Time from Symptom Onset to Diagnosis and Treatment among Haematological Malignancies: Influencing Factors and Associated Negative Outcomes
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
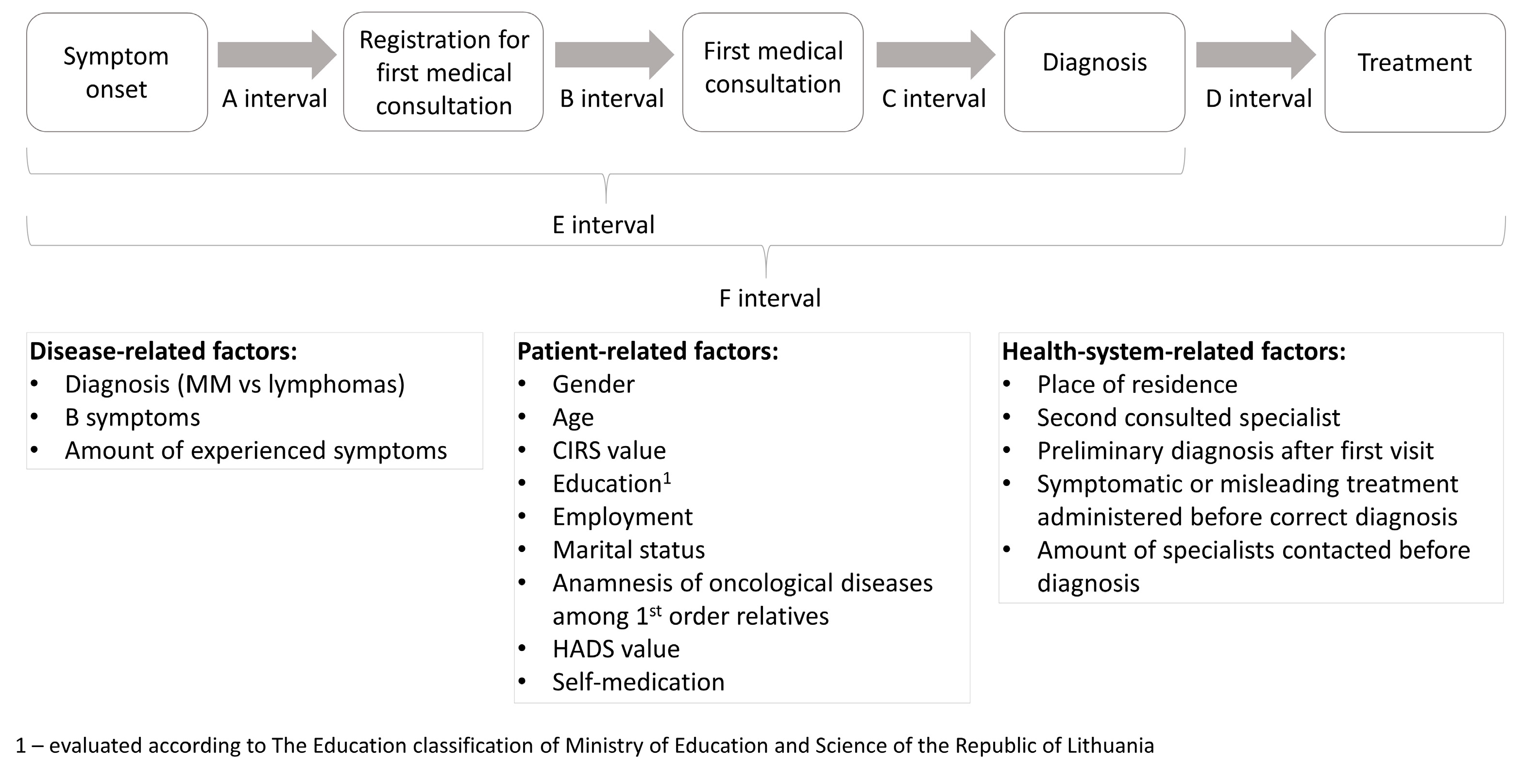
2.2. Study Design
2.3. Statistical Analysis
3. Results
3.1. Patient Characteristics
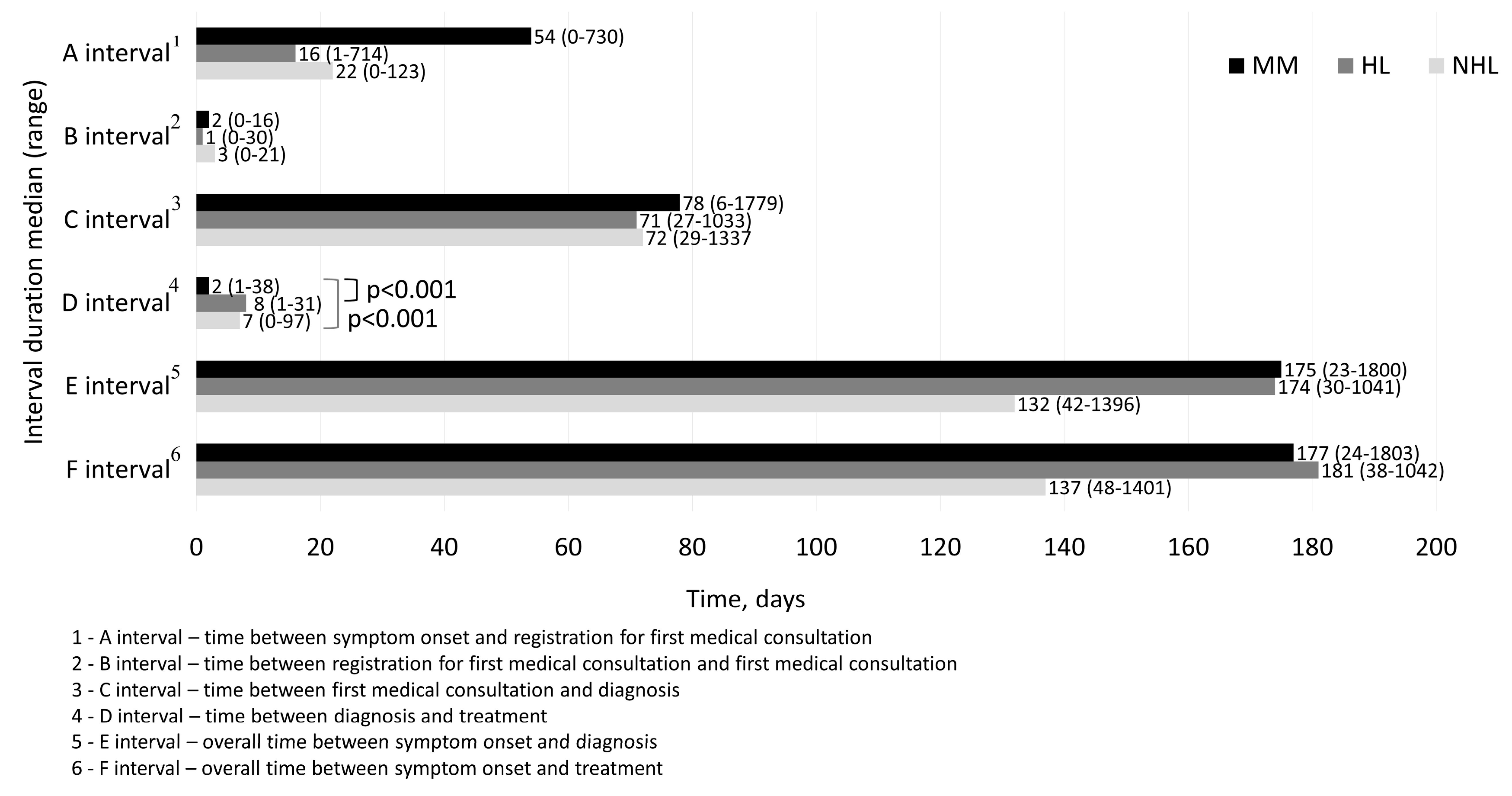
3.2. A, B, C, D, E, F Interval Durations
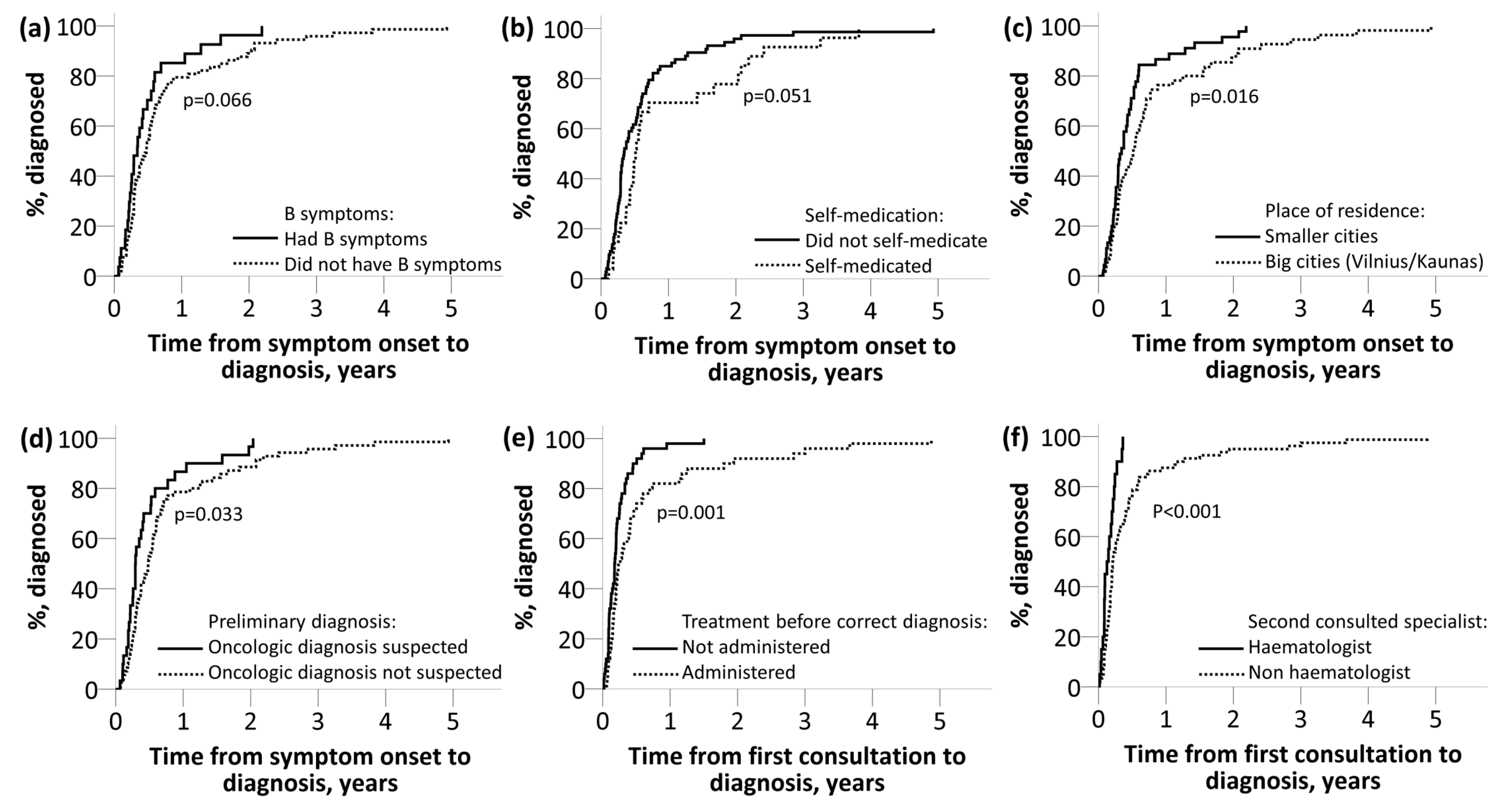
3.3. Disease-Related Factors’ Influence on Diagnostic Lag Time
3.4. Influence of Patient-Related Factors on Diagnostic Intervals
3.5. Health-System-Related Factors’ Influence on Interval Durations
3.6. Influence of Disease, Patient and Health-System-Related Factors on Interval Durations—Multiple Linear Regression
3.7. Effect of Diagnostic Delay on Disease Stage and Complications at the Time of Diagnosis
4. Discussion
4.1. Interval Durations and Comparison with Other Studies
4.2. Disease-Related Factors’ Effect on Diagnostic Lag Time
4.3. Patient-Related Factors’ Effect on Interval Durations
4.4. Health-System-Related Factors’ Effect on Diagnostic Lag Time
4.5. Diagnostic Delay Effect on Disease Stage and Burden of Complications
4.6. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Rodriguez-Abreu, D.; Bordoni, A.; Zucca, E. Epidemiology of hematological malignancies. Ann. Oncol. 2007, 18, i3–i8. [Google Scholar] [CrossRef]
- Kariyawasan, C.C.; Hughes, D.A.; Jayatillake, M.M.; Mehta, A.B. Multiple myeloma: Causes and consequences of delay in diagnosis. QJM 2007, 100, 635–640. [Google Scholar] [CrossRef]
