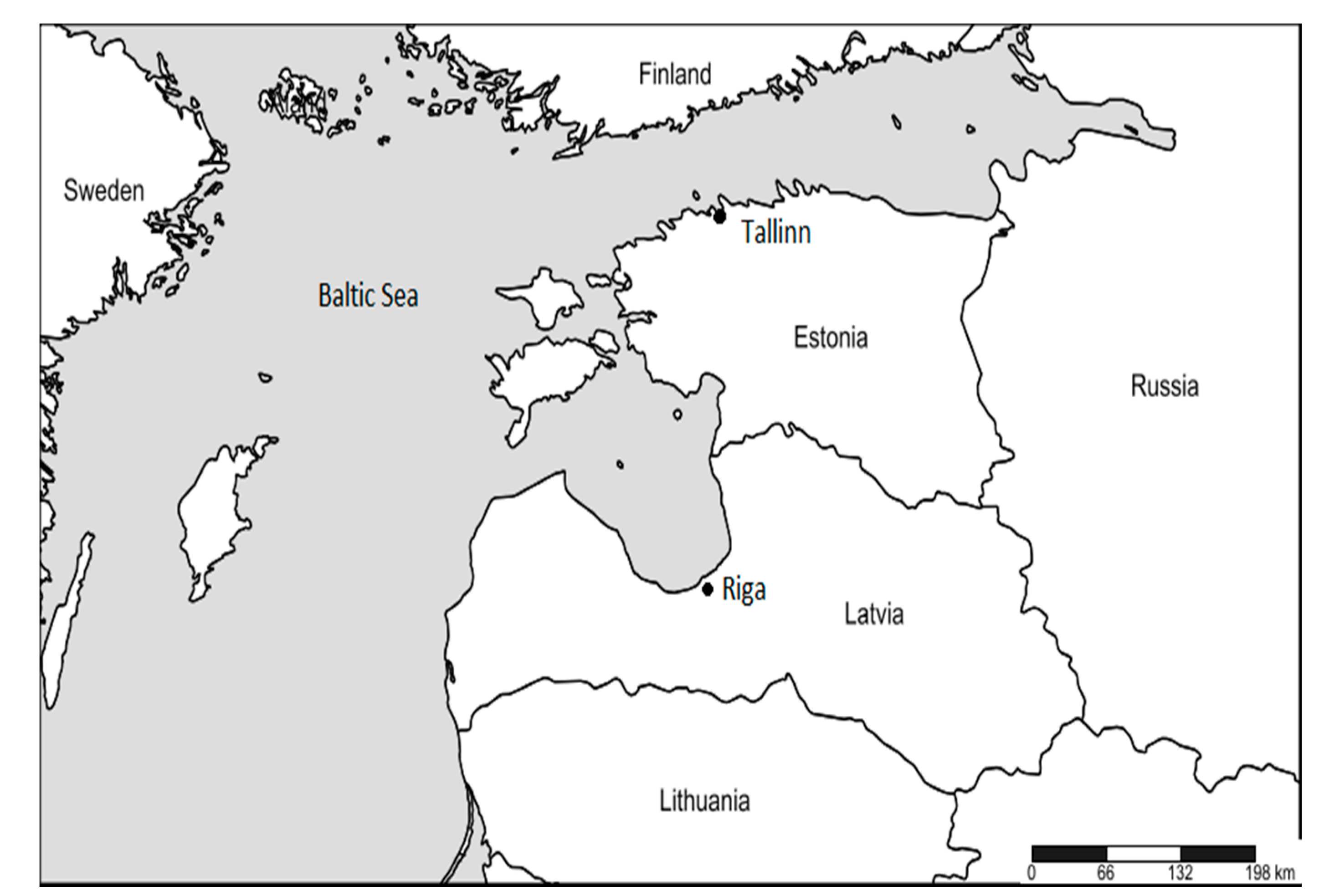
Mortality Related to Cold Temperatures in Two Capitals of the Baltics: Tallinn and Riga
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Guo, Y.; Gasparrini, A.; Armstrong, B.G.; Tawatsupa, B.; Tobias, A.; Lavigne, E.; de Sousa Zanotti Stagliorio Coelho, M.; Pan, X.; Kim, H.; Hashizume, M.; et al. Heat Wave and Mortality: A Multicountry, Multicommunity Study. Environ. Health Perspect. 2017, 125, 087006. [Google Scholar] [CrossRef] [PubMed]
- Åström, D.O.; Åström, C.; Forsberg, B.; Vicedo-Cabrera, A.M.; Gasparrini, A.; Oudin, A.; Sundquist, K. Heat wave–related mortality in Sweden: A case-crossover study investigating effect modification by neighbourhood deprivation. Scand. J. Public Health 2018. [CrossRef]
- Ruuhela, R.; Hyvärinen, O.; Jylhä, K.; Ruuhela, R.; Hyvärinen, O.; Jylhä, K. Regional Assessment of Temperature-Related Mortality in Finland. Int. J. Environ. Res. Public Health 2018, 15, 406. [Google Scholar] [CrossRef] [PubMed]
- Graczyk, D.; Kundzewicz, Z.W.; Choryński, A.; Førland, E.J.; Pińskwar, I.; Szwed, M. Heat-related mortality during hot summers in Polish cities. Theor. Appl. Climatol. 2019, 136, 1259–1273. [Google Scholar] [CrossRef]
- Åström, D.O.; Åström, C.; Rekker, K.; Indermitte, E.; Orru, H. High Summer Temperatures and Mortality in Estonia. PLoS ONE 2016, 11, e0155045. [Google Scholar]
- Åström, D.O.; Ebi, K.L.; Vicedo-Cabrera, A.M.; Gasparrini, A. Investigating changes in mortality attributable to heat and cold in Stockholm, Sweden. Int. J. Biometeorol. 2018, 62, 1777–1780. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A.; Guo, Y.; Hashizume, M.; Lavigne, E.; Zanobetti, A.; Schwartz, J.; Tobias, A.; Tong, S.; Rocklöv, J.; Forsberg, B.; et al. Mortality risk attributable to high and low ambient temperature: A multicountry observational study. Lancet 2015, 386, 369–375. [Google Scholar] [CrossRef]
- Cui, Y.; Yin, F.; Deng, Y.; Volinn, E.; Chen, F.; Ji, K.; Zeng, J.; Zhao, X.; Li, X. Heat or Cold: Which One Exerts Greater Deleterious Effects on Health in a Basin Climate City? Impact of Ambient Temperature on Mortality in Chengdu, China. Int. J. Environ. Res. Public Health 2016, 13, 1225. [Google Scholar]
