Coverage and Determinants of Full Immunization: Vaccination Coverage among Senegalese Children
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Outcome Variable
2.3. Explanatory Variables
2.4. Statistical Analysis
3. Results
3.1. Characteristics of Study Participants
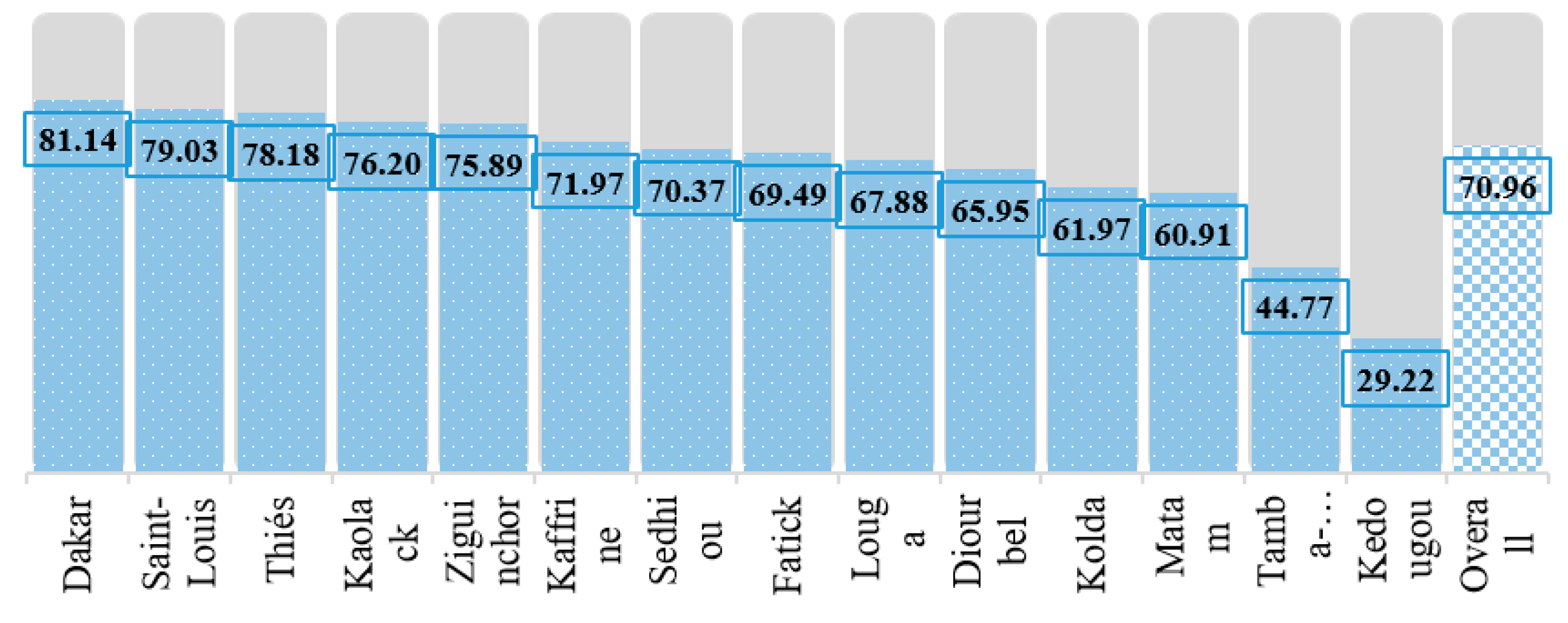
3.2. Vaccination Coverage Rate among Study Participants
3.3. Associated Factors for the Vaccination Coverage
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Protecting People from Vaccine Preventable Diseases: Strategic Plan (2010–2013); WHO: Geneva, Switzerland, 2013. [Google Scholar]
- Andre, F.E.; Booy, R.; Bock, H.L.; Clemens, J.; Datta, S.K.; John, T.J.; Lee, B.W.; Lolekha, S.; Peltola, H.; Ruff, T.A.; et al. Vaccination greatly reduces disease, disability, death and inequity worldwide. Bull. World Health Organ. 2008, 86, 140–146. [Google Scholar] [CrossRef] [PubMed]
- WHO; UNICEF; World Bank. State of the World’s Vaccine and Immunization, 3rd ed.; World Health Organization (WHO): Geneva, Switzerland, 2009. [Google Scholar]
- WHO. Ten Years in Public Health 2007–2017: Report by Dr. Margaret Chan, Director-General; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Jamil, K.; Bhuiya, A.; Streatfield, K.; Chakrabarty, N. The immunization programme in Bangladesh: Impressive gains in coverage, but gaps remain. Health Policy Plan. 1999, 14, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Keja, K.; Chan, C.; Hayden, G.; Henderson, R.H. Expanded programme on immunization. World Health Stat. Q. 1988, 41, 59–63. [Google Scholar] [PubMed]
- World Health Organization. Immunization Coverage: Key Facts; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- Mbengue, M.A.S.; Sarr, M.; Faye, A.; Badiane, O.; Camara, F.B.N.; Mboup, S.; Dieye, T.N. Determinants of complete immunization among senegalese children aged 12-23 months: Evidence from the demographic and health survey. BMC Public Health 2017, 17, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Mbengue, M.A.S.; Mboup, A.; Ly, I.D.; Faye, A.; Camara, F.B.N.; Thiam, M.; Ndiaye, B.P.; Dieye, T.N.; Mboup, S. Vaccination coverage and immunization timeliness among children aged 12-23 months in Senegal: A Kaplan-Meier and Cox regression analysis approach. Pan Afr. Med. J. 2017, 27, 8. [Google Scholar] [CrossRef] [PubMed]
- Seck, I.; Faye, A.; Leye, M.M.M.; Bathily, A.; Camara, M.D.; Ndiaye, P.; Dia, A.T. Measles epidemic and response in the region of Dakar (Senegal) in 2009. Sante Publique. (Paris) 2012, 24, 121–132. [Google Scholar] [CrossRef]
