Influence of Burnout on Patient Safety: Systematic Review and Meta-Analysis
Abstract
1. Introduction
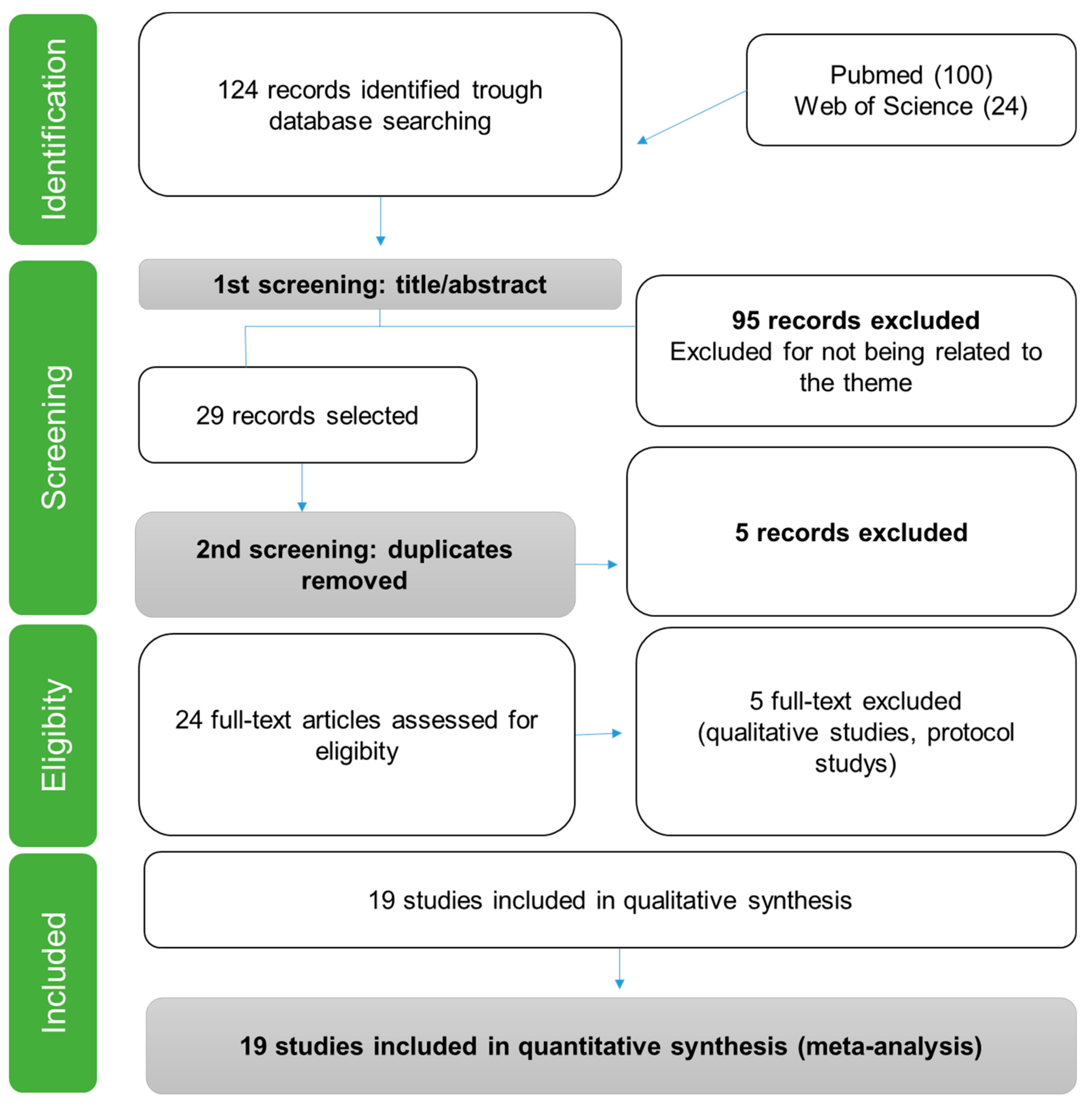
2. Materials and Methods
2.1. Search Strategy
2.2. Data Extraction and Quality Assessment
2.3. Eligibility Criteria
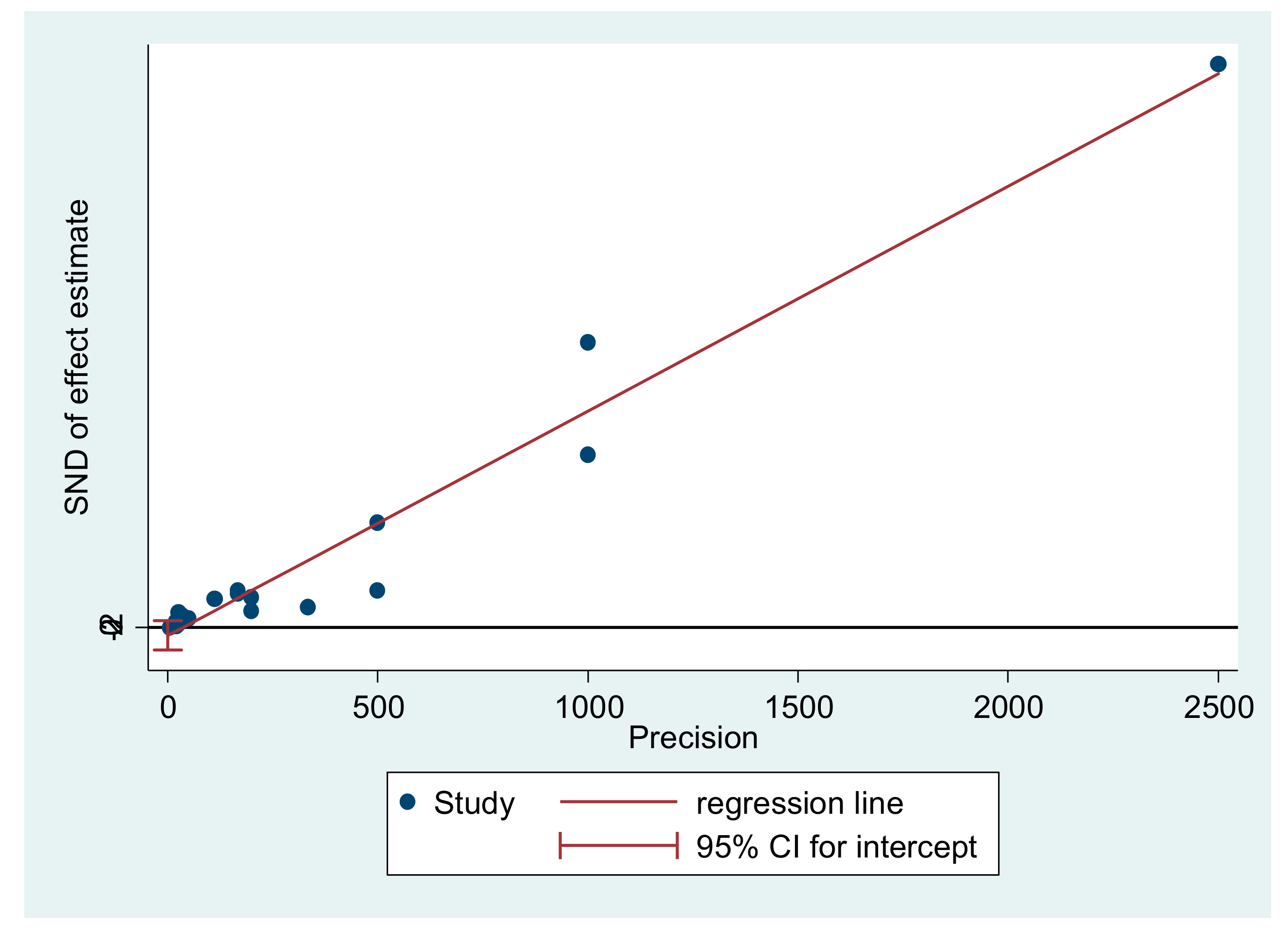
2.4. Statistical Analysis of Meta-Analysis
3. Results
Study Characteristics
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Makary, A.M.; Daniel, M. Medical error-the third leading cause of death in the US. BMJ 2016, 353, i2139. [Google Scholar] [CrossRef] [PubMed]
- Haukland, E.C.; Mevik, K.; Von Plessen, C.; Nieder, C.; Vonen, B. Contribution of adverse events to death of hospitalised patients. BMJ Open Qual. 2019, 8, e000377. [Google Scholar] [CrossRef] [PubMed]
- Bagnasco, A.; Tubino, B.; Piccotti, E.; Rosa, F.; Aleo, G.; Di Pietro, P.; Sasso, L. Identifying and correcting communication failures among health professionals working in the Emergency Department. Int. Emerg. Nurs. 2013, 21, 168–172. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.; Allen, K.; Daly, M. A Communication and Patient Safety training programme for all healthcare staff: Can it make a difference? BMJ Qual. Saf. 2012, 21, 84–88. [Google Scholar] [CrossRef] [PubMed]
- West, C.P.; Huschka, M.M.; Novotny, P.J.; Sloan, J.A.; Kolars, J.C.; Habermann, T.M.; Shanafelt, T.D. Association of Perceived Medical Errors with Resident Distress and Empathy. JAMA 2006, 296, 1071–1078. [Google Scholar] [CrossRef] [PubMed]
- Saleh, A.M.; Awadalla, N.J.; El-Masri, Y.M.; Sleem, W.F. Impacts of nurses’ circadian rhythm sleep disorders, fatigue, and depression on medication administration errors. Egypt. J. Chest Dis. Tuberc. 2014, 63, 145–153. [Google Scholar] [CrossRef]
- Hall, L.H.; Johnson, J.; Watt, I.; Tsipa, A.; O’Connor, D.B. Healthcare Staff Wellbeing, Burnout, and Patient Safety: A Systematic Review. PLoS ONE 2016, 11, e0159015. [Google Scholar] [CrossRef]
- Heeb, J.L.; Haberey-Knuessi, V. Health Professionals Facing Burnout: What Do We Know about Nursing Managers? Nurs. Res. Pract 2014, 2014, 1–7. [Google Scholar] [CrossRef]
- de Andrade, P.S.; de Olivira, T.A. Prazer e dor na docência: Revisão bibliográfica sobre a Síndrome de Burnout. Saúde Soc. 2012, 21, 129–140. [Google Scholar] [CrossRef]
- Rotenstein, L.S.; Torre, M.; Ramos, M.A.; Rosales, R.C.; Guille, C.; Sen, S.; Mata, D.A. Prevalence of Burnout Among Physicians. JAMA 2018, 320, 1131–1150. [Google Scholar] [CrossRef]
- Gómez-Urquiza, J.L.; Albendín-García, L.; Vargas-Pecino, C.; De La Fuente-Solana, E.I.; Ortega-Campos, E.M.; La Fuente, G.A.C.D. Prevalence of Burnout Syndrome in Emergency Nurses: A Meta-Analysis. Crit. Care Nurse 2017, 37. [Google Scholar] [CrossRef] [PubMed]
- Gipson, D.S.; Kirkendall, E.S.; Gumbs-Petty, B.; Quinn, T.; Steen, A.; Hicks, A.; McMahon, A.; Nicholas, S.; Zhao-Wong, A.; Taylor-Zapata, P.; et al. Development of a Pediatric Adverse Events Terminology. Pediatrics 2017, 139, e20160985. [Google Scholar] [CrossRef] [PubMed]
- Maslach, C.; Jackson, S.E.; Leiter, M.P.; Schaufeli, W.B.; Schwab, R.L. Maslach Burnout Inventory; Consulting Psychologists Press: Palo Alto, CA, USA, 1986; Volume 21. [Google Scholar]
- Maslach, C.; Goldberg, J. Prevention of burnout: New perspectives. Appl. Prev. Psychol. 1998, 7, 63–74. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E. The measurement of experienced burnout. J. Organ. Behav. 1981, 2, 99–113. [Google Scholar] [CrossRef]