- Walter, F.; Webster, A.; Scott, S.; Emery, J. The Andersen Model of Total Patient Delay: A systematic review of its application in cancer diagnosis. J. Health Serv. Res. Policy 2012, 17, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Neal, R.D. Do diagnostic delays in cancer matter? Br. J. Cancer 2009, 101, S9–S12. [Google Scholar] [CrossRef] [PubMed]
- Hosseini, S.N.; Mousavinasab, S.N.; Moghimi, M.H.; Fallah, R. Delay in diagnosis and treatment of gastric cancer: From the beginning of symptoms to surgery—An Iranian study. Turk. J. Gastroenterol. 2007, 18, 77–81. [Google Scholar] [PubMed]
- Korsgaard, M.; Pedersen, L.; Laurberg, S. Delay of diagnosis and treatment of colorectal cancer—A population-based Danish Study. Cancer Detect. Prev. 2008, 32, 45–51. [Google Scholar] [CrossRef]
- Pitchers, M.; Weber, G.F. Delay in referral of oropharyngeal squamous cell carcinoma to secondary care correlates with a more advanced stage at presentation, and is associated with poorer survival. Br. J. Cancer 2006, 94, 955–958. [Google Scholar] [CrossRef] [PubMed]
- Jiwa, M.; Reid, J.; Handley, C.; Grimwood, J.; Ward, S.; Turner, K.; Ibbotson, M.; Thorman, N. Less haste more speed: Factors that prolong the interval from presentation to diagnosis in some cancers. Fam. Pr. 2004, 21, 299–303. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Dwivedi, A.K.; Dwivedi, S.N.; Deo, S.; Shukla, R.; Pandey, A.; Dwivedi, D.K. An epidemiological study on delay in treatment initiation of cancer patients. Health (Irvine Calif.) 2012, 4, 66–79. [Google Scholar] [CrossRef]