- Unicef. Monitoring the Situation of Children and Women; Country profile: Senegal; Unicef: New York, NY, USA, 2019. [Google Scholar]
- EPI. EPI Comprehensive Multi-Year Plan 2012-2016: Complete Multi-Year EPI Plan; Republic of Senegal; EPI: Washington, DC, USA, 2011. [Google Scholar]
- Dia, N.; Fall, A.; Ka, R.; Fall, A.; Kiori, D.E.; Goudiaby, D.G.; Fall, A.D.; Dosseh, A.; Ndiaye, K.; Diop, O.M.; et al. Epidemiology and genetic characterization of measles strains in Senegal, 2004-2013. PLoS ONE 2015, 10, 2004–2013. [Google Scholar] [CrossRef]
- Anderson, R.M. Revisiting the Behavioral Model and Access to Medical Care Does it Matter? J. Health Soc. Behav. 1995, 36, 1–10. [Google Scholar] [CrossRef]
- Bekondi, C.; Zanchi, R.; Seck, A.; Garin, B.; Giles-Vernick, T.; Gody, J.C.; Bata, P.; Pondy, A.; Tetang, S.M.; Ba, M.; et al. HBV immunization and vaccine coverage among hospitalized children in Cameroon, Central African Republic and Senegal: A cross-sectional study. BMC Infect. Dis. 2015, 15, 25–28. [Google Scholar] [CrossRef]
- Ndiaye, N.M.; Ndiaye, P.; Diédhiou, A.; Guèye, A.S.; Tal-Dia, A. Facteurs d’abandon de la vaccination des enfants âgés de 10 à 23 mois à Ndoulo (Sénégal). Cah. Santé 2009, 19, 9–13. [Google Scholar] [CrossRef]
- Rutstein, S.O.; Rojas, G. Guide to DHS Statistics: Demographic and Health Surveys Methodology; Agency for International Development: Calverton, MD, USA, 2006. [Google Scholar]
- Agence Nationale de la Statistique et de la Démographie (ANSD). Senegal Continuing Demographic and Health Survey 2017 (EDS-Continued); ANSD et ICF: Rockville, MD, USA, 2017. [Google Scholar]
- Herliana, P.; Douiri, A. Determinants of immunisation coverage of children aged 12-59 months in Indonesia: A cross-sectional study. BMJ Open 2017, 7, 1–14. [Google Scholar] [CrossRef]
- Ibnouf, A.H.; den Borne, H.W.V.; Maarse, J.A.M. Factors influencing immunisation coverage among children under five years of age in Khartoum State, Sudan. South Afr. Fam. Pract. 2007, 49, 14a–14f. [Google Scholar] [CrossRef]
- Titaley, C.R.; Dibley, M.J.; Roberts, C.L. Factors associated with underutilization of antenatal care services in Indonesia: Results of Indonesia Demographic and Health Survey 2002/2003 and 2007. BMC Public Health 2010, 10, 485. [Google Scholar] [CrossRef] [PubMed]
- Humanium. Realizing Children’s Rights in Senegal. Main Problem Faced by Child. 2019. Available online: https://www.humanium.org/en/senegal/ (accessed on 25 April 2019).
