Nurses Training and Capacitation for Palliative Care in Emergency Units: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Information Sources and Search Criteria
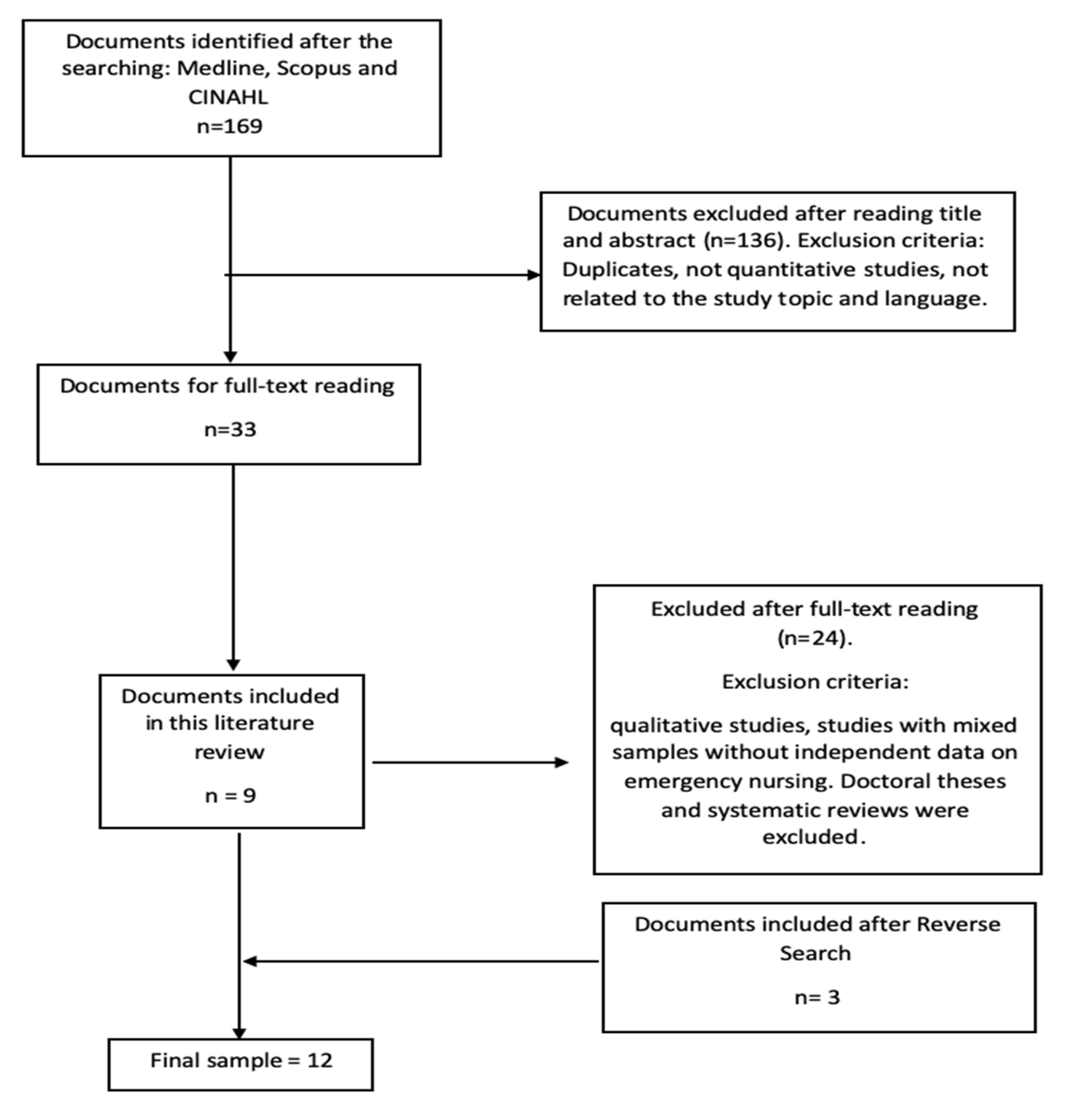
2.2. Studies Selection Process and Evidence Level
2.3. Data Collection and Data Analysis
3. Results
3.1. Studies Selection and Characteristics of the Studies
3.2. Nurses’ Training, Capacitation and Interventions in Palliative Care Patients that Visit Emergency Services
3.2.1. Emergency Nurses Interventions for Terminal Patients
3.2.2. Emergency Nurses Training and Capacitation for PC
3.3. Access Model to Palliative Care in ES and Influence of PC Nurses in the ES
3.3.1. Access to Palliative Care. Emergency Department-Palliative Service (ED-PALS) Care Model
3.3.2. Influence of Palliative Care Nurses in the Emergency Service
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- WHO. Ageing and Life-Course. Available online: https://www.who.int/ageing/about/facts/en/ (accessed on 5 September 2020).