- Gronlund, C.J.; Sullivan, K.P.; Kefelegn, Y.; Cameron, L.; O’Neill, M.S. Climate change and temperature extremes: A review of heat- and cold-related morbidity and mortality concerns of municipalities. Maturitas 2018, 114, 54–59. [Google Scholar] [CrossRef]
- Guo, Y.; Gasparrini, A.; Armstrong, B.; Li, S.; Tawatsupa, B.; Tobias, A.; Lavigne, E.; de Sousa Zanotti Stagliorio Coelho, M.; Leone, M.; Pan, X.; et al. Global variation in the effects of ambient temperature on mortality: A systematic evaluation. Epidemiology 2014, 25, 781–789. [Google Scholar] [CrossRef]
- Wang, C.; Zhang, Z.; Zhou, M.; Zhang, L.; Yin, P.; Ye, W.; Chen, Y. Nonlinear relationship between extreme temperature and mortality in different temperature zones: A systematic study of 122 communities across the mainland of China. Sci. Total Environ. 2017, 586, 96–106. [Google Scholar] [CrossRef]
- Ryti, N.R.I.; Guo, Y.; Jaakkola, J.J.K. Global Association of Cold Spells and Adverse Health Effects: A Systematic Review and Meta-Analysis. Environ. Health Perspect. 2016, 124, 12–22. [Google Scholar] [CrossRef]
- Chen, T.H.; Li, X.; Zhao, J.; Zhang, K. Impacts of cold weather on all-cause and cause-specific mortality in Texas, 1990–2011. Environ. Pollut. 2017, 225, 244–251. [Google Scholar] [CrossRef]
- Bai, L.; Li, Q.; Wang, J.; Lavigne, E.; Gasparrini, A.; Copes, R.; Yagouti, A.; Burnett, R.T.; Goldberg, M.S.; Cakmak, S.; et al. Increased coronary heart disease and stroke hospitalisations from ambient temperatures in Ontario. Heart 2018, 104, 673–679. [Google Scholar] [CrossRef]
- Ryti, N.R.I.; Mäkikyrö, E.M.S.; Antikainen, H.; Junttila, M.J.; Hookana, E.; Ikäheimo, T.M.; Kortelainen, M.-L.; Huikuri, H.V.; Jaakkola, J.J.K. Cold spells and ischaemic sudden cardiac death: Effect modification by prior diagnosis of ischaemic heart disease and cardioprotective medication. Sci. Rep. 2017, 7, 41060. [Google Scholar] [CrossRef]
- Sun, Z.; Chen, C.; Xu, D.; Li, T. Effects of ambient temperature on myocardial infarction: A systematic review and meta-analysis. Environ. Pollut. 2018, 241, 1106–1114. [Google Scholar] [CrossRef]
- Mohammad, M.A.; Koul, S.; Rylance, R.; Fröbert, O.; Alfredsson, J.; Sahlén, A.; Witt, N.; Jernberg, T.; Muller, J.; Erlinge, D. Association of Weather With Day-to-Day Incidence of Myocardial Infarction. JAMA Cardiol. 2018, 3, 1081. [Google Scholar] [CrossRef]
