Long-Term Survival after Acute Myocardial Infarction in Lithuania during Transitional Period (1996–2015): Data from Population-Based Kaunas Ischemic Heart Disease Register
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Sample
2.2. Ascertainment of Outcome Events
2.3. Statistical Analysis
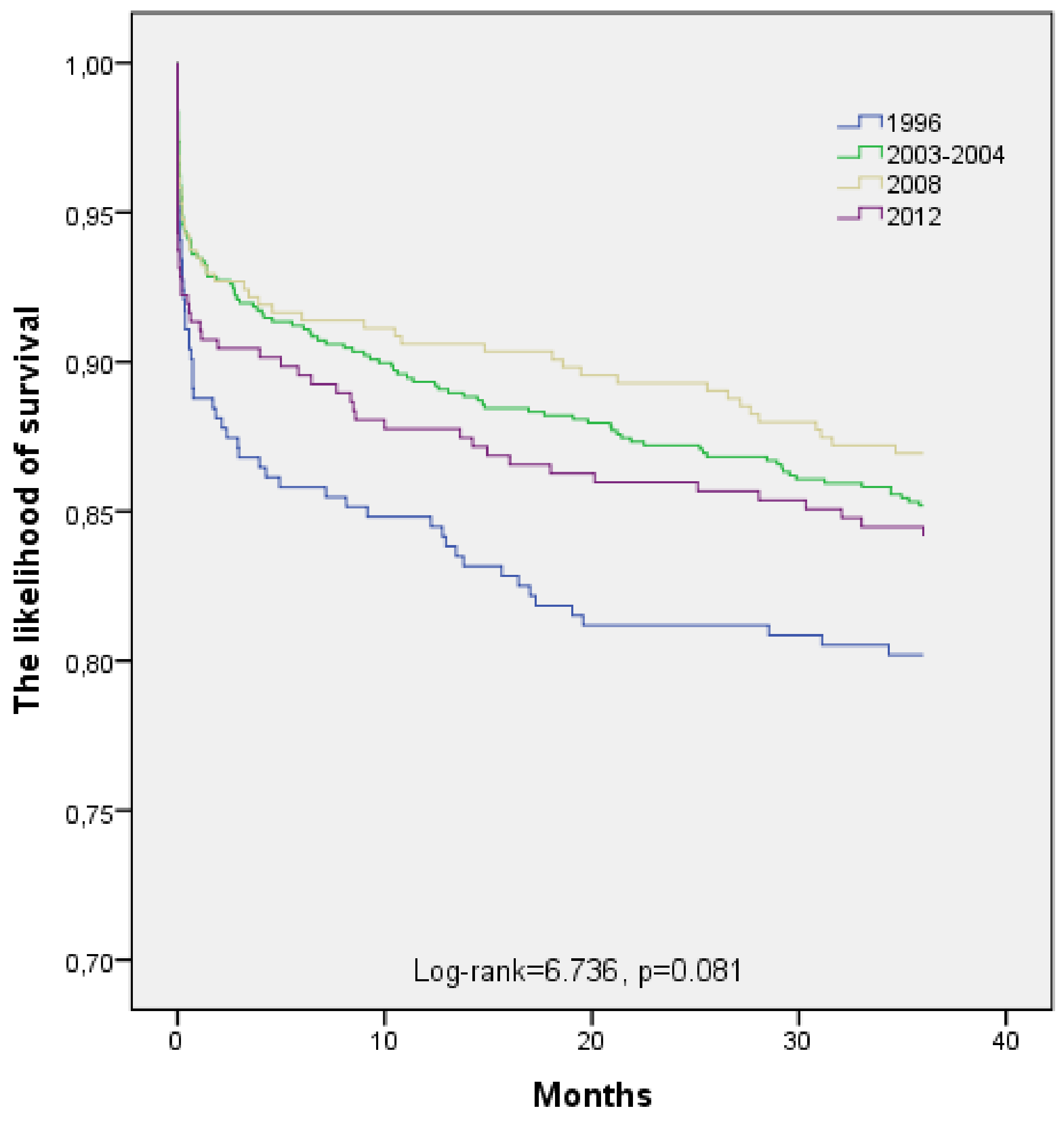
