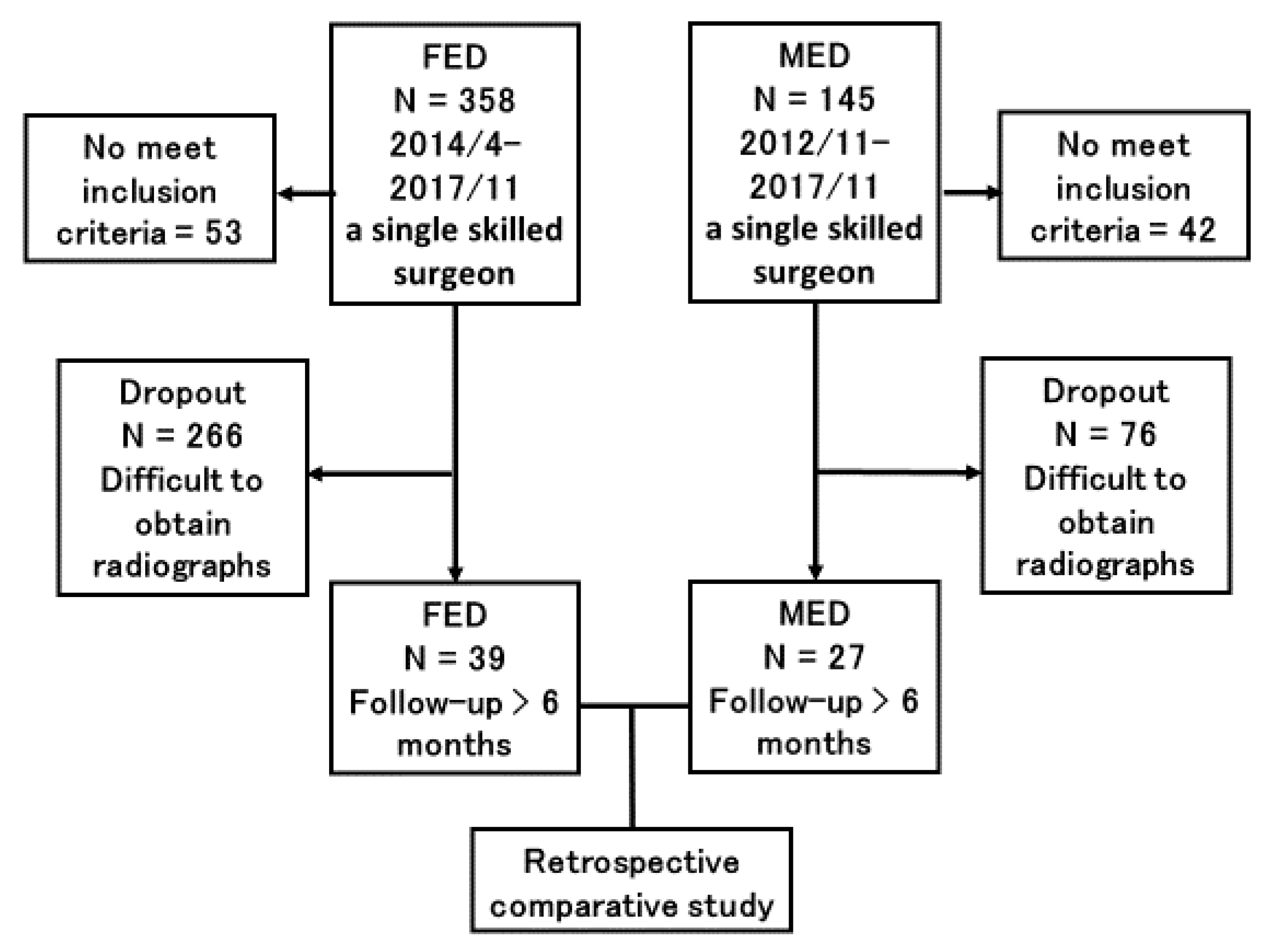
2. Materials and Methods
2.1. Patient Selection
2.2. Surgical Procedures
2.3. Evaluation of Pain
2.4. Evaluation of LDH Size Removed Disc Weight
2.5. Statistical Analysis
2.6. Evaluation of Disc Height
3. Results
4. Discussion
Limitation of This Study
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Ethical Standards
References
- Foley, K.T.; Smith, M.M.; Rampersaud, Y.R. Microendoscopic approach to far-lateral lumbar disc herniation. Neurosurg. Focus 1999, 7, e5. [Google Scholar] [CrossRef]
- Perez-Cruet, M.J.; Foley, K.T.; Isaacs, R.E.; Rice-Wyllie, L.; Wellington, R.; Smith, M.M.; Fessler, R.G. Microendoscopic Lumbar Discectomy: Technical Note. Neurosurgery 2002, 51 (Suppl. 5), S129–S136. [Google Scholar] [CrossRef] [PubMed]
- Oshima, Y.; Inanami, H.; Iwai, H.; Koga, H.; Takano, Y.; Oshina, M.; Oka, H.; Tanaka, S. Is Microendoscopic Discectomy Effective for Patients with Concomitant Lumbar Disc Herniation and Spondylolysis? Glob. Spine J. 2020, 10, 700–705. [Google Scholar] [CrossRef]
- Pang, J.-Y.; Tan, F.; Chen, W.-W.; Li, C.-H.; Dou, S.-P.; Guo, J.-R.; Zhao, L.-Y. Comparison of microendoscopic discectomy and open discectomy for single-segment lumbar disc herniation. World J. Clin. Cases 2020, 8, 2942–2949. [Google Scholar] [CrossRef] [PubMed]
- Yadav, R.I.; Long, L.; Yanming, C. Comparison of the effectiveness and outcome of microendoscopic and open discectomy in patients suffering from lumbar disc herniation. Medicine (Baltimore) 2019, 98, e16627. [Google Scholar] [CrossRef] [PubMed]
- Phan, K.; Xu, J.; Schultz, K.; Alvi, M.A.; Lu, V.M.; Kerezoudis, P.; Maloney, P.R.; Murphy, M.E.; Mobbs, R.J.; Bydon, M. Full-endoscopic versus micro-endoscopic and open discectomy: A systematic review and meta-analysis of outcomes and complications. Clin. Neurol. Neurosurg. 2017, 154, 1–12. [Google Scholar] [CrossRef]
- Chen, Z.; Zhang, L.; Dong, J.; Xie, P.; Liu, B.; Wang, Q.; Chen, R.; Feng, F.; Yang, B.; Shu, T.; et al. Percutaneous transforaminal endoscopic discectomy compared with microendoscopic discectomy for lumbar disc herniation: 1-year results of an ongoing randomized controlled trial. J. Neurosurg. Spine 2018, 28, 300–310. [Google Scholar] [CrossRef]
- Chen, Z.; Zhang, L.; Dong, J.; Xie, P.; Liu, B.; Wang, Q.; Chen, R.; Shu, T.; Li, S.; Feng, F.; et al. Percutaneous Transforaminal Endoscopic Discectomy Versus Microendoscopic Discectomy for Lumbar Disc Herniation: Two-Year Results of a Randomized Controlled Trial. Spine (Phila Pa 1976) 2020, 45, 493–503. [Google Scholar] [CrossRef]