- D’Amato, M.; Molino, A.; Calabrese, G.; Cecchi, L.; Annesi-Maesano, I.; D’Amato, G. The impact of cold on the respiratory tract and its consequences to respiratory health. Clin. Transl. Allergy 2018, 8, 1–8. [Google Scholar] [CrossRef]
- Marí-Dell’Olmo, M.; Tobías, A.; Gómez-Gutiérrez, A.; Rodríguez-Sanz, M.; de Olalla, P.G.; Camprubí, E.; Gasparrini, A.; Borrell, C. Social inequalities in the association between temperature and mortality in a South European context. Int. J. Public Health 2019, 64, 27–37. [Google Scholar] [CrossRef]
- Orru, H.; Åström, D.O. Increases in external cause mortality due to high and low temperatures: Evidence from northeastern Europe. Int. J. Biometeorol. 2017, 61, 963–966. [Google Scholar] [CrossRef]
- Carmona, R.; Díaz, J.; Mirón, I.J.; Ortíz, C.; León, I.; Linares, C. Geographical variation in relative risks associated with cold waves in Spain: The need for a cold wave prevention plan. Environ. Int. 2016, 88, 103–111. [Google Scholar] [CrossRef]
- Peel, M.C.; Finlayson, B.L.; McMahon, T.A. Updated world map of the Köppen-Geiger climate classification. Hydrol. Earth Syst. Sci. 2007, 11, 1633–1644. [Google Scholar] [CrossRef]
- Lu, Y.; Zeger, S.L. On the equivalence of case-crossover and time series methods in environmental epidemiology. Biostatistics 2007, 8, 337–344. [Google Scholar] [CrossRef]
- Armstrong, B.G.; Gasparrini, A.; Tobias, A. Conditional Poisson models: A flexible alternative to conditional logistic case cross-over analysis. BMC Med. Res. Methodol. 2014, 14, 122. [Google Scholar] [CrossRef]
- Gasparrini, A.; Armstrong, B.; Kenward, M.G. Distributed lag non-linear models. Stat. Med. 2010, 29, 2224–2234. [Google Scholar] [CrossRef]
- Gasparrini, A. Distributed Lag Linear and Non-Linear Models in R: The Package dlnm. J. Stat. Softw. 2011, 43, 1–20. [Google Scholar] [CrossRef]
- Healy, J.D. Excess winter mortality in Europe: A cross country analysis identifying key risk factors. J. Epidemiol. Commun. Health 2003, 57, 784–789. [Google Scholar] [CrossRef]
- Health in the Baltic Countries. 2015. Available online: http://rahvatervis.ut.ee/handle/1/6850 (accessed on 11 June 2019).