- World Health Organization (WHO). Immunization Coverage. Glob. 2017. Available online: https://www.who.int/news-room/fact-sheets/detail/immunization-coverage (accessed on 25 April 2019).
- Lo Vecchio, A.; Cambriglia, M.D.; Fedele, M.C.; Basile, F.W.; Chiatto, F.; del Giudice, VM.M.; Guarino, A. Determinants of low measles vaccination coverage in children living in an endemic area. Eur. J. Pediatr. 2019, 178, 243–251. [Google Scholar] [CrossRef] [PubMed]
- Tohme, R.A.; Francois, J.; Wannemuehler, K.; Iyengar, P.; Dismer, A.; Adrien, P.; Hyde, T.B.; Marston, B.J.; Date, K.; Mintz, E.; et al. Oral cholera vaccine coverage, barriers to vaccination, and adverse events following vaccination, Haiti, 2013. Emerg. Infect. Dis. 2015, 21, 984–991. [Google Scholar] [CrossRef] [PubMed]
- Clouston, S.; Kidman, R.; Palermo, T. Social inequalities in vaccination uptake among children aged 0–59 months living in Madagascar: An analysis of Demographic and Health Survey data from 2008 to 2009. Vaccine 2014, 32, 3533–3539. [Google Scholar] [CrossRef] [PubMed]
- Antai, D. Inequitable childhood immunization uptake in Nigeria: A multilevel analysis of individual and contextual determinants. BMC Infect. Dis. 2009, 9, 181. [Google Scholar] [CrossRef]
- Uddin, M.J.; Koehlmoos, T.P.; Saha, N.C.; Khan, I.A. Child immunization coverage in rural hard-to-reach areas of Bangladesh. Vaccine 2010, 28, 1221–1225. [Google Scholar] [CrossRef]
- Abadura, S.A.; Lerebo, W.T.; Kulkarni, U.; Mekonnen, Z.A. Individual and community level determinants of childhood full immunization in Ethiopia: A multilevel analysis Global health. BMC Public Health 2015, 15, 1–10. [Google Scholar] [CrossRef]
- Maharani, A.; Kuroda, Y. Determinants of immunization status among 12- to 23-month-old children in Indonesia (2008-2013): A multilevel analysis. BMC Public Health 2018, 18, 1–11. [Google Scholar] [CrossRef]
- Mitchell, S.; Andersson, N.; Ansari, N.M.; Omer, K.; Soberanis, J.L.; Cockcroft, A. Equity and vaccine uptake: A cross-sectional study of measles vaccination in Lasbela District, Pakistan. BMC Int. Health Hum. Rights 2009, 9, s7. [Google Scholar] [CrossRef] [PubMed]
- Lanaspa, M.; Balcells, R.; Sacoor, C.; Nhama, A.; Aponte, J.J.; Bassat, Q. The performance of the expanded programme on immunization in a rural area of Mozambique. Acta Trop. 2015, 149, 262–266. [Google Scholar] [CrossRef] [PubMed]
- Shrivastwa, N.; Gillespie, B.W.; Kolenic, G.E.; Lepkowski, J.M.; Boulton, M.L. Predictors of Vaccination in India for Children Aged 12-36 Months. Am. J. Prev. Med. 2015, 49, S435–S444. [Google Scholar] [CrossRef] [PubMed]
- Langsten, R.; Hill, K. The accuracy of mothers’ reports of child vaccination: evidence from rural Egypt. Soc. Sci. Med. 1998, 46, 1205–1212. [Google Scholar] [CrossRef]

