What Makes Bariatric Operations Difficult–Results of a National Survey
Abstract
1. Introduction
2. Material and Methods
2.1. Study Design
2.2. Inclusion and Exclusion Criteria
2.3. Survey
- Baseline characteristics of the participant: age, sex, stage of surgical training-resident/specialist, experience in general surgery (years), experience in bariatric surgery (years), and number of performed LSGs, LRYGBs, and OAGB-MGBs.
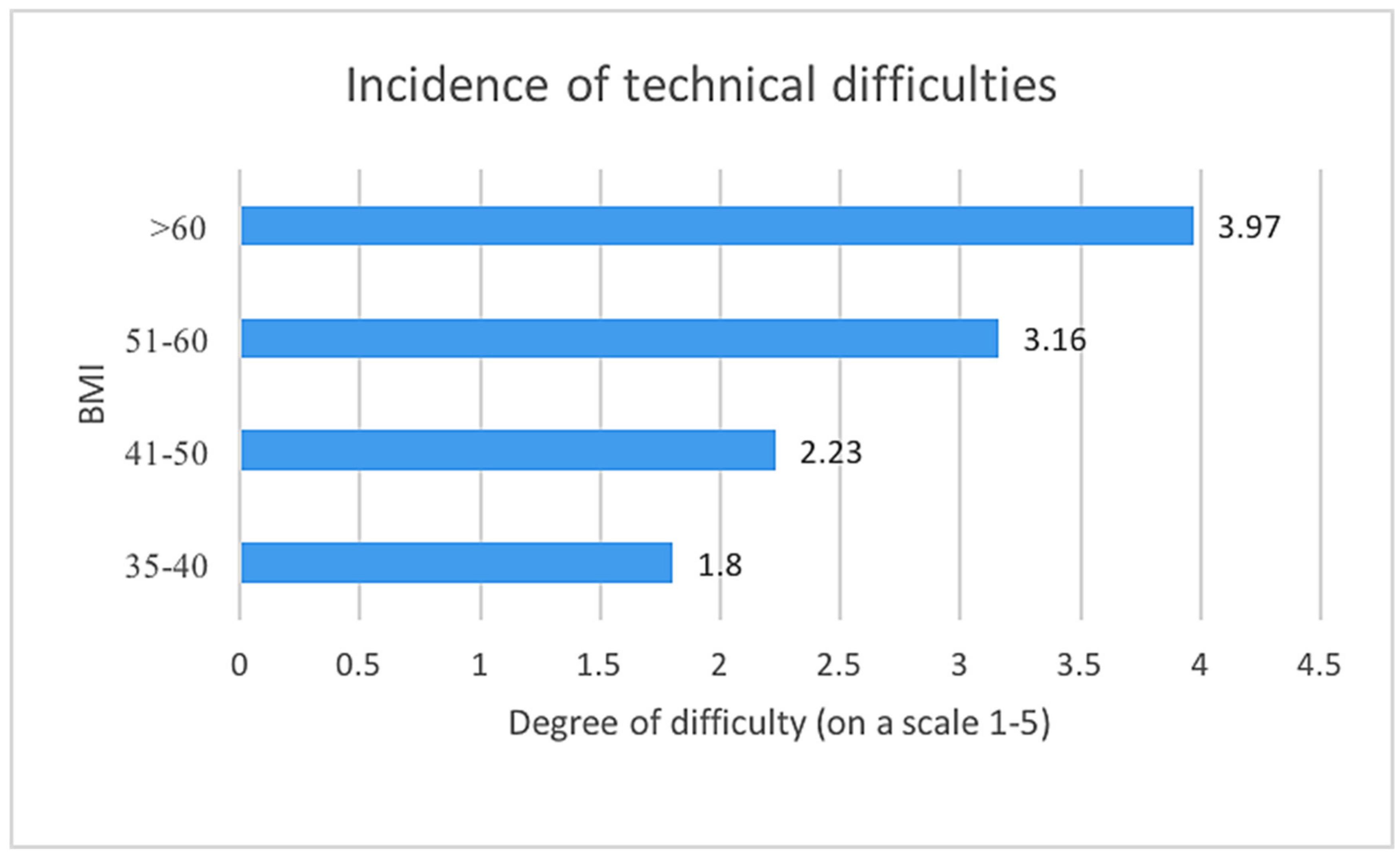
- The incidence of technical difficulties during bariatric operations in groups of patients based on the Body Mass Index (BMI) 35–40, 41–50, 51–60, and >60 (five-point Likert scale).