- Reis, C.T.; LaGuardia, J.; Vasconcelos, A.G.G.; Martins, M. Reliability and validity of the Brazilian version of the Hospital Survey on Patient Safety Culture (HSOPSC): A pilot study. Cad. Saúde Pública 2016, 32, e00115614. [Google Scholar] [CrossRef]
- Akbari, N.; Malek, M.; Ebrahimi, P.; Haghani, H.; Aazami, S. Safety culture in the maternity unit of hospitals in Ilam province, Iran: A census survey using HSOPSC tool. Pan Afr. Med J. 2017, 27. [Google Scholar] [CrossRef] [PubMed]
- Stoyanova, R.; Dimova, R.; Tarnovska, M.; Boeva, T. Linguistic Validation and Cultural Adaptation of Bulgarian Version of Hospital Survey on Patient Safety Culture (HSOPSC). Open Access Maced. J. Med. Sci. 2018, 6, 925–930. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Altman, D.G. Assessing risk of bias in included studies. Cochrane Handb. Syst. Rev. Interv. Cochrane B Ser. 2008, 1, 187–241. [Google Scholar]
- Sexton, J.B.; Adair, K.C.; Leonard, M.W.; Frankel, T.C.; Proulx, J.; Watson, S.R.; Magnus, B.; Bogan, B.; Jamal, M.; Schwendimann, R.; et al. Providing feedback following Leadership WalkRounds is associated with better patient safety culture, higher employee engagement and lower burnout. BMJ Qual. Saf. 2018, 27, 261–270. [Google Scholar] [CrossRef]
- Dahl, A.B.; Ben Abdallah, A.; Maniar, H.; Avidan, M.S.; Bollini, M.L.; Patterson, G.A.; Steinberg, A.; Scaggs, K.; Dribin, B.V.; Ridley, C.H. Building a collaborative culture in cardiothoracic operating rooms: Pre and postintervention study protocol for evaluation of the implementation of team STEPPS training and the impact on perceived psychological safety. BMJ Open 2017, 7, e017389. [Google Scholar] [CrossRef]
- Johnson, J.; Louch, G.; Dunning, A.; Johnson, O.; Grange, A.; Reynolds, C.; Hall, L.; O’Hara, J. Burnout mediates the association between depression and patient safety perceptions: A cross-sectional study in hospital nurses. J. Adv. Nurs. 2017, 73, 1667–1680. [Google Scholar] [CrossRef] [PubMed]
- Tawfik, D.S.; Sexton, J.B.; Kan, P.; Sharek, P.J.; Nisbet, C.C.; Rigdon, J.; Lee, H.C.; Profit, J. Burnout in the neonatal intensive care unit and its relation to healthcare-associated infections. J. Perinatol. 2017, 37, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Aiken, L.H.; Sloane, D.; Griffiths, P.; Rafferty, A.M.; Bruyneel, L.; McHugh, M.; Maier, C.B.; Moreno-Casbas, T.; Ball, J.E.; Ausserhofer, D.; et al. Nursing skill mix in European hospitals: Cross-sectional study of the association with mortality, patient ratings, and quality of care. BMJ Qual. Saf. 2017, 26, 559–568. [Google Scholar] [CrossRef] [PubMed]
- Gilles, I.; Mayer, M.; Courvoisier, N.; Peytremann-Bridevaux, I. Joint analyses of open comments and quantitative data: Added value in a job satisfaction survey of hospital professionals. PLoS ONE 2017, 12, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Vifladt, A.; Simonsen, B.O.; Lydersen, S.; Farup, P.G. The association between patient safety culture and burnout and sense of coherence: A cross-sectional study in restructured and not restructured intensive care units. Intensiv. Crit. Care Nurs. 2016, 36, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Quillivan, R.R.; Burlison, J.D.; Browne, E.K.; Scott, S.D.; Hoffman, J.M.; Information, P.E.K.F.C. Patient Safety Culture and the Second Victim Phenomenon: Connecting Culture to Staff Distress in Nurses. Jt. Comm. J. Qual. Patient Saf. 2016, 42, 377–384. [Google Scholar] [CrossRef]