- Howell, D.A.; Smith, A.G.; Roman, E. Help-seeking behaviour in patients with lymphoma. Eur. J. Cancer Care (Engl.) 2008, 17, 394–403. [Google Scholar] [CrossRef] [PubMed]
- Howell, D.A.; Smith, A.G.; Jack, A.; Patmore, R.; Macleod, U.; Mironska, E.; Roman, E. Time-to-diagnosis and symptoms of myeloma, lymphomas and leukaemias: A report from the Haematological Malignancy Research Network. BMC Blood Disord. 2013, 13, 9. [Google Scholar] [CrossRef] [PubMed]
- Howell, D.A.; Hart, R.I.; Smith, A.G.; Macleod, U.; Patmore, R.; Cook, G.; Roman, E. Myeloma: Patient accounts of their pathways to diagnosis. PLoS ONE 2018, 13, e0194788. [Google Scholar] [CrossRef] [PubMed]
- Friese, C.R.; Abel, G.A.; Magazu, L.S.; Neville, B.A.; Richardson, L.C.; Earle, C.C. Diagnostic delay and complications for older adults with multiple myeloma. Leuk Lymphoma 2009, 50, 392–400. [Google Scholar] [CrossRef] [PubMed]
- Nassur, R.; Mangel, J.; Chin-Yee, I. Delays in the Cancer Pathway from Symptom Onset to Initiation of Treatment – A Retrospective Study in Patients with Non-Hodgkin’s Lymphoma. Blood 2015, 108, 347. [Google Scholar]
- Buckstein, R.; Giurgis, H.; Cheung, M.C. Predictors Of Delay In Diagnosis and Treatment In Diffuse Large B-Cell Lymphoma and Impact on Survival. Blood 2013, 122, 4322. [Google Scholar]
