Hepatoprotective Effect of Melatonin in Toxic Liver Injury in Rats
Abstract
1. Introduction
2. Materials and Methods
2.1. Animal Model
2.2. Induction of Toxic Liver Injury
2.3. Blood and Tissue Acquisition
2.4. Determination of Liver Enzymes and Urea in Serum
2.5. NOS Assays
- Liver homogenates were prepared using saline at a ratio of 1:10.
- Liver cells suspension was centrifuged for 5 min at 300 g, then the supernatant was removed.
- Cells were washed twice in saline, after each wash they were centrifuged for 5 min at 300 g
- Lysis Phosphate-buffered saline was added in correlation 1 mL of buffer at 1 × 106 liver cells. Suspension was centrifuged for 5 min at 300 g.
- The supernatant was collected. The enzymes activities were estimated immediately or frozen at −20 °C for postponed testing.
2.6. Oxygen Reactive Substances and Antioxidant Enzymes Activities
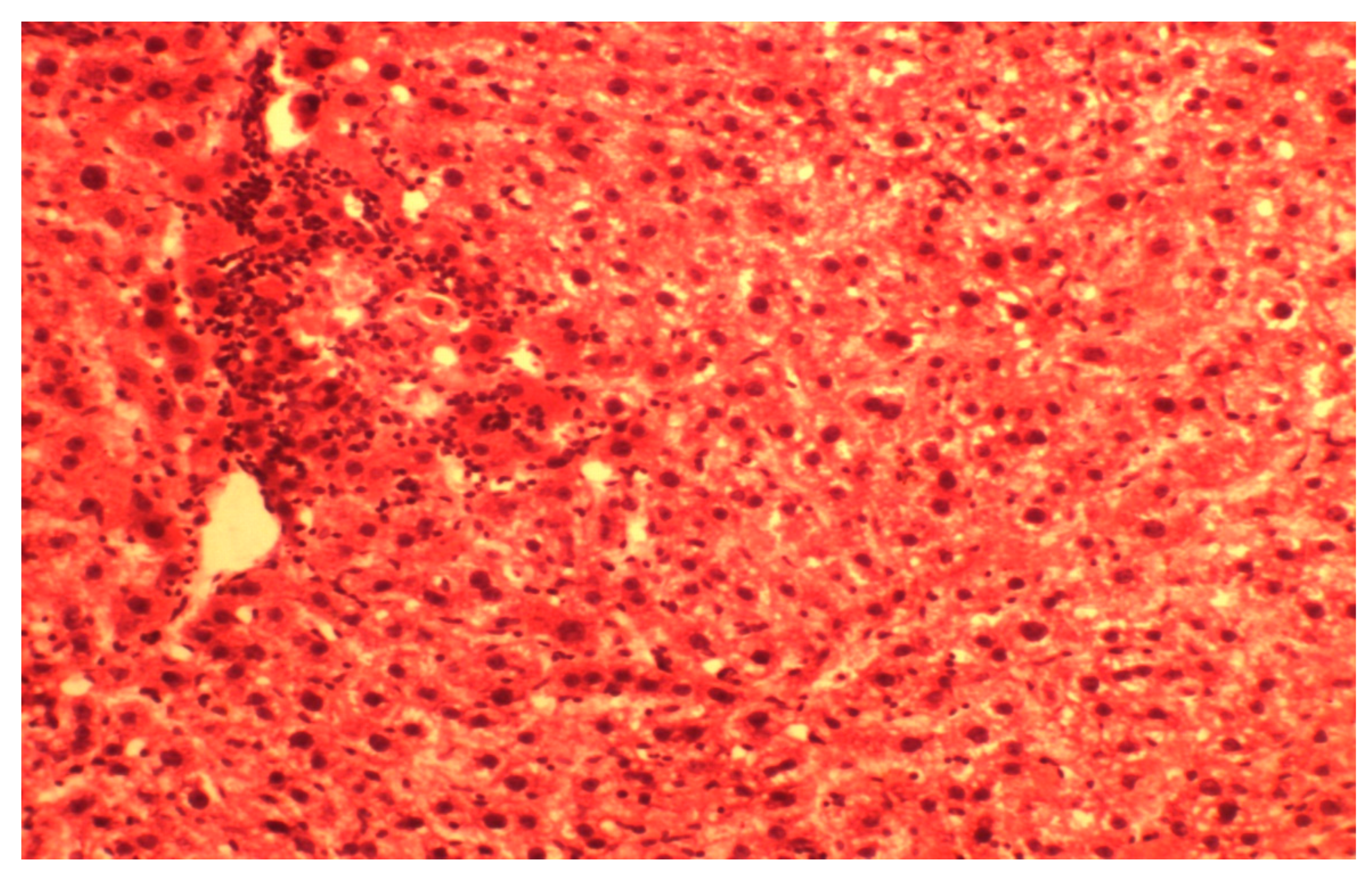
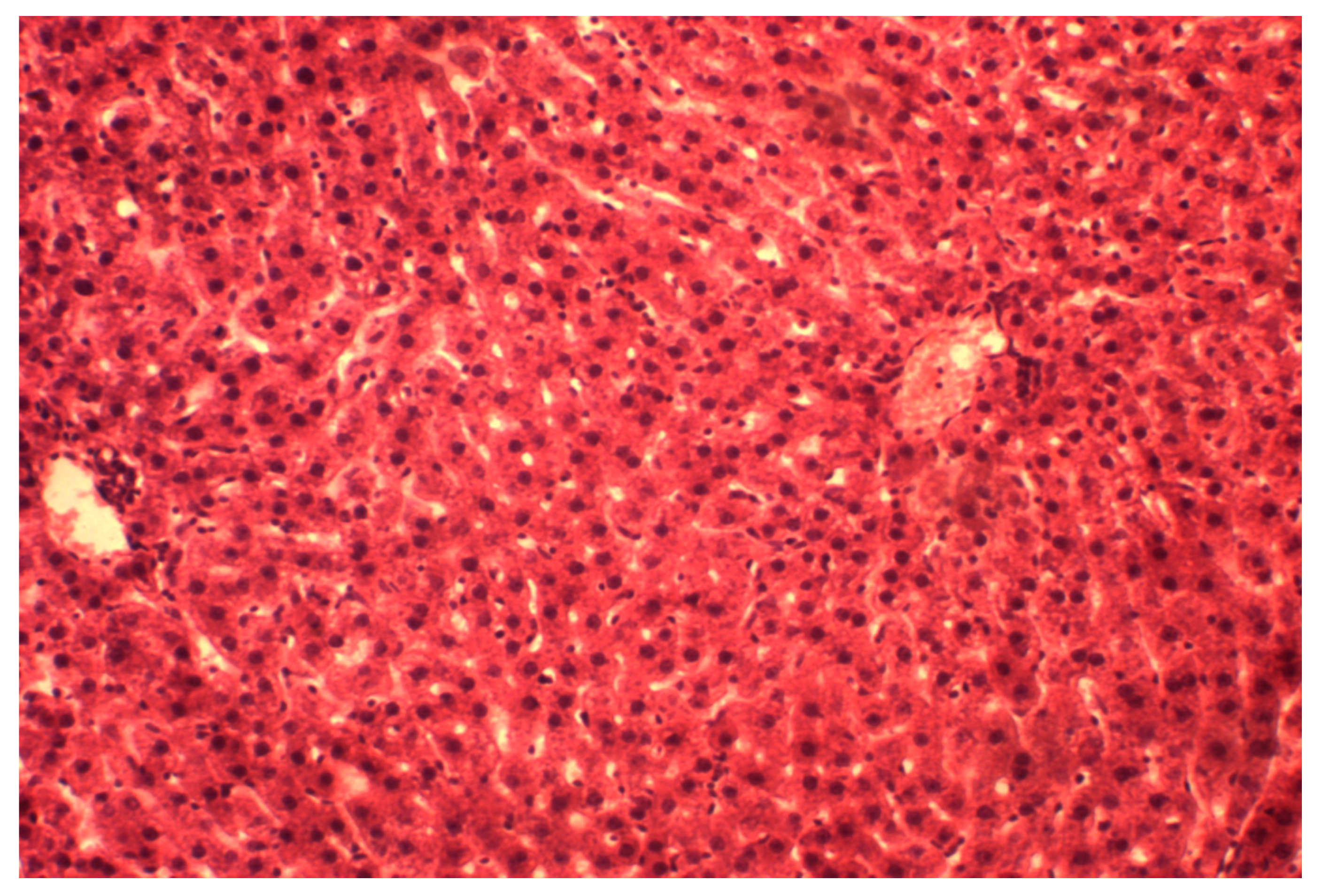
2.7. Histopathological Study
2.8. Statistical Analysis
