Subclinical and Asymptomatic Atrial Fibrillation: Current Evidence and Unsolved Questions in Clinical Practice
Abstract
:1. Introduction
2. Definitions
3. Pathophysiological Links between AF, Dementia, and Stroke
4. Asymptomatic AF and Its Impact on Prognosis
5. Screening for Atrial Fibrillation
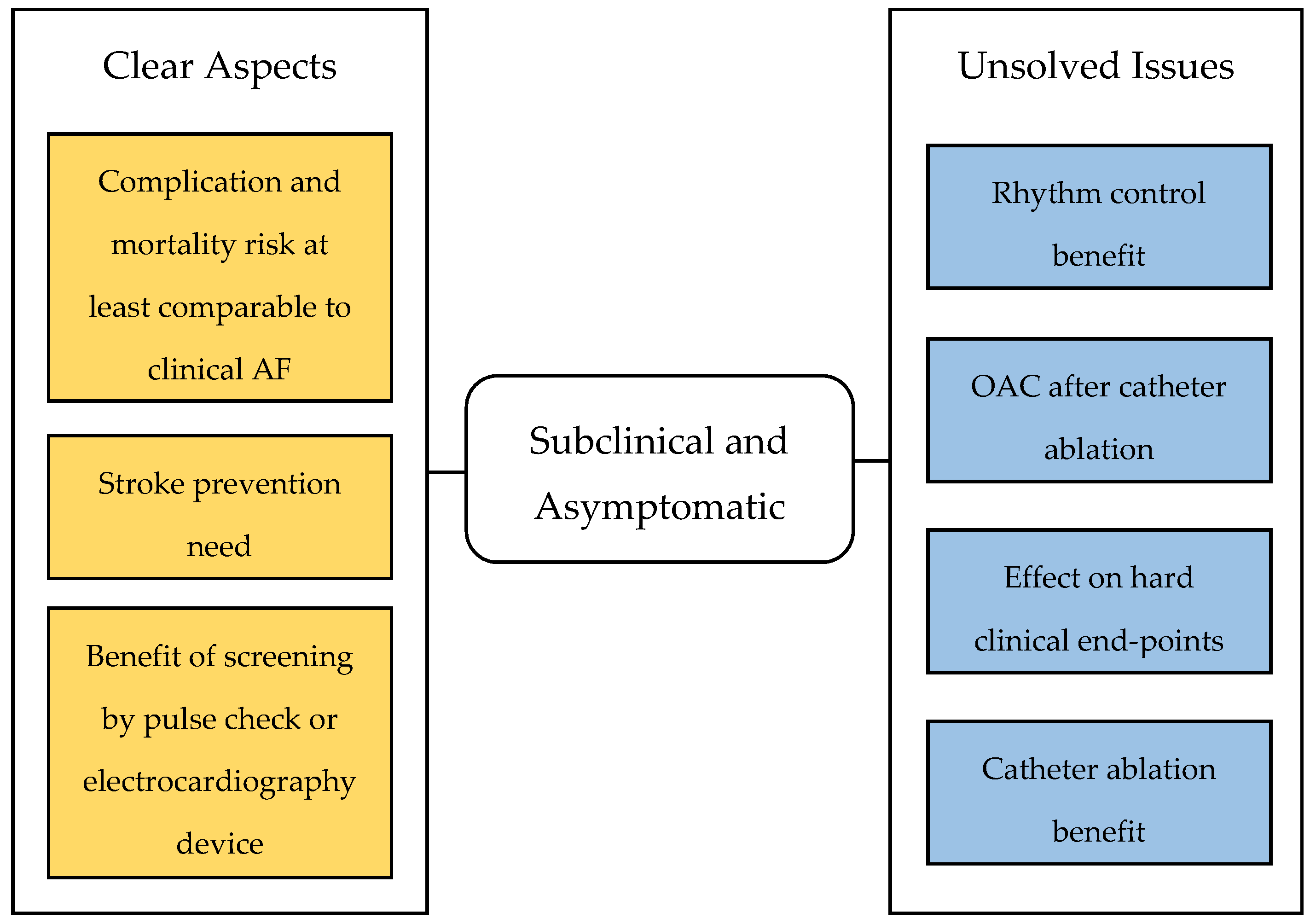
6. Management of Subclinical and Asymptomatic AF
6.1. Clinical Approach to the Patient with Asymptomatic Atrial Fibrillation
6.2. Anticoagulation Therapy
6.3. Anti-Arrhythmic Drug Management
6.4. Catheter Ablation
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Andrade, J.; Khairy, P.; Dobrev, D.; Nattel, S. The clinical profile and pathophysiology of atrial fibrillation: Relationships among clinical features, epidemiology, and mechanisms. Circ. Res. 2014. [Google Scholar] [CrossRef] [PubMed]
- Wolf, P.A.; Abbott, R.D.; Kannel, W.B. Atrial fibrillation as an independent risk factor for stroke: The Framingham Study. Stroke 1991, 22, 983–988. [Google Scholar] [CrossRef] [PubMed]
- Kalantarian, S.; Stern, T.A.; Mansour, M.; Ruskin, J.N. Cognitive Impairment Associated With Atrial Fibrillation: A Meta-analysis. Ann. Intern. Med. 2013, 158, 338. [Google Scholar] [CrossRef] [PubMed]
- Saglietto, A.; Matta, M.; Gaita, F.; Jacobs, V.; Bunch, T.J.; Anselmino, M. Stroke-independent contribution of atrial fibrillation to dementia: A meta-analysis. Open Heart 2019, 6, e000984. [Google Scholar] [CrossRef] [PubMed]
- Kirchhof, P.; Benussi, S.; Kotecha, D.; Ahlsson, A.; Atar, D.; Casadei, B.; Castella, M.; Diener, H.C.; Heidbuchel, H.; Hendriks, J.; et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur. J. Cardiothorac. Surg. 2016, 50, e1–e88. [Google Scholar] [CrossRef] [PubMed]
- Bakhai, A.; Darius, H.; De Caterina, R.; Smart, A.; Le Heuzey, J.Y.; Schilling, R.J.; Zamorano, J.L.; Shah, M.; Bramlage, P.; Kirchhof, P. Characteristics and outcomes of atrial fibrillation patients with or without specific symptoms: Results from the PREFER in AF registry. Eur. Heart J. Qual. Care Clin. Outcomes 2016, 2, 299–305. [Google Scholar] [CrossRef]
- Boriani, G.; Laroche, C.; Diemberger, I.; Fantecchi, E.; Popescu, M.I.; Rasmussen, L.H.; Sinagra, G.; Petrescu, L.; Tavazzi, L.; Maggioni, A.P.; et al. Asymptomatic Atrial Fibrillation: Clinical Correlates, Management, and Outcomes in the EORP-AF Pilot General Registry. Am. J. Med. 2015, 128, 509–518. [Google Scholar] [CrossRef]
- Lévy, S.; Maarek, M.; Coumel, P.; Guize, L.; Lekieffre, J.; Medvedowsky, J.L.; Sebaoun, A. Characterization of different subsets of atrial fibrillation in general practice in France: The ALFA study. The College of French Cardiologists. Circulation 1999, 99, 3028–3035. [Google Scholar] [CrossRef]
- Freeman, J.V.; Simon, D.N.; Go, A.S.; Spertus, J.; Fonarow, G.C.; Gersh, B.J.; Hylek, E.M.; Kowey, P.R.; Mahaffey, K.W.; Thomas, L.E.; et al. Association between Atrial Fibrillation Symptoms, Quality of Life, and Patient Outcomes: Results from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF). Circ. Cardiovasc. Qual. Outcomes 2015, 8, 393–402. [Google Scholar] [CrossRef]
- Rienstra, M.; Vermond, R.A.; Crijns, H.J.G.M.; Tijssen, J.G.P.; Van Gelder, I.C. Asymptomatic persistent atrial fibrillation and outcome: Results of the RACE study. Heart Rhythm 2014, 11, 939–945. [Google Scholar] [CrossRef]
- Siontis, K.C.; Gersh, B.J.; Killian, J.M.; Noseworthy, P.A.; McCabe, P.; Weston, S.A.; Roger, V.L.; Chamberlain, A.M. Typical, atypical, and asymptomatic presentations of new-onset atrial fibrillation in the community: Characteristics and prognostic implications. Heart Rhythm 2016, 13, 1418–1424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flaker, G.C.; Belew, K.; Beckman, K.; Vidaillet, H.; Kron, J.; Safford, R.; Mickel, M.; Barrell, P.; AFFIRM Investigators. Asymptomatic atrial fibrillation: Demographic features and prognostic information from the Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) study. Am. Heart J. 2005, 149, 657–663. [Google Scholar] [CrossRef] [PubMed]