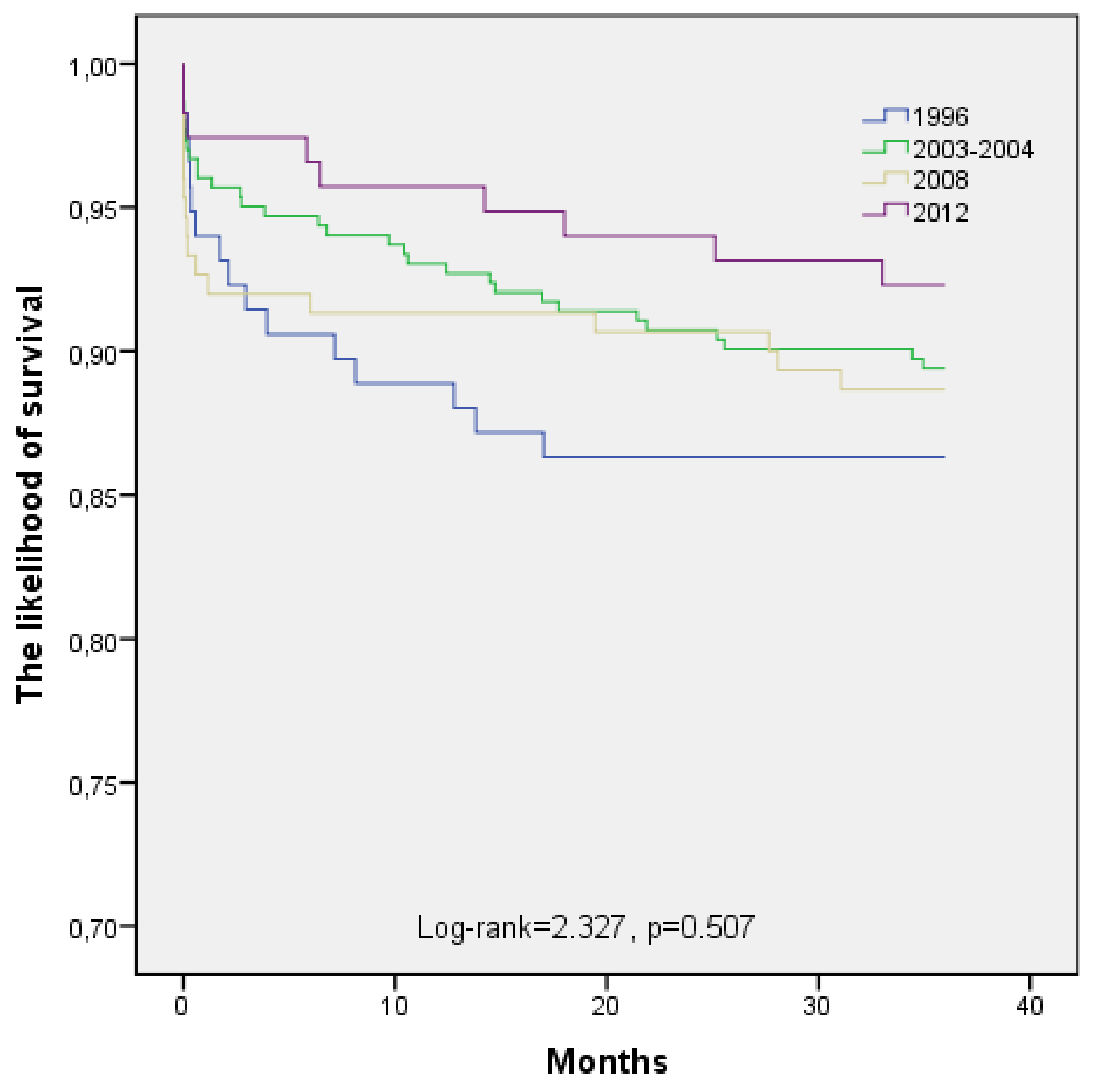
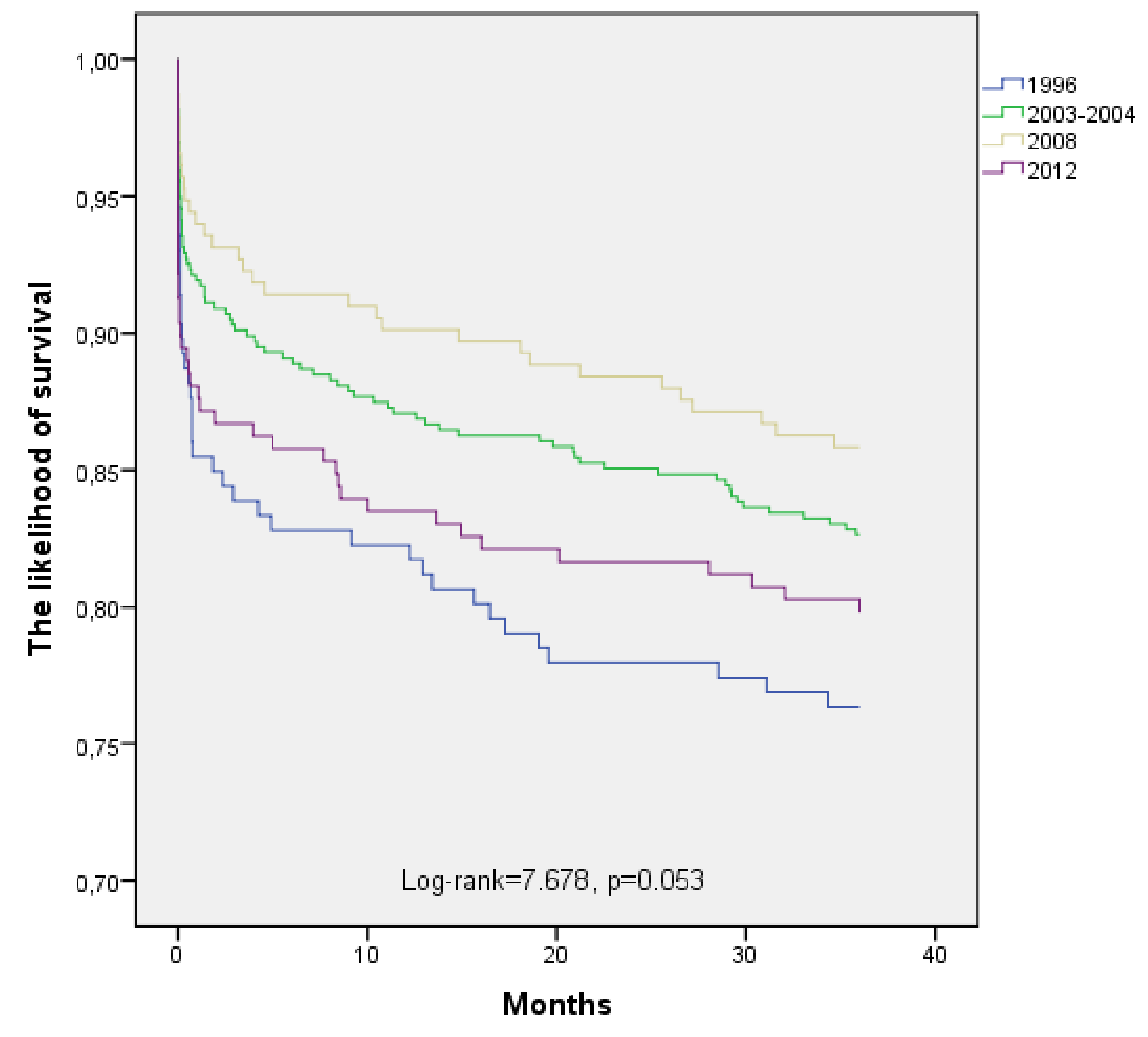
3. Results
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Causes of Death Statistics, Eurostat 5/2014. Available online: http://ec.europa.eu/eurostat/statistics-explained/index.php/Causes_of_death_statistics# (accessed on 15 October 2015).
