Neurodevelopmental Outcome in Extremely Low Birth Weight Infants at 2–3 Years of Age
Abstract
1. Introduction
2. Materials and Methods
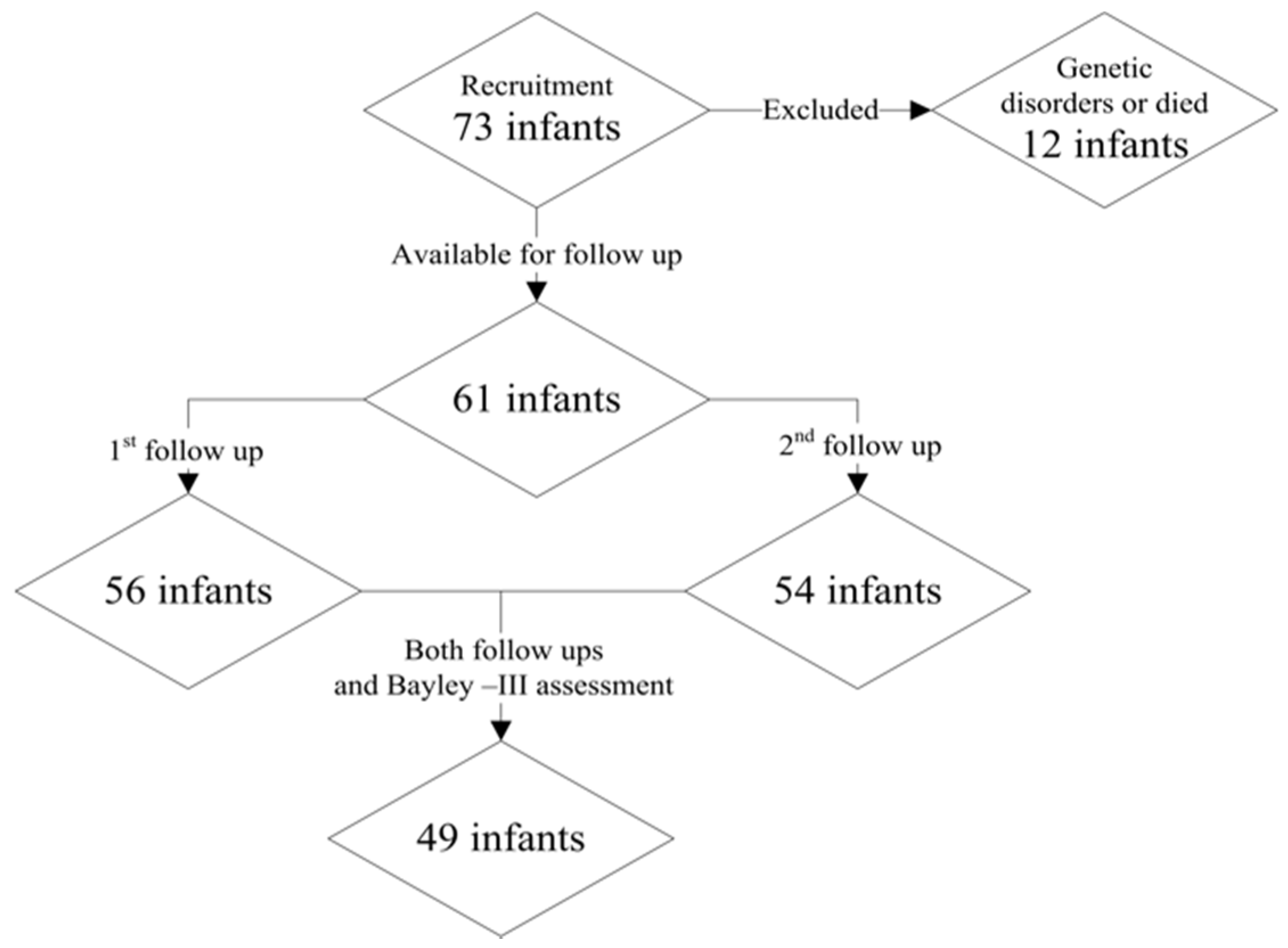
2.1. Participants
2.2. Statistical Analysis
3. Results
3.1. Characteristics of Study Participants
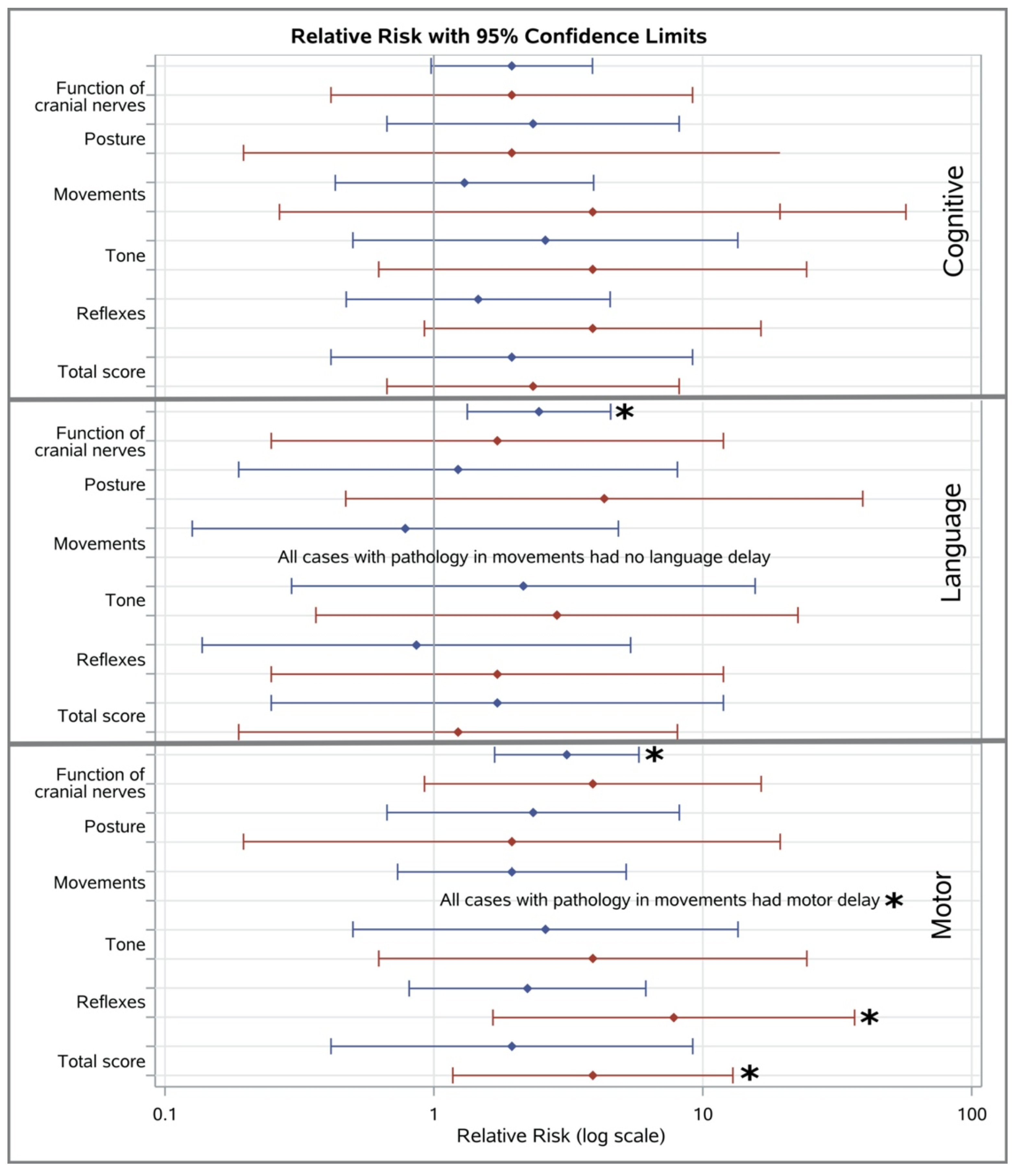
3.2. Association between Hammersmith Infant Neurological Examination Testing and Bayley-III Scales Scores
3.2.1. Cognitive Performance
3.2.2. Language Performance
3.2.3. Motor Performance
3.3. Factors Associated with Bayley-III Scales
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Jefferies, A.L.; Kirpalani, H.M.; Canadian Paediatric Society Fetus; Newborn Committee. Counselling and management for anticipated extremely preterm birth. Paediatr. Child Health 2012, 17, 443–446. [Google Scholar] [CrossRef]
- Hack, M.; Wright, L.L.; Shankaran, S.; Tyson, J.E.; Horbar, J.D.; Bauer, C.R.; Younes, N.; National Institute of Child Health and Human Development Neonatal Research Network. Very-low-birth-weight outcomes of the National Institute of Child Health and Human Development Neonatal Network, November 1989 to October 1990. Am. J. Obstet. Gynecol. 1995, 172 Pt 1, 457–464. [Google Scholar] [CrossRef]
- La Pine, T.R.; Jackson, J.C.; Bennett, F.C. Outcome of infants weighing less than 800 grams at birth: 15 years’ experience. Pediatrics 1995, 96 Pt 1, 479–483. [Google Scholar] [CrossRef]
- Vohr, B.R.; Wright, L.L.; Dusick, A.M.; Mele, L.; Verter, J.; Steichen, J.J.; Simon, N.P.; Wilson, D.C.; Broyles, S.; Bauer, C.R.; et al. Neurodevelopmental and Functional Outcomes of Extremely Low Birth Weight Infants in the National Institute of Child Health and Human Development Neonatal Research Network, 1993–1994. Pediatrics 2000, 105, 1216–1226. [Google Scholar] [CrossRef]
- Singh, L.; Das, S.; Bhat, V.B.; Plakkal, N. Early Neurodevelopmental Outcome of Very Low Birthweight Neonates with Culture-positive Blood Stream Infection: A Prospective Cohort Study. Cureus 2018, 10, e3492. [Google Scholar] [CrossRef] [PubMed]