- Friberg, L.; Engdahl, J.; Frykman, V.; Svennberg, E.; Levin, L.Å.; Rosenqvist, M. Population screening of 75- and 76-year-old men and women for silent atrial fibrillation (STROKESTOP). Europace 2013, 15, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Fitzmaurice, D.A.; Hobbs, F.D.R.; Jowett, S.; Mant, J.; Murray, E.T.; Holder, R.; Raftery, J.P.; Bryan, S.; Davies, M.; Lip, G.Y.; et al. Screening versus routine practice in detection of atrial fibrillation in patients aged 65 or over: Cluster randomised controlled trial. Br. Med. J. 2007, 335, 383–386. [Google Scholar] [CrossRef] [PubMed]
- Jaakkola, J.; Virtanen, R.; Vasankari, T.; Salminen, M.; Airaksinen, K.E.J. Self-detection of atrial fibrillation in an aged population: Three-year follow-up of the LietoAF intervention study. BMC Geriatr. 2017, 17, 218. [Google Scholar] [CrossRef] [PubMed]
- Halcox, J.P.J.; Wareham, K.; Cardew, A.; Gilmore, M.; Barry, J.P.; Phillips, C.; Gravenor, M.B. Assessment of Remote Heart Rhythm Sampling Using the AliveCor Heart Monitor to Screen for Atrial Fibrillation. Circulation 2017, 136, 1784–1794. [Google Scholar] [CrossRef] [PubMed]
- Lopes, R.D.; Alings, M.; Connolly, S.J.; Beresh, H.; Granger, C.B.; Mazuecos, J.B.; Boriani, G.; Nielsen, J.C.; Conen, D.; Hohnloser, S.H.; et al. Rationale and design of the Apixaban for the Reduction of Thrombo-Embolism in Patients With Device-Detected Sub-Clinical Atrial Fibrillation (ARTESiA) trial. Am. Heart J. 2017, 189, 137–145. [Google Scholar] [CrossRef]
- Healey, J.S.; Connolly, S.J.; Gold, M.R.; Israel, C.W.; Van Gelder, I.C.; Capucci, A.; Lau, C.P.; Fain, E.; Yang, S.; Bailleul, C.; et al. Subclinical Atrial Fibrillation and the Risk of Stroke. N. Engl. J. Med. 2012, 366, 120–129. [Google Scholar] [CrossRef] [Green Version]
- Glotzer, T.V.; Hellkamp, A.S.; Zimmerman, J.; Sweeney, M.O.; Yee, R.; Marinchak, R.; Cook, J.; Paraschos, A.; Love, J.; Radoslovich, G.; et al. Atrial High Rate Episodes Detected by Pacemaker Diagnostics Predict Death and Stroke. Circulation 2003, 107, 1614–1619. [Google Scholar] [CrossRef]
- Glotzer, T.V.; Daoud, E.G.; Wyse, D.G.; Singer, D.E.; Holbrook, R.; Pruett, K.; Smith, K.; Hilker, C.E. Rationale and design of a prospective study of the clinical significance of atrial arrhythmias detected by implanted device diagnostics: The TRENDS study. J. Interv. Card. Electrophysiol. 2006, 15, 9–14. [Google Scholar] [CrossRef]
- Hohnloser, S.H.; Capucci, A.; Fain, E.; Gold, M.R.; van Gelder, I.C.; Healey, J.; Israel, C.W.; Lau, C.P.; Morillo, C.; Connolly, S.J.; et al. ASymptomatic atrial fibrillation and Stroke Evaluation in pacemaker patients and the atrial fibrillation Reduction atrial pacing Trial (ASSERT). Am. Heart J. 2006, 152, 442–447. [Google Scholar] [CrossRef]
- Ip, J.; Waldo, A.L.; Lip, G.Y.H.; Rothwell, P.M.; Martin, D.T.; Bersohn, M.M.; Choucair, W.K.; Akar, J.G.; Wathen, M.S.; Rohani, P.; et al. Multicenter randomized study of anticoagulation guided by remote rhythm monitoring in patients with implantable cardioverter-defibrillator and CRT-D devices: Rationale, design, and clinical characteristics of the initially enrolled cohort. The IMPACT study. Am. Heart J. 2009, 158, 364–370. [Google Scholar] [CrossRef]
- Kirchhof, P.; Blank, B.F.; Calvert, M.; Camm, A.J.; Chlouverakis, G.; Diener, H.-C.; Goette, A.; Huening, A.; Lip, G.Y.H.; Simantirakis, E.; et al. Probing oral anticoagulation in patients with atrial high rate episodes: Rationale and design of the Non–vitamin K antagonist Oral anticoagulants in patients with Atrial High rate episodes (NOAH–AFNET 6) trial. Am. Heart J. 2017, 190, 12–18. [Google Scholar] [CrossRef]
- Kim, D.; Yang, P.-S.; Yu, H.T.; Kim, T.-H.; Jang, E.; Sung, J.-H.; Pak, H.N.; Lee, M.Y.; Lee, M.H.; Lip, G.Y.H.; et al. Risk of dementia in stroke-free patients diagnosed with atrial fibrillation: Data from a population-based cohort. Eur. Heart J. 2019, 40, 2313–2323. [Google Scholar] [CrossRef]
- Chen, L.Y.; Lopez, F.L.; Gottesman, R.F.; Huxley, R.R.; Agarwal, S.K.; Loehr, L.; Mosley, T.; Alonso, A. Atrial Fibrillation and Cognitive Decline–The Role of Subclinical Cerebral Infarcts. Stroke 2014, 45, 2568–2574. [Google Scholar] [CrossRef]
- Gaita, F.; Corsinovi, L.; Anselmino, M.; Raimondo, C.; Pianelli, M.; Toso, E.; Bergamasco, L.; Boffano, C.; Valentini, M.C.; Cesarani, F.; et al. Prevalence of silent cerebral ischemia in paroxysmal and persistent atrial fibrillation and correlation with cognitive function. J. Am. Coll. Cardiol. 2013, 62, 1990–1997. [Google Scholar] [CrossRef]