- Moran, A.E.; Forouzanfar, M.H.; Roth, G.A.; Mensah, G.A.; Ezzati, M.; Flaxman, A.; Murray, C.J.; Naghavi, M. The global burden of ischemic heart disease in 1990 and 2010: The Global Burden of Disease 2010 study. Circulation 2014, 129, 1493–1501. [Google Scholar] [CrossRef] [PubMed]
- Nichols, M.; Townsend, N.; Scarborough, P.; Rayner, M. Trends in age-specific coronary heart disease mortality in the European Union over three decades: 1980–2009. Eur. Heart J. 2013, 34, 3017–3027. [Google Scholar] [CrossRef]
- Smolina, K.; Wright, L.; Rayner, M.; Goldcare, M. Determinants of the decline in mortality from acute myocardial infarction in England between 2002 and 2012: Linked national database study. BMJ 2012, 344, d8059. [Google Scholar] [CrossRef] [PubMed]
- Bjork, L.; Capewell, S.; O’Flaherty, M.; Lappas, G.; Bennett, K.; Rosengren, A. Decline in coronary mortality in Sweden between 1986 and 2002: Comparing contributions from primary and secondary prevention. PLoS ONE 2015, 10, e0124769. [Google Scholar] [CrossRef]
- Bucholz, E.M.; Butala, N.M.; Rathore, S.S.; Dreyer, R.P.; Lansky, A.J.; Krumholz, H.M. Sex differences in long-term mortality after myocardial infarction: A systematic review. Circulation 2014, 130, 757–767. [Google Scholar] [CrossRef] [PubMed]
- Nedkoff, L.; Atkins, E.; Knuiman, M.; Sanfilippo, F.M.; Rankin, J.; Hung, J. Age-specific gender differences in long-term recurrence and mortality following incident myocardial infarction: A population-based study. Heart Lung Circ. 2015, 24, 442–449. [Google Scholar] [CrossRef] [PubMed]
- Roffi, M.; Patrono, C.; Collet, J.P.; Mueller, C.; Valgimigli, M.; Andreotti, F.; Bax, J.J.; Borger, M.A.; Brotons, C.; Chew, D.P.; et al. ESC Scientific Document Group. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2016, 37, 267–315. [Google Scholar] [CrossRef] [PubMed]
- Lukšienė, D.; Milvidaitė, I.; Slapikas, R.; Jaruševičius, G.; Siudikas, A.; Venclovienė, J.; Zaliūnas, R. The impact of myocardial revascularization after acute coronary syndromes on one-year cardiovascular mortality. Medicina (Kaunas) 2011, 47, 305–312. [Google Scholar] [CrossRef]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. ESC Scientific Document Group. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2018, 39, 119–177. [Google Scholar] [CrossRef]
- Brković, E.; Novak, K.; Puljak, L. Pain-to-hospital times, cardiovascular risk factors, and early intrahospital mortality in patients with acute myocardial infarction. Ther. Clin. Risk Manag. 2015, 11, 209–216. [Google Scholar] [CrossRef][Green Version]
- Sugiyama, T.; Hasegawa, K.; Kobayashi, Y.; Takahashi, O.; Fukui, T.; Tsugawa, Y. Differential time trends of Outcomes and Costs of Care for Acute Myocardial Infarction Hospitalizations by ST Elevation and Type of Intervention in the United States. 2001–2011. J. Am. Heart Assoc. 2015, 4, e001445. [Google Scholar] [CrossRef] [PubMed]
- Blöndal, M.; Ainla, T.; Marandi, T.; Baburin, A.; Eha, J. Changes in treatment and mortality of acute myocardial infarction in Estonian tertiary and secondary care hospitals in 2001 and 2007. BMC Res. Notes 2012, 5, 71. [Google Scholar] [CrossRef] [PubMed]
- Blöndal, M.; Ainla, T.; Marandi, T.; Baburin, A.; Rahu, M.; Eha, J. Better outcomes for acute myocardial infarction patients first admitted to PCI hospitals in Estonia. Acta Cardiol. 2010, 65, 541–548. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.Y.; Gore, J.M.; Lapane, K.L.; Yarzebski, J.; Person, S.D.; Gurwitz, J.H.; Kiefe, C.I.; Goldberg, R.J. A 35-Year Perspective (1975 to 2009) into the Long-Term Prognosis and Hospital Management of Patients Discharged from the Hospital After a First Acute Myocardial Infarction. Am. J. Cardiol. 2015, 116, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Saar, A.; Marandi, T.; Ainla, T.; Fischer, K.; Blondal, M.; Eha, J. Improved treatment and prognosis after acute myocardial infarction in Estonia: Cross-sectional study from a high risk country. BMC Cardiovasc. Disord. 2015, 15, 136. [Google Scholar] [CrossRef] [PubMed]
- Erglis, A.; Mintale, I.; Latkovskis, G.; Balode, I.; Jegere, S.; Bajare, I.; Rozenbergs, A.; Greenlaw, N.; Ferrari, R.; Steg, P.G. Management of coronary artery disease patients in Latvia compared with practice in Central-Eastern Europe and globally: Analysis of the CLARIFY registry. Medicina (Kaunas) 2015, 51, 240–246. [Google Scholar] [CrossRef][Green Version]