- Lee, D.Y.; Lee, S.-H. Learning Curve for Percutaneous Endoscopic Lumbar Discectomy. Neurol. Med. Chir. 2008, 48, 383–389. [Google Scholar] [CrossRef]
- Baba, S.; Oshima, Y.; Iwahori, T.; Takano, Y.; Inanami, H.; Koga, H. Microendoscopic posterior decompression for the treatment of thoracic myelopathy caused by ossification of the ligamentum flavum: A technical report. Eur. Spine J. 2016, 25, 1912–1919. [Google Scholar] [CrossRef]
- Schubert, M.; Hoogland, T. Endoscopic transforaminal nucleotomy with foraminoplasty for lumbar disk herniation. Oper. Orthop. Traumatol. 2005, 17, 641–661. [Google Scholar] [CrossRef] [PubMed]
- Choi, G.; Lee, S.H.; Deshpande, K.; Choi, H. Working channel endoscope in lumbar spine surgery. J. Neurosurg. Sci. 2014, 58, 77–85. [Google Scholar] [PubMed]
- Inomata, Y.; Oshima, Y.; Inoue, H.; Takano, Y.; Inanami, H.; Koga, H. Percutaneous endoscopic lumbar discectomy via adjacent interlaminar space for highly down-migrated lumbar disc herniation: A technical report. J. Spine Surg. 2018, 4, 483–489. [Google Scholar] [CrossRef] [PubMed]
- Koga, H.; Inanami, H. Minimal laminectomy using the interlaminar approach for percutaneous endoscopic lumbar discectomy. Mini-Invasive Surg. 2017, 1, 56–62. [Google Scholar] [CrossRef]
- Kondo, M.; Oshima, Y.; Inoue, H.; Takano, Y.; Inanami, H.; Koga, H. Significance and pitfalls of percutaneous endoscopic lumbar discectomy for large central lumbar disc herniation. J. Spine Surg. 2018, 4, 79–85. [Google Scholar] [CrossRef]
- Ishibashi, K.; Fujita, M.; Takano, Y.; Iwai, H.; Inanami, H.; Koga, H. Chemonucleolysis with Chondroitin Sulfate ABC Endolyase for Treating Lumbar Disc Herniation: Exploration of Prognostic Factors for Good or Poor Clinical Outcomes. Medicina 2020, 56, 627. [Google Scholar] [CrossRef]
- Inoue, H.; Ohmori, K.; Miyasaka, K.; Hosoe, H. Radiographic evaluation of the lumbosacral disc height. Skelet. Radiol. 1999, 28, 638–643. [Google Scholar] [CrossRef]
- Lee, S.-H.; Bae, J.S. Comparison of clinical and radiological outcomes after automated open lumbar discectomy and conventional microdiscectomy: A prospective randomized trial. Int. J. Clin. Exp. Med. 2015, 8, 12135–12148. [Google Scholar]
- Zhao, X.-M.; Yuan, Q.; Liu, L.; Shi, Y.-M.; Zhang, Y.-G. Is It Possible to Replace Microendoscopic Discectomy with Percutaneous Transforaminal Discectomy for Treatment of Lumbar Disc Herniation? A Meta-Analysis Based on Recurrence and Revision Rate. J. Korean Neurosurg. Soc. 2020, 63, 477–486. [Google Scholar] [CrossRef]
- Xu, J.; Li, Y.; Xu, J.; Lv, G.; Li, L.; Dai, Y.; Jiang, B.; Zheng, Z. Minimum 2-Year Efficacy of Percutaneous Endoscopic Lumbar Discectomy versus Microendoscopic Discectomy: A Meta-Analysis. World Neurosurg. 2020, 138, 19–26. [Google Scholar] [CrossRef]