- Adhanom-Ghebreyesus, T. Palliative Care Who. Available online: https://www.who.int/cancer/palliative/es/ (accessed on 18 May 2020).
- National Institute of Statistics. Available online: https://www.ine.es/ (accessed on 13 June 2020).
- Abellán-García, A.; Aceituno-Nieto, P.; Pérez-Días, J.; Ramiro-Fariñas, D.; Ayala-García, A.; Pujol-Rodríguez, R. A profile of the elderly in Spain. Net. Aging Rep. 2019, 22, 5–38. [Google Scholar]
- Andalusian Palliative Care Plan. Available online: https://www.redpal.es/plan-andaluz-de-cuidados-paliativos/ (accessed on 10 June 2020).
- Buigues-Mengual, F.; Torres-Pérez, J.; Mas-Sesé, G.; Femenía-Pérez, M.; Baydal-Cardona, R. Terminal Patient. Clinical Action Guide. 2020. Available online: http://www.san.gva.es/documents/246911/251004/guiasap027terminal.pdf (accessed on 18 May 2020).
- Hill, J.; Cuthel, A.m.; Lin, P.; Grudzen, C.R. Primary Palliative Care for Emergency Medicine (PRIM-ER), 2020. Applying form and function to a theory-based complex intervention. Contemp. Clin. Trials Commun. 2020, 18, 100570. [Google Scholar] [CrossRef] [PubMed]
- Basol, N. The integration of palliative care into the emergency department. Turk. J. Emerg. Med. 2016, 15, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Grudzen, C.R.; Stone, S.C.; Sean Morrison, R. The palliative care model for emergency department patient with advanced illness. J. Palliat. Med. 2011, 14, 945–950. [Google Scholar] [CrossRef] [PubMed]
- OCEBM. Levels of Evidence-CEBM. Available online: https://www.cebm.net/2016/05/ocebm-levels-of-evidence/ (accessed on 22 April 2020).
- Pereira, M.; Barbosa, A.; Dixe, M. Palliative care for end-of-life patients in a basic emergency service. Scand. J. Caring Sci. 2018, 32, 1056–1063. [Google Scholar] [CrossRef]
- Sutradhar, R.; Barbera, L.; Seow, H.Y. Palliative homecare is associated with reduced high- and low-acuity emergency department visits at the end of life: A population-based cohort study of cancer decedents. Palliat. Med. 2017, 31, 448–455. [Google Scholar] [CrossRef]
- Alsirafy, S.A.; Raheem, A.A.; Al-Zahrain, A.S.; Mohamed, A.A.; Sherisher, M.A.; El-Kashif, A.T.; Ghanem, H.M. Emergency department visits at the end of life of patients with terminal cancer: Pattern, causes, and avoidance. Am. J. Hosp. Palliat. Med. 2016, 33, 658–662. [Google Scholar] [CrossRef]
- Koh, M.Y.H.; Lee, J.F.; Montalbán, S.; Foo, C.L.; Hum, A.Y.M. ED-PALS: A comprehensive palliative care service for oncology patients in the emergency department. Am. J. Hosp. Palliat. Care 2019, 36, 571–576. [Google Scholar] [CrossRef]
- Barbera, L.; Taylor, C.; Dudgeon, D. Why do patients with cancer visit De emergency department near the end of life? Can. Med. Assoc. J. 2010, 182, 563–568. [Google Scholar] [CrossRef]
- Weng, T.-C.; Yang, Y.-C.; Chen, P.-J.; Kuo, W.-F.; Wang, W.-L.; Ke, Y.-T.; Hsu, C.-C.; Lin, K.-C.; Huang, C.-C.; Chien, T.-W. Implementing a novel model for hospice and palliative care in the emergency department: An experience from a tertiary medical center in Taiwan. Medicine 2017, 96, e6943. [Google Scholar] [CrossRef]
- Shearer, F.M.; Rogers, I.R.; Monterosso, L.; Ross-Adjie, G.; Rogers, J.R. Understanding emergency department staff needs and perceptions in the provision of palliative care. Emerg. Med. Australas 2014, 26, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Russ, A.; Mountain, D.; Rogers, I.R.; Shearer, F.; Monterosso, L.; Ross-Adjie, G.; Rogers, J.R. Staff perceptions of palliative care in a public Australian, metropolitan emergency department. Emerg. Med. Australas 2015, 27, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Weiland, T.J.; Lane, H.; Jelinek, G.A.; Marck, C.H.; Weil, J.; Boughey, M.; Philip, J. Managing the advanced cancer patient in the Australian Department of emergency: Findings from a national survey of emergency department physicians. Int. J. Emerg. Med. 2015, 8, 4. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Babarro, A.; Astray-Mochales, J.; Domínguez-Berjón, F.; Gènova-Maleras, R.; Bruera, E.; Díaz-Mayordomo, A.; Cortes, C.C. The association between in-patient death, utilization of hospital resources and availability of palliative home care for cancer patients. Palliat. Med. 2013, 27, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Seow, H.; Brazil, K.; Sussman, J.; Pereira, J.; Marshall, D.; Austin, P.C.; Husain, A.; Rangrej, J.; Barbera, L. Impact of community based, specialist palliative care teams on hospitalizations and emergency department visits late in life and hospital deaths: A pooled analysis. BMJ 2014, 348, g3496. [Google Scholar] [CrossRef]
- Kitsler, E.A.; Morrison, R.S.; Richardson, L.D.; Ortiz, J.M.; Grudzen, Q.C. Emergency Department-triggered Palliative Care in Advanced Cancer: Proof of Concept. Acad. Emerg. Med. 2015, 22, 237–239. [Google Scholar] [CrossRef]
- Carpenter, C.R.; Melady, D.; Krausz, C.; Wagner, J.; Froelke, B.; Cordia, J.; Lowery, D.; Ruoff, B.E.; Byrne, L.E.; Miller, D.K.; et al. Improving care in the emergency department for elderly people of Missouri: Guidelines, accreditation and collaboration. Mo Med. 2017, 114, 447–452. [Google Scholar]
- Perera-Milian, L.S.; Aguilar-Hernández, I.; Oliva-Pino, M. Palliative care in terminal patients. Medimay 2016, 23, 1–6. [Google Scholar]
- Ersek, M.; Hickman, S.E.; Thomas, A.C.; Bernard, B.; Unroe, K.T. Stakeholder Perspectives on the Optimizing Patient Transfers, Impacting Medical Quality, and Improving Symptoms: Transforming Institutional Care (OPTIMISTIC) Project. Gerontologist 2018, 58, 1177–1187. [Google Scholar] [CrossRef]
- Hickman, S.E.; Miech, E.J.; Stump, T.E.; Fowler, N.R.; Unroe, K.T. Identifying the Implementation Conditions Associated With Positive Outcomes in a Successful Nursing Facility Demonstration Project. Gerontologist 2020. [Google Scholar] [CrossRef]
- Gonella, S.; Clari, M.; Basso, I.; Di Giulio, P. What contributes to family carers’ decision to transition towards palliative-oriented care for their relatives in nursing homes? Qualitative findings from bereaved family carers’ experiences. Palliat. Support. Care 2020, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Park, T.; Hegadoren, K.; Workun, B. Working at the Intersection of Palliative End-of-Life and Mental Health Care: Provider Perspectives. J. Palliat. Care 2020, 825859720951360. [Google Scholar] [CrossRef] [PubMed]
- Revels, A.; Sabo, B.; Snelgrove-Clarke, E.; Price, S.; Field, S.; Helwig, M. Experiences of emergency department nurses in providing palliative care to adults with advanced cancer: A systematic review protocol. JBI Database Syst. Rev. Implement. Rep. 2016, 14, 75–86. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, M.P.; Chaves, C. Role of palliative care in the emergency service. Med. Leg. Costa Rica 2017, 34, 165–174. [Google Scholar]
- Hwang, U.; Dresden, S.M.; Rosenberg, M.S.; Garrido, M.M.; Loo, G.; Sze, J.; Mba, S.G.; Courtney, D.M.; Kang, R.; Zhu, C.W.; et al. Geriatric emergency department. Innovations: Transition care nurses and hospital use. J. Am. Geriatr. Soc. 2018, 66, 459–466. [Google Scholar] [CrossRef]
- Mills, S.E.E.; Geneen, L.J.; Buchanan, D.; Guthrie, B.; Smith, B.H. Factors associated with unscheduled care use by cancer decedents: A systematic review with narrative synthesis. BMJ Support. Palliat. Care 2020. [Google Scholar] [CrossRef]
- Chu, C.P.; Huang, C.Y.; Kuo, C.J.; Chen, Y.Y.; Chen, C.T.; Yang, T.W.; Liu, H.C. Palliative care for nursing home patients with dementia: Service evaluation and risk factors of mortality. BMC Palliat. Care 2020, 19, 122. [Google Scholar] [CrossRef]