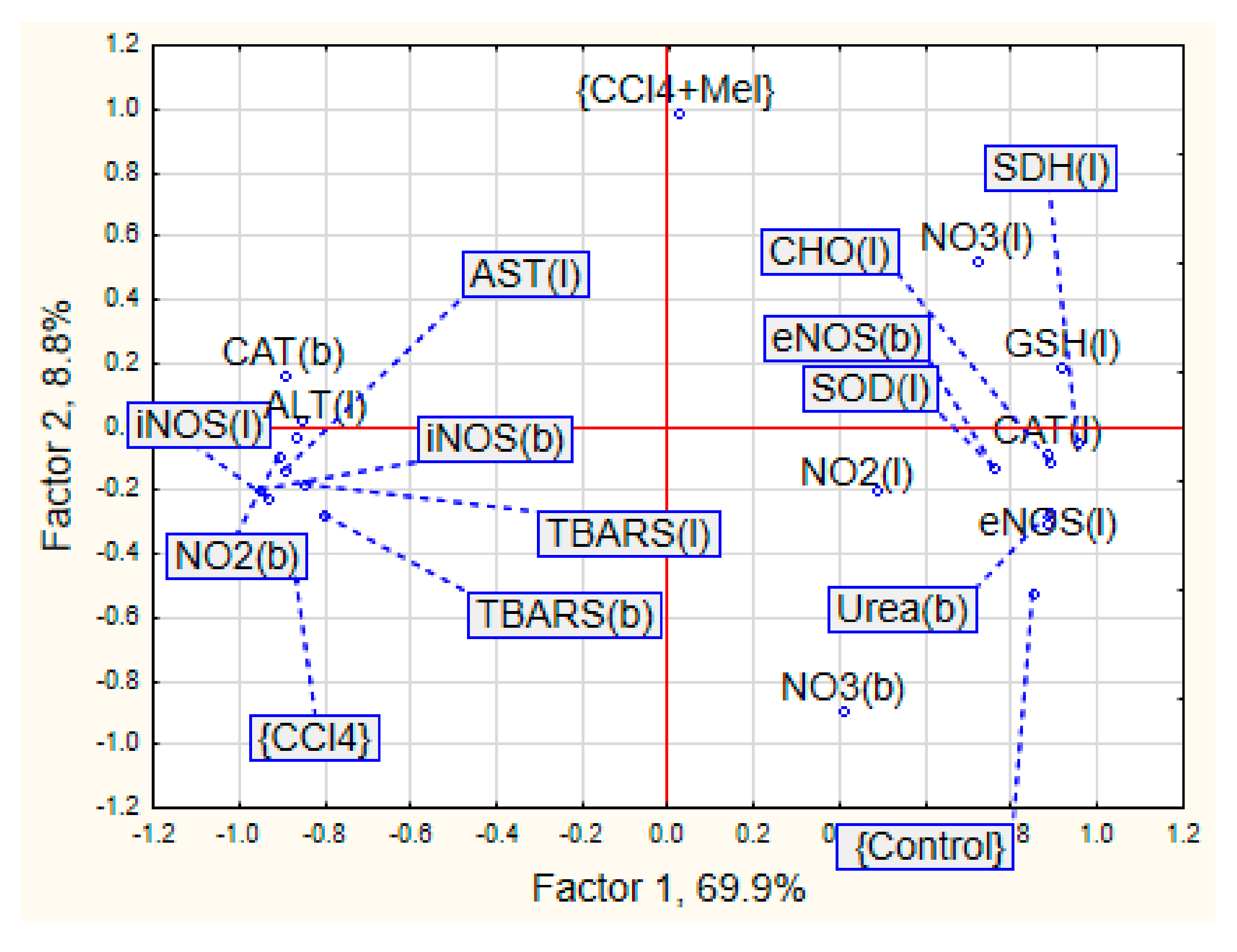
3. Results
4. Discussion
5. Conclusions
- a decrease of cytolysis enzymes activity, and activation of mitochondrial respiration in hepatocytes;
- partial restoration of the structural organization of the liver, reduction of its dystrophic necrotic manifestations;
- reduction of the oxidative stress manifestations and restoration of antioxidant system balance;
- block of iNOS both in blood and in the liver leads to reduction of nitro oxidative stress.