- Van Gerven, E.; Vander Elst, T.; Vandenbroeck, S.; Dierickx, S.; Euwema, M.; Sermeus, W.; De Witte, H.; Godderis, L.; Vanhaecht, K. Increased Risk of Burnout for Physicians and Nurses Involved in a Patient Safety Incident. Med. Care 2016, 54, 937–943. [Google Scholar] [CrossRef]
- Welp, A.; Meier, L.L.; Manser, T. The interplay between teamwork, clinicians’ emotional exhaustion, and clinician-rated patient safety: A longitudinal study. Crit. Care 2016, 20, 908. [Google Scholar] [CrossRef]
- Garrouste-Orgeas, M.; Perrin, M.; Soufir, L.; Vesin, A.; Blot, F.; Maxime, V.; Beuret, P.; Troché, G.; Klouche, K.; Argaud, L.; et al. The Iatroref study: Medical errors are associated with symptoms of depression in ICU staff but not burnout or safety culture. Intensiv. Care Med. 2015, 41, 273–284. [Google Scholar] [CrossRef]
- Profit, J.; Sharek, P.J.; Amspoker, A.B.; Kowalkowski, M.A.; Nisbet, C.C.; Thomas, E.J.; Chadwick, A.W.; Sexton, J.B. Burnout in the NICU setting and its relation to safety culture. BMJ Qual. Saf. 2014, 23, 806–813. [Google Scholar] [CrossRef]
- Milosevic, M.; Brborovic, H.; Mustajbegovic, J.; Montgomery, A. Patients and health care professionals: Partners in health care in Croatia? Br. J. Health Psychol. 2014, 19, 670–682. [Google Scholar] [CrossRef] [PubMed]
- Van Bogaert, P.; Timmermans, O.; Weeks, S.M.; van Heusden, D.; Wouters, K.; Franck, E. Nursing unit teams matter: Impact of unit-level nurse practice environment, nurse work characteristics, and burnout on nurse reported job outcomes, and quality of care, and patient adverse events—A cross-sectional survey. Int. J. Nurs. Stud. 2014, 51, 1123–1134. [Google Scholar] [CrossRef] [PubMed]
- Sexton, J.B.; Sharek, P.J.; Thomas, E.J.; Gould, J.B.; Nisbet, C.C.; Amspoker, A.B.; Kowalkowski, A.M.; Schwendimann, R.; Profit, J. Exposure to Leadership WalkRounds in neonatal intensive care units is associated with a better patient safety culture and less caregiver burnout. BMJ Qual. Saf. 2014, 23, 814–822. [Google Scholar] [CrossRef] [PubMed]
- Rathert, C.; Williams, E.S.; Lawrence, E.R.; Halbesleben, J.R. Emotional exhaustion and workarounds in acute care: Cross sectional tests of a theoretical framework. Int. J. Nurs. Stud. 2012, 49, 969–977. [Google Scholar] [CrossRef] [PubMed]
- Holden, R.J.; Patel, N.R.; Scanlon, M.C.; Shalaby, T.M.; Arnold, J.M.; Karsh, B.T. Effects of mental demands during dispensing on perceived medication safety and employee well being: A study of workload in pediatric hospital pharmacies. Res. Soc. Adm. Pharm. 2010, 6, 293–306. [Google Scholar] [CrossRef] [PubMed]
- Teng, C.I.; Shyu, Y.I.L.; Chiou, W.K.; Fan, H.C.; Lam, S.M. Interactive effects of nurse-experienced time pressure and burnout on patient safety: A cross-sectional survey. Int. J. Nurs. Stud. 2010, 47, 1442–1450. [Google Scholar] [CrossRef] [PubMed]
- Halbesleben, J.R.B.; Wakefield, B.J.; Wakefield, D.S.; Cooper, L.B. Nurse Burnout and Patient Safety Outcomes. West. J. Nurs. Res. 2008, 30, 560–577. [Google Scholar] [CrossRef] [PubMed]
- Williams, E.S.; Manwell, L.B.; Konrad, T.R.; Linzer, M. The relationship of organizational culture, stress, satisfaction, and burnout with physician-reported error and suboptimal patient care. Health Care Manag. Rev. 2007, 32, 203–212. [Google Scholar] [CrossRef]