- Stoll, B.J.; Hansen, N.I.; Adams-Chapman, I.; Fanaroff, A.A.; Hintz, S.R.; Vohr, B.R.; Higgins, R.D.; National Institute of Child Health and Human Development Neonatal Research Network. Neurodevelopmental and growth impairment among extremely low-birth-weight infants with neonatal infection. JAMA 2004, 292, 2357–2365. [Google Scholar] [CrossRef]
- Costeloe, K.L.; Hennessy, E.M.; Haider, S.; Stacey, F.; Marlow, N.; Draper, E.S. Short term outcomes after extreme preterm birth in England: Comparison of two birth cohorts in 1995 and 2006 (the EPICure studies). BMJ 2012, 345, e7976. [Google Scholar] [CrossRef] [PubMed]
- Johnson, S.; Marlow, N. Early and long-term outcome of infants born extremely preterm. Arch. Dis. Child. 2017, 102, 97–102. [Google Scholar] [CrossRef]
- Wusthoff, C.J. How to use: The neonatal neurological examination. Arch. Dis. Child. Educ. Pr. Ed. 2013, 98, 148–153. [Google Scholar] [CrossRef] [PubMed]
- Gardon, L.; Picciolini, O.; Squarza, C.; Frigerio, A.; Gianni, M.L.; Gangi, S.; Fumagalli, M.; Mosca, F. Neurodevelopmental outcome and adaptive behaviour in extremely low birth weight infants at 2 years of corrected age. Early Hum. Dev. 2019, 128, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Maitre, N.L.; Chorna, O.; Romeo, D.M.; Guzzetta, A. Implementation of the Hammersmith Infant Neurological Examination in a High-Risk Infant Follow-Up Program. Pediatr. Neurol. 2016, 65, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Bayley, N. Bayley Scales of Infant and Toddler Development, 3rd ed.; Harcourt Assessment: San Antonio, TX, USA, 2005. [Google Scholar]
- Moore, T.; Hennessy, E.M.; Myles, J.; Johnson, S.J.; Draper, E.S.; Costeloe, K.L.; Marlow, N. Neurological and developmental outcome in extremely preterm children born in England in 1995 and 2006: The EPICure studies. BMJ 2012, 345, e7961. [Google Scholar] [CrossRef] [PubMed]