- Martin, S.; Ulrich, C.; Munsell, M.; Taylor, S.; Lange, G.; Bleyer, A. Delays in Cancer Diagnosis in Underinsured Young Adults and Older Adolescents. Oncologist 2007, 12, 816–824. [Google Scholar] [CrossRef]
- Summerfield, G.P.; Carey, P.J.; Galloway, M.J.; Tinegate, H.N. An audit of delays in diagnosis and treatment of lymphoma in district hospitals in the northern region of the United Kingdom. Clin. Lab. Haematol. 2000, 22, 157–160. [Google Scholar] [CrossRef] [PubMed]
- Graziani, G.; Herget, G.W.; Ihorst, G.; Schafer, H.; Neubauer, J.; May, A.M.; Duyster, J.; Einsele, H.; Wäsch, R.; Engelhardt, M. Time from First Symptom Onset to the Final Diagnosis of Multiple Myeloma—Possible Risks and Future Solutions: Large Retrospective and Confirmatory Prospective “Deutsche Studiengruppe Multiples Myelom” (DSMM) Analysis. Blood 2017, 130, 4710. [Google Scholar]
- Howell, D.; Smith, A.; Appleton, S.; Bagguley, T.; Macleod, U.; Cook, G.; Patmore, R.; Roman, E. Multiple myeloma: Routes to diagnosis, clinical characteristics and survival—Findings from a UK population-based study. Br. J. Haematol. 2017, 177, 67–71. [Google Scholar] [CrossRef]
- International Myeloma Working Group|International Myeloma Working Group (IMWG). Criteria for the Diagnosis of Multiple Myeloma. 2015. Available online: http://imwg.myeloma.org/international-myeloma-working-group-imwg-criteria-for-the-diagnosis-of-multiple-myeloma/ (accessed on 2 May 2019).