| Vaccine | Recommended Schedule with the National EPI Program | WHO Recommended Time Range |
|---|---|---|
| BCG + VPO zero | At birth | Birth–4weeks |
| Penta 1 + Pneumo 1 + VPO1 + Rota1 | 6 weeks | 4 weeks–2 months |
| Penta 2 + Pneumo 2 + VPO2+ Rota2 | 10 weeks | 8 weeks–4 months |
| Penta 3 + Pneumo 3 + VPO3 | 14 weeks | 12 weeks–6 months |
| MR1 + VAA | 9 months | 38 weeks–12 months |
| MR2 | 15 months | 15–19 months |
| Characteristics of Sample | Frequency (%) | Full Immunization Coverage [95% CI] |
|---|---|---|
| Immunization status | ||
| Partially immunized | 1283 (29.04) | - |
| Fully immunized | 3133 (70.96) | - |
| External Environment | ||
| Area of residence | ||
| Urban | 1672 (37.87) | 76.51 [74.42, 78.48] |
| Rural | 2744 (62.13) | 67.57 [65.79, 69.29] |
| Ecological zone | ||
| North | 738 (16.70) | 70.30 [66.90, 73.49] |
| West | 1449 (32.82) | 80.00 [77.85, 81.98] |
| Central | 1353 (30.63) | 69.94 [67.44, 72.33] |
| South | 877 (19.85) | 58.13 [54.83, 61.36] |
| Ethnicity | ||
| Poular | 1238 (28.04) | 65.74 [63.05, 68.34] |
| Wolof | 1635 (37.02) | 74.95 [72.79, 76.99] |
| Serer | 747 (16.92) | 77.24 [74.09, 80.11] |
| Other | 796 (18.02) | 64.96 [61.58, 68.20] |
| Predisposing Characteristics | ||
| Sex | ||
| Male | 2240 (50.73) | 71.79 [69.89, 73.62] |
| Female | 2176 (49.27) | 70.09 [68.13, 71.98] |
| Birth order | ||
| First | 1043 (23.61) | 71.61 [68.79, 74.27] |
| Second | 1522 (34.47) | 73.29 [71.01, 75.45] |
| Third or more | 1851 (41.92) | 68.67 [66.52, 70.74] |
| Mother’s age at delivery | ||
| <20 years | 546 (12.36) | 63.81 [59.69, 67.74] |
| 20–34 years | 3113 (70.48) | 71.86 [70.25, 73.41] |
| 35 years and more | 758 (17.16) | 72.38 [69.09, 75.46] |
| Current marital status | ||
| Married or living with partner | 4142 (93.79) | 71.27 [69.87, 72.63] |
| Other (widowed/divorced etc.) | 274 (6.21) | 66.16 [60.35, 71.53] |
| Family size | ||
| less than 4 | 71 (1.61) | 74.66 [63.25, 83.46] |
| 4–6 | 573 (12.98) | 73.67 [69.90, 77.11] |
| 7–10 | 1100 (24.91) | 68.92 [66.12, 71.59] |
| More than 10 | 2672 (60.50) | 71.11 [69.36, 72.80] |
| Mother’s education a | ||
| No formal education | 2605 (59) | 68.14 [66.32, 69.90] |
| Primary | 1027 (23.26) | 73.43 [70.64, 76.05] |
| Secondary | 656 (14.87) | 76.26 [72.85, 79.36] |
| Higher | 127 (2.88) | 81.48 [73.73, 87.33] |
| Father’s education a | ||
| No formal education | 3143 (71.17) | 68.14 [66.49, 69.75] |
| Primary | 611 (13.84) | 76.06 [72.51, 79.28] |
| Secondary | 448 (10.14) | 77.27 [73.15, 80.92] |
| Higher | 214 (4.84) | 84.52 [79.01, 88.78] |
| Mass media access | ||
| Yes | 3583 (81.13) | 73.11 [71.63, 74.54] |
| No | 833 (18.87) | 61.69 [58.33, 64.93] |
| Enabling Resources | ||
| Place of delivery | ||
| Home | 867 (19.63) | 58.35 [55.03, 61.59] |
| Institution | 3549 (80.37) | 74.03 [72.57, 75.45] |