- Yu, P.; Qiang, H.; Zhou, J.; Huang, P. Percutaneous Transforaminal Endoscopic Discectomy versus Micro-Endoscopic Discectomy for Lumbar Disc Herniation. Med Sci. Monit. 2019, 25, 2320–2328. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Chamoli, U.; Lapkin, S.; Castillo, J.V.; Diwan, A.D. Complication rates of different discectomy techniques for the treatment of lumbar disc herniation: A network meta-analysis. Eur. Spine J. 2019, 28, 2588–2601. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Chamoli, U.; Castillo, J.V.; Ramakrishna, V.A.S.; Diwan, A.D. Complication rates of different discectomy techniques for symptomatic lumbar disc herniation: A systematic review and meta-analysis. Eur. Spine J. 2020, 29, 1752–1770. [Google Scholar] [CrossRef] [PubMed]
- Feng, F.; Xu, Q.; Yan, F.; Xie, Y.; Deng, Z.; Hu, C.; Zhu, X.; Cai, L. Comparison of 7 Surgical Interventions for Lumbar Disc Herniation: A Network Meta-analysis. Pain Physician 2017, 20, E863–E871. [Google Scholar] [PubMed]
- Shi, R.; Wang, F.; Hong, X.; Wang, Y.-T.; Bao, J.-P.; Liu, L.; Wang, X.-H.; Xie, Z.-Y.; Wu, X.-T. Comparison of percutaneous endoscopic lumbar discectomy versus microendoscopic discectomy for the treatment of lumbar disc herniation: A meta-analysis. Int. Orthop. 2019, 43, 923–937. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Yuan, S.; Tian, Y.; Wang, L.; Gong, L.; Zheng, Y.; Li, J. Comparison of percutaneous endoscopic transforaminal discectomy, microendoscopic discectomy, and microdiscectomy for symptomatic lumbar disc herniation: Minimum 2-year follow-up results. J. Neurosurg. Spine 2018, 28, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Song, H.-P.; Sheng, H.-F.; Xu, W.-X. A case-control study on the treatment of protrusion of lumbar intervertebral disc through PELD and MED. Exp. Ther. Med. 2017, 14, 3708–3712. [Google Scholar] [CrossRef]
- Kettler, A.; Wilke, H.J. Review of existing grading systems for cervical or lumbar disc and facet joint degeneration. Eur. Spine J. 2006, 15, 705–718. [Google Scholar] [CrossRef]

| Characteristic | FED (N = 39) | MED (N = 27) | p Value |
|---|---|---|---|
| Age (years), median (IQR Q25–75) | 46 (39–53) | 44 (28–55) | 0.25 |
| Sex male, n (%) | 25 (64.1%) | 17 (63.0%) | 0.92 |
| Height (cm), median (IQR Q25–75) | 168 (160–177) | 164 (161–170) | 0.44 |
| BMI (kg/m2), median (IQR Q25–75) | 24.56 (21.48–26.23) | 23.80 (20.08–26.77) | 0.62 |
| Smoking history, n (%) | 9 (23.1%) | 8 (29.6%) | 0.55 |