- Rosen, P.J.; Wender, R.C.; Kadkhoda, H.; Kober, S.L. Measuring the Ability of Primary-Care Physicians To Diagnose and Manage Patients with Hematologic Malignancies. Blood 2015, 110, 3312. [Google Scholar]
- Friese, C.R.; Abel, G.A.; Magazu, L.A.; Neville, B.A.; Richardson, L.C.; Earle, C.C. Predictors of Diagnosis Delay and Complications for Newly-Diagnosed Myeloma Patients. Blood 2015, 110, 368. [Google Scholar]
- Jassem, J.; Ozmen, V.; Bacanu, F.; Drobniene, M.; Eglitis, J.; Lakshmaiah, K.C.; Kahan, Z.; Mardiak, J.; Pieńkowski, T.; Semiglazova, T. Delays in diagnosis and treatment of breast cancer: A multinational analysis. Eur. J. Public Health 2014, 24, 761–767. [Google Scholar] [CrossRef] [PubMed]
- Allgar, V.L.; Neal, R.D. Delays in the diagnosis of six cancers: Analysis of data from the National Survey of NHS Patients: Cancer. Br. J. Cancer 2005, 92, 1959–1970. [Google Scholar] [CrossRef]
- Dang-Tan, T.; Franco, E.L. Diagnosis delays in childhood cancer. Cancer 2007, 110, 703–713. [Google Scholar] [CrossRef] [PubMed]
- Buckle, G.C.; Collins, J.P.; Sumba, P.O.; Nakalema, B.; Omenah, D.; Stiffler, K.; Casper, C.; Otieno, J.A.; Orem, J.; Moormann, A.M. Factors influencing time to diagnosis and initiation of treatment of endemic Burkitt Lymphoma among children in Uganda and western Kenya: A cross-sectional survey. Infect. Agent Cancer 2013, 8, 36. [Google Scholar] [CrossRef] [PubMed]
- Stefan, D.C.; Siemonsma, F. Delay and causes of delay in the diagnosis of childhood cancer in Africa. Pediatr. Blood Cancer 2011, 56, 80–85. [Google Scholar] [CrossRef] [PubMed]
- Varga, G.; Mikala, G.; Andrikovics, H.; Masszi, T. How long does a myeloma patient currently wait for the diagnosis in Hungary? Orv. Hetil. 2014, 155, 1538–1543. [Google Scholar] [CrossRef][Green Version]
- Chukwu, B.F.; Ezenwosu, O.U.; Ikefuna, A.N.; Emodi, I.J. Diagnostic Delay in Pediatric Cancer in Enugu, Nigeria: A Prospective Study. Pediatr. Hematol. Oncol. 2015, 32, 164–171. [Google Scholar] [CrossRef] [PubMed]
- Abel, G.A.; Friese, C.R.; Magazu, L.S.; Richardson, L.C.; Fernandez, M.E.; De Zengotita, J.J.; Earle, C.C. Delays in referral and diagnosis for chronic hematologic malignancies: A literature review. Leuk Lymphoma 2008, 49, 1352–1359. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.-H.; Chang, F.-C.; Hsu, S.-D.; Chi, H.-Y.; Huang, L.-J.; Yeh, M.-K. Inappropriate self-medication among adolescents and its association with lower medication literacy and substance use. PLoS ONE 2017, 12, e0189199. [Google Scholar] [CrossRef]
- Du, Y.; Knopf, H. Self-medication among children and adolescents in Germany: Results of the National Health Survey for Children and Adolescents (KiGGS). Br. J. Clin. Pharm. 2009, 68, 599–608. [Google Scholar] [CrossRef] [PubMed]
- Paula Martins, A.; da Costa Miranda, A.; Mendes, Z.; Soares, M.A.; Ferreira, P.; Nogueira, A. Self-medication in a Portuguese urban population: A prevalence study. Pharm. Drug Saf. 2002, 11, 409–414. [Google Scholar] [CrossRef] [PubMed]
- Alghanim, A.S. Self-medication practice among patients in a public health care system. East Mediterr. Health J. 2011, 17, 409–416. [Google Scholar] [CrossRef] [PubMed]
- Cancer Research UK Cancer Awareness Measure (CAM) Toolkit (version 2.1); Cancer Research UK: London, UK, 2007.