| No. of ANC received b | ||
| No ANC | 70 (1.85) | 38.23 [27.61, 50.12] |
| 1–3 | 1487 (39.13) | 71.28 [68.92, 73.52] |
| 4 and more | 2243 (59.02) | 74.01 [72.15, 75.78] |
| Received any PNC c | ||
| No | 1875 (42.46) | 64.25 [62.05, 66.39] |
| Yes | 2541 (57.54) | 75.9 [74.20, 77.53] |
| Wealth index | ||
| Poorest | 1025 (23.22) | 59.77 [56.74, 62.74] |
| Poorer | 968 (21.92) | 70.22 [67.26, 73.02] |
| Middle | 910 (20.61) | 71.46 [68.44, 74.31] |
| Richer | 715 (16.19) | 75.1 [71.79, 78.13] |
| Richest | 797 (18.06) | 81.93 [79.1, 84.45] |
| Mother’s healthcare decision-maker | ||
| Herself | 237 (5.71) | 78.68 [72.98, 83.45] |
| Jointly with husband | 771 (18.61) | 70.93 [67.62, 74.03] |
| Husband alone | 3054 (73.72) | 70.92 [69.28, 72.50] |
| By other | 81 (1.95) | 66.24 [55.23, 75.73] |
| Distance of health facility is a problem | ||
| Yes | 1240 (28.09) | 63.35 [60.62, 65.98] |
| No | 3176 (71.91) | 73.93 [72.37, 75.43] |
| Regions | BCG | DPT 1 | DPT 2 | DPT 3 | Polio 1 | Polio 2 | Polio 3 | Measles |
|---|---|---|---|---|---|---|---|---|
| Coverage (95% CI) | Coverage (95% CI) | Coverage (95% CI) | Coverage (95% CI) | Coverage (95% CI) | Coverage (95% CI) | Coverage (95% CI) | Coverage (95% CI) | |
| Dakar | 99.52 (98.77, 99.82) | 99.52 (98.77, 99.82) | 99.18 (98.32, 99.61) | 98.33 (97.24, 98.99) | 96.49 (95.06, 97.52) | 96.49 (95.06, 97.52) | 83.95 (81.39, 86.22) | 96.30 (94.84, 97.36) |
| Diourbel | 95.44 (93.40, 96.87) | 94.06 (91.81, 95.72) | 92.93 (90.52, 94.75) | 89.93 (87.20, 92.14) | 95.70 (93.70, 97.08) | 92.72 (90.29, 94.58) | 73.29 (69.52, 76.74) | 87.00 (83.99, 89.50) |
| Fatick | 98.72 (96.01, 99.6) | 98.82 (96.14, 99.65) | 98.51 (95.73, 99.49) | 95.83 (92.27, 97.79) | 97.96 (95.01, 99.18) | 97.46 (94.36, 98.88) | 74.92 (68.83, 80.15) | 91.44 (87.00, 94.46) |
| Kaffrine | 96.15 (92.87, 97.96) | 97.57 (94.68, 98.91) | 95.52 (92.09, 97.51) | 94.29 (90.59, 96.59) | 96.38 (93.15, 98.11) | 94.98 (91.43, 97.11) | 79.51 (73.99, 84.11) | 89.44 (84.93, 92.72) |
| Kaolack | 99.71 (97.70, 99.96) | 99.50 (97.58, 99.90) | 97.81 (95.39, 98.97) | 95.23 (92.17, 97.13) | 98.86 (96.78, 99.60) | 96.69 (93.97, 98.21) | 82.53 (77.84, 86.41) | 90.98 (87.19, 93.73) |
| Kedougou | 61.90 (48.70, 73.55) | 68.10 (54.94, 78.89) | 64.89 (51.69, 76.15) | 59.77 (46.60, 71.66) | 68.06 (54.91, 78.85) | 63.70 (50.49, 75.12) | 42.94 (30.75, 56.04) | 49.24 (36.53, 62.04) |
| Kolda | 91.88 (87.63, 94.76) | 95.44 (91.89, 97.48) | 93.21 (89.19, 95.80) | 91.91 (87.67, 94.78) | 93.96 (90.09, 96.38) | 92.19 (87.99, 95.00) | 68.93 (62.72, 74.52) | 87.21 (82.30, 90.91) |
| Louga | 94.55 (91.22, 96.66) | 95.91 (92.88, 97.68) | 95.07 (91.86, 97.06) | 91.84 (88.05, 94.51) | 93.60 (90.10, 95.92) | 91.31 (87.43, 94.07) | 77.96 (72.78, 82.40) | 84.1 (79.38, 87.90) |