- Spence Laschinger, H.K.; Leiter, M.P. The impact of nursing work environments on patient safety outcomes: The mediating role of burnout/engagement. J. Nurs. Adm. 2006, 36, 259–267. [Google Scholar] [CrossRef]
- Santos, M.F.; Felício, J.; de Souza, M.T. Educação em saúde no contexto da Saúde da Família na perspectiva do usuário. Interface Comun. Saúde Educ. 2012, 16, 315–329. [Google Scholar] [CrossRef]
- Cimiotti, J.P.; Aiken, L.H.; Sloane, D.M.; Wu, E.S. Nurse staffing, burnout, and health care–associated infection. Am. J. Infect. Control 2012, 40, 486–490. [Google Scholar] [CrossRef] [PubMed]
- Carayon, P.; Wetterneck, T.B.; Rivera-Rodriguez, A.J.; Hundt, A.S.; Hoonakker, P.; Holden, R.; Gurses, A.P. Human factors systems approach to healthcare quality and patient safety. Appl. Ergon. 2014, 45, 14–25. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, R.M.; Da Silva, L.M.S.; Sánchez, R.G.; Torres, R.A.M.; Guedes, M.V.C.; Oliveira, A.C.D.S. Analyzing the concept of disruptive behavior in healthcare work: An integrative review. Rev. Esc. Enferm. USP 2016, 50, 695–704. [Google Scholar] [CrossRef] [PubMed]
- Abreu, L.C.D.; Pereira, V.X.; Silva, R.P.M.; Macedo, H., Jr.; Bezerra, I.M.P. The right to scientific information: One of the main elements of the unified health system. J. Hum. Growth Dev. 2017, 27, 258. [Google Scholar] [CrossRef]
- Alves, S.A.A.; de Oliveira, M.L.B. Sociocultural aspects of health and disease and their pragmatic impact. J. Hum. Growth Dev. 2018, 28, 183. [Google Scholar] [CrossRef]
- Bezerra, I.M.P.; Sorpreso, I.C.E. Concepts and movements in health promotion to guide educational practices. J. Hum. Growth Dev. 2016, 26, 11. [Google Scholar] [CrossRef]
- Bezerra, I.M.P. Translational medicine and its contribution to public health. J. Hum. Growth Dev. 2017, 27, 6. [Google Scholar] [CrossRef][Green Version]
| Authors | Year | Country/Location | Method |
|---|---|---|---|
| Sexton et al. [20] | 2018 | United States | Cross-sectional study |
| Johnson et al. [21] | 2017 | United Kingdom | Cross-sectional study |
| Tawfik et al. [22] | 2017 | United States | Cross-sectional study |
| Aiken et al. [23] | 2017 | Belgium, England, Finland, Ireland, Spain, and Switzerland | Cross-sectional study |
| Gilles, Courvoisier, and Peytremann-Bridevaux [24] | 2017 | Switzerland | Cross-sectional study |
| Vifladt et al. [25] | 2016 | Norway | Cross-sectional study |
| Quillivan et al. [26] | 2016 | United States | Cross-sectional study |
| Gerven et al. [27] | 2016 | Belgium | Cross-sectional study |
| Welp, Meier, and Manser [28] | 2016 | Switzerland | Longitudinal study |
| Garrouste-Orgeas et al. [29] | 2015 | France | Prospective, observational, and multicentric Study |
| Profit et al. [30] | 2014 | United States | Cross-sectional study |
| Bogaert et al. [31] | 2014 | Belgium | Cross-sectional study |
| Sexton et al. [32] | 2014 | United States | Cross-sectional study |
| Rathert et al. [33] | 2012 | United States | Cross-sectional study |
| Holden et al. [34] | 2011 | United States | Cross-sectional study |
| Teng et al. [35] | 2010 | Taiwan | Cross-sectional study |
| Halbesleben et al. [36] | 2008 | United States | Cross-sectional study |
| Williams et al. [37] | 2007 | United States | Cross-sectional study |