- Vohr, B.R.; Stephens, B.E.; Higgins, R.D.; Bann, C.M.; Hintz, S.R.; Das, A.; Newman, J.E.; Peralta-Carcelen, M.; Yolton, K.; Dusick, A.M.; et al. Are Outcomes of Extremely Preterm Infants Improving? Impact of Bayley Assessment on Outcomes. J. Pediatr. 2012, 161, 222–228. [Google Scholar] [CrossRef] [PubMed]
- Milne, S.; McDonald, J.; Comino, E.J. The use of the bayley scales of infant and toddler development III with clinical populations: A preliminary exploration. Phys. Occup. Ther. Pediatr. 2012, 32, 24–33. Available online: http://www.ncbi.nlm.nih.gov/pubmed/21812743 (accessed on 28 June 2020). [CrossRef] [PubMed]
- Fenton, T.R.; Kim, J.H. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013, 13, 59. [Google Scholar] [CrossRef]
- Bell, M.J.; Ternberg, J.L.; Feigin, R.D.; Keating, J.P.; Marshall, R.; Barton, L.; Brotherton, T. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann. Surg. 1978, 187, 1–7. [Google Scholar] [CrossRef]
- Frisone, M.F.; Mercuri, E.; Laroche, S.; Foglia, C.; Maalouf, E.F.; Haataja, L.; Cowan, F.; Dubowitz, L. Prognostic value of the neurologic optimality score at 9 and 18 months in preterm infants born before 31 weeks’ gestation. J. Pediatr. 2002, 140, 57–60. [Google Scholar] [CrossRef]
- Romeo, D.M.M.; Cioni, M.; Scoto, M.; Pizzardi, A.; Romeo, M.G.; Guzzetta, A. Prognostic value of a scorable neurological examination from 3 to 12 months post-term age in very preterm infants: A longitudinal study. Early Hum. Dev. 2009, 85, 405–408. [Google Scholar] [CrossRef]
- Haataja, L.; Mercuri, E.; Regev, R.; Cowan, F.; Rutherford, M.; Dubowitz, V.; Dubowitz, L. Optimality score for the neurologic examination of the infant at 12 and 18 months of age. J. Pediatr. 1999, 135 Pt 1, 153–161. [Google Scholar] [CrossRef]
- Palisano, R.J.; Hanna, S.E.; Rosenbaum, P.L.; Russell, D.J.; Walter, S.D.; Wood, E.P.; Raina, P.S.; Galuppi, B.E. Validation of a model of gross motor function for children with cerebral palsy. Phys. Ther. 2000, 80, 974–985. [Google Scholar] [CrossRef]