- Difficulty of the LSG and particular stages of this operation (five-point Likert scale) including: creation of pneumoperitoneum, visualization of the operative field, releasing the adhesions, liver retraction, dissection off the greater curvature of the stomach from the gastro-colic ligament, dissection of the short gastric vessels, calibration of the sleeve with the probe, resection of the stomach with stapler, staple line reinforcement with stitches, control of the potential hemorrhage from the staple line, leak test, removal of the resected portion of the stomach from the peritoneal cavity, and suturing the port sites. We also asked our respondents about their method for stopping bleeding from the staple line during the LSG.
- Difficulty of the LRYGB and particular stages of this operation (five-point Likert scale) including: creation of pneumoperitoneum, visualization of the operative field, releasing the adhesions, liver retraction, dissection of the fundus of the stomach, creation of the pouch, division of the jejunum into the alimentary and the enzymatic limb, creation of the gastrojejunostomy, dissection of the greater omentum, measuring the length of jejunum to create appropriate jejunojejunostomy, creation of the jejunojejunostomy, closure of the Petersen space and the intermesenteric space, and suturing the port sites. We also asked our respondents about their method for creating the gastro-jejunal anastomosis during the LRYGB.
- Difficulty of the OAGB-MGB and particular stages of this operation (five-point Likert scale) including: creation of pneumoperitoneum, visualization of the operative field, releasing the adhesions, liver retraction, dissection of the fundus of the stomach, creation of the pouch, measuring the length of jejunum to create appropriate gastrojejunostomy, creation of the gastrojejunostomy, closure of the Petersen space and the intermesenteric space, and suturing the port sites.
2.4. Statistical Analysis
2.5. Ethics Approval and Consent to Participate in the Study
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Piché, M.È.; Auclair, A.; Harvey, J.; Marceau, S.; Poirier, P. How to Choose and Use Bariatric Surgery in 2015. Can. J. Cardiol. 2015, 31, 153–166. [Google Scholar] [CrossRef] [PubMed]
- Janik, M.R.; Stanowski, E.; Paśnik, K. Present status of bariatric surgery in Poland. Wideochir. Inne. Tech. Maloinwazyjne 2016, 1, 22–25. [Google Scholar] [CrossRef]
- Walędziak, M.; Różańska-Walędziak, A.; Kowalewski, P.K.; Janik, M.R.; Brągoszewski, J.; Paśnik, K.; Bednarczyk, G.; Wallner, G.; Matłok, M. Present trends in bariatric surgery in Poland. Wideochir. Inne. Tech. Maloinwazyjne 2019, 14, 86–89. [Google Scholar] [CrossRef] [PubMed]
- SAGES guideline for clinical application of laparoscopic bariatric surgery. Surg. Endosc. 2008, 22, 2281–2300. [CrossRef]
- Fried, M.; Yumuk, V.; Oppert, J.M.; Scopinaro, N.; Torres, A.; Weiner, R.; Yashkov, Y.; Frühbeck, G.; International Federation for Surgery of Obesity and Metabolic Disorders-European Chapter (IFSO-EC); European Association for the Study of Obesity (EASO); et al. Interdisciplinary European guidelines on metabolic and bariatric surgery. Obes. Surg. 2014, 24, 42–55. [Google Scholar] [CrossRef] [PubMed]
- Budzyński, A.; Major, P.; Głuszek, S.; Kaseja, K.; Koszutski, T.; Leśniak, S.; Lewandowski, T.; Lipka, M.; Lisik, W.; Makarewicz, W.; et al. Polskie rekomendacje w zakresie chirurgii bariatrycznej i metabolicznej. Med. Prakt. Chir. 2016, 6, 13–25. [Google Scholar]