| Spence Laschinger and Leiter [38] | 2006 | Canada | Cross-sectional study |
| Authors | Objective | Main Results |
|---|---|---|
| Sexton et al. [20] | Evaluate the associations between receiving comments on actions taken as a result of the patient safety visit routine walk rounds (WR) and health worker assessments of patient safety culture, employee involvement, burnout, and work–life balance life. | Feeling as if health professionals have minimal control over quality of care through patient safety visit routine walk rounds (WR) can reduce their own perceptions of burnout, for example, that they are working too hard or feeling frustrated at work. These findings indicate that feedback WR may provide a significant opportunity to reduce fatigue. |
| Johnson et al. [21] | To investigate the relationships between depressive symptoms, burnout, and patient safety perceptions. | When tested in separate analyses, depressive symptoms and facets of burnout were associated with patient safety measures. In addition, the proposed mediation model was supported, with associations between depressive symptoms and patient safety perceptions fully mediated by burnout. |
| Tawfik et al. [22] | To examine the prevalence of burnout among California’s neonatal intensive care units (NICUs) and test the relationship between infection due to burnout and healthcare associated infections (HAI) rates in very low birth weight infants (VLBW). | Variable prevalence of burnout was found in the surveyed NICUs (mean 25.2 ± 10.1%). HAI rates were 8.3 ± 5.1% during the study period. The highest prevalence of burnout was found among nursing professionals and respiratory therapists, day shift workers, and workers with five or more years of service. |
| Aiken et al. [23] | To determine the association of hospital nursing skill mixed with patient mortality, care patient assessments, and quality of care indicators. | In a standard hospital, almost 30% of nurses scored high on the burnout scale, and a similar percentage expressed dissatisfaction with their jobs. |
| Gilles, Courvoisier, and Peytremann-Bridevaux [24] | To qualitatively analyze the open comments included in a job satisfaction survey and align these with quantitative results. | About a third of the comments addressed scheduling issues, mainly related to change-related problems and exhaustion, work–life balance, difficulties with colleagues’ absences, and the consequences for quality of care and patient safety. While some comments were provided equally by all professional groups, others were group-specific, as follows: work pressures and hierarchy observed by physicians, quality of health and patient safety noted by nurses, and skill recognition mentioned by administrative staff. |
| Vifladt et al. [25] | Examine the relationship between the perception of registered nurses (RNs) on patient safety culture, burnout, and sense of coherence, and compare burnout and the sense of coherence in ICUs restructured and not restructured. | A positive safety culture was statistically significantly associated with a low burnout score and a strong sense of coherence. No statistically significant differences were found in burnout and sense of coherence between restructured and non-restructured ICUs. |