- Bernotiene, G.; Radisauskas, R.; Tamosiunas, A.; Milasauskiene, Z. Trends in out-of-hospital ischemic heart disease mortality for the 25–64 year old population of Kaunas, Lithuania, based on data from the 1988-2012 Ischemic Heart Disease Registry. Scand. J. Public Health 2015, 43, 648–656. [Google Scholar] [CrossRef]
- Smith, F.G.; Brogan, R.A.; Alabas, O.; Laut, K.G.; Quinn, T.; Bugiardini, R.; Gale, C.P. Comparative care and outcomes for acute coronary syndromes in Central and Eastern European Transitional countries: A review of the literature. Eur. Heart J. Acute Cardiovasc. Care 2015, 4, 537–554. [Google Scholar] [CrossRef]
- World Health Organization MONICA Project. MONICA Manual; World Health Organization MONICA Project: Geneva, Switzerland, 1990. [Google Scholar]
- Radisauskas, R.; Rastenyte, D.; Bernotiene, G.; Sopagiene, D.; Jancaityte, L. Morbidity and mortality from the major cardiovascular diseases in Kaunas population from 1983 to 2002. Medicina (Kaunas) 2003, 39, 1208–1214. [Google Scholar]
- Bangalore, S.; Toklu, B.; Amoroso, N.; Fusaro, M.; Kumar, S.; Hannan, E.L.; Faxon, D.P.; Feit, F. Bare metal stents, durable polymer drug eluting stents, and biodegradable polymer drug eluting stents for coronary artery disease: Mixed treatment comparison meta-analysis. BMJ 2013, 347, f6625. [Google Scholar] [CrossRef]
- Hubacek, J.A.; Stanek, V.; Gebauerova, M.; Adamkova, V.; Lesauskaite, V.; Zaliaduonyte-Peksiene, D.; Tamosiunas, A.; Supiyev, A.; Kossumov, A.; Zhumadilova, A.; et al. Traditional risk factors of acute coronary syndrome in four different male population–total cholesterol values does not seem to be relevant risk factor. Physiol. Res. 2017, 66 (Suppl. 1), S121–S128. [Google Scholar]
- Miller, B.R.; Nguyen, H.; Hu, C.J.; Lin, C.; Nguyen, Q.T. New and emerging drugs and targets for type 2 diabetes: Reviewing the evidence. Am. Health Drug Benefits 2014, 7, 452–463. [Google Scholar] [PubMed]
- Kotseva, K.; Wood, D.; De Backer, G.; De Bacquer, D.; Pyorala, K.; Keil, U.; EUROASPIRE Study Group. Cardiovascular prevention guidelines in daily practice: A comparison of EUROASPIRE I, II, and III surveys in eight European countries. Lancet 2009, 373, 929–940. [Google Scholar] [CrossRef]
- Wood, D.A.; Kotseva, K.; Connolly, S.; Jennings, C.; Mead, A.; Jones, J.; Holden, A.; De Bacquer, D.; Collier, T.; De Backer, G.; et al. Nurse-coordinated multidisciplinary, family-based cardiovascular disease prevention programme (EUROACTION) for patients with coronary heart disease and asymptomatic individuals at high risk of cardiovascular disease: A paired, cluster-randomised controlled trial. Lancet 2008, 371, 1999–2012. [Google Scholar] [CrossRef] [PubMed]
- Urbinati, S.; Olivari, Z.; Gonzini, L.; Savonitto, S.; Farina, R.; Del Pinto, M.; Valbusa, A.; Fantini, G.; Mazzoni, A.; Maggioni, A.P. BLITZ-4 Investigators. Secondary prevention after acute myocardial infarction: Drug adherence, treatment goals, and predictors of health lifestyle habits. The BLITZ-4 Registry. Eur. J. Prev. Cardiol. 2015, 22, 1548–1556. [Google Scholar] [CrossRef] [PubMed]
- Dziewierz, A.; Siudak, Z.; Dykla, D.; Rakowski, T.; Mielecki, W.; Dubiel, J.S.; Dudek, D. Management and mortality in patients with non-ST-segment elevation vs. ST-segment elevation myocardial infarction. Data from the Malopolska Registry of Acute Coronary Syndromes. Kardiol. Pol. 2009, 67, 115–120. [Google Scholar] [PubMed]
- McManus, D.D.; Gore, J.; Yarzebski, J.; Spencer, F.; Lessard, D.; Goldberg, R.J. Recent trends in the incidence, treatment, and outcomes of patients with STEMI and NSTEMI. Am. J. Med. 2011, 124, 40–47. [Google Scholar] [CrossRef]
- Alnasser, S.M.; Huang, W.; Gore, J.M.; Steg, P.G.; Eagle, P.A.; Anderson, F.A., Jr.; Fox, K.A.; Gurfinkel, E.; Brieger, D.; Klein, W.; et al. Late Consequences of Acute Coronary Syndromes: Global Registry of Acute Coronary Events (GRACE) Follow-up. Am. J. Med. 2015, 128, 766–775. [Google Scholar] [CrossRef]
- Sinnaeve, P.R.; Zeymer, U.; Bueno, H.; Danchin, N.; Medina, J.; Sánchez-Covisa, J.; Licour, M.; Annemans, L.; Jukema, J.W.; Pocock, S.; et al. Contemporary inter-hospital transfer patterns for the management of acute coronary syndrome patients: Findings from the EPICOR study. Eur. Heart J. Acute Cardiovasc. Care 2015, 4, 254–262. [Google Scholar] [CrossRef]