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Tan, D.X.; Manchester, L.C.; Hardeland, R.; Lopez-Burillo, S.; Mayo, J.C.; Sainz, R.M.; Reiter, R.J. Melatonin: A hormone, a tissue factor, an autocoid, a paracoid and an antioxidant vitamin. J. Pineal Res. 2003, 34, 75–78. [Google Scholar] [CrossRef] [PubMed]
- Reiter, R.J. Melatonin: Clinical relevance. Best Pract. Res. Clin. Endocrinol. Metab. 2003, 17, 273–285. [Google Scholar] [CrossRef]
- Dawson, D.; Encel, N. Melatonin and sleep in humans. J. Pineal Res. 1993, 15, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Reiter, R.J.; Tan, D.X.; Terron, M.P.; Flores, L.J.; Czarnocki, Z. Melatonin and its metabolites: New findings regarding their production and their radical scavenging actions. Acta Biochim. Pol. 2007, 54, 1–9. [Google Scholar] [PubMed]
- Dubocovich, M.L.; Cardinali, D.P.; Delagrange, P.; Krause, D.N.; Strosberg, D.; Sugden, D.; Yocca, F.D. Melatonin receptors. In The IUPHAR Compendium of Receptor Characterization and Classification, 2nd ed.; Girdlestone, D., Ed.; IUPHAR Media: London, UK, 2000; Volume 2, pp. 270–277. [Google Scholar]
- Karasek, M.; Winczyk, K. Melatonin in Humans. J. Physiol. Pharmacol. 2006, 57, 19–39. [Google Scholar] [PubMed]
- Reiter, R.J. The role of the neurohormone melatonin as a buffer against macromolecular oxidative damage. Neurochem. Int. 1995, 27, 453–460. [Google Scholar] [CrossRef]
- Brzezinski, A. Melatonin in humans. N. Engl. J. Med. 1997, 336, 186–195. [Google Scholar] [CrossRef]
- Dweik, R.A. Nitric oxide, hypoxia, and superoxide: The good, the bad, and the ugly! Thorax 2005, 60, 265–267. [Google Scholar] [CrossRef][Green Version]
- Farzaneh-Far, R.; Moore, K. Nitric oxide in the liver. Liver 2001, 21, 161–174. [Google Scholar] [CrossRef]
- Laskin, J.D.; Heck, D.E.; Gardner, C.R.; Laskin, D.L. Prooxidant and antioxidant function of nitric oxide in liver toxicity. Antioxid. Redox Signal. 2001, 3, 261–271. [Google Scholar] [CrossRef]
- Grigorov, I.; Bogojevic, D.; Jovanovic, S.; Petrovic, A.; Ivanovic-Matic, S.; Zolotarevski, L.; Poznanovic, G.; Martinovic, V. Hepatoprotective effects of melatonin against pronecrotic cellular events in streptozotocin-induced diabetic rats. J. Physiol. Biochem. 2014, 70, 441–450. [Google Scholar] [CrossRef] [PubMed]
- Bedini, A.; Fraternale, A.; Crinelli, R.; Mari, M.; Bartolucci, S.; Chiarantini, L.; Spadoni, G. Design, Synthesis, and Biological Activity of Hydrogen Peroxide Responsive Arylboronate Melatonin Hybrids. Chem. Res. Toxicol. 2019, 32, 100–112. [Google Scholar] [CrossRef] [PubMed]
- Jahovic, N.; Cevik, H.; Sehirli, A.O.; Yegen, B.C.; Sener, G. Melatonin prevents methotrexate-induced hepatorenal oxidative injury in rats. J. Pineal Res. 2003, 34, 282–287. [Google Scholar] [CrossRef] [PubMed]