- Scarsoglio, S.; Saglietto, A.; Anselmino, M.; Gaita, F.; Ridolfi, L. Alteration of cerebrovascular haemodynamic patterns due to atrial fibrillation: An in silico investigation. J. R. Soc. Interface 2017, 14, 20170180. [Google Scholar] [CrossRef]
- Anselmino, M.; Scarsoglio, S.; Saglietto, A.; Gaita, F.; Ridolfi, L. Transient cerebral hypoperfusion and hypertensive events during atrial fibrillation: A plausible mechanism for cognitive impairment. Sci. Rep. 2016, 6, 28635. [Google Scholar] [CrossRef]
- Watson, T.; Shantsila, E.; Lip, G.Y. Mechanisms of thrombogenesis in atrial fibrillation: Virchow’s triad revisited. Lancet 2009, 373, 155–166. [Google Scholar] [CrossRef]
- Brambatti, M.; Connolly, S.J.; Gold, M.R.; Morillo, C.A.; Capucci, A.; Muto, C.; Lau, C.P.; Van Gelder, I.C.; Hohnloser, S.H.; Carlson, M.; et al. Temporal Relationship Between Subclinical Atrial Fibrillation and Embolic Events. Circulation 2014, 129, 2094–2099. [Google Scholar] [CrossRef] [Green Version]
- Daoud, E.G.; Glotzer, T.V.; Wyse, D.G.; Ezekowitz, M.D.; Hilker, C.; Koehler, J.; Ziegler, P.D.; TRENDS Investigators. Temporal relationship of atrial tachyarrhythmias, cerebrovascular events, and systemic emboli based on stored device data: A subgroup analysis of TRENDS. Heart Rhythm 2011, 8, 1416–1423. [Google Scholar] [CrossRef]
- Ausma, J.; Wijffels, M.; Thoné, F.; Wouters, L.; Allessie, M.; Borgers, M. Structural changes of atrial myocardium due to sustained atrial fibrillation in the goat. Circulation 1997, 96, 3157–3163. [Google Scholar] [CrossRef]
- Marrouche, N.F.; Wilber, D.; Hindricks, G.; Jais, P.; Akoum, N.; Marchlinski, F.; Kholmovski, E.; Burgon, N.; Hu, N.; Mont, L.; et al. Association of Atrial Tissue Fibrosis Identified by Delayed Enhancement MRI and Atrial Fibrillation Catheter Ablation. JAMA 2014, 311, 498. [Google Scholar] [CrossRef]
- Rolf, S.; Kircher, S.; Arya, A.; Eitel, C.; Sommer, P.; Richter, S.; Gaspar, T.; Bollmann, A.; Altmann, D.; Piedra, C.; et al. Tailored Atrial Substrate Modification Based on Low-Voltage Areas in Catheter Ablation of Atrial Fibrillation. Circ. Arrhythmia Electrophysiol. 2014, 7, 825–833. [Google Scholar] [CrossRef] [Green Version]
- Verma, A.; Wazni, O.M.; Marrouche, N.F.; Martin, D.O.; Kilicaslan, F.; Minor, S.; Schweikert, R.A.; Saliba, W.; Cummings, J.; Burkhardt, J.D.; et al. Pre-existent left atrial scarring in patients undergoing pulmonary vein antrum isolation. J. Am. Coll. Cardiol. 2005, 45, 285–292. [Google Scholar] [CrossRef]
- Kottkamp, H. Human atrial fibrillation substrate: Towards a specific fibrotic atrial cardiomyopathy. Eur. Heart J. 2013, 34, 2731–2738. [Google Scholar] [CrossRef]
- Kottkamp, H. Fibrotic Atrial Cardiomyopathy: A Specific Disease/Syndrome Supplying Substrates for Atrial Fibrillation, Atrial Tachycardia, Sinus Node Disease, AV Node Disease, and Thromboembolic Complications. J. Cardiovasc. Electrophysiol. 2012, 23, 797–799. [Google Scholar] [CrossRef]
- Pollak, W.M.; Simmons, J.D.; Interian, A.; Atapattu, S.A.; Castellanos, A.; Myerburg, R.J.; Mitrani, R.D. Clinical utility of intraatrial pacemaker stored electrograms to diagnose atrial fibrillation and flutter. Pacing Clin. Electrophysiol. 2001, 24, 424–429. [Google Scholar] [CrossRef]
- Glotzer, T.V.; Daoud, E.G.; Wyse, D.G.; Singer, D.E.; Ezekowitz, M.D.; Hilker, C.; Miller, C.; Qi, D.; Ziegler, P.D. The Relationship Between Daily Atrial Tachyarrhythmia Burden from Implantable Device Diagnostics and Stroke Risk. Circ. Arrhythmia Electrophysiol. 2009, 2, 474–480. [Google Scholar] [CrossRef]
- Kennedy, H.L. Silent Atrial Fibrillation: Definition, Clarification, and Unanswered Issues. Ann. Noninvasive Electrocardiol. 2015, 20, 518–525. [Google Scholar] [CrossRef]
- Abed, H.S.; Wittert, G.A.; Leong, D.P.; Shirazi, M.G.; Bahrami, B.; Middeldorp, M.E.; Lorimer, M.F.; Lau, D.H.; Antic, N.A.; Brooks, A.G.; et al. Effect of weight reduction and cardiometabolic risk factor management on symptom burden and severity in patients with atrial fibrillation: A randomized clinical trial. JAMA J. Am. Med. Assoc. 2013, 310, 2050–2060. [Google Scholar] [CrossRef]
- Malmo, V.; Nes, B.M.; Amundsen, B.H.; Tjonna, A.E.; Stoylen, A.; Rossvoll, O.; Wisloff, U.; Loennechen, J.P. Aerobic interval training reduces the burden of Atrial fibrillation in the short term: A randomized trial. Circulation 2016, 133, 466–473. [Google Scholar] [CrossRef]