- Trahan, L.M.; Spiers, J.A.; Cummings, G.G. Decisions to Transfer Nursing Home Residents to Emergency Departments: A Scoping Review of Contributing Factors and Staff Perspectives. J. Am. Med. Dir. Assoc. 2016, 17, 994–1005. [Google Scholar] [CrossRef]
- Hickman, S.E.; Unroe, K.T.; Ersek, M.; Stump, T.E.; Tu, W.; Ott, M.; Sachs, G.A. Systematic Advance Care Planning and Potentially Avoidable Hospitalizations of Nursing Facility Residents. J. Am. Geriatr. Soc. 2019, 67, 1649–1655. [Google Scholar] [CrossRef]
| Author Year (Nation) | Design | Sample (N) | Results Aim A (to Describe the Training, Capacitation and Interventions of Registered Nurses that Works in the ES Regarding to PC) | Results Aim B (to Describe the Influence of PC in Visits to ES and to Analyze the PC Access Model When Attending Emergency Services) | Evidence Level and Grade of Recommendation |
|---|---|---|---|---|---|
| Pereira MED et al. [11], 2017 (Portugal) | Cross-Sectional Study | 83 | The most used invasive procedures were: IV channeling, IV medication administration and intravenous therapy, blood extractions. They were performed under medical prescription. Only the usual comfort measures were performed in the service. Only 14.5% of non-essential medication was discontinued. This decision was not recorded in 83 per cent of cases. In 71.1% of cases, agony was not diagnosed. In 2.9% of those that did, it was done without recognizing at least two factors proper to agony. The factors that most helped nurses to recognize imminent death were comatose status (94%) and worsening of dyspnea (20.5%). In the face of imminent death, CPR maneuvers and aspiration of secretions were carried out. | 2c/B | |
| Sutradhar R et al. [12], 2016 (Ontario, Canada) | Cohort study | 113,902 | Home PC by nursing to terminal patients decreased the rate of emergency visits. The rate of visits to high-acuity ES (per 100 person-days) was 2.35. This rate was reduced to 0.33 during the time during which PC services were used in the home. The rate of visits to low-acuity ES (per 100 person-days) was 0.531; this rate fell to 0.0831 during the time during which PC services were used in the home. | 2b/B | |
| Alsirafy SA et al. [13], 2016. (Saudi Arabia) | Cohort study | 154 | 19% of visits to the ES were considered avoidable due to poorly controlled symptoms. | 2b/B | |
| Koh MYH et al. [14], 2019 (USA) | Cohort study | 340 | A tripartite model of collaboration between PC, ES and hospitalization is advocated. It allows earlier access to the palliative care unit and direct income to this unit and care rooms: Patients who went to the ES and could not be attended by the PC service were referred to the “PC clinics”. Patients who required hospitalization were admitted directly from the ES. | 2b/B | |
| Barbera L et al. [15], 2010 (USA) | Cohort study | 91,561 | Proper symptom control would decrease the number of unnecessary visits to the U.S. | 2b/B | |
| Weng TC et al. [16], 2017 (Taiwan) | Clinical trial | 648 | Capacity of emergency nurses to perform PC:
| 1a/A | |
| Shearer FM et al. [17], 2014 (Australia) | Cross-Sectional Study | 66. | It is claimed that more training is needed with regard to PC. Only 9.5% of respondents correctly identified the main causes of death, as cancer was overvalued and other diseases such as dementia, or COPD were undervalued. Regarding the management of physical symptoms: staff showed more confidence in symptom management, but deficiencies in ethical and communication issues. | 2c/B | |
| Russ A et al. [18], 2015. (Australia) | Cross-Sectional Study | 65 | All staff were comfortable with managing the symptoms. There is a need to increase PC training, especially in ethical and communication issues. The nurses reflected the existence of legal problems that limit the provision of PC. Causes of death in PC patients: emergency personnel overestimate cancer as a cause of death and underestimate other non-cancerous diagnoses. | 2c/B | |