- Andreeva, L.I.; Kozhemyakin, L.A.; Kiskun, A.A. Modification of the method for determining lipid peroxide in the test with thiobarbituric acid. Lab. Delo 1988, 11, 41–43. [Google Scholar]
- Green, I.C.; Davie, A.W.; Golawski, J. Analysis of nitrate, nitrite and [15N] nitrate in biological fluids. Anal. Biochem. 1982, 126, 131–138. [Google Scholar] [CrossRef]
- Korolyuk, M.A.; Ivanova, L.I.; Mayorova, I.G.; Tokarev, V.E. Method for determination of catalase activity. Lab. Delo 1988, 1, 16–19. [Google Scholar]
- Kolb, V.G.; Kamyshnikov, V.S. Handbook of Clinical Chemistry; Minsk, Belarus, 1982; p. 311. [Google Scholar]
- Chevari, C.; Csaba, J.; Sekey, J. The role of superoxide dismutase in oxidative processes in cells and the method of its determination in biological materials. Lab. Delo 1985, 11, 678–684. [Google Scholar]
- Gavrilov, V.B.; Mishkorudnaya, M.I. Spectrophotometric determination of lipid hydroperoxide in the blood plasma. Lab. Delo 1983, 3, 33–35. [Google Scholar]
- Orekhovich, V.N. Modern Methods in Biochemistry; AMS USSR Moscow, Medicine; 1977; p. 390. [Google Scholar]
- Eshchenko, N.D.; Volsky, G.G. Determination of the amount of succinic acid and succinate dehydrogenase activity. In Methods of Biochemical Researches; Publishing House of Leningrad University: Leningrad, Russia, 1982; pp. 207–212. [Google Scholar]
- Ellman, G.L. Tissue sulfhydryl groups. Arch. Biochem. Biophys. 1959, 82, 70–77. [Google Scholar] [CrossRef]
- Liang, X.; Wu, K.; Liu, M.; Yang, B. Adverse impact of carbon tetrachloride on metabolic function in mice. J. Cellul. Biochem. 2019, 120, 11973–11980. [Google Scholar] [CrossRef]
- Containment Levels for Chemical Administration in Animals; Agreement of Boston University Environmental Health and Safety: Boston, MA, USA, 2019.
- Tanaka, N.; Takana, K.; Nagashima, Y.; Kondo, M.; Sekihara, H. Nitric oxide increase hepatic arterial blood flow in rats with carbon tetrachloride-induced acute hepatic injury. Gastroenterology 1999, 117, 173–178. [Google Scholar] [CrossRef]
- Cabeza, J.; Motilva, V.; Martin, M.J.; Lastra, C.A. Mechanisms involved in gastric protection of melatonin against oxidant stress by ischemia-reperfusion in rats. Life Sci. 2001, 68, 1405–1415. [Google Scholar] [CrossRef]
- Gilad, E.; Cuzzocrea, S.; Zingarelli, B.; Salzman, A.L.; Szabo, C. Melatonin is a scavenger of peroxynitrite. Life Sci. 1997, 60, 169–174. [Google Scholar] [CrossRef]
- Boll, M.; Weber, L.W.; Becker, E.; Stampfl, A. Mechanism of carbon tetrachloride-induced hepatotoxicity. Hepatocellular damage by reactive carbon tetrachloride metabolites. Z. Naturforsch C 2001, 56, 649–659. [Google Scholar] [CrossRef] [PubMed]
- Hubsky, Y.I. Correction of the chemical liver injury. In The Health; Kiev, Ukraine, 1989; p. 168. [Google Scholar]