- Chen, L.Y.; Chung, M.K.; Allen, L.A.; Ezekowitz, M.; Furie, K.L.; McCabe, P.; Noseworthy, P.A.; Perez, M.V.; Turakhia, M.P.; American Heart Association Council on Clinical Cardiology; et al. Atrial Fibrillation Burden: Moving Beyond Atrial Fibrillation as a Binary Entity: A Scientific Statement From the American Heart Association. Circulation 2018, 137, e623–e644. [Google Scholar] [CrossRef]
- January, C.T.; Wann, L.S.; Calkins, H.; Chen, L.Y.; Cigarroa, J.E.; Cleveland, J.C.; Ellinor, P.T.; Ezekowitz, M.D.; Field, M.E.; Furie, K.L.; et al. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart, R. Circulation 2019, 140, 125–151. [Google Scholar] [CrossRef]
- Al-Khatib, S.M.; Thomas, L.; Wallentin, L.; Lopes, R.D.; Gersh, B.; Garcia, D.; Ezekowitz, J.; Alings, M.; Yang, H.; Alexander, J.H. Outcomes of apixaban vs. warfarin by type and duration of atrial fibrillation: Results from the ARISTOTLE trial. Eur. Heart J. 2013, 34, 2464–2471. [Google Scholar] [CrossRef]
- Link, M.S.; Giugliano, R.P.; Ruff, C.T.; Scirica, B.M.; Huikuri, H.; Oto, A.; Crompton, A.E.; Murphy, S.A.; Lanz, H.; Mercuri, M.F. Stroke and Mortality Risk in Patients with Various Patterns of Atrial Fibrillation: Results from the ENGAGE AF-TIMI 48 Trial (Effective Anticoagulation with Factor Xa Next Generation in Atrial Fibrillation-Thrombolysis in Myocardial Infarction 48). Circ. Arrhythmia Electrophysiol. 2017, 10, 1–7. [Google Scholar] [CrossRef]
- Steinberg, B.A.; Hellkamp, A.S.; Lokhnygina, Y.; Patel, M.R.; Breithardt, G.; Hankey, G.J.; Becker, R.C.; Singer, D.E.; Halperin, J.L.; Hacke, W.; et al. Higher risk of death and stroke in patients with persistent vs. paroxysmal atrial fibrillation: Results from the ROCKET-AF Trial. Eur. Heart J. 2015, 36, 288–296. [Google Scholar] [CrossRef]
- Sposato, L.A.; Cipriano, L.E.; Saposnik, G.; Vargas, E.R.; Riccio, P.M.; Hachinski, V. Diagnosis of atrial fibrillation after stroke and transient ischaemic attack: A systematic review and meta-analysis. Lancet Neurol. 2015, 14, 377–387. [Google Scholar] [CrossRef]
- Kishore, A.; Vail, A.; Majid, A.; Dawson, J.; Lees, K.R.; Tyrrell, P.J.; Smith, C.J. Detection of Atrial Fibrillation After Ischemic Stroke or Transient Ischemic Attack. Stroke 2014, 45, 520–526. [Google Scholar] [CrossRef] [Green Version]
- January, C.T.; Wann, L.S.; Alpert, J.S.; Calkins, H.; Cigarroa, J.E.; Cleveland, J.C.; Conti, J.B.; Ellinor, P.T.; Ezekowitz, M.D.; Field, M.E.; et al. 2014 AHA/ACC/HRS Guideline for the Management of Patients with Atrial Fibrillation. Circulation 2014, 130, 1–2. [Google Scholar] [CrossRef]
- Jonas, D.E.; Kahwati, L.C.; Yun, J.D.Y.; Middleton, J.C.; Coker-Schwimmer, M.; Asher, G.N. Screening for Atrial Fibrillation with Electrocardiography. JAMA 2018, 320, 485. [Google Scholar] [CrossRef]
- Curry, S.J.; Krist, A.H.; Owens, D.K.; Barry, M.J.; Caughey, A.B.; Davidson, K.W.; Doubeni, C.A.; Epling, J.W., Jr.; Kemper, A.R.; Kubik, M.; et al. Screening for Atrial Fibrillation with Electrocardiography. JAMA 2018, 320, 478. [Google Scholar] [CrossRef]
- Svennberg, E.; Engdahl, J.; Al-Khalili, F.; Friberg, L.; Frykman, V.; Rosenqvist, M. Mass Screening for Untreated Atrial Fibrillation. Circulation 2015, 131, 2176–2184. [Google Scholar] [CrossRef] [Green Version]
- Aronsson, M.; Svennberg, E.; Rosenqvist, M.; Engdahl, J.; Al-Khalili, F.; Friberg, L.; Frykman-Kull, V.; Levin, L.Å. Cost-effectiveness of mass screening for untreated atrial fibrillation using intermittent ECG recording. Europace 2015, 17, 1023–1029. [Google Scholar] [CrossRef]
- Sinha, A.-M.; Diener, H.-C.; Morillo, C.A.; Sanna, T.; Bernstein, R.A.; Di Lazzaro, V.; Passman, R.; Beckers, F.; Brachmann, J. Cryptogenic Stroke and underlying Atrial Fibrillation (CRYSTAL AF): Design and rationale. Am. Heart J. 2010, 160, 36–41. [Google Scholar] [CrossRef]
- Sanna, T.; Diener, H.-C.; Passman, R.S.; Di Lazzaro, V.; Bernstein, R.A.; Morillo, C.A.; Rymer, M.M.; Thijs, V.; Rogers, T.; Beckers, F.; et al. Cryptogenic Stroke and Underlying Atrial Fibrillation. N. Engl. J. Med. 2014, 370, 2478–2486. [Google Scholar] [CrossRef] [Green Version]
- Gladstone, D.J.; Spring, M.; Dorian, P.; Panzov, V.; Thorpe, K.E.; Hall, J.; Vaid, H.; O‘Donnell, M.; Laupacis, A.; Côté, R.; et al. Atrial Fibrillation in Patients with Cryptogenic Stroke. N. Engl. J. Med. 2014, 370, 2467–2477. [Google Scholar] [CrossRef] [Green Version]