- “Know 4 Sure” Campaign|Cancer Research UK. Available online: http://www.cancerresearchuk.org/health-professional/awareness-and-prevention/be-clear-on-cancer/know-4-sure-campaign (accessed on 3 March 2018).
- Usha Isaac John SIsaac, G.J.I. Causes of delay in cancer diagnosis. Isra Med. J. 2013, 5, 116–120. [Google Scholar]
- Lyratzopoulos, G.; Wardle, J.; Rubin, G. Rethinking diagnostic delay in cancer: How difficult is the diagnosis? BMJ 2014, 349, 1–6. [Google Scholar] [CrossRef]
- Shephard, E.A.; Neal, R.D.; Rose, P.; Walter, F.M.; Litt, E.J.; Hamilton, W.T. Quantifying the risk of multiple myeloma from symptoms reported in primary care patients: A large case–control study using electronic records. Br. J. Gen. Pract. 2015, 65, e106–e113. [Google Scholar] [CrossRef]
- WHO|Density of Physicians. Total Number per 1000 Population, Latest Available Year; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- Neal, R.D.; Tharmanathan, P.; France, B.; Din, N.U.; Cotton, S.; Fallon-Ferguson, J.; Hamilton, W.; Hendry, A.; Hendry, M.; Lewis, R.; et al. Is increased time to diagnosis and treatment in symptomatic cancer associated with poorer outcomes? Systematic review. Br. J. Cancer 2015, 112, S92–S107. [Google Scholar] [CrossRef]
| Patient-Related Factors | MM | Lymphoma |
|---|---|---|
| Gender—male/female N | 26/27 | 21/26 |
| Age (years) median (range) | 53 (44–84) | 47 (19–81) |
| CIRS 1 median (range) | 5 (3–12) | 5 (3–11) |
| Education—no higher education/higher education N | 26/27 | 20/27 |
| Employment before disease—unemployed/employed N | 16/37 | 15/32 |
| Marital status—married/not married N | 37/16 | 24/23 |
| Anamnesis of oncological diseases among 1st order relatives—no/yes N | 32/21 | 34/13 |
| HADS 2 median (range) | 7 (0–24) | 7 (0–23) |
| Self-medication—no/yes N | 35/18 | 38/9 |
| Health-system-related factors | ||
| Place of residence—Vilnius/Kaunas/smaller cities N | 27/1/25 | 24/3/20 |
| First consulted doctor—general practitioner/other specialist N | 44/9 | 42/5 |
| Second consulted doctor—hematologist/other specialist N | 4/49 | 9/38 |
| Oncologic diagnosis suspected after first visit/not suspected N | 15/38 | 15/32 |
| Treatment 3 before correct diagnosis not administered/administered N | 22/31 | 28/19 |
| Number of specialists before correct diagnosis median (range) | 3 (2–8) | 3 (2–10) |
| Beta Value * | Percentile Beta Value ** | t Value | p Value | |
|---|---|---|---|---|
| B 1 interval model (adjusted R2 = 0.052, p = 0.027) | ||||
| (Intercept) | 1.567 | - | 5.650 | <0.001 |
| CIRS value, range 3–12 | −0.098 | −9.3% | −2.367 | 0.019 |
| HADS value, range 0-24 | 0.031 | 3.2% | 1.501 | 0.136 |
| C 2 interval model (adjusted R2 = 0.332, p < 0.001) | ||||
| (Intercept) | 1.609 | - | 3.352 | 0.001 |
| Number of specialists before correct diagnosis, range 2–10 | 0.252 | 28.7% | 4.185 | <0.001 |
| Oncologic diagnosis suspected after 1st visit: 1—Yes, 2—No | 0.651 | 91.7% | 3.139 | 0.002 |