- Sachdeva, M.; Chadha, R.; Kumar, A.; Karan, M.; Singh, T.; Dhingra, S. Hepatoprotective effect of trimethylgallic acid esters against carbon tetrachloride-induced liver injury in rats. J. Exp. Biol. 2015, 53, 803–809. [Google Scholar]
- Gonskii, I.I.; Korda, M.M.; Klishch, I.N.; Fira, L.S. Role of the antioxidant system in the pathogenesis of toxic hepatitis. Patol. Fiziol. Eksp Ter. 1996, 2, 43–45. [Google Scholar]
- Shiryaeva, A.; Baidyuk, E.; Arkadieva, A.; Okovityy, S.; Morozov, V.; Sakuta, G. Hepatocyte mitochondrion electron-transport chain alterations in CCl4 and alcohol induced hepatitis in rats and their correction with simvastatin. J. Bioenerg. Biomemb. 2008, 40, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Oleshchuk, O.M.; Ivankiv, Y.I. Melatonin as hepatoprotector at diabetes. Bull. Sci. Res. 2015, 1, 10–14. [Google Scholar] [CrossRef][Green Version]
- Ivankiv, Y.I.; Oleshchuk, O.M. Indicators of prooxidant-antioxidant homeostasis of healthy animals under the introduction of melatonin. Med. Clin. Chem. 2015, 17, 39–42. [Google Scholar] [CrossRef]
- Jaworek, J.; Konturek, S.J.; Leja-Szpak, A. Role of endogenous melatonin and its MT2 receptor in the modulation of caerulein-induced pancreatitis in the rats. J. Physiol. Pharmacol. 2002, 53, 791–804. [Google Scholar]
- Aydogan, S.; Yerer, M.B.; Goktas, A. Melatonin and nitric oxide. J. Endocrinol. Investig. 2006, 29, 281–287. [Google Scholar] [CrossRef] [PubMed]
- Galano, A.; Medina, M.E.; Tan, D.X.; Reiter, R.J. Melatonin and its metabolites as copper chelating agents and their role in inhibiting oxidative stress: A physicochemical analysis. J. Pineal Res. 2015, 58, 107–116. [Google Scholar] [CrossRef]
- Limson, J.; Nyokong, T.; Daya, S. The interaction of melatonin and its precursors with aluminium, cadmium, copper, iron, lead, and zinc: An adsorptive voltammetric study. J. Pineal Res. 1998, 24, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Morrell, A.; Tallino, S.; Yu, L.; Burkhead, J.L. The role of insufficient copper in lipid synthesis and fatty-liver disease. IUBMB Life 2017, 69, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Tarantino, G.; Porcu, C.; Arciello, M.; Andreozzi, P.; Balsano, C. Prediction of carotid intima–media thickness in obese patients with low prevalence of comorbidities by serum copper bioavailability. J. Gastroenterol. Hepatol. 2018, 33, 1511–1517. [Google Scholar] [CrossRef] [PubMed]
- Acuna-Castroviejo, D.; Escames, G.; Carazo, A.; Leon, J.; Khaldy, H.; Reiter, R.J. Melatonin, mitochondria homeostasis and mitochondrial-related diseases. Curr. Top. Med. Chem. 2002, 2, 133–152. [Google Scholar] [CrossRef] [PubMed]
| Control | CCl4 | CCl4/Melatonin | |
|---|---|---|---|
| ALT, mmoL/(g × L) | 0.45 ± 0.10 | 1.13 ± 0.07 | 0.75 ± 0.04 |
| p < 0.01 | p1 < 0.01 | ||
| AST, mmoL/(g × L) | 1.70 ± 0.21 | 3.17 ± 0.16 | 2.23 ± 0.60 |
| p < 0.01 | p1 < 0.01 | ||
| CAT (serum), mcat/L | 14.58 ± 0.40 | 18.93 ± 0.30 | 15.84 ± 0.17 |