- Conen, D.; Rodondi, N.; Müller, A.; Beer, J.H.; Ammann, P.; Moschovitis, G.; Auricchio, A.; Hayoz, D.; Kobza, R.; Shah, D.; et al. Relationships of Overt and Silent Brain Lesions with Cognitive Function in Patients With Atrial Fibrillation. J. Am. Coll. Cardiol. 2019, 73, 989–999. [Google Scholar] [CrossRef]
- Mark, D.B.; Anstrom, K.J.; Sheng, S.; Piccini, J.P.; Baloch, K.N.; Monahan, K.H.; Monahan, K.H.; Daniels, M.R.; Bahnson, T.D.; Poole, J.E.; et al. Effect of Catheter Ablation vs Medical Therapy on Quality of Life Among Patients With Atrial Fibrillation. JAMA 2019, 321, 1275. [Google Scholar] [CrossRef]
- Wokhlu, A.; Monahan, K.H.; Hodge, D.O.; Asirvatham, S.J.; Friedman, P.A.; Munger, T.M.; Bradley, D.J.; Bluhm, C.M.; Haroldson, J.M.; Packer, D.L. Long-Term Quality of Life After Ablation of Atrial Fibrillation. J. Am. Coll. Cardiol. 2010, 55, 2308–2316. [Google Scholar] [CrossRef]
- Marrouche, N.F.; Brachmann, J.; Andresen, D.; Siebels, J.; Boersma, L.; Jordaens, L.; Merkely, B.; Pokushalov, E.; Sanders, P.; Proff, J.; et al. Catheter Ablation for Atrial Fibrillation with Heart Failure. N. Engl. J. Med. 2018, 378, 417–427. [Google Scholar] [CrossRef]
- Dagres, N.; Chao, T.-F.; Fenelon, G.; Aguinaga, L.; Benhayon, D.; Benjamin, E.J.; Bunch, T.J.; Chen, L.Y.; Chen, S.A.; Darrieux, F.; et al. European Heart Rhythm Association (EHRA)/Heart Rhythm Society (HRS)/Asia Pacific Heart Rhythm Society (APHRS)/Latin American Heart Rhythm Society (LAHRS) expert consensus on arrhythmias and cognitive function: What is the best practice? Europace 2018, 20, 1399–1421. [Google Scholar] [CrossRef]
- Herm, J.; Fiebach, J.B.; Koch, L.; Kopp, U.A.; Kunze, C.; Wollboldt, C.; Brunecker, P.; Schultheiss, H.P.; Schirdewan, A.; Endres, M.; et al. Neuropsychological effects of MRI-detected brain lesions after left atrial catheter ablation for atrial fibrillation: Long-term results of the MACPAF study. Circ. Arrhythmia Electrophysiol. 2013, 6, 843–850. [Google Scholar] [CrossRef]
- Medi, C.; Evered, L.; Silbert, B.; Teh, A.; Halloran, K.; Morton, J.; Kistler, P.; Kalman, J. Subtle post-procedural cognitive dysfunction after atrial fibrillation ablation. J. Am. Coll. Cardiol. 2013, 62, 531–539. [Google Scholar] [CrossRef]
- Allan, V.; Banerjee, A.; Shah, A.D.; Patel, R.; Denaxas, S.; Casas, J.-P.; Hemingway, H. Net clinical benefit of warfarin in individuals with atrial fibrillation across stroke risk and across primary and secondary care. Heart 2017, 103, 210–218. [Google Scholar] [CrossRef]
- Friberg, L.; Rosenqvist, M.; Lip, G.Y.H. Net clinical benefit of warfarin in patients with atrial fibrillation: A report from the swedish atrial fibrillation cohort study. Circulation 2012, 125, 2298–2307. [Google Scholar] [CrossRef]
- Ruff, C.T.; Giugliano, R.P.; Braunwald, E.; Hoffman, E.B.; Deenadayalu, N.; Ezekowitz, M.D.; Camm, A.J.; Weitz, J.I.; Lewis, B.S.; Parkhomenko, A.; et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: A meta-analysis of randomised trials. Lancet 2014, 383, 955–962. [Google Scholar] [CrossRef]
- Martin, D.T.; Bersohn, M.M.; Lwaldo, A.; Wathen, M.S.; Choucair, W.K.; Lip, G.Y.; Ip, J.; Holcomb, R.; Akar, J.G.; Halperin, J.L.; et al. Randomized trial of atrial arrhythmia monitoring to guide anticoagulation in patients with implanted defibrillator and cardiac resynchronization devices. Eur. Heart J. 2015, 36, 1660–1668. [Google Scholar] [CrossRef] [Green Version]
- Greene, H.L. Baseline characteristics of patients with atrial fibrillation: The AFFIRM study. Am. Heart J. 2002, 143, 991–1001. [Google Scholar] [CrossRef]
- Investigators TAFFI of RM (AFFIRM). A Comparison of Rate Control and Rhythm Control in Patients with Atrial Fibrillation. N. Engl. J. Med. 2002, 347, 1825–1833. [Google Scholar] [CrossRef]
- Van Gelder, I.C.; Hagens, V.E.; Bosker, H.A.; Kingma, J.H.; Kamp, O.; Kingma, T.; Said, S.A.; Darmanata, J.I.; Timmermans, A.J.; Tijssen, J.G.; et al. A Comparison of Rate Control and Rhythm Control in Patients with Recurrent Persistent Atrial Fibrillation. N. Engl. J. Med. 2002, 347, 1834–1840. [Google Scholar] [CrossRef]