- Wyleżoł, M.; Paśnik, K.; Dąbrowiecki, S.; Głuszek, S.; Michalik, M.; Strzelczyk, J.; Wierbicki, Z.; Kwiatkowski, A.; Stanowski, E. Polish recommendations for bariatric surgery. Wideochir. Inne. Tech. Maloinwazyjne 2009, 4, 8. [Google Scholar]
- Weinstein, A.L.; Marascalchi, B.J.; Spiegel, M.A.; Saunders, J.K.; Fagerlin, A.; Parikh, M. Patient Preferences and Bariatric Surgery Procedure Selection; the Need for Shared Decision-Making. Obes. Surg. 2014, 24, 1933–1939. [Google Scholar] [CrossRef]
- Castagneto Gissey, L.; Casella Mariolo, J.R.; Mingrone, G. How to Choose the Best Metabolic Procedure? Curr. Atheroscler. Rep. 2016, 18, 43. [Google Scholar] [CrossRef]
- Major, P.; Wysocki, M.; Dworak, J.; Pedziwiatr, M.; Pisarska, M.; Wierdak, M.; Zub-Pokrowiecka, A.; Natkaniec, M.; Małczak, P.; Nowakowski, M.; et al. Analysis of Laparoscopic Sleeve Gastrectomy Learning Curve and Its Influence on Procedure Safety and Perioperative Complications. Obes. Surg. 2018, 28, 1672–1680. [Google Scholar] [CrossRef]
- Major, P.; Stefura, T.; Malczak, P.; Wysocki, M.; Witowski, J.; Kulawik, J.; Wierdak, M.; Pisarska, M.; Pędziwiatr, M.; Budzyński, A. Postoperative Care and Functional Recovery After Laparoscopic Sleeve Gastrectomy vs. Laparoscopic Roux-en-Y Gastric Bypass Among Patients Under ERAS Protocol. Obes. Surg. 2018, 28, 1031–1039. [Google Scholar] [CrossRef]
- De Luca, M.; Tie, T.; Ooi, G.; Higa, K.; Himpens, J.; Carbajo, M.A.; Mahawar, K.; Shikora, S.; Brown, W.A. Mini Gastric Bypass-One Anastomosis Gastric Bypass (MGB-OAGB)-IFSO Position Statement. Obes. Surg. 2018, 28, 1188–1206. [Google Scholar] [CrossRef]
- Rosenthal, R.J. Readmissions after bariatric surgery: Does operative technique and procedure choice matter? Surg. Obes. Relat. Dis. 2014, 10, 385–386. [Google Scholar] [CrossRef]
- Jamali, F.R.; Soweid, A.M.; Dimassi, H.; Bailey, C.; Leroy, J.; Marescaux, J. Evaluating the degree of difficulty of laparoscopic colorectal surgery. Arch. Surg. 2008, 143, 762–767. [Google Scholar] [CrossRef]
- Iwashita, Y.; Ohyama, T.; Honda, G.; Hibi, T.; Yoshida, M.; Miura, F.; Takada, T.; Han, H.S.; Hwang, T.L.; Shinya, S.; et al. What are the appropriate indicators of surgical difficulty during laparoscopic cholecystectomy? Results from a Japan-Korea-Taiwan multinational survey. J. Hepatobiliary Pancreat. Sci. 2016, 23, 533–547. [Google Scholar] [CrossRef]
- Kang, S.-B.; Park, J.-S.; Kim, D.-W.; Lee, T.-G. Intraoperative technical difficulty during laparoscopy-assisted surgery as a prognostic factor for colorectal cancer. Dis. Colon. Rectum 2010, 53, 1400–1408. [Google Scholar] [CrossRef]
- Akiyoshi, T.; Watanabe, T.; Ueno, M. Can intraoperative technical difficulty predict the long-term outcome in laparoscopic surgery for colorectal cancer? Dis. Colon. Rectum 2011, 54, e204. [Google Scholar] [CrossRef]
- Benaiges, D.; Más-Lorenzom, A.; Goday, A.; Ramon, J.M.; Chillaran, J.J.; Pedro-Botet, J.; et al. Laparoscopic sleeve gastrectomy: More than a restrictive bariatric surgery procedure? World J. Gastroenterol. 2015, 21, 11804–11814. [Google Scholar] [CrossRef]
- Ri, M.; Miyata, H.; Aikou, S.; Seto, Y.; Akazawa, K.; Takeuchi, M.; et al. Effects of body mass index (BMI) on surgical outcomes: a nationwide survey using a Japanese web-based database. Surg. Today 2015, 45, 1271–1279. [Google Scholar] [CrossRef]