- Becerra, V.; Gracia, A.; Desai, K.; Abogunrin, S.; Brand, S.; Chapman, R.; Garcia Alonso, F.; Fuster, V.; Sanz, G. Cost-effectiveness and public health benefit of secondary cardiovascular disease prevention from improved adherence using a polypill in the UK. BMJ Open 2015, 5, e007111. [Google Scholar] [CrossRef]
- Rodriguez, F.; Cannon, C.P.; Steg, P.G.; Kumbhani, D.J.; Goto, S.; Smith, S.C.; Eagle, K.A.; Ohman, E.M.; Umez-Eronini, A.A.; Hoffman, E.; et al. REACH Registry Investigators. Predictors of long-term adherence to evidence-based cardiovascular disease medications in outpatients with stable atherothrombotic disease: Findings from the REACH Registry. Clin. Cardiol. 2013, 36, 721–727. [Google Scholar] [CrossRef] [PubMed]
- Puymirat, E.; Battler, A.; Birkhead, J.; Bueno, H.; Clemmensen, P.; Cottin, Y.; Fox, K.A.; Gorenek, B.; Hamm, C.; Huber, K.; et al. Euro Heart Survey 2009 Snapshot: Regional variations in presentation and management of patients with AMI in 47 countries. Eur. Heart J. Acute Cardiovasc. Care 2013, 2, 359–370. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, S.D.; Laut, K.G.; Fajadet, J.; Kaifoszova, Z.; Kala, P.; Di Mario, C.; Wijns, W.; Clemmensen, P.; Agladze, V.; Antoniades, L.; et al. Reperfusion therapy for ST elevation acute myocardial infarction 2010/2011: Current status in 37 ESC countries. Eur. Heart J. 2014, 35, 1957–1970. [Google Scholar] [CrossRef] [PubMed]
- Huber, K.; Gersh, B.J.; Goldstein, P.; Granger, C.B.; Armstrong, P.W. The organization, function, and outcomes of ST-elevation myocardial infarction networks worldwide: Current state, unmet needs and future directions. Eur. Heart J. 2014, 35, 1526–1532. [Google Scholar] [CrossRef] [PubMed]
- Thim, T.; Johansen, M.B.; Chisholm, G.E.; Schmidt, M.; Kaltoft, A.; Sørensen, H.T.; Thuesen, L.; Kristensen, S.D.; Botker, H.E.; Krusell, L.R.; et al. Clopidogrel discontinuation within the first year after coronary drug-eluting stent implantation: An observational study. BMC Cardiovasc. Disord. 2014, 14, 100. [Google Scholar] [CrossRef] [PubMed]
- Ho, P.M.; Spertus, J.A.; Masoudi, F.A.; Reid, K.J.; Peterson, E.D.; Magid, D.J.; Krumholz, H.M.; Rumsfeld, J.S. Impact of medication therapy discontinuation on mortality after myocardial infarction. Arch. Intern. Med. 2006, 166, 1842–1847. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.Y.; Cooke, C.E.; Robertson, T.A. Use of Secondary Prevention Drug Therapy in Patients with Acute Coronary Syndrome After Hospital Discharge. J. Manag. Care Pharm. 2008, 14, 271–280. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, E.; Subherwal, S.; Roe, M.T.; Holmes, D.N.; Thomas, L.; Alexander, K.P.; Wang, T.Y.; Peterson, E.D. Do patients treated at academic hospitals have better longitudinal outcomes after admission for non-ST-elevation myocardial infarction? Am. Heart J. 2014, 167, 762–769. [Google Scholar] [CrossRef] [PubMed]
- McNamara, R.L.; Chung, S.C.; Jernberg, T.; Holmes, D.; Roe, M.; Timmis, A.; James, S.; Deanfield, J.; Fonarow, G.C.; Peterson, E.D.; et al. International comparisons of the management of patients with non-ST segment elevation acute myocardial infarction in the United Kingdom, Sweden, and the United States: The MINAP/NICOR, SWEDEHEART/RIKS-HIA, and ACTION Registry-GWTG/NCDR registries. Int. J. Cardiol. 2014, 175, 240–247. [Google Scholar] [CrossRef]
- Campo, G.; Saia, F.; Guastaroba, P.; Marchesini, J.; Varani, E.; Manari, A.; Ottani, F.; Tondi, S.; De Palma, R.; Marzocchi, A. Prognostic impact of hospital readmissions after primary percutaneous coronary intervention. Arch. Intern. Med. 2011, 171, 1948–1949. [Google Scholar] [CrossRef]
- Moretti, C.; D’Ascenzo, F.; Omedè, P.; Sciuto, F.; Presutti, D.G.; Di Cuia, M.; Colaci, C.; Giusto, F.; Ballocca, F.; Cerrato, E.; et al. Thirty-day readmission rates after PCI in a metropolitan center in Europe: Incidence and impact on prognosis. J. Cardiovasc. Med. (Hagerstown) 2015, 16, 238–245. [Google Scholar] [CrossRef] [PubMed]
- Marandi, T.; Baburin, A.; Ainla, T. Use of evidence-based pharmacotherapy after myocardial infarction in Estonia. BMC Public Health 2010, 10, 358. [Google Scholar] [CrossRef] [PubMed]