- Hadders-Algra, M.; Tacke, U.; Pietz, J.; Rupp, A.; Philippi, H. Reliability and predictive validity of the Standardized Infant NeuroDevelopmental Assessment neurological scale. Dev. Med. Child Neurol. 2019, 61, 654–660. [Google Scholar] [CrossRef] [PubMed]
- Romeo, D.M.M.; Cioni, M.; Palermo, F.; Cilauro, S.; Romeo, M.G. Neurological assessment in infants discharged from a neonatal intensive care unit. Eur. J. Paediatr. Neurol. 2013, 17, 192–198. [Google Scholar] [CrossRef] [PubMed]
- Romeo, D.M.; Ricci, D.; Brogna, C.; Mercuri, E. Use of the Hammersmith Infant Neurological Examination in infants with cerebral palsy: A critical review of the literature. Dev. Med. Child Neurol. 2016, 58, 240–245. [Google Scholar] [CrossRef] [PubMed]
- Benasich, A.A.; Thomas, J.J.; Choudhury, N. The importance of rapid auditory processing abilities to early language development. Brain Behav. Immun. 2008, 22, 629. [Google Scholar]
- De Groot, L. Posture and motility in preterm infants. Dev. Med. Child Neurol. 2000, 42, 65–68. [Google Scholar] [CrossRef]
- Georgieff, M.K.; Bernbaum, J.C.; Hoffman-Williamson, M.; Daft, A. Abnormal truncal muscle tone as a useful early marker for developmental delay in low birth weight infants. Pediatrics 1986, 77, 659–663. [Google Scholar]
- Hadders-Algra, M. General movements in early infancy: What do they tell us about the nervous system? Early Hum. Dev. 1993, 34, 29–37. [Google Scholar] [CrossRef]
- Shore, R. Rethinking the Brain: New Insights into Early Development; Families and Work Institute: New York, NY, USA, 1997. [Google Scholar]
- Als, H.; McAnulty, G.B. The Newborn Individualized Developmental Care and Assessment Program (NIDCAP) with Kangaroo Mother Care (KMC): Comprehensive Care for Preterm Infants. Curr. Womens Health Rev. 2011, 7, 288–301. [Google Scholar] [CrossRef]
- NeuroDevelopmental Treatment Association. Available online: https://www.ndta.org (accessed on 21 July 2020).