- Hrabe, J.E.; Sherman, S.K.; Charlton, M.E.; Cromwell, J.W.; Byrn, J.C. Effect of BMI on outcomes in proctectomy. Dis. Colon. Rectum 2014, 57, 608–615. [Google Scholar] [CrossRef]
- Bouwman, F.; Smits, A.; Lopes, A.; Das, N.; Pollard, A.; Massuger, L.; Bekkers, R.; Galaal, K. The impact of BMI on surgical complications and outcomes in endometrial cancer surgery-an institutional study and systematic review of the literature. Gynecol. Oncol. 2015, 139, 369–376. [Google Scholar] [CrossRef]
- Wu, X.-S.; Wu, W.-G.; Li, M.-L.; Yang, J.-H.; Ding, Q.-C.; Zhang, L.; Mu, J.S.; Gu, J.; Dong, P.; Lu, J.H.; et al. Impact of being overweight on the surgical outcomes of patients with gastric cancer: a meta-analysis. World J. Gastroenterol. 2013, 19, 4596–4606. [Google Scholar] [CrossRef] [PubMed]
- Peterli, R.; Borbély, Y.; Kern, B.; Gass, M.; Peters, T.; Thurnheer, M.; Schultes, B.; Laederach, K.; Bueter, M.; Schiesser, M. Early Results of the Swiss Multicentre Bypass or Sleeve Study (SM-BOSS). Ann. Surg. 2013, 258, 690–695. [Google Scholar] [CrossRef]
- Major, P.; Wysocki, M.; Dworak, J.; Pędziwiatr, M.; Małczak, P.; Budzyński, A. Are bariatric operations performed by residents safe and efficient? Surg. Obes. Relat. Dis. 2017, 13, 614–621. [Google Scholar] [CrossRef] [PubMed]
- Blanchet, M.-C.; Gignoux, B.; Matussière, Y.; Vulliez, A.; Lanz, T.; Monier, F.; Frering, V. Experience with an Enhanced Recovery After Surgery (ERAS) Program for Bariatric Surgery: Comparison of MGB and LSG in 374 Patients. Obes. Surg. 2017, 27, 1896–1900. [Google Scholar] [CrossRef] [PubMed]
- Salama, T.M.S.; Sabry, K. Redo Surgery after Failed Open VBG: Laparoscopic Minigastric Bypass versus Laparoscopic Roux en Y Gastric Bypass-Which Is Better? Minim. Invasive. Surg. 2016, 2016, 8737519. [Google Scholar] [CrossRef][Green Version]
- Stefanidis, D.; Hope, W.W.; Korndorffer, J.R.; Markley, S.; Scott, D.J. Initial Laparoscopic Basic Skills Training Shortens the Learning Curve of Laparoscopic Suturing and Is Cost-Effective. J. Am. Coll. Surg. 2010, 210, 436–440. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Li, S.; Wang, X.; Liu, B. Intensive Laparoscopic Training Shortens the Learning Curve of Laparoscopic Suturing in Surgical Postgraduate Students: Feasible or Not? J. Endourol. 2012, 26, 895–902. [Google Scholar] [CrossRef]
- Buckley, C.E.; Kavanagh, D.O.; Nugent, E.; Ryan, D.; Traynor, O.J.; Neary, P.C. The impact of aptitude on the learning curve for laparoscopic suturing. Am. J. Surg. 2014, 207, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Kassir, R.; Gugenheim, J.; Debs, T.; Tiffet, O.; Amor, I.B.; Boutet, C. Staple Line Bleeding in Sleeve Gastrectomy: A Simple and Cost-Effective Solution. Obes. Surg. 2016, 26, 3021–3022. [Google Scholar] [CrossRef] [PubMed]
- Chakravartty, S.; Sarma, D.R.; Chang, A.; Patel, A.G. Staple Line Bleeding in Sleeve Gastrectomy—A Simple and Cost-Effective Solution. Obes. Surg. 2016, 26, 1422–1488. [Google Scholar] [CrossRef]
- Sabry, K.; Hamed, A.; Habib, H.; Helmy, M.; Abouzeid, T. Management of Acute Bleeding Post Laparoscopic Sleeve Gastrectomy. J. Obes. Weight. Loss. Ther. 2017, 7, 1–4. [Google Scholar] [CrossRef]
- Bendewald, F.P.; Choi, J.N.; Blythe, L.S.; Selzer, D.J.; Ditslear, J.H.; Mattar, S.G. Comparison of hand-sewn, linear-stapled, and circular-stapled gastrojejunostomy in laparoscopic Roux-en-Y gastric bypass. Obes. Surg. 2011, 21, 1671–1675. [Google Scholar] [CrossRef]