- Berķe-Berga, A.; Paul, P.; Valtonen, H. Examining Health Inequalities in Latvia: A Decade of Association between Socioeconomic Position and Perceived Health Status. Biomed. Res. Int. 2017, 2017, 7541416. [Google Scholar] [CrossRef]
- Yang, J.; Yin, P.; Zhou, M.; Ou, C.-Q.; Li, M.; Li, J.; Liu, X.; Gao, J.; Liu, Y.; Qin, R.; et al. The burden of stroke mortality attributable to cold and hot ambient temperatures: Epidemiological evidence from China. Environ. Int. 2016, 92, 232–238. [Google Scholar] [CrossRef]
- Respiratory diseases statistics—Statistics Explained. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php/Respiratory_diseases_statistics#Deaths_from_diseases_of_the_respiratory_system (accessed on 13 May 2019).
- Martinez, G.S.; Diaz, J.; Hooyberghs, H.; Lauwaet, D.; De Ridder, K.; Linares, C.; Carmona, R.; Ortiz, C.; Kendrovski, V.; Adamonyte, D. Cold-related mortality vs. heat-related mortality in a changing climate: A case study in Vilnius (Lithuania). Environ. Res. 2018, 166, 384–393. [Google Scholar]
- Murage, P.; Hajat, S.; Bone, A.; Murage, P.; Hajat, S.; Bone, A. Variation in Cold-Related Mortality in England Since the Introduction of the Cold Weather Plan: Which Areas Have the Greatest Unmet Needs? Int. J. Environ. Res. Public Health 2018, 15, 2588. [Google Scholar] [CrossRef]
- Ruuhela, R.; Jylhä, K.; Lanki, T.; Tiittanen, P.; Matzarakis, A. Biometeorological Assessment of Mortality Related to Extreme Temperatures in Helsinki Region, Finland, 1972–2014. Int. J. Environ. Res. Public Health 2017, 14, 944. [Google Scholar] [CrossRef]
- Analitis, A.; Katsouyanni, K.; Biggeri, A.; Baccini, M.; Forsberg, B.; Bisanti, L.; Kirchmayer, U.; Ballester, F.; Cadum, E.; Goodman, P.G.; et al. Effects of Cold Weather on Mortality: Results From 15 European Cities Within the PHEWE Project. Am. J. Epidemiol. 2008, 168, 1397–1408. [Google Scholar] [CrossRef]
- Hu, K.; Guo, Y.; Hochrainer-Stigler, S.; Liu, W.; See, L.; Yang, X.; Zhong, J.; Fei, F.; Chen, F.; Zhang, Y.; et al. Evidence for Urban–Rural Disparity in Temperature–Mortality Relationships in Zhejiang Province, China. Environ. Health Perspect. 2019, 127, 037001. [Google Scholar] [CrossRef]