- Spencer-Smith, M.M.; Spittle, A.J.; Lee, K.J.; Doyle, L.W.; Anderson, P.J. Bayley-III cognitive and language scales in preterm children. Pediatrics 2015, 135, e1258–e1265. [Google Scholar] [CrossRef]
- Spittle, A.J.; Spencer-Smith, M.M.; Eeles, A.L.; Lee, K.J.; Lorefice, L.E.; Anderson, P.J.; Doyle, L.W. Does the Bayley-III Motor Scale at 2 years predict motor outcome at 4 years in very preterm children? Dev. Med. Child Neurol. 2013, 55, 448–452. [Google Scholar] [CrossRef]
| Characteristics of Study Participants | Examined (n = 49) | Not-Examined (n = 12) | p-Value |
|---|---|---|---|
| Gestational age (weeks) a | 27.7 (1.85) | 27.9 (2.4) | ns |
| Birthweight (g) b | 870 (530–1000) | 870 (590–1000) | ns |
| Head Circumference (cm) b | 25 (21–28) | 25 (20–26.5) | ns |
| Gender (male), n(%) c | 26 (53.1) | 5 (41.7) | ns |
| Multiparity (n) c | 15 (30.6) | 1 (8.3) | ns |
| Multiple gestation, n (%) c | 19 (38.8) | 1 (8.3) | 0.083 |
| Mode of delivery (caesarean section), (n%) c | 45 (91.8) | 10 (83.3) | ns |
| Chorioamnionitis, n (%) c | 3 (6.1) | 1 (8.3) | ns |
| Preeclampsia/Eclampsia, n(%) c | 6 (12.2) | 1 (8.3) | ns |
| Gestational diabetes, n(%) c | 3 (6.1) | 1 (8.3) | ns |
| APGAR scores 5min b | 8 (1–9) | 8 (3–9) | ns |
| Prenatal corticosteroids, n(%) c | 40 (81.6) | 8 (66.7) | ns |
| Small for gestational age, n(%) c | 14 (28.6) | 5 (41.7) | ns |
| Intrauterine Growth Retardation, n (%) c | 13 (26.5) | 4 (33.3) | ns |
| Respiratory distress syndrome, n(%) c | 43 (87.8) | 8 (66.7) | 0.096 |
| Surfactant administration n(%) c | 35 (71.4) | 7 (58.3) | ns |
| Patent ductus arteriosus, n(%) c | 10 (20.4) | 4 (33.3) | ns |
| Nosocomial sepsis, n(%) c | 37 (75.5) | 8 (66.7) | ns |
| Ventilation days (n) b | 5 (0–44) | 9.5 (0–67) | ns |
| O2 days (n) a | 37.8 (26.6) | 33.9 (30.2) | ns |
| Bronchopulmonary Dysplasia | 28 (57.1) | 6 (50) | ns |
| Necrotizing Enterocolitis | 3 (6.1) | 2 (16.7) | ns |
| Intraventricular Hemorrhage ΙΙI-IV | 6 (12.5) | 1 (8.3) | ns |
| Periventricular Leucomalacia | 1 (2) | 0 | ns |
| Cerebral Palsy | 4 (8.2) | 0 | ns |
| Hospital stay (days) b | 67 (31–154) | 74.5 (43–120) | ns |
| Composite Scores | n | Mean | Range | SD |
|---|---|---|---|---|
| Cognitive | 49 | 96.3 | 75–115 | 9.8 |
| Language | 48 | 99.9 | 74–135 | 11.9 |
| Motor | 49 | 93.2 | 70–112 | 9.9 |
| Bayley III | Composite Scores | Cognitive Scores, n(%) | Language Scores, n(%) | Motor Scores, n(%) |
|---|---|---|---|---|
| Above average (+1SD) | >116 | 0 | 3 (6.3) | 0 |
| Average | 86–115 | 39 (79.6) | 40 (83.3) | 39 (79.6) |
| Low average (−1SD) | 71–85 | 10 (20.4) | 5 (10.4) | 8 (16.3) |
| Extremely low (−2SD) | 56–70 | 0 | 0 | 2 (4.1) |
| HINE Sections | Median 1 (Range) | SD | 10th Percentile | Median 2 (Range) | SD | 10th Percentile |
|---|---|---|---|---|---|---|
