Risk Assessment for Self Reported Obstructive Sleep Apnea and Excessive Daytime Sleepiness in a Greek Nursing Staff Population
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. OSAS and EDS Assessment Tools
2.3. Statistical Analysis
3. Results
3.1. Study Population
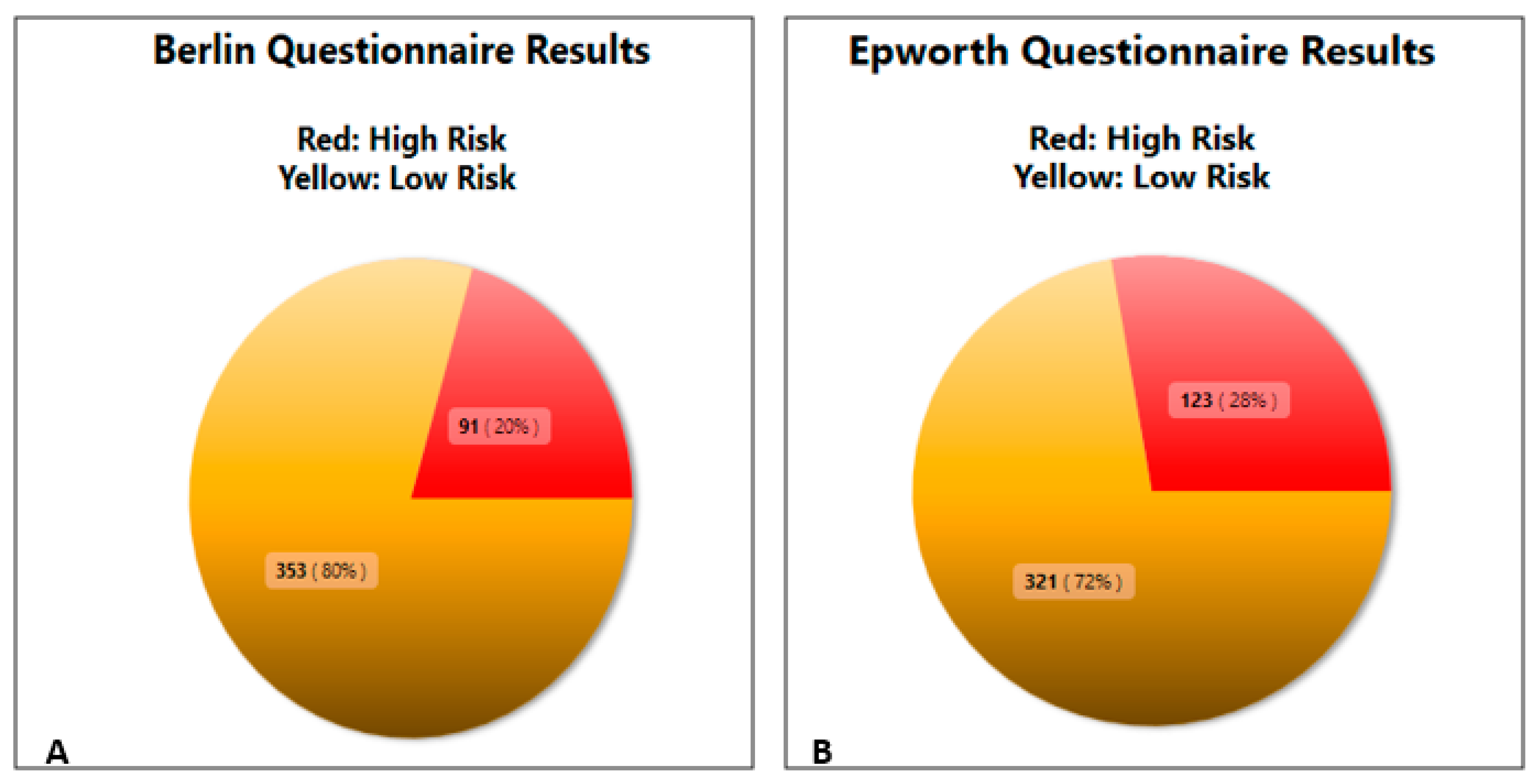
3.2. BQ and ESS Questionnaire Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Veale, D. Chronic respiratory care and rehabilitation in France. Chron. Respir. Dis. 2006, 3, 215–216. [Google Scholar] [CrossRef] [PubMed]
- Berry, R.B.; Budhiraja, R.; Gottlieb, D.J.; Gozal, D.; Iber, C.; Kapur, V.K.; Marcus, C.L.; Mehra, R.; Parthasarathy, S.; Quan, S.F.; et al. Rules for scoring respiratory events in sleep: Update of the 2007 AASM manual for the scoring of sleep and associated events. J. Clin. Sleep Med. 2012, 8, 597–619. [Google Scholar] [CrossRef] [PubMed]
- Jennum, P.; Riha, R.L. Epidemiology of sleep apnoea/hypopnoea syndrome and sleep-disordered breathing. Eur. Respir. J. 2009, 33, 907–914. [Google Scholar] [CrossRef] [PubMed]
- Carlucci, M.; Smith, M.; Corbridge, S.J. Poor sleep, hazardous breathing: an overview of obstructive sleep apnea. Nurse Pract. 2013, 38, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Peppard, P.E.; Young, T.; Barnet, J.H.; Palta, M.; Hagen, E.W.; Hla, K.M. Increased prevalence of sleep-disordered breathing in adults. Am. J. Epidemiol. 2013, 177, 1006–1014. [Google Scholar] [CrossRef] [PubMed]
- Heinzer, R.; Vat, S.; Marques-Vidal, P.; Marti-Soler, H.; Andries, D.; Tobback, N.; Mooser, V.; Preisig, M.; Malhotra, A.; Waeber, G.; et al. Prevalence of sleep-disordered breathing in the general population: The HypnoLaus study. Lancet Respir. Med. 2015, 3, 310–318. [Google Scholar] [CrossRef]
- Simpson, L.; Hillman, D.R.; Cooper, M.N.; Ward, K.L.; Hunter, M.; Cullen, S.; James, A.; Palmer, L.J.; Mukherjee, S.; Eastwood, P. High prevalence of undiagnosed obstructive sleep apnoea in the general population and methods for screening for representative controls. Sleep Breath. 2013, 17, 967–973. [Google Scholar] [CrossRef] [PubMed]
- Punjabi, N.M. The epidemiology of adult obstructive sleep apnea. Proc. Am. Thorac. Soc. 2008, 5, 136–143. [Google Scholar] [CrossRef]
- Mirrakhimov, A.E.; Sooronbaev, T.; Mirrakhimov, E.M. Prevalence of obstructive sleep apnea in Asian adults: a systematic review of the literature. BMC Pulm. Med. 2013, 13, 10. [Google Scholar] [CrossRef]