- Jernberg, T.; Johanson, P.; Held, C.; Svennblad, B.; Lindback, J.; Wallentin, L.; SWEDEHEART/RIKS-HIA. Association between adoption of evidence-based treatment and survival for patients with ST-elevation myocardial infarction. JAMA 2011, 305, 1677–1684. [Google Scholar] [CrossRef] [PubMed]
- Krumholz, H.M.; Wang, Y.; Chen, J.; Drye, E.E.; Spertus, J.A.; Ross, J.S.; Curtis, J.P.; Nallamothu, B.K.; Lichtman, J.H.; Havranek, E.P.; et al. Reduction in acute myocardial infarction mortality in the United States: Risk-standardized mortality rates from 1995–2006. JAMA 2009, 302, 767–773. [Google Scholar] [CrossRef] [PubMed]
- Keyhani, S.; Scobie, J.V.; Hebert, P.L.; McLaughlin, M.A. Gender disparities in blood pressure control and cardiovascular care in a national sample of ambulatory care visits. Hypertension 2008, 51, 1149–1155. [Google Scholar] [CrossRef]
- Cohen-Mansfield, J. Smoking and mortality among persons aged 75–94. Prev. Med. 2013, 56, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Berg, J.; Björck, L.; Nielsen, S.; Lappas, G.; Rosengren, A. Sex differences in survival after myocardial infarction in Sweden, 1987–2010. Heart 2017, 103, 1625–1630. [Google Scholar] [CrossRef]
- Kvakkestad, K.M.; Wang Fagerland, M.; Eritsland, J.; Halvorsen, S. Gender differences in all-cause, cardiovascular and cancer mortality during long-term follow-up after acute myocardial infarction; a prospective cohort study. BMC Cardiovasc. Disord. 2017, 17, 75. [Google Scholar] [CrossRef]
| Variables | 1996 | 2003–2004 | 2008 | 2012 | p for Trend |
|---|---|---|---|---|---|
| N = 303 | N = 797 | N = 383 | N = 335 | ||
| Mean age (SD) | 55.3 (7.3) | 55.0 (7.4) | 55.6 (6.9) | 56.0 (6.4) | 0.26 |
| Men, % | 77.2 * | 72.8 | 69.2 | 73.7 | 0.37 |
| 55–64 years, % | 61.4 | 62.1 | 60.8 | 65.1 | 0.41 |
| Clinical diagnosis | |||||
| AMI | 75.6 * | 60.0 | 54.6 | 61.2 | 0.23 |
| Unstable AP | 19.1 * | 38.8 | 42.8 | 34.3 | 0.25 |
| EDC | |||||
| Definite AMI | 45.9 o | 47.7 | 51.7 | 55.8 | 0.04 |
| Possible AMI | 53.1 o | 51.7 | 47.0 | 39.4 | 0.1 |
| STEMI, % | 39.6 | 37.3 | 33.4 | 37.3 | 0.4 |
| AH, % | 65.7 * | 71.0 | 80.2 | 83.0 | 0.02 |
| Stroke, % | 4.3 | 3.6 | 2.6 | 4.5 | 0.81 |
| Diabetes, % | 9.6 @ | 14.4 | 13.8 | 17.0 | 0.07 |
| Previous AMI, % | 27.1 | 25.6 | 22.7 | 22.4 | 0.03 |
| Previous Acute heart failure, % | 10.2 * | 6.8 | 6.0 | 6.3 | 0.1 |
| Smoking, % | 39.6 o | 37.3 | 38.9 | 30.1 | 0.26 |
| Overweight, % | 66.3 | 60.6 # | 67.6 | 63.9 | 0.95 |
| Hospital bed-days, mean, (SD) | 15.1 (9.4) & | 11.2 (7.0) | 8.9 (5.5) | 8.0 (6.1) | 0.004 |
| Variables/Age Group (Years) | 1996 | 2003–2004 | 2008 | 2012 | p for Trend |
|---|---|---|---|---|---|
| N = 303 | N = 797 | N = 383 | N = 335 | ||
| Clinical diagnosis | |||||
| AMI | |||||
| 25–54 | 82.1 * | 62.9 | 60.7 | 64.1 | 0.19 |
| 55–64 | 71.5 * | 58.2 | 50.6 | 59.6 | 0.29 |
| Unstable AP | |||||
| 25–54 | 13.7 * | 36.1 | 36.7 | 34.2 | 0.18 |
| 55–64 | 22.6 * | 40.4 | 46.8 | 34.4 | 0.32 |
| EDC | |||||
| Definite AMI | |||||
| 25–54 | 43.6 * | 49.7 | 54.7 | 57.3 | 0.004 |
| 55–64 | 47.3 | 46.5 | 49.8 | 55 | 0.17 |
| Possible AMI | |||||
| 25–54 | 56.4 * | 50.3 | 43.3 | 41 | 0.009 |
| 55–64 | 51.1 @ | 52.5 | 49.4 | 38.5 | 0.25 |
| STEMI, % | |||||
| 25–54 | 37.6 | 38.7 | 38.7 | 35.9 | 0.6 |
| 55–64 | 40.9 * | 36.4 | 30 | 38.1 | 0.52 |
| AH, % | |||||
| 25–54 | 69.2 * | 69.5 | 78 | 85.5 | 0.09 |
| 55–64 | 63.4 * | 71.9 | 81.5 | 81.7 | 0.03 |
| Stroke, % | |||||
| 25–54 | 1.7 | 2.6# | 0.7 | 2.6 | 0.96 |
| 55–64 | 5.9 | 4.2 | 3.9 | 5.5 | 0.7 |
| Diabetes, % | |||||
| 25–54 | 3.4 *o | 9.3 | 10.2 | 13.9 | 0.049 |
| 55–64 | 13.7 | 17.8 | 16.5 | 20 | 0.12 |
| Previous AMI, % | |||||
| 25–54 | 21.4 * | 16.2 | 16 | 14.5 | 0.05 |
| 55–64 | 30.6 | 31.3 | 27 | 26.6 | 0.16 |
| Previous acute heart failure, % | |||||
| 25–54 | 6.8 | 6.3 | 4 | 3.4 | 0.06 |
| 55–64 | 12.4 o | 7.1 | 7.3 | 7.8 | 0.24 |
| Smoking, % | |||||
| 25–54 | 56.4 * | 52 | 48 | 40.2 | 0.05 |
| 55–64 | 29 | 28.3 | 33 | 24.8 | 0.72 |
| Overweight, % | |||||
| 25–54 | 62.4 | 60.3 # | 68.7 | 69.2 | 0.21 |
| 55–64 | 68.8 o | 60.8 | 67 | 61 | 0.44 |
| Hospital bed-days, mean, (SD) | |||||
| 25–54 | 14.1 (5.9) * | 10.6 (6.6) | 8.3 (4.9) | 8.1 (6.4) | 0.02 |
| 55–64 | 15.8 (10.9) * | 11.3 (7.2) | 9.2 (5.7) | 8.0 (6.0) | 0.002 |
| Sex and Age Groups | Study Year | Total N | N of Death | Survived | Means of Survival Time in Months | |||
|---|---|---|---|---|---|---|---|---|
| Estimate | 95% CI | |||||||
| N | % | Lower | Upper | |||||