- Donaldson, G.C.; Witt, C.; Näyhä, S. Changes in cold-related mortalities between 1995 and 2016 in South East England. Public Health 2019, 169, 36–40. [Google Scholar] [CrossRef]
- O’Neill, M.S.; Zanobetti, A.; Schwartz, J. Modifiers of the Temperature and Mortality Association in Seven US Cities. Am. J. Epidemiol. 2003, 157, 1074–1082. [Google Scholar] [CrossRef]
- Analitis, A.; de’ Donato, F.; Scortichini, M.; Lanki, T.; Basagana, X.; Ballester, F.; Astrom, C.; Paldy, A.; Pascal, M.; Gasparrini, A.; et al. Synergistic Effects of Ambient Temperature and Air Pollution on Health in Europe: Results from the PHASE Project. Int. J. Environ. Res. Public Health 2018, 15, 1856. [Google Scholar] [CrossRef]
- Cheng, Y.; Kan, H. Effect of the interaction between outdoor air pollution and extreme temperature on daily mortality in Shanghai, China. J. Epidemiol. 2012, 22, 28–36. [Google Scholar] [CrossRef]
- Olstrup, H.; Johansson, C.; Forsberg, B.; Åström, C.; Olstrup, H.; Johansson, C.; Forsberg, B.; Åström, C. Association between Mortality and Short-Term Exposure to Particles, Ozone and Nitrogen Dioxide in Stockholm, Sweden. Int. J. Environ. Res. Public Health 2019, 16, 1028. [Google Scholar] [CrossRef]
- Shah, V.; Jaeglé, L.; Thornton, J.A.; Lopez-Hilfiker, F.D.; Lee, B.H.; Schroder, J.C.; Campuzano-Jost, P.; Jimenez, J.L.; Guo, H.; Sullivan, A.P.; et al. Chemical feedbacks weaken the wintertime response of particulate sulfate and nitrate to emissions reductions over the eastern United States. Proc. Natl. Acad. Sci. USA. 2018, 115, 8110–8115. [Google Scholar] [CrossRef]
- Chen, K.; Wolf, K.; Breitner, S.; Gasparrini, A.; Stafoggia, M.; Samoli, E.; Andersen, Z.J.; Bero-Bedada, G.; Bellander, T.; Hennig, F.; et al. Two-way effect modifications of air pollution and air temperature on total natural and cardiovascular mortality in eight European urban areas. Environ. Int. 2018, 116, 186–196. [Google Scholar] [CrossRef]