| Function of cranial nerves | 13 (8–15) | 1.66 | 11 | 15 (12–15) | 1.06 | 12 |
| Posture | 14 (8–16) * | 1.94 | 9 | 14 (10–18) | 1.85 | 13 |
| Movements | 6 (2–6) | 0.98 | 3 | 6 (4–6) | 0.54 | 4 |
| Tone | 16 (7–24) * | 2.82 | 13 | 18 (10–24) | 2.99 | 14 |
| Reflexes | 7 (3–12) ** | 1.69 | 4 | 8 (5–13) | 1.89 | 5 |
| Total score | 56 (28–68) ** | 6.98 | 48 | 62 (43–76) | 6.5 | 54 |
| HINE Sections | Cognitive | Language | Motor | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Coeff | CI | N | Coeff | CI | N | Coeff | CI | |
| Function of cranial nerves | 49 | 0.25 | −0.2,3.5 * | 48 | 0.22 | −0.45, 3.7 | 49 | 0.45 | 1.1,4.3 ** |
| Posture | 49 | 0.27 | −0.06, 2.78 * | 48 | 0.13 | −1, 2.5 | 49 | 0.26 | −0.1, 2.8 * |
| Movements | 49 | 0.08 | −2.1, 3.7 | 48 | 0.42 | −3, 4.1 | 49 | 0.37 | 1, 6.5 ** |
| Tone | 49 | 0.37 | 0.32, 2.2 ** | 48 | 0.15 | −0.56, 1.87 | 49 | 0.32 | −0.13, 2 ** |
| Reflexes | 49 | 0.06 | −1.3, 2 | 48 | 1 | −2.9, 1.2 | 49 | 0.1 | −1.1, 2.3 |
| Total score | 49 | 0.3 | −0.04, 0.82 ** | 48 | 0.13 | −0.28, 0.7 | 49 | 0.39 | −0.16, 0.94 ** |
| HINE Sections | Cognitive | Language | Motor | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Coeff | CI | N | Coeff | CI | N | Coeff | CI | |
| Function of cranial nerves | 49 | 0.06 | −2.1, 3.2 | 48 | 1 | −2.1, 4.4 | 49 | 0.27 | −0.15,5.15 * |
| Posture | 49 | 0.05 | −1.3,1.8 | 48 | −0.53 | −1.5, 2.3 | 49 | 0.2 | −0.5, 2.6 |
| Movements | 49 | 0.07 | −4, 6.6 | 48 | 0.05 | −5.3, 7.6 | 49 | 0.36 | −1.58, 11.7 ** |
| Tone | 49 | 0.22 | −0.2, 1.7 | 48 | 0.09 | −0.8, 1.6 | 49 | 0.27 | −0.05, 1.84 * |
| Reflexes | 49 | 0.12 | −0.9, 2 | 48 | −0.06 | −1.47, 2.3 | 49 | 0.25 | −0.2, 2.8 * |
| Total score | 49 | 0.16 | −0.2, 0.7 | 48 | −0.09 | −0.38, 0.7 | 49 | 0.2 | 0.05, 0.9 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kyriakidou, M.; Chatziioannidis, I.; Mitsiakos, G.; Lampropoulou, S.; Pouliakis, A. Neurodevelopmental Outcome in Extremely Low Birth Weight Infants at 2–3 Years of Age. Medicina 2020, 56, 649. https://doi.org/10.3390/medicina56120649
Kyriakidou M, Chatziioannidis I, Mitsiakos G, Lampropoulou S, Pouliakis A. Neurodevelopmental Outcome in Extremely Low Birth Weight Infants at 2–3 Years of Age. Medicina. 2020; 56(12):649. https://doi.org/10.3390/medicina56120649
Chicago/Turabian StyleKyriakidou, Maria, Ilias Chatziioannidis, Georgios Mitsiakos, Sofia Lampropoulou, and Abraham Pouliakis. 2020. "Neurodevelopmental Outcome in Extremely Low Birth Weight Infants at 2–3 Years of Age" Medicina 56, no. 12: 649. https://doi.org/10.3390/medicina56120649
APA StyleKyriakidou, M., Chatziioannidis, I., Mitsiakos, G., Lampropoulou, S., & Pouliakis, A. (2020). Neurodevelopmental Outcome in Extremely Low Birth Weight Infants at 2–3 Years of Age. Medicina, 56(12), 649. https://doi.org/10.3390/medicina56120649