- Epstein, A.E. Relationships Between Sinus Rhythm, Treatment, and Survival in the Atrial Fibrillation Follow-Up Investigation of Rhythm Management (AFFIRM) Study. Circulation 2004, 109, 1509–1513. [Google Scholar] [CrossRef]
- Tsadok, M.A.; Jackevicius, C.A.; Essebag, V.; Eisenberg, M.J.; Rahme, E.; Humphries, K.H.; Tu, J.V.; Behlouli, H.; Pilote, L. Rhythm Versus Rate Control Therapy and Subsequent Stroke or Transient Ischemic Attack in Patients with Atrial Fibrillation. Circulation 2012, 126, 2680–2687. [Google Scholar] [CrossRef]
- Khan, A.R.; Khan, S.; Sheikh, M.A.; Khuder, S.; Grubb, B.; Moukarbel, G.V. Catheter ablation and antiarrhythmic drug therapy as first- or second-line therapy in the management of atrial fibrillation: Systematic review and meta-analysis. Circ. Arrhythmia Electrophysiol. 2014, 7, 853–860. [Google Scholar] [CrossRef]
- Packer, D.L.; Mark, D.B.; Robb, R.A.; Monahan, K.H.; Bahnson, T.D.; Poole, J.E.; Noseworthy, P.A.; Rosenberg, Y.D.; Jeffries, N.; Mitchell, L.B.; et al. Effect of Catheter Ablation vs Antiarrhythmic Drug Therapy on Mortality, Stroke, Bleeding, and Cardiac Arrest Among Patients with Atrial Fibrillation. JAMA 2019, 321, 1261–1274. [Google Scholar] [CrossRef]
- Bunch, T.J.; May, H.T.; Bair, T.L.; Weiss, J.P.; Crandall, B.G.; Osborn, J.S.; Mallender, C.; Anderson, J.L.; Muhlestein, B.J.; Lappe, D.L.; et al. Atrial fibrillation ablation patients have long-term stroke rates similar to patients without atrial fibrillation regardless of CHADS2 score. Heart Rhythm 2013, 10, 1272–1277. [Google Scholar] [CrossRef]
- Hunter, R.J.; McCready, J.; Diab, I.; Page, S.P.; Finlay, M.; Richmond, L.; French, A.; Earley, M.J.; Sporton, S.; Jones, M.; et al. Maintenance of sinus rhythm with an ablation strategy in patients with atrial fibrillation is associated with a lower risk of stroke and death. Heart 2012, 98, 48–53. [Google Scholar] [CrossRef]
- Karasoy, D.; Gislason, G.H.; Hansen, J.; Johannessen, A.; K’ber, L.; Hvidtfeldt, M.; Özcan, C.; Torp-Pedersen, C.; Hansen, M.L. Oral anticoagulation therapy after radiofrequency ablation of atrial fibrillation and the risk of thromboembolism and serious bleeding: Long-term follow-up in nationwide cohort of Denmark. Eur. Heart J. 2015, 36, 307–314. [Google Scholar] [CrossRef]
- Gallo, C.; Battaglia, A.; Anselmino, M.; Bianchi, F.; Grossi, S.; Nangeroni, G.; Toso, E.; Gaido, L.; Scaglione, M.; Ferraris, F.; et al. Long-term events following atrial fibrillation rate control or transcatheter ablation. J. Cardiovasc. Med. 2016, 17, 187–193. [Google Scholar] [CrossRef]
- Kirchhof, P.; Breithardt, G.; Camm, A.J.; Crijns, H.J.; Kuck, K.-H.; Vardas, P.; Wegscheider, K. Improving outcomes in patients with atrial fibrillation: Rationale and design of the Early treatment of Atrial fibrillation for Stroke prevention Trial. Am. Heart J. 2013, 166, 442–448. [Google Scholar] [CrossRef]
- Verma, A.; Ha, A.C.T.; Kirchhof, P.; Hindricks, G.; Healey, J.S.; Hill, M.D.; Sharma, M.; Wyse, D.G.; Champagne, J.; Essebag, V.; et al. The Optimal Anti-Coagulation for Enhanced-Risk Patients Post–Catheter Ablation for Atrial Fibrillation (OCEAN) trial. Am. Heart J. 2018, 197, 124–132. [Google Scholar] [CrossRef]
- Kalman, J.M.; Sanders, P.; Rosso, R.; Calkins, H. Should We Perform Catheter Ablation for Asymptomatic Atrial Fibrillation? Circulation 2017, 136, 490–499. [Google Scholar] [CrossRef]
| Authors (Study Year) | AHRE/Subclinical/Asymptomatic AF Diagnostic Method | Terminology Used in the Study | Terminology Used in This Review |
|---|---|---|---|
| Implanted device monitoring | |||
| Glotzer et al. (2003) [19] | AHRE: atrial rate ≥ 220 bpm lasting at least 5 min (detected by pacemaker) | AHRE | AHRE |
| Glotzer et al. (2006) [20] | AHRE: atrial rate > 175 bpm lasting at least 20 s | Device-detected atrial tachycardia (AT)/AF burden (AHRE) | |
| Hohnloser et al. (2006) [21] | AHRE: atrial rate ≥ 190 bpm lasting at least 6 min (detected by pacemaker or ICD) | Asymptomatic AF/AHRE | |
| Ip et al. (2009) [22] | AHRE: atrial rate ≥ 220 beat/min lasting at least 5 min, | AHRE | |
| Kirchhof et al. (2017) [23] | AHRE: atrial rate ≥ 180 bpm lasting at least 6 min | AHRE | |
| Lopes et al. (2017) [17] | One episode of device-detected subclinical AF lasting at least 6 min. Subclinical AF requires at least one episode of electrogram confirmation | Subclinical AF | Subclinical AF |