- Ballester, J.; Robine, J.-M.; Herrmann, F.R.; Rodó, X. Long-term projections and acclimatization scenarios of temperature-related mortality in Europe. Nat. Commun. 2011, 2, 358. [Google Scholar] [CrossRef]
- Vicedo-Cabrera, A.M.; Guo, Y.; Sera, F.; Huber, V.; Schleussner, C.-F.; Mitchell, D.; Tong, S.; de Sousa Zanotti Stagliorio Coelho, M.; Saldiva, P.H.N.; Lavigne, E.; et al. Temperature-related mortality impacts under and beyond Paris Agreement climate change scenarios. Clim. Change 2018, 150, 391–402. [Google Scholar] [CrossRef]
- Jaagus, J.; Briede, A.; Rimkus, E.; Remm, K. Variability and trends in daily minimum and maximum temperatures and in the diurnal temperature range in Lithuania, Latvia and Estonia in 1951–2010. Theor. Appl. Climatol. 2014, 118, 57–68. [Google Scholar] [CrossRef]
- Conlon, K.C.; Rajkovich, N.B.; White-Newsome, J.L.; Larsen, L.; O’Neill, M.S. Preventing cold-related morbidity and mortality in a changing climate. Maturitas 2011, 69, 197–202. [Google Scholar] [CrossRef]
- Arbuthnott, K.; Hajat, S.; Heaviside, C.; Vardoulakis, S. What is cold-related mortality? A multi-disciplinary perspective to inform climate change impact assessments. Environ. Int. 2018, 121, 119–129. [Google Scholar]
| Min | 2.5th Percentile | 5th Percentile | Median | Mean | SD * | 95th Percentile | Max | |
|---|---|---|---|---|---|---|---|---|
| Tallinn | −29.4 | −18.3 | −15.7 | −2.6 | −4.0 | 6.1 | 4.3 | 9.6 |
| Riga | −24.4 | −16.5 | −14.3 | −0.4 | −2.1 | 6.1 | 6 | 8.8 |
| Cause of Mortality or Age Group | Average Size of Population during the Years | Number of Deaths or People in Age Group during the Whole Study Period | Annual Winter Mortality Rate (per 1000 Inhabitants) | Daily Number of Deaths | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD * | Median | Min | Max | ||||
| Tallinn | ||||||||
| Total | 402,250 | 36,645 | 4.8 | 12.8 | 4.1 | 12 | 2 | 29 |
| Cardiovascular | 18,941 | 2.5 | 6.6 | 2.7 | 6 | 0 | 20 | |
| Respiratory | 1180 | 0.2 | 0.4 | 0.6 | 0 | 0 | 5 | |
| External | 3096 | 0.4 | 1.1 | 1.2 | 1 | 0 | 8 | |
| 0–74 | 18,320 | 2.6 | 6.4 | 2.7 | 6 | 0 | 19 | |