| Surgical level, number, n (%) | <0.05 | ||
| L1/2 | 2 (5.1%) | 0 | |
| L2/3 | 3 (7.7%) | 0 | |
| L3/4 | 5 (12.8%) | 0 | |
| L4/5 | 7 (17.9%) | 17 (63.0%) | |
| L5/S1 | 22 (56.4%) | 10 (37.0%) | |
| Follow-up Period (months), median (IQR Q25–75) | 20 (12–31) | 17 (12–36) | 0.98 |
| Parameter | FED (N = 39) | MED (N = 27) | p Value |
|---|---|---|---|
| NRS scores for Low Back, median (IQR Q25–75) | |||
| Preoperative | 5 (2–7) | 6 (3–8) | 0.6 |
| At Discharge | 1 (0–4) | 1 (0–2) | 0.47 |
| NRS scores for Leg, median (IQR Q25–75) | |||
| Preoperative | 7 (5–8) | 6 (5–8) | 0.91 |
| At Discharge | 0 (0–2) | 0 (0–2) | 0.46 |
| Preoperative DHI, median (IQR Q25–75) | 0.23 (0.19–0.29) | 0.24 (0.22–0.27) | 0.43 |
| Postoperative DHI, median (IQR Q25–75) | 0.22 (0.18–0.27) | 0.22 (0.20–0.24) | 0.69 |
| DHI ratio, median (IQR Q25–75) | 0.94 (0.89–1.03) | 0.90 (0.79–0.95) | <0.05 |
| Operation Time (minutes), median (IQR Q25–75) | 42.0 (33.0–61.0) | 43.0 (33.0–50.0) | 0.79 |
| Blood Loss (ml), median (IQR Q25–75) | <50 | 60 (50–90) | <0.05 |
| Postoperative Hospital Stay (days), median (IQR Q25–75) | 2 (1–3) | 5 (4–5) | <0.05 |
| Weight of LDH (g), median (IQR Q25–75) | 0.60 (0.50–1.10) | 0.80 (0.40–1.90) | 0.17 |
| maximum occupancy ratio of LDH on axial MRI (%), median (IQR Q25–75) | 26.0 (17.3–36.7) | 29.1 (18.6–37.0) | 0.75 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fujita, M.; Kitagawa, T.; Hirahata, M.; Inui, T.; Kawano, H.; Iwai, H.; Inanami, H.; Koga, H. Comparative Study between Full-Endoscopic Discectomy and Microendoscopic Discectomy for the Treatment of Lumbar Disc Herniation. Medicina 2020, 56, 710. https://doi.org/10.3390/medicina56120710
Fujita M, Kitagawa T, Hirahata M, Inui T, Kawano H, Iwai H, Inanami H, Koga H. Comparative Study between Full-Endoscopic Discectomy and Microendoscopic Discectomy for the Treatment of Lumbar Disc Herniation. Medicina. 2020; 56(12):710. https://doi.org/10.3390/medicina56120710
Chicago/Turabian StyleFujita, Muneyoshi, Tomoaki Kitagawa, Masahiro Hirahata, Takahiro Inui, Hirotaka Kawano, Hiroki Iwai, Hirohiko Inanami, and Hisashi Koga. 2020. "Comparative Study between Full-Endoscopic Discectomy and Microendoscopic Discectomy for the Treatment of Lumbar Disc Herniation" Medicina 56, no. 12: 710. https://doi.org/10.3390/medicina56120710
APA StyleFujita, M., Kitagawa, T., Hirahata, M., Inui, T., Kawano, H., Iwai, H., Inanami, H., & Koga, H. (2020). Comparative Study between Full-Endoscopic Discectomy and Microendoscopic Discectomy for the Treatment of Lumbar Disc Herniation. Medicina, 56(12), 710. https://doi.org/10.3390/medicina56120710