| Quillivan et al. [26] | To evaluate the influence of patient safety culture on the distress related to the second victim. | Of the 358 nurses from a specialized pediatric hospital, 169 (47.2%) completed two surveys (patient safety culture and the second victim experience and support tool). Hierarchical linear regression demonstrated that the size of the patient safety culture survey and non-positive response to error was significantly associated with reductions in the second victim’s psychological, physical, and occupational survey dimensions (p < 0.001). As a mediator, organizational support fully explained the nonpunitive response to error, physical anguish and the nonpunitive response to professional-error relationships, and partially explained the unpalpable response to the psychological-error relationship. |
| Gerven et al. [27] | To investigate the prevalence of health professionals personally involved in a patient safety incident (PSI), as well as the relationship of involvement and degree of harm with problematic medication use, excessive alcohol consumption, risk of burnout, work–home interference (WHI), and turnover intentions | Nine percent of the total sample was involved in an PSI during the previous 6 months. Involvement in a PSI was related to a higher risk of burnout (β = 0.40, OR = 2.07), to problematic drug use (β = 0.33, OR = 1.84), to higher WHI (β = 0.24), and higher turnover intentions (β = 0.22). Injury to the patient was a predictor of problematic medication use (β = 0.14, OR = 1.56), risk of burnout (β = 0.16, OR = 1.62), and WHI (β = 0.19). |
| Welp, Meier, and Manser [28] | The study focused on the long-term development of teamwork, emotional exhaustion, and patient safety in interprofessional intensive care teams, exploring the causal relationships between these constructs. A secondary objective was to break down the effects of interpersonal and cognitive behavioral teamwork. | Emotional exhaustion had a lagged effect on interpersonal teamwork. In addition, interpersonal and cognitive behavioral teamwork influenced each other. Finally, cognitive behavioral teamwork predicted clinician-rated patient safety. |
| Garrouste-Orgeas et al. [29] | To assess whether burnout, depression symptoms, and safety culture affect the frequency of medical errors and adverse events in ICUs. | The symptoms of depression were an independent risk factor for medical errors. Burnout was not associated with medical errors. The safety culture score had a limited influence on medical errors. Other independent risk factors for medical errors or adverse events were related to ICU organization (40% of ICU staff out of work the day before), staff (safety-specific training), and patients (workload). |
| Profit et al. [30] | Examine the relationships between burnout in neonatal intensive care units (NICUs) and patient safety culture. | The percentage of participants in each NICU reporting burnout ranged from 7.5% to 54.4%. Burnout varied significantly between NICUs, p < 0.0001, but was less prevalent in physicians compared to non-physicians. NICUs with higher burnout scores had a lower teamwork climate, safety climate, job satisfaction, management perceptions, and working conditions. |