| Matam | 91.90 (86.88, 95.1) | 94.10 (89.54, 96.75) | 92.25 (87.30, 95.37) | 89.55 (84.13, 93.26) | 86.68 (80.86, 90.92) | 84.39 (78.30, 89.01) | 70.40 (63.29, 76.63) | 81.83 (75.47, 86.82) |
| Saint-Louis | 99.20 (97.02, 99.79) | 99.18 (97.00, 99.78) | 98.34 (95.89, 99.34) | 97.74 (95.10, 98.97) | 95.97 (92.86, 97.76) | 93.92 (90.38, 96.22) | 82.91 (77.96, 86.94) | 94.95 (91.61, 97.01) |
| Sedhiou | 95.77 (91.21, 98.01) | 97.16 (93.01, 98.87) | 94.89 (90.10, 97.43) | 89.74 (83.91, 93.62) | 93.51 (88.41, 96.46) | 90.25 (84.50, 94.01) | 77.40 (70.19, 83.29) | 88.96 (83.01, 93.00) |
| Tamba-counda | 72.96 (67.45, 77.84) | 78.17 (72.94, 82.63) | 72.39 (66.85, 77.31) | 70.51 (64.90, 75.56) | 76.50 (71.17, 81.10) | 71.28 (65.70, 76.28) | 56.97 (51.10, 62.65) | 65.5 (59.73, 70.84) |
| Thiés | 98.89 (97.59, 99.49) | 99.70 (98.65, 99.93) | 99.70 (98.65, 99.93) | 98.48 (97.05, 99.22) | 98.60 (97.21, 99.30) | 98.6 (97.21, 99.30) | 85.05 (81.85, 87.77) | 92.52 (90.03, 94.43) |
| Ziguinchor | 99.69 (94.50, 99.98) | 98.67 (94.69, 99.67) | 97.37 (93.04, 99.04) | 94.57 (89.45, 97.28) | 96.05 (91.32, 98.25) | 93.71 (88.38, 96.68) | 79.94 (72.61, 85.69) | 92.00 (86.31, 95.45) |
| Overall | 95.33 (94.66, 95.91) | 96.11 (95.50, 96.64) | 94.82 (94.12, 95.43) | 92.83 (92.03, 93.55) | 94.37 (93.65, 95.02) | 92.69 (91.88, 93.42) | 77.47 (76.22, 78.68) | 88.69 (87.72, 89.59) |
| Characteristics | Model I | Model II | ||
|---|---|---|---|---|
| Unadjusted OR (95% CI) | p-Value | Adjusted OR (95% CI) | p-Value | |
| External Environment | ||||
| Area of residence | ||||
| Urban | 1.56 (1.36, 1.80) | <0.001 | 0.96 (0.77, 1.21) | 0.752 |
| Rural | 1.00 | 1.00 | ||
| Ecological zone | ||||
| North | 1.71 (1.39, 2.10) | <0.001 | 1.42 (1.09, 1.84) | 0.009 |
| West | 2.88 (2.39, 3.47) | <0.001 | 1.66 (1.25, 2.21) | 0.001 |
| Central | 1.68 (1.4, 2.00) | <0.001 | 1.14 (0.89, 1.46) | 0.288 |
| South | 1.00 | 1.00 | ||
| Ethnicity | ||||
| Poular | 1.00 | 1.00 | ||
| Wolof | 1.56 (1.33, 1.83) | <0.001 | 1.15 (0.93, 1.42) | 0.197 |
| Serer | 1.77 (1.44, 2.18) | <0.001 | 1.43 (1.09, 1.88) | 0.011 |
| Other | 0.97 (0.80, 1.16) | 0.719 | 0.86 (0.68, 1.10) | 0.232 |
| Predisposing Characteristics | ||||
| Sex | ||||
| Male | 1.09 (0.95, 1.24) | 0.212 | 1.08 (0.93, 1.26) | 0.314 |
| Female | 1.00 | 1.00 | ||
| Birth order | ||||
| First | 1.15 (0.97, 1.36) | 0.098 | 1.25 (0.95, 1.64) | 0.108 |
| Second | 1.25 (1.08, 1.45) | 0.003 | 1.17 (0.97, 1.43) | 0.103 |
| Third or more | 1.00 | 1.00 | ||
| Mother’s age at delivery | ||||
| <20 years | 1.00 | 1.00 | ||
| 20–34 years | 1.45 (1.20, 1.75) | <0.001 | 1.45 (1.10, 1.93) | 0.009 |
| 35 years and more | 1.49 (1.17, 1.88) | 0.001 | 1.57 (1.10, 2.23) | 0.012 |
| Mother’s education | ||||
| No formal education | 1.00 | 1.00 | ||
| Primary | 1.29 (1.10, 1.52) | 0.002 | 0.91 (0.74, 1.12) | 0.361 |