| Men | 1996 | 234 | 47 | 187 | 79.9 | 29.9 | 28.5 | 31.4 |
| 2003–2004 | 580 | 91 | 489 | 84.3 | 31.9 | 31.2 | 32.6 | |
| 2008 | 265 | 39 | 226 | 85.3 | 32.4 | 31.4 | 33.4 | |
| 2012 | 247 | 43 | 204 | 82.6 | 30.9 | 29.4 | 32.4 | |
| Overall | 1326 | 220 | 1106 | 83.4 | 31.2 | 30.6 | 31.8 | |
| Women | 1996 | 69 | 13 | 56 | 81.2 | 30.7 | 27.8 | 33.5 |
| 2003–2004 | 217 | 27 | 190 | 87.6 | 32.6 | 31.3 | 33.9 | |
| 2008 | 118 | 11 | 107 | 90.7 | 33.6 | 32.1 | 35.2 | |
| 2012 | 88 | 10 | 78 | 88.6 | 32.5 | 30.4 | 34.7 | |
| Overall | 492 | 61 | 431 | 87.6 | 32.6 | 31.7 | 33.5 | |
| 25–54 Years | 1996 | 117 | 16 | 101 | 86.3 | 31.7 | 29.7 | 33.7 |
| 2003–2004 | 302 | 32 | 270 | 89.4 | 33.2 | 32.2 | 34.2 | |
| 2008 | 150 | 17 | 133 | 88.7 | 32.7 | 31.1 | 34.3 | |
| 2012 | 117 | 9 | 108 | 92.3 | 34.1 | 32.8 | 35.4 | |
| Overall | 686 | 74 | 612 | 89.2 | 33.0 | 32.3 | 33.7 | |
| 55–64 Years | 1996 | 186 | 44 | 142 | 76.3 | 28.8 | 26.9 | 30.8 |
| 2003–2004 | 495 | 86 | 409 | 82.6 | 31.1 | 30.2 | 32.1 | |
| 2008 | 233 | 33 | 200 | 85.8 | 32.2 | 30.9 | 33.5 | |
| 2012 | 218 | 44 | 174 | 79.8 | 29.9 | 28.1 | 31.6 | |
| Overall | 1132 | 207 | 925 | 81.7 | 30.7 | 30.0 | 31.4 | |
| Total | 1996 | 303 | 60 | 243 | 80.2 | 29.9 | 28.5 | 31.4 |
| 2003–2004 | 797 | 118 | 679 | 85.2 | 31.9 | 31.2 | 32.6 | |
| 2008 | 383 | 50 | 333 | 86.9 | 32.4 | 31.4 | 33.4 | |
| 2012 | 335 | 53 | 282 | 84.2 | 31.4 | 30.1 | 32.6 | |
| Overall | 1818 | 281 | 1537 | 84.5 | 31.6 | 31.1 | 32.1 | |
| Mortality | Sex | Age Group (Years) | ||
|---|---|---|---|---|
| Men | Women | 25–54 | 55–64 | |
| HR (95% CI) | ||||
| 1996 | 1 | 1 | 1 | 1 |
| 2003–2004 | 0.754 (0.53–1.072) | 0.631 (0.325–1.222) | 0.756 (0.415–1.377) | 0.70 (0.487–1.007) |
| 2008 | 0.707 (0.463–1.081) | 0.464 (0.208–1.037) | 0.824 (0.416–1.63) | 0.559 (0.356–0.878) |
| 2012 | 0.855 (0.565–1.293) | 0.584 (0.256–1.332) | 0.540 (0.239–1.222) | 0.845 (0.556–1.283) |
| p trend | 0.51 | 0.16 | 0.21 | 0.4 |
| Adjusted HR (95% CI) * | ||||
| 1996 | 1 | 1 | 1 | 1 |
| 2003–2004 | 0.762 (0.536–1.083) | 0.652 (0.336–1.264) | 0.765 (0.42–1.395) | 0.708 (0.493–1.019) |
| 2008 | 0.692 (0.453–1.058) | 0.486 (0.218–1.085) | 0.812 (0.41–1.607) | 0.554 (0.353–0.870) |
| 2012 | 0.833 (0.551–1.26) | 0.606 (0.266–1.384) | 0.520 (0.23–1.179) | 0.857 (0.564–1.302) |
| p trend | 0.4 | 0.18 | 0.17 | 0.4 |
| Adjusted HR (95% CI) ** | ||||
| 1996 | 1 | 1 | 1 | 1 |
| 2003–2004 | 1.067 (0.731–1.556) | 0.922 (0.468–1.817) | 1.220 (0.623–2.392) | 0.961 (0.657–1.406) |
| 2008 | 0.968 (0.621–1.507) | 0.606 (0.266–1.384) | 0.988 (0.463–2.109) | 0.798 (0.501–1.270) |
| 2012 | 0.868 (0.550–1.371) | 0.732 (0.314–1.709) | 0.647 (0.261–1.601) | 0.891 (0.570–1.393) |
| p trend | 0.41 | 0.28 | 0.31 | 0.44 |
| Adjusted HR (95% CI) *** | ||||
| 1996 | 1 | 1 | ||
| 2003–2004 | 1.329 (0.858–2.058) | 1.193 (0.513–2.775) | ||
| 2008 | 1.241 (0.737–2.089) | 1.211 (0.388–3.784) | ||
| 2012 | 1.219 (0.690–2.153) | 1.088 (0.342–3.461) | ||
| p trend | 0.62 | 0.90 | ||
| Adjusted HR (95% CI) **** | ||||
| 1996 | 1 | 1 | ||
| 2003–2004 | 1.176 (0.536–2.578) | 1.403 (0.904–2.178) | ||
| 2008 | 1.796 (0.735–4.391) | 1.203 (0.693–2.089) | ||
| 2012 | 0.894 (0.312–2.561) | 1.350 (0.760–2.399) | ||
| p trend | 0.82 | 0.47 | ||
| Variables | B | HR | 95% CI | p | |
|---|---|---|---|---|---|
| Men | |||||
| Time-year period (every 1 period) | 0.043 | 1.044 | 0.881 | 1.237 | 0.619 |
| Age (every 1 year) | 0.028 | 1.028 | 1.003 | 1.055 | 0.029 |
| AMI (ref.) | 1 | ||||
| Unstable AP | −0.391 | 0.676 | 0.394 | 1.162 | 0.156 |
| Definite AMI (ref.) | 1 | ||||
| Possible AMI | −0.186 | 0.830 | 0.528 | 1.306 | 0.420 |
| STEMI (ref. no) | 0.222 | 1.249 | 0.827 | 1.886 | 0.292 |
| Previous acute heart failure (ref. no) | 1.833 | 6.255 | 4.335 | 9.024 | 0.0001 |
| Previous AMI (ref. no) | 0.408 | 1.503 | 1.070 | 2.113 | 0.019 |
| AH (ref. no) | −0.176 | 0.838 | 0.589 | 1.194 | 0.329 |
| Stroke (ref. no) | 0.630 | 1.877 | 1.030 | 3.422 | 0.040 |
| Diabetes (ref. no) | 0.656 | 1.926 | 1.296 | 2.864 | 0.001 |
| Normal weight (ref.) | 1 | ||||
| Overweight | −0.399 | 0.671 | 0.473 | 0.953 | 0.026 |
| Obesity | 0.634 | 1.884 | 1.070 | 3.318 | 0.028 |
| Smoking (ref. never smokers) | 0.098 | 1.103 | 0.794 | 1.532 | 0.559 |
| Women | |||||
| Time-year period (every 1 period) | 0.024 | 1.024 | 0.714 | 1.469 | 0.896 |