| Bogaert et al. [31] | Investigate the impact of factors of the nurse’s practice environment, nurse work characteristics, and nurse burnout reported work outcomes, quality of care, and patient adverse event variables at the nursing unit level. | Several unit-level associations (simple models) were identified between factors of the nurse’s practice environment, nurse’s work characteristics, burnout dimensions, and outcome variables reported by the nurse. Multiple multilevel models showed several independent variables, such as unit-level nursing management, social capital, emotional exhaustion, and depersonalization, as important predictors of nurse-reported outcome variables, such as job satisfaction, turnover intentions, quality, patient and family complaints, patient and family verbal abuse, patient falls, nosocomial infections, and medication errors. |
| Sexton et al. [32] | Compare stress perceptions and intensity among hospital shift nurses across three countries: Israel, USA (Ohio State), and Thailand. | The patient safety leadership walk rounds tool has been associated with improved safety culture outcomes and lower NICU burnout rates. |
| Rathert et al. [33] | Based on the resource conservation theory, the study examined a conceptual model that links the job environment with alternative solutions in acute care nurses and other clinicians, and the hypothesis that burnout (specifically emotional exhaustion) intervene this relationship. | The hypotheses were examined using structural equation modeling. Time pressure was positively related to exhaustion, and autonomy was negatively related. Exhaustion was positively related to alternative solutions and mediated the time pressure and autonomy for alternative solution relations. Contrary to expectations, the physical environment was directly and negatively related to alternative solutions. |
| Holden et al. [34] | This study sought to measure the effect of workload on safety and outcomes of workers in two pediatric hospitals using a new approach to workload measurement. | Pharmacists and pharmacy technicians reported high levels of external and internal mental demands during dispensation. The study supported the hypothesis that external demands (interruptions, divided attention, and running) negatively impacted medication safety and employee welfare outcomes. However, as hypothesized, increasing levels of internal demands (concentration and effort) were not associated with a higher perceived probability of error, adverse drug events, or burnout, and even had a positive effect on job satisfaction. |
| Teng et al. [35] | Investigate how time pressure and the interaction of nurse’s time pressure and burnout affect patient safety. | While regression analysis results suggest that time pressure did not significantly affect patient safety (β = −0.0, p > 0.05), time pressure and burnout had an interactive effect on patient safety (β = −0.08, p < 0.05). Specifically, for nurses with high burnout (n = 223), time pressure was negatively related to patient safety (β = −10, p < 0.05). |
| Halbesleben et al. [36] | To analyze the relationship between burnout and patient safety indicators in nurses. | After controlling for work-related demographics, multiple regression analysis supported the prediction that burnout was associated with perceived lower patient safety. Burnout was not associated with event reporting behavior but was negatively associated with reporting errors that did not lead to adverse events. |