| Secondary | 1.5 (1.23, 1.83) | <0.001 | 1.21 (0.91, 1.61) | 0.199 |
| Higher | 2.06 (1.31, 3.24) | 0.002 | 0.68 (0.39, 1.20) | 0.184 |
| Father’s education | ||||
| No formal education | 1.00 | 1.00 | ||
| Primary | 1.49 (1.22, 1.81) | <0.001 | 1.05 (0.82, 1.34) | 0.680 |
| Secondary | 1.59 (1.26, 2.01) | <0.001 | 1.06 (0.80, 1.42) | 0.686 |
| Higher | 2.55 (1.75, 3.73) | <0.001 | 1.48 (0.93, 2.35) | 0.102 |
| Mass media access | ||||
| Yes | 1.69 (1.44, 1.98) | <0.001 | 1.40 (1.15, 1.71) | 0.001 |
| No | 1.00 | 1.00 | ||
| Enabling Resources | ||||
| Wealth index | ||||
| Poorest | 1.00 | 1.00 | ||
| Poorer | 1.59 (1.32, 1.91) | <0.001 | 1.26 (1.00, 1.59) | 0.049 |
| Middle | 1.69 (1.39, 2.04) | <0.001 | 1.05 (0.81, 1.38) | 0.704 |
| Richer | 2.03 (1.64, 2.50) | <0.001 | 1.09 (0.78, 1.53) | 0.597 |
| Richest | 3.05 (2.45, 3.80) | <0.001 | 1.34 (0.91, 1.99) | 0.140 |
| No. of ANC received | ||||
| No ANC | 1.00 | 1.00 | ||
| 1–3 | 4.01 (2.45, 6.57) | <0.001 | 2.27 (1.32, 3.90) | 0.003 |
| 4 and more | 4.60 (2.82, 7.51) | <0.001 | 2.06 (1.19, 3.57) | 0.010 |
| Place of delivery | ||||
| Home | 1.00 | 1.00 | ||
| Institution | 2.04 (1.74, 2.38) | <0.001 | 1.47 (1.20, 1.80) | <0.001 |
| Received any PNC | ||||
| No | 1.00 | 1.00 | ||
| Yes | 1.75 (1.54, 2.00) | <0.001 | 1.25 (1.05, 1.49) | 0.011 |
| Mother’s healthcare decision-maker | ||||
| Husband alone | 1.00 | 1.00 | ||
| Herself | 1.51 (1.10, 2.09) | 0.011 | 1.30 (0.90, 1.87) | 0.155 |
| Jointly with husband | 1.00 (0.84, 1.19) | 0.993 | 0.89 (0.73, 1.09) | 0.271 |
| By other | 0.80 (0.5, 1.28) | 0.362 | 0.81 (0.49, 1.36) | 0.433 |
| Distance of health facility is a problem | ||||
| Yes | 1.00 | 1.00 | ||
| No | 1.64 (1.43, 1.89) | <0.001 | 1.13 (0.94, 1.37) | 0.194 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sarker, A.R.; Akram, R.; Ali, N.; Chowdhury, Z.I.; Sultana, M. Coverage and Determinants of Full Immunization: Vaccination Coverage among Senegalese Children. Medicina 2019, 55, 480. https://doi.org/10.3390/medicina55080480
Sarker AR, Akram R, Ali N, Chowdhury ZI, Sultana M. Coverage and Determinants of Full Immunization: Vaccination Coverage among Senegalese Children. Medicina. 2019; 55(8):480. https://doi.org/10.3390/medicina55080480
Chicago/Turabian StyleSarker, Abdur Razzaque, Raisul Akram, Nausad Ali, Zahedul Islam Chowdhury, and Marufa Sultana. 2019. "Coverage and Determinants of Full Immunization: Vaccination Coverage among Senegalese Children" Medicina 55, no. 8: 480. https://doi.org/10.3390/medicina55080480
APA StyleSarker, A. R., Akram, R., Ali, N., Chowdhury, Z. I., & Sultana, M. (2019). Coverage and Determinants of Full Immunization: Vaccination Coverage among Senegalese Children. Medicina, 55(8), 480. https://doi.org/10.3390/medicina55080480