| 75+ | 18,325 | 45.7 | 6.4 | 2.9 | 6 | 0 | 24 | |
| Riga | ||||||||
| Total | 656,877 | 27,495 | 6.0 | 26.0 | 5.5 | 26 | 10 | 79 |
| Cardiovascular | 15,090 | 3.3 | 14.3 | 3.9 | 14 | 3 | 28 | |
| Respiratory | 800 | 0.2 | 0.8 | 0.9 | 1 | 0 | 7 | |
| External | 1673 | 0.4 | 1.6 | 2.1 | 1 | 0 | 54 | |
| 0–74 | 13,332 | 3.2 | 12.6 | 3.9 | 12 | 3 | 65 | |
| 75+ | 14,163 | 35.1 | 13.4 | 3.8 | 13 | 3 | 26 | |
| Tallinn | Riga | |||
|---|---|---|---|---|
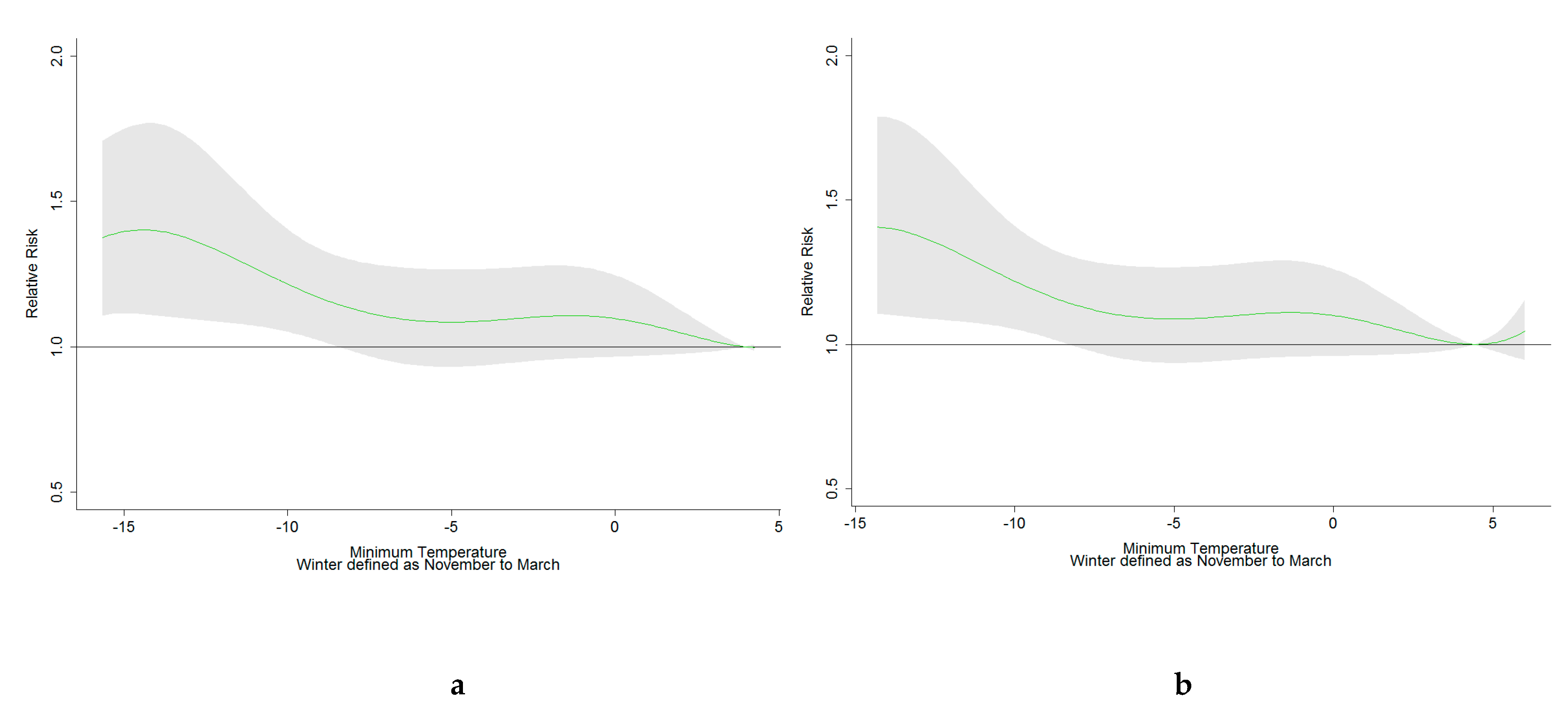
| Cause of Mortality or Age Group | RR * (95% CI) | MMT (°C) | RR (95% CI) | MMT (°C) |
| Total | 1.28 (1.01–1.62) | 4.0 | 1.41 (1.11–1.79) | 4.4 |
| Cardiovascular | 1.83 (1.31–2.55) | 4.3 | 1.13 (0.86–1.49) | −0.9 |
| Respiratory | 2.50 (0.79–7.86) | 3.3 | 1.37 (0.74–2.54) | −11.5 |
| External causes | 1.38 (0.63–3.02) | −1.0 | 1.96 (0.77–4.96) | 3.2 |
| 0–74 | 1.08 (0.79–1.47) | 2.7 | 1.58 (1.12–2.22) | 4.5 |
| 75+ | 1.64 (1.17–2.31) | 4.3 | 1.25 (0.90–1.73) | 4.3 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Åström, D.O.; Veber, T.; Martinsone, Ž.; Kaļužnaja, D.; Indermitte, E.; Oudin, A.; Orru, H. Mortality Related to Cold Temperatures in Two Capitals of the Baltics: Tallinn and Riga. Medicina 2019, 55, 429. https://doi.org/10.3390/medicina55080429
Åström DO, Veber T, Martinsone Ž, Kaļužnaja D, Indermitte E, Oudin A, Orru H. Mortality Related to Cold Temperatures in Two Capitals of the Baltics: Tallinn and Riga. Medicina. 2019; 55(8):429. https://doi.org/10.3390/medicina55080429
Chicago/Turabian StyleÅström, Daniel Oudin, Triin Veber, Žanna Martinsone, Darja Kaļužnaja, Ene Indermitte, Anna Oudin, and Hans Orru. 2019. "Mortality Related to Cold Temperatures in Two Capitals of the Baltics: Tallinn and Riga" Medicina 55, no. 8: 429. https://doi.org/10.3390/medicina55080429
APA StyleÅström, D. O., Veber, T., Martinsone, Ž., Kaļužnaja, D., Indermitte, E., Oudin, A., & Orru, H. (2019). Mortality Related to Cold Temperatures in Two Capitals of the Baltics: Tallinn and Riga. Medicina, 55(8), 429. https://doi.org/10.3390/medicina55080429