- Sharma, S.K.; Ahluwalia, G. Epidemiology of adult obstructive sleep apnoea syndrome in India. Indian J. Med. Res. 2010, 131, 171–175. [Google Scholar]
- Mahboub, B.; Afzal, S.; Alhariri, H.; Alzaabi, A.; Vats, M.; Soans, A. Prevalence of symptoms and risk of sleep apnea in Dubai, UAE. Int. J. Gen. Med. 2013, 6, 109–114. [Google Scholar] [PubMed]
- BaHammam, A.S.; Alrajeh, M.S.; Al-Jahdali, H.H.; BinSaeed, A.A. Prevalence of symptoms and risk of sleep apnea in middle-aged Saudi males in primary care. Saudi Med. J. 2008, 29, 423–426. [Google Scholar] [PubMed]
- Kang, K.; Seo, J.G.; Seo, S.H.; Park, K.S.; Lee, H.W. Prevalence and related factors for high-risk of obstructive sleep apnea in a large Korean population: Results of a questionnaire-based study. J. Clin. Neurol. 2014, 10, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Tufik, S.; Santos-Silva, R.; Taddei, J.A.; Bittencourt, L.R.A. Obstructive Sleep Apnea Syndrome in the Sao Paulo Epidemiologic Sleep Study. Sleep Med. 2010, 11, 441–446. [Google Scholar] [CrossRef] [PubMed]
- Akkoyunlu, M.E.; Altin, R.; Kart, L.; Atalay, F.; Örnek, T.; Bayram, M.; Tor, M. Investigation of obstructive sleep apnoea syndrome prevalence among long-distance drivers from Zonguldak, Turkey. Multidiscip. Respir. Med. 2013, 8, 2–7. [Google Scholar] [CrossRef]
- Geiger-Brown, J.; Rogers, V.E.; Han, K.; Trinkoff, A.; Bausell, R.B.; Scharf, S.M. Occupational screening for sleep disorders in 12-h shift nurses using the Berlin Questionnaire. Sleep Breath. 2013, 17, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Simpson, G. Circadian rhythm sleep disorders. J. R. Coll. Physicians Edinb. 2011, 41, 94. [Google Scholar]
- Rajaratnam, S.M.W.; Howard, M.E.; Grunstein, R.R. Sleep loss and circadian disruption in shift work: health burden and management. Med. J. Aust. 2013, 199, 11–15. [Google Scholar] [CrossRef]
- Ko, H.S.; Kim, M.Y.; Kim, Y.H.; Lee, J.; Park, Y.G.; Moon, H.B.; Kil, K.C.; Lee, G.; Kim, S.J.; Shin, J.C. Obstructive sleep apnea screening and perinatal outcomes in Korean pregnant women. Arch. Gynecol. Obstet. 2013, 287, 429–433. [Google Scholar] [CrossRef]
- Lee, Y.C.; Eun, Y.G.; Shin, S.Y.; Kim, S.W. Prevalence of snoring and high risk of obstructive sleep apnea syndrome in young male soldiers in Korea. J. Korean Med. Sci. 2013, 28, 1373–1377. [Google Scholar] [CrossRef]