| Non-Invasive ECG monitoring | |||
| Flaker et al. (2005) [12] | AF diagnosed with ECG or rhythm strip. Symptoms evaluated by a questionnaire | Asymptomatic AF | Asymptomatic AF |
| Rienstra et al. (2014) [10] | Recurrent persistent AF without symptoms according to a questionnaire | Asymptomatic AF/Silent AF | |
| Boriani et al. (2015) [7] | ECG diagnosed AF and EHRA score I | Asymptomatic AF/Silent AF | |
| Freeman et al. (2015) [9] | Electrocardiographically documented AF and EHRA score I | Asymptomatic AF | |
| Bakhai et al. (2016) [6] | ECG diagnosed AF and EHRA score I | Asymptomatic AF/Silent AF | |
| Siontis et al. (2016) [11] | AF detected incidentally (routine physical examination, preoperative evaluation, emergency department or clinic visit for unrelated problem) | Asymptomatic AF | Subclinical AF |
| Jaakkola et al. (2017) [15] | ECG diagnosis in a screening program | AF | |
| Halcox et al. (2017) [16] | Device detected AF in a screening program | AF | |
| Friberg et al. (2013) [13] | Device detected AF in a screening program and confirmed by Holter for uncertain cases | Silent AF | |
| Authors (Study Year) | AHRE/Subclinical/Asymptomatic AF Diagnostic Method | Stroke and TE Incidence (%) * | Mortality (%) * | Correlation with Stroke or Mortality |
|---|---|---|---|---|
| Implanted device monitoring | ||||
| Glotzer et al. (2003) [19] | AHRE: atrial rate ≥ 220 bpm lasting at least 5 min (detected by pacemaker) | AHRE: 33/160 (20.6) No AHRE: 16/152 (10.5) | AHRE: 28/160 (17.5) No AHRE: 16/152 (10.5) | Yes (for total mortality, stroke, and AF development) |
| Glotzer et al. (2009) [39] | AHRE: atrial rate > 175 bpm lasting at least 20 s. Patients were stratified according to 30 days window monitoring in: zero, low, and high AHRE burden | Annualized TE incidence rate: zero AHRE burden 1.1%; Low AHRE burden 1.1%; High AHRE burden 2.4% | NA | No |
| Healey et al. (2012) [18] | AHRE: atrial rate ≥ 190 bpm lasting at least 6 min (detected by pacemaker or ICD) | AHRE in the previous 3 months: 11/261 (4.2) No AHRE in the previous 3 months: 40/2319 (1.7) | From vascular causes AHRE in the previous 3 months: 19/261 (7.3) No AHRE in the previous 3 months: 153/2319 (6.6) | Yes |
| Non-Invasive ECG monitoring | ||||
| Flaker et al. (2005) [12] | AF diagnosed with ECG or rhythm strip. Symptoms evaluated by a questionnaire | Asymptomatic AF: 21 Symptomatic AF: 136 | Asymptomatic AF: 60 (19) Symptomatic AF: 606 (27) | No (in comparison with symptomatic patients) |
| Rienstra et al. (2014) [10] | Recurrent persistent AF without symptoms according to a questionnaire | Asymptomatic AF: 8/157 Symptomatic AF: 28/365 | Asymptomatic AF: 9/157 Symptomatic AF: 26/365 (death from cardiovascular causes) | No † |
| Boriani et al. (2015) [7] | ECG diagnosed AF and EHRA score I | EHRA I: 10/962 (1.0%) EHRA II–IV: 15/1344 (1.1%) | EHRA I: 102/1086 (9.4%) EHRA II–IV: 65/1556 (4.2%) | Yes (for mortality compared to symptomatic patients) |
| Freeman et al. (2015) [9] | Electrocardiographically documented AF and EHRA score I | EHRA I: 99/3682 EHRA II–IV: 168/5918 | EHRA I: 311/3682 EHRA II–IV: 561/5918 | No ‡ |
| Bakhai et al. (2016) [6] | ECG diagnosed AF and EHRA score I | EHRA I: ischemic stroke 8/489 (1.6) TIA 7/488 (1.4) arterial embolism 2/488 (0.4) EHRA II–IV: ischemic stroke 44/5514 (0.8) TIA 73/5510 (1.3) arterial embolism 11/5514 (0.2) | NA | No (only EHRA score IV was associated with a higher events occurrence) |
| Siontis et al. (2016) [11] | AF detected incidentally (routine physical examination, preoperative evaluation, emergency department, or clinic visit for unrelated problem) | HR compared to typical AF: Subclinical AF 2.60 (95% C.I. 1.10–6.11) Atypical AF 3.12 (95% C.I. 1.27–7.66) | HR compared to typical AF: Subclinical AF 4.01 (95% C.I. 2.32–6.91) Atypical AF 3.19 (95% C.I. 1.78–5.71) | Yes (compared to typical AF) |
| Name of Study | Number of Patients | Study Arms | Primary Endpoints | Secondary Endpoints |
|---|---|---|---|---|
| STROKESTOP (NCT01593553) | 7173 (in screening) 14,381 (controls not screened) | Intervention group: ECG screening for AF using intermittent ECG recorder. Control group: standard of care | Composite of ischemic and hemorrhagic stroke, systemic embolism, major bleeding requiring hospitalization, and all-cause mortality | Each single component of the composite primary outcome; dementia; cardiovascular mortality; hospitalization due to cardiovascular disease; cost-effectiveness; OAC initiation and compliance; AF detection; pulmonary embolism and deep vein thrombosis |