| Weiland TJ et al. [19], 2015 (Australia) | Cross-Sectional Study | 681 | Environmental barriers: most respondents agreed that work overload, lack of privacy, lack of time, and noise affected patient care. 73.6% felt unable to proportional the desired level of care to patients with advanced cancer in the U.S. (for reasons independent of training). | Access to PC in ES: 80% of participants had access to specialized PC services 35.1% reported having a PC unit for hospitalized patients with available beds. 14.7% had no access or reference to external PC services | 2c/B |
| Alonso-Babarro A at al [20], 2013 (Spain) | Cross-Sectional Study | 200,000 | 524 patients were studied to determine the place of death. A total of 387 (74%) patients died in the hospital, 90 (17%) died in the Home, 29 (6%) died in one and 18 (3%) died in a nursing home. The frequency of hospital death was significantly lower among patients in the area with Home PC equipment (ECPD) (61% versus 77%, p < 0.001). Patients in the area with PC equipment used ES less frequently than those in the area without Home PC equipment (68% versus 79%, p = 0.004 and 66 versus 76%, p = 0.012, respectively). The mean number of days of hospitalization among patients who died in the home was 7, compared to 17 Days of patients who died in the hospital (p <0.001) | 2c/B | |
| Seow H et al. [21], 2014 (Canadá) | Cohort study | 3109 | In the exposed group (patients with PC team), 970 (31.2%) were in the hospital and 896 (28.9%) had an ES visit in the last two weeks of life, respectively, compared to 1219 (39.3%) and 1070 (34.5%) in the non-exposed group. Fewer exposed patients than non-exposed patients died in the hospital. Specialized community-based PC teams were effective in reducing emergency room visits and hospital deaths. There is a difficulty in communicating with the PC unit outside working hours | 2b/B | |
| Kitsler EA et al. [22], 2015 (USA) | Clinical trial | 134 | The experimental group was referred directly to PC (in addition to the corresponding emergency consultation) by the research team when analyzing its medical history. The control group was only derived if requested by the Attending Physician. 88% of the intervention group received care from the palliative care team during their admission, compared to 18% of the control group. In the experimental group palliative care was received on average about 1.48 days compared to the 2.9 days in the control group. | 1a/A |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ortega Romero, S.; Velando-Soriano, A.; Romero-Bejar, J.L.; Vargas-Román, K.; Albendín-García, L.; Suleiman-Martos, N.; Cañadas-De la Fuente, G.A. Nurses Training and Capacitation for Palliative Care in Emergency Units: A Systematic Review. Medicina 2020, 56, 648. https://doi.org/10.3390/medicina56120648
Ortega Romero S, Velando-Soriano A, Romero-Bejar JL, Vargas-Román K, Albendín-García L, Suleiman-Martos N, Cañadas-De la Fuente GA. Nurses Training and Capacitation for Palliative Care in Emergency Units: A Systematic Review. Medicina. 2020; 56(12):648. https://doi.org/10.3390/medicina56120648
Chicago/Turabian StyleOrtega Romero, Sonia, Almudena Velando-Soriano, José Luis Romero-Bejar, Keyla Vargas-Román, Luis Albendín-García, Nora Suleiman-Martos, and Guillermo Arturo Cañadas-De la Fuente. 2020. "Nurses Training and Capacitation for Palliative Care in Emergency Units: A Systematic Review" Medicina 56, no. 12: 648. https://doi.org/10.3390/medicina56120648
APA StyleOrtega Romero, S., Velando-Soriano, A., Romero-Bejar, J. L., Vargas-Román, K., Albendín-García, L., Suleiman-Martos, N., & Cañadas-De la Fuente, G. A. (2020). Nurses Training and Capacitation for Palliative Care in Emergency Units: A Systematic Review. Medicina, 56(12), 648. https://doi.org/10.3390/medicina56120648