| Williams et al. [37] | To investigate the cultural conditions that affect medical stress, dissatisfaction, and burnout syndrome by examining whether they offer poor quality of care. | Cultural emphasis on quality played a key role in quality outcomes. In addition, it was found that stressed and dissatisfied doctors report a higher probability of making mistakes and more frequent cases of sub-optimal patient care, associating this result with burnout syndrome. |
| Spence Laschinger and Leiter [38] | To test a theoretical model of professional nursing environments linking the conditions of professional nursing practice to burnout, and subsequently, to patient safety outcomes. | Nursing leadership played a key role in the quality of working life in relation to political involvement, staffing levels, support for a nursing care model (vs. physician), and nurse/physician relationships. Staff adequacy directly affected emotional exhaustion, and the use of a nursing care model had a direct effect on nurses’ personal fulfillment. Both directly affected patient safety outcomes. |
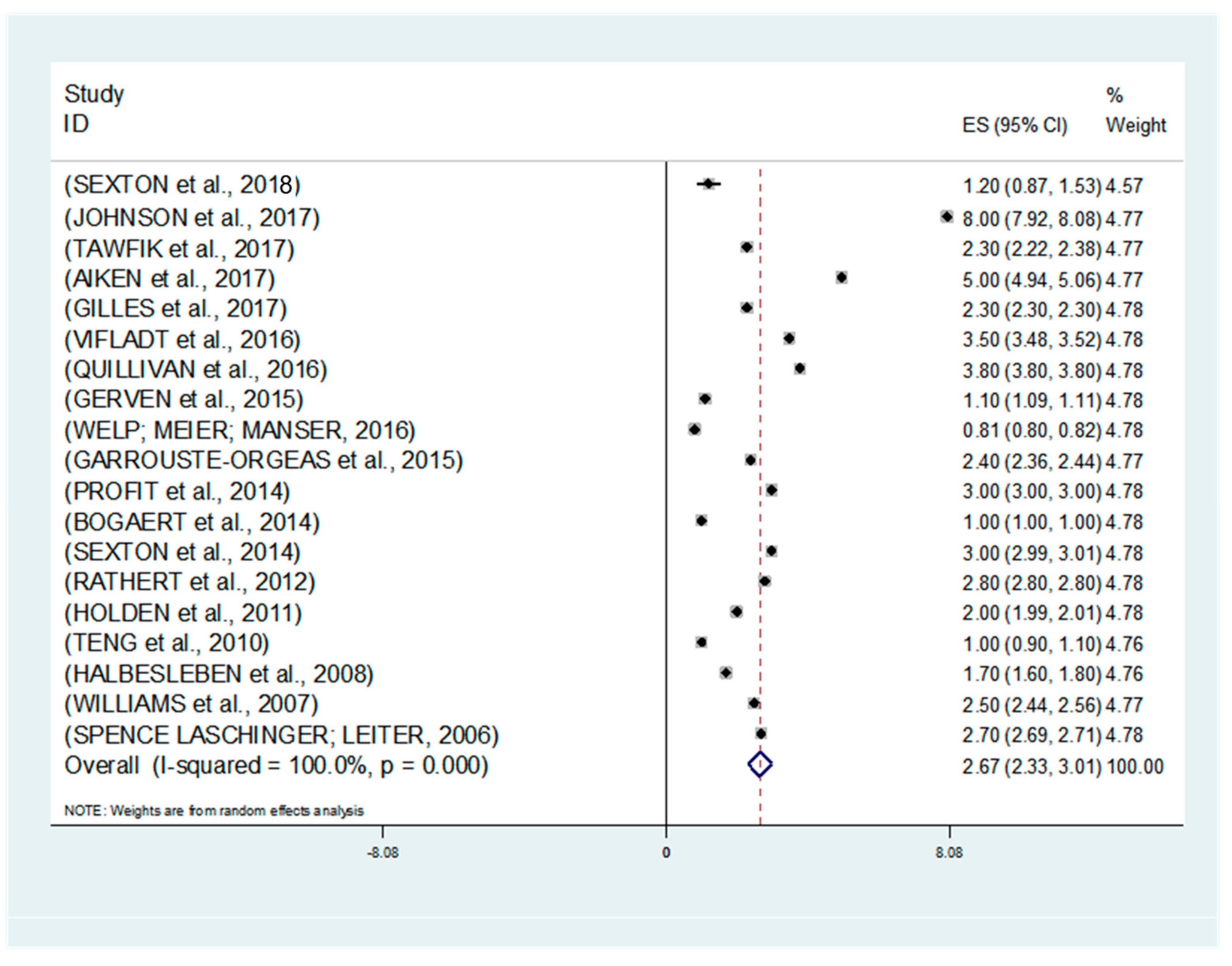
| Study | ES | 95% Conf. Interval | %Weight | |
|---|---|---|---|---|
| Sexton et al. [20] | 0.32 | 0.32 | 0.33 | 4.84 |
| Johnson et al. [21] | 0.77 | 0.73 | 0.82 | 4.78 |
| Tawfik et al. [22] | 0.72 | 0.70 | 0.74 | 4.83 |
| Aiken et al. [23] | 0.77 | 0.76 | 0.78 | 4.84 |
| Gilles. Courvoisier. and Peytremann-Bridevaux [24] | 0.42 | 0.41 | 0.44 | 4.84 |
| Vifladt et al. [25] | 0.49 | 0.44 | 0.55 | 4.74 |
| Quillivan et al. [26] | 0.47 | 0.42 | 0.52 | 4.76 |
| Gerven et al. [27] | 0.52 | 0.51 | 0.53 | 4.84 |
| Welp. Meier. and Manser [28] | 0.71 | 0.69 | 0.73 | 4.83 |
| Garrouste-Orgeas et al. [29] | 0.52 | 0.50 | 0.55 | 4.82 |
| Profit et al. [30] | 0.51 | 0.49 | 0.53 | 4.83 |
| Bogaert et al. [31] | 0.72 | 0.69 | 0.75 | 4.82 |
| Sexton et al. [32] | 0.72 | 0.70 | 0.74 | 4.83 |
| Rathert et al. [33] | 0.50 | 0.47 | 0.53 | 4.81 |
| Holden et al. [34] | 0.73 | 0.67 | 0.78 | 4.73 |
| Teng et al. [35] | 0.49 | 0.44 | 0.53 | 4.77 |
| Halbesleben et al. [36] | 0.50 | 0.40 | 0.60 | 4.55 |
| Williams et al. [37] | 0.59 | 0.54 | 0.63 | 4.77 |
| Spence Laschinger and Leiter [38] | 0.70 | 0.69 | 0.71 | 4.84 |
| Random pooled ES | 0.60 | 0.51 | 0.68 | 100.0 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garcia, C.d.L.; Abreu, L.C.d.; Ramos, J.L.S.; Castro, C.F.D.d.; Smiderle, F.R.N.; Santos, J.A.d.; Bezerra, I.M.P. Influence of Burnout on Patient Safety: Systematic Review and Meta-Analysis. Medicina 2019, 55, 553. https://doi.org/10.3390/medicina55090553
Garcia CdL, Abreu LCd, Ramos JLS, Castro CFDd, Smiderle FRN, Santos JAd, Bezerra IMP. Influence of Burnout on Patient Safety: Systematic Review and Meta-Analysis. Medicina. 2019; 55(9):553. https://doi.org/10.3390/medicina55090553
Chicago/Turabian StyleGarcia, Cíntia de Lima, Luiz Carlos de Abreu, José Lucas Souza Ramos, Caroline Feitosa Dibai de Castro, Fabiana Rosa Neves Smiderle, Jaçamar Aldenora dos Santos, and Italla Maria Pinheiro Bezerra. 2019. "Influence of Burnout on Patient Safety: Systematic Review and Meta-Analysis" Medicina 55, no. 9: 553. https://doi.org/10.3390/medicina55090553
APA StyleGarcia, C. d. L., Abreu, L. C. d., Ramos, J. L. S., Castro, C. F. D. d., Smiderle, F. R. N., Santos, J. A. d., & Bezerra, I. M. P. (2019). Influence of Burnout on Patient Safety: Systematic Review and Meta-Analysis. Medicina, 55(9), 553. https://doi.org/10.3390/medicina55090553