| NOAH-AFNET 6 (NCT02618577) | 2686 (3400 estimated) patients (≥65 years old and ≥1 additional CHA2DS2-VASc factor) with AHRE documented by implanted devices | Intervention group: Edoxaban (standard AF dosing) Control group: ASA or placebo | Composite of stroke, systemic embolism and cardiovascular death (measured as time from randomization to event occurrence) | MACE (cardiac death, MI, acute coronary syndrome), all-cause death, major bleeding events, quality of life changes at 12 and 24 months, patient satisfaction at 12 and 24 months, cost effectiveness and health resource utilization, autonomy status changes in patients affected by stroke during study participation, cognitive function at 12 and 24 months |
| ARTESiA (NCT01938248) | ≈4000 patients with subclinical AF at high risk for stroke (estimated) | Intervention group: Apixaban (standard AF dosing) Control group: ASA (81 mg/die) | Efficacy outcome: composite of stroke (including TIA) and systemic embolism. Safety outcome: major bleeding | Ischemic stroke; MI; vascular death; total death; composite of stroke, MI, systemic embolism and total death; composite of stroke, MI, systemic embolism, total death, and major bleeding. |
| EAST (NCT01288352) | 2789 patients with new AF (<1 year) and risk factors for stroke | Intervention group: guidelines-based therapy andearly rhythm control therapy (AAD or PVI) Control group: usual care | First coprimary outcome: composite of cardiovascular death, stroke (including TIA), acute coronary syndrome, and worsening of heart failure. Second coprimary outcome: nights in hospital per year | Cardiovascular death, stroke, worsening of heart failure, acute coronary syndrome, time to recurrent AF, cardiovascular hospitalizations, all-cause hospitalizations, left ventricular function, quality of life, cognitive function |
| OCEAN (NCT02168829) | 1572 patients free from AF for at least 1 year after catheter ablation for non-valvular AF (estimated) | Active Comparator: rivaroxaban 15 mg/die Active Comparator: ASA 75–160 mg/die | Composite of clinically overt stroke, systemic embolism, and covert stroke detected by brain MRI | Each single component of the composite primary outcome; major bleeding, clinically relevant non-major bleeding, minor bleeding and their composite; overt intracranial hemorrhage; microbleedings as detected by MRI; TIA; all-cause mortality; net clinical benefit; occurrence of nonprimary end point MRI changes; correlation of AF burden/recurrence to occurrence of clinical or covert stroke; neuropsychological testing; quality of life |
| OAT (NCT01959425) | 100 patients free from AF for at least 3 months after catheter ablation and at high risk for stroke (estimated) | Intervention group: OAC discontinuation Control group: OAC continuation | Composite of any major thromboembolic event and major hemorrhagic complication | Bleeding; hospitalization; mortality; quality of Life; AF recurrence; repeat ablation |
| SWISS-AF (NCT02105844) | 2415 AF patients | NA | Stroke or systemic embolism | Hospitalization for heart failure |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ballatore, A.; Matta, M.; Saglietto, A.; Desalvo, P.; Bocchino, P.P.; Gaita, F.; De Ferrari, G.M.; Anselmino, M. Subclinical and Asymptomatic Atrial Fibrillation: Current Evidence and Unsolved Questions in Clinical Practice. Medicina 2019, 55, 497. https://doi.org/10.3390/medicina55080497
Ballatore A, Matta M, Saglietto A, Desalvo P, Bocchino PP, Gaita F, De Ferrari GM, Anselmino M. Subclinical and Asymptomatic Atrial Fibrillation: Current Evidence and Unsolved Questions in Clinical Practice. Medicina. 2019; 55(8):497. https://doi.org/10.3390/medicina55080497
Chicago/Turabian StyleBallatore, Andrea, Mario Matta, Andrea Saglietto, Paolo Desalvo, Pier Paolo Bocchino, Fiorenzo Gaita, Gaetano Maria De Ferrari, and Matteo Anselmino. 2019. "Subclinical and Asymptomatic Atrial Fibrillation: Current Evidence and Unsolved Questions in Clinical Practice" Medicina 55, no. 8: 497. https://doi.org/10.3390/medicina55080497