| Age (every 1 year) | 0.056 | 1.057 | 0.990 | 1.129 | 0.095 |
| AMI (ref.) | 1 | ||||
| Unstable AP | −0.082 | 0.921 | 0.329 | 2.577 | 0.876 |
| Definite AMI (ref.) | 1 | ||||
| Possible AMI | 0.066 | 1.068 | 0.478 | 2.388 | 0.873 |
| STEMI (ref. no) | 0.978 | 2.660 | 1.086 | 6.513 | 0.032 |
| Previous acute heart failure (ref. no) | 2.215 | 9.166 | 4.217 | 19.923 | 0.0001 |
| Previous AMI (ref. no) | −0.044 | 0.957 | 0.455 | 2.011 | 0.908 |
| AH (ref. no) | −0.548 | 0.578 | 0.281 | 1.188 | 0.136 |
| Stroke (ref. no) | 1.602 | 4.964 | 1.843 | 13.374 | 0.002 |
| Diabetes (ref. no) | 1.354 | 3.873 | 1.961 | 7.648 | 0.0001 |
| Normal weight (ref.) | 1 | ||||
| Overweight | −0.769 | 0.464 | 0.235 | 0.913 | 0.026 |
| Obesity | −0.538 | 0.584 | 0.201 | 1.699 | 0.324 |
| Smoking (ref. no) | −1.357 | 0.257 | 0.034 | 1.950 | 0.189 |
| B | HR | 95% CI | p | ||
|---|---|---|---|---|---|
| 25–54 age group | |||||
| Time-year period (every 1 period) | 0.008 | 1.008 | 0.753 | 1.350 | 0.956 |
| Age (every 1 year) | 0.052 | 1.053 | 0.994 | 1.115 | 0.077 |
| Sex (ref. men) | −1.014 | 0.363 | 0.132 | 0.996 | 0.049 |
| AMI (ref.) | 1 | ||||
| Unstable AP | −0.087 | 0.916 | 0.350 | 2.396 | 0.859 |
| Definite AMI (ref.) | 1 | ||||
| Possible AMI | −0.491 | 0.612 | 0.265 | 1.409 | 0.248 |
| STEMI (ref. no) | −0.186 | 0.830 | 0.408 | 1.690 | 0.608 |
| Previous acute heart failure (ref. no) | 2.528 | 12.531 | 6.322 | 24.835 | 0.0001 |
| Previous AMI (ref. no) | 0.182 | 1.20 | 0.596 | 2.415 | 0.610 |
| AH (ref. no) | −0.133 | 0.875 | 0.480 | 1.597 | 0.664 |
| Stroke (ref. no) | 1.378 | 3.966 | 1.316 | 11.953 | 0.014 |
| Diabetes (ref. no) | 0.532 | 1.702 | 0.692 | 4.183 | 0.247 |
| Normal weight (ref.) | 1 | ||||
| Overweight | −0.606 | 0.546 | 0.298 | 1.000 | 0.050 |
| Obesity | 0.580 | 1.785 | 0.655 | 4.869 | 0.257 |
| Smoking (ref. no) | 0.084 | 1.088 | 0.582 | 2.035 | 0.792 |
| 55–64 age group | |||||
| Time-year period (every 1 period) | 0.064 | 1.066 | 0.894 | 1.271 | 0.475 |
| Age (every 1 year) | 0.014 | 1.014 | 0.958 | 1.074 | 0.633 |
| Sex (ref. men) | −0.119 | 0.888 | 0.595 | 1.325 | 0.561 |
| AMI (ref.) | 1 | ||||
| Unstable AP | −0.422 | 0.656 | 0.376 | 1.144 | 0.137 |
| Definite AMI (ref.) | 1 | ||||
| Possible AMI | −0.026 | 0.975 | 0.619 | 1.535 | 0.912 |
| STEMI (ref. no) | 0.592 | 1.807 | 1.152 | 2.834 | 0.010 |
| Previous acute heart failure (ref. no) | 1.737 | 5.680 | 3.903 | 8.264 | 0.0001 |
| Previous AMI (ref. no) | 0.402 | 1.495 | 1.062 | 2.104 | 0.021 |
| AH (ref. no) | −0.328 | 0.721 | 0.497 | 1.046 | 0.084 |
| Stroke (ref. no) | 0.661 | 1.938 | 1.104 | 3.401 | 0.021 |
| Diabetes (ref. no) | 0.863 | 2.371 | 1.656 | 3.397 | 0.0001 |
| Normal weight (ref.) | 1 | ||||
| Overweight | −0.473 | 0.623 | 0.431 | 0.901 | 0.012 |
| Obesity | 0.234 | 1.264 | 0.708 | 2.256 | 0.429 |
| Smoking (ref. no) | −0.055 | 0.946 | 0.656 | 1.365 | 0.768 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Radisauskas, R.; Kirvaitiene, J.; Bernotiene, G.; Virviciutė, D.; Ustinaviciene, R.; Tamosiunas, A. Long-Term Survival after Acute Myocardial Infarction in Lithuania during Transitional Period (1996–2015): Data from Population-Based Kaunas Ischemic Heart Disease Register. Medicina 2019, 55, 357. https://doi.org/10.3390/medicina55070357
Radisauskas R, Kirvaitiene J, Bernotiene G, Virviciutė D, Ustinaviciene R, Tamosiunas A. Long-Term Survival after Acute Myocardial Infarction in Lithuania during Transitional Period (1996–2015): Data from Population-Based Kaunas Ischemic Heart Disease Register. Medicina. 2019; 55(7):357. https://doi.org/10.3390/medicina55070357
Chicago/Turabian StyleRadisauskas, Ricardas, Jolita Kirvaitiene, Gailutė Bernotiene, Dalia Virviciutė, Ruta Ustinaviciene, and Abdonas Tamosiunas. 2019. "Long-Term Survival after Acute Myocardial Infarction in Lithuania during Transitional Period (1996–2015): Data from Population-Based Kaunas Ischemic Heart Disease Register" Medicina 55, no. 7: 357. https://doi.org/10.3390/medicina55070357
APA StyleRadisauskas, R., Kirvaitiene, J., Bernotiene, G., Virviciutė, D., Ustinaviciene, R., & Tamosiunas, A. (2019). Long-Term Survival after Acute Myocardial Infarction in Lithuania during Transitional Period (1996–2015): Data from Population-Based Kaunas Ischemic Heart Disease Register. Medicina, 55(7), 357. https://doi.org/10.3390/medicina55070357