- Laudencka, A.; Klawe, J.J.; Tafil-Klawe, M.; Zlomanczuk, P. Does night-shift work induce apnea events in osbtructive sleep apnea patients? J. Physiol. Pharmacol. 2007, 58, 345–347. [Google Scholar]
- Paciorek, M.; Korczynski, P.; Bielicki, P.; Byśkiniewicz, K.; Zieliński, J.; Chazan, R. Obstructive sleep apnea in shift workers. Sleep Med. 2011, 12, 274–277. [Google Scholar] [CrossRef]
- Bouloukaki, I.; Komninos, I.D.; Mermigkis, C.; Micheli, K.; Komninou, M.; Moniaki, V.; Mauroudi, E.; Siafakas, N.M.; Schiza, S.E. Translation and validation of Berlin questionnaire in primary health care in Greece. BMC Pulm. Med. 2013, 13, 6. [Google Scholar] [CrossRef]
- Tsara, V.; Serasli, E.; Amfilochiou, A.; Constantinidis, T.; Christaki, P. Greek version of the Epworth Sleepiness Scale. Sleep Breath. 2004, 8, 91–95. [Google Scholar] [CrossRef]
- Romandini, M.; Gioco, G.; Perfetti, G.; Deli, G.; Staderini, E.; Laforì, A. The association between periodontitis and sleep duration. J. Clin. Periodontol. 2017, 44, 490–501. [Google Scholar] [CrossRef]
- Gaspar, L.S.; Alvaro, A.R.; Moita, J.; Cavadas, C. Obstructive sleep apnea and hallmarks of aging. Trends Mol. Med. 2017, 23, 675–692. [Google Scholar] [CrossRef]
- Roky, R.; Chapotot, F.; Benchekroun, M.T.; Benaji, B.; Hakkou, F.; Elkhalifi, H.; Buguet, A. Daytime sleepiness during Ramadan intermittent fasting: polysomnographic and quantitative waking EEG study. J. Sleep Res. 2003, 12, 95–101. [Google Scholar] [CrossRef]
- Vagiakis, E.; Kapsimalis, F.; Lagogianni, I.; Perraki, H.; Minaritzoglou, A.; Alexandropoulou, K.; Roussos, C.; Kryger, M. Gender differences on polysomnographic findings in Greek subjects with obstructive sleep apnea syndrome. Sleep Med. 2006, 7, 424–430. [Google Scholar] [CrossRef]
- Barger, L.K.; Lockley, S.W.; Shea, S.A.; Wang, W.; Landrigan, C.P.; O’Brien, C.S.; Qadri, S.; Sullivan, J.P.; Cade, B.E.; Epstein, L.J.; et al. Sleep disorders, health and safety in Police Officers. Jama 2013, 306, 2567–2578. [Google Scholar]
- Gander, P.; OKeeffe, K.; Santos-Fernandez, E.; Annette, H.; Leonie, W.; Jinny, W. Fatigue and nurses’ work patterns: An online questionnaire survey. Int. J. Nurs. Stud. 2019, 98, 67–74. [Google Scholar] [CrossRef]
- Brown, J.G.; Wieroney, M.; Blair, L.; Zhu, S.; Warren, J.; Scharf, S.M.; Hinds, P.S. Measuring subjective sleepiness at work in hospital nurses: Validation of a modified delivery format of the Karolinska Sleepiness Scale. Sleep Breath. 2014, 18, 731–739. [Google Scholar] [CrossRef]