| p < 0.005 | p1 < 0.001 | ||
| CAT (liver), mcat/kg | 4.31 ± 0.11 | 2.71 ± 0.32 | 3.31 ± 0.13 |
| p < 0.01 | p1 > 0.05 | ||
| SOD, U/g | 4.59 ± 0.10 | 2.95 ± 0.19 | 3.60 ± 0.19 |
| p < 0.005 | p1 ≤ 0.05 | ||
| LHP, U/g | 1.77 ± 0.14 | 3.05 ± 0.13 | 2.43 ± 0.21 |
| p < 0.005 | p1 ≤ 0.05 | ||
| TBARS (serum), mmoL/L | 2.18 ± 0.11 | 3.18 ± 0.20 | 2.36 ± 0.05 |
| p < 0.01 | p1 < 0.01 | ||
| TBARS (liver), mmoL/kg | 3.06 ± 0.10 | 4.40 ± 0.22 | 3.46 ± 0.19 |
| p < 0.01 | p1 < 0.05 | ||
| CP, mg/L | 230.42 ± 5.35 | 278.54 ± 7.99 | 250.83 ± 12.84 |
| p < 0.01 | p1 > 0.05 | ||
| GSH (liver), mmoL/kg | 4.20 ± 0.08 | 2.86 ± 0.10 | 3.67 ± 0.14 |
| p < 0.005 | p1 < 0.01 | ||
| CHO, mmoL/(kg × min) | 8.73 ± 0.28 | 6.65 ± 0.16 | 7.51 ± 0.48 |
| p < 0.01 | p1 < 0.01 | ||
| SDH, mmoL/(kg × min) | 8.85 ± 0.11 | 6.78 ± 0.11 | 7.51 ± 0.12 |
| p < 0.005 | p1 < 0.001 | ||
| Urea, mmoL/L | 5.88 ± 0.11 | 3.83 ± 0.23 | 4.39 ± 0.14 |
| p < 0.001 | p1 > 0.05 |
| Blood (µmol/L) | Liver (µmol/kg) | |||
|---|---|---|---|---|
| NO2− | NO3− | NO2− | NO3− | |
| Control | 1.17 ± 0.06 | 10.21 ± 0.07 | 2.19 ± 0.15 | 8.77 ± 0.26 |
| CCl4 | 3.18 ± 0.26 | 8.36 ± 0.18 | 1.80 ± 0.18 | 6.79 ± 0.24 |
| p < 0.005 | p < 0.005 | p > 0.05 | p < 0.01 | |
| CCl4/melatonin | 1.98 ± 0.17 | 5.92 ± 0.05 | 1.88 ± 0.07 | 9.01 ± 0.45 |
| p < 0.01 | p < 0.005 | p > 0.05 | p > 0.05 | |
| p1 < 0.01 | p1 < 0.005 | p1 > 0.05 | p1 < 0.01 | |
| Serum | Liver (1 mL−1 × 106 Cells) | |||
|---|---|---|---|---|
| eNOS U/mL | iNOS ng/mL | eNOS U/mL | iNOS ng/mL | |
| Control | 2.33 ± 0.26 | 15.38 ± 0.82 | 3.79 ± 0.17 | 2.30 ± 0.34 |
| CCl4 | 1.27 ± 0.07 | 96.51 ± 5.21 | 1.26 ± 0.20 | 11.28 ± 0.79 |
| p < 0.05 | p < 0.001 | p < 0.01 | p < 0.001 | |
| CCl4 + melatonin | 1.72 ± 0.21 | 38.88 ± 3.06 | 2.05 ± 0.13 | 4.76 ± 0.34 |
| p > 0.1 | p < 0.001 | p < 0.01 | p < 0.01 | |
| p1 > 0.05 | p1< 0.001 | p1 > 0.05 | p1 < 0.001 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oleshchuk, O.; Ivankiv, Y.; Falfushynska, H.; Mudra, A.; Lisnychuk, N. Hepatoprotective Effect of Melatonin in Toxic Liver Injury in Rats. Medicina 2019, 55, 304. https://doi.org/10.3390/medicina55060304
Oleshchuk O, Ivankiv Y, Falfushynska H, Mudra A, Lisnychuk N. Hepatoprotective Effect of Melatonin in Toxic Liver Injury in Rats. Medicina. 2019; 55(6):304. https://doi.org/10.3390/medicina55060304
Chicago/Turabian StyleOleshchuk, Oleksandra, Yana Ivankiv, Halina Falfushynska, Alla Mudra, and Nataliya Lisnychuk. 2019. "Hepatoprotective Effect of Melatonin in Toxic Liver Injury in Rats" Medicina 55, no. 6: 304. https://doi.org/10.3390/medicina55060304
APA StyleOleshchuk, O., Ivankiv, Y., Falfushynska, H., Mudra, A., & Lisnychuk, N. (2019). Hepatoprotective Effect of Melatonin in Toxic Liver Injury in Rats. Medicina, 55(6), 304. https://doi.org/10.3390/medicina55060304