| Place of residence: 1—smaller cities, 2—Vilnius/Kaunas | 0.343 | 40.9% | 1.931 | 0.057 |
| HADS value, range 0–24 | 0.032 | 3.3% | 1.740 | 0.085 |
| D 3 interval model (adjusted R2 = 0.143, p < 0.001) | ||||
| (Intercept) | 2.626 | - | 9.901 | <0.001 |
| Diagnosis: 1—lymphoma, 2—MM | −0.605 | −45.4% | −3.669 | <0.001 |
| Education: 1—no higher education, 2—higher education | −0.315 | −27.0% | −1.932 | 0.056 |
| Marital status: 1—married, 2—not married | 0.265 | 30.3% | 1.562 | 0.121 |
| E 4 interval model (adjusted R2 = 0.215, p < 0.001) | ||||
| (Intercept) | 3.002 | - | 7.344 | <0.001 |
| Place of residence: 1—smaller cities, 2—Vilnius/Kaunas | 0.445 | 56.1% | 2.727 | 0.008 |
| HADS scale value, range 0–24 | 0.054 | 5.6% | 3.124 | 0.002 |
| Number of specialists before correct diagnosis, range 2–10 | 0.121 | 12.9% | 2.331 | 0.022 |
| Self-medication: 1—No, 2—Yes | 0.436 | 54.7% | 2.377 | 0.019 |
| Beta Value | p Value | Odds Ratio | (95% CI) | |
|---|---|---|---|---|
| Factors included in MM 1 Complications (measured as ≤1 and >1) Regression Model | ||||
| (Intercept) | −3.875 | 0.107 | 0.019 | - |
| E 2 interval duration, range 23–1800 days | 0.003 | 0.024 | 1.003 | 1.000–1.006 |
| Gender: 1—male, 2—female | −0.752 | 0.255 | 0.471 | 0.129–1.720 |
| Age, range 19–84 years | 0.035 | 0.329 | 1.035 | 0.966–1.110 |
| CIRS index value, range 3–12 | −0.050 | 0.707 | 0.951 | 0.733–1.234 |
| Factors included in MM 1 Durie-Salmon stage (measured as 1 = 1A, 2 = IB, etc.) regression model | ||||
| (Intercept) | 0.644 | 0.218 | 1.904 | - |
| E 2 interval duration, range 23–1800 days | 0.001 | 0.049 | 1.001 | 1.000–1.001 |
| Gender: 1—male, 2—female | −0.160 | 0.261 | 0.085 | 0.644–1.127 |
| Age, range 19-84 years | 0.010 | 0.216 | 1.010 | 0.994–1.026 |
| CIRS index value, range 3–12 | 0.015 | 0.580 | 1.016 | 0.962–1.072 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dapkevičiūtė, A.; Šapoka, V.; Martynova, E.; Pečeliūnas, V. Time from Symptom Onset to Diagnosis and Treatment among Haematological Malignancies: Influencing Factors and Associated Negative Outcomes. Medicina 2019, 55, 238. https://doi.org/10.3390/medicina55060238
Dapkevičiūtė A, Šapoka V, Martynova E, Pečeliūnas V. Time from Symptom Onset to Diagnosis and Treatment among Haematological Malignancies: Influencing Factors and Associated Negative Outcomes. Medicina. 2019; 55(6):238. https://doi.org/10.3390/medicina55060238
Chicago/Turabian StyleDapkevičiūtė, Austėja, Virginijus Šapoka, Elena Martynova, and Valdas Pečeliūnas. 2019. "Time from Symptom Onset to Diagnosis and Treatment among Haematological Malignancies: Influencing Factors and Associated Negative Outcomes" Medicina 55, no. 6: 238. https://doi.org/10.3390/medicina55060238
APA StyleDapkevičiūtė, A., Šapoka, V., Martynova, E., & Pečeliūnas, V. (2019). Time from Symptom Onset to Diagnosis and Treatment among Haematological Malignancies: Influencing Factors and Associated Negative Outcomes. Medicina, 55(6), 238. https://doi.org/10.3390/medicina55060238