- Chen, L.; Luo, C.; Liu, S.; Chen, W.; Liu, Y.; Li, Y.; Du, Y.; Zou, H.; Pan, J. Excessive daytime sleepiness in general hospital nurses: prevalence, correlates, and its association with adverse events. Sleep Breath. 2019, 23, 209–216. [Google Scholar] [CrossRef]
- Khan, S.; Duan, P.; Yao, L.; Hou, H. Shiftwork-mediated disruptions of circadian rhythms and sleep homeostasis cause serious health problems. Int. J. Genomics 2018, 2018, 8576890. [Google Scholar] [CrossRef]

| Males | Females | p Value | |
|---|---|---|---|
| Gender (%) | 56 (12.6%) | 388 (87.4%) | - |
| Age (years) | 42.91 ± 5.76 | 41.41 ± 5.92 | 0.047 |
| Height (m) | 1.78 ± 0.06 | 1.65 ± 0.05 | <0.001 |
| Weight (kg) | 86.05 ± 14.30 | 67.91 ± 12.03 | <0.001 |
| BMI | 27.17 ± 4.32 | 25.08 ± 4.43 | <0.001 |
| Smokers—Yes(#) | 29 (51.79%) | 171 (44.07%) | 0.39 |
| Pack Years (#) | 14.61 ± 11.31 | 15.78 ± 11.18 | 0.59 |
| Alcohol Consumption—Yes (%) | 40 (70.42%) | 192 (49.48%) | 0.004 |
| Working on Night Shifts—Yes (%) | 44 (78.57%) | 287 (73.97%) | 0.52 |
| Night Shifts per month (#) | 4.43 ± 1.87 | 6.25 ± 2.25 | <0.001 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alexandropoulou, A.; Vavougios, G.D.; Hatzoglou, C.; Gourgoulianis, K.I.; Zarogiannis, S.G. Risk Assessment for Self Reported Obstructive Sleep Apnea and Excessive Daytime Sleepiness in a Greek Nursing Staff Population. Medicina 2019, 55, 468. https://doi.org/10.3390/medicina55080468
Alexandropoulou A, Vavougios GD, Hatzoglou C, Gourgoulianis KI, Zarogiannis SG. Risk Assessment for Self Reported Obstructive Sleep Apnea and Excessive Daytime Sleepiness in a Greek Nursing Staff Population. Medicina. 2019; 55(8):468. https://doi.org/10.3390/medicina55080468
Chicago/Turabian StyleAlexandropoulou, Alexia, Georgios D. Vavougios, Chrissi Hatzoglou, Konstantinos I. Gourgoulianis, and Sotirios G. Zarogiannis. 2019. "Risk Assessment for Self Reported Obstructive Sleep Apnea and Excessive Daytime Sleepiness in a Greek Nursing Staff Population" Medicina 55, no. 8: 468. https://doi.org/10.3390/medicina55080468
APA StyleAlexandropoulou, A., Vavougios, G. D., Hatzoglou, C., Gourgoulianis, K. I., & Zarogiannis, S. G. (2019). Risk Assessment for Self Reported Obstructive Sleep Apnea and Excessive Daytime Sleepiness in a Greek Nursing Staff Population. Medicina, 55(8), 468. https://doi.org/10.3390/medicina55080468