- Stroh, C.E.; Nesterov, G.; Weiner, R.; Benedix, F.; Knoll, C.; Pross, M.; Manger, T. Obesity Surgery Working Group; Competence Network Obesity. Circular Versus Linear Versus Hand-Sewn Gastrojejunostomy in Roux-en-Y-Gastric Bypass Influence on Weight Loss and Amelioration of Comorbidities: Data Analysis from a Quality Assurance Study of the Surgical Treatment of Obesity in Germany. Front. Surg. 2014, 1, 23. [Google Scholar]
- Sima, E.; Hedberg, J.; Ehrenborg, A.; Sundbom, M. Differences in early complications between circular and linear stapled gastrojejunostomy in laparoscopic gastric bypass. Obes. Surg. 2014, 24, 599–603. [Google Scholar] [CrossRef]
- Edholm, D.; Sundbom, M. Comparison between circular- and linear-stapled gastrojejunostomy in laparoscopic Roux-en-Y gastric bypass—A cohort from the Scandinavian Obesity Registry. Surg. Obes. Relat. Dis. 2015, 11, 1126–1233. [Google Scholar] [CrossRef]
- Major, P.; Janik, M.R.; Wysocki, M.; Waledziak, M.; Pedziwiatr, M.; Kowalewski, P.K.; Małczak, P.; Paśnik, K.; Budzyński, A. Comparison of circular- and linear-stapled gastrojejunostomy in laparoscopic Roux-en-Y gastric bypass: A multicenter study. Wideochir Inne. Tech. Maloinwazyjne 2017, 12, 140–146. [Google Scholar] [CrossRef]
| Variable | Overall n = 70 (100%) | Residents n = 19 (27.14%) | Surgeons n = 51 (72.86%) | p |
|---|---|---|---|---|
| Males, n (%) | 57 (81.43) | 10 (52.63) | 47 (92.16) | <0.01 |
| Females, n (%) | 13 (18.57) | 9 (47.37) | 4 (7.84) | |
| Age, years, mean ± SD | 41.04 ± 11.10 | 30.28 ± 2.37 | 44.92 ± 10.54 | <0.01 |
| Experience in general surgery, years, mean ± SD | 15.31 ± 11.78 | 3.92 ± 2.43 | 19.64 ± 10.99 | <0.01 |
| Experience in bariatric surgery, years, mean ± SD | 7.39 ± 5.91 | 2.82 ± 1.98 | 9.09 ± 5.99 | <0.01 |
| Number of performed LSGs, median (IQR) | 75 (20–200) | 5 (0–40) | 130 (40–230) | <0.01 |
| Number of performed LRYGBs, median (IQR) | 10 (0–50) | 0 (0–0) | 25 (2–74) | <0.01 |
| Number of performed OAGB-MGBs, median (IQR) | 2 (0–5) | 0 (0–0) | 5 (0–8) | <0.01 |
| Stage of the Operation | Overall Degree of Difficulty on a Scale 1–5 (Mean ± SD) | Degree of Difficulty Among Residents (Mean ± SD) | Degree of Difficulty Among Surgeons (Mean ± SD) | p | Correlation Between Degree of Difficulty and Years of Experience in General Surgery | |
|---|---|---|---|---|---|---|
| r | p | |||||
| Creation of pneumoperitoneum | 1.68 ± 0.78 | 1.61± 0.78 | 1.71 ± 0.78 | 0.66 | 0.11 | 0.37 |
| Visualization of the operative field | 1.77 ± 0.81 | 1.78 ± 0.73 | 1.76 ± 0.84 | 0.95 | −0.06 | 0.63 |
| Release of adhesions | 2.18 ± 0.96 | 2.39 ± 0.98 | 2.1 ± 0.95 | 0.28 | −0.06 | 0.63 |
| Liver retraction | 1.72 ± 0.83 | 1.82 ± 0.64 | 1.69 ± 0.88 | 0.56 | 0.04 | 0.75 |
| Dissection of the greater curvature of the stomach from the gastro-colic ligament | 2.14 ± 0.99 | 2.39 ± 0.78 | 2.01 ± 1.04 | 0.23 | 0.03 | 0.79 |
| Dissection of the short gastric vessels | 2.71 ± 0.99 | 3.06 ± 0.73 | 2.59 ± 1.04 | 0.08 | −0.19 | 0.13 |
| Calibration with the probe | 2.13 ± 0.97 | 2.39 ± 0.98 | 2.04 ± 0.96 | 0.19 | −0.17 | 0.18 |
| Resection of the stomach with a stapler | 2.67 ± 1.16 | 3 ± 1.03 | 2.55 ± 1.19 | 0.16 | −0.08 | 0.53 |
| Staple line reinforcement with sutures | 3.17 ± 1.19 | 3.77 ±1.03 | 2.96 ± 1.18 | 0.02 | −0.27 | 0.03 |
| Control of the potential hemorrhage from the staple line | 2.64 ± 1.11 | 3.11 ± 1.023 | 2.47 ± 1.1 | 0.03 | −0.16 | 0.18 |
| Leak test | 1.61 ± 0.79 | 1.44 ± 0.61 | 1.67 ± 0.84 | 0.31 | 0.16 | 0.20 |
| Removal of the resected portion of the stomach from the peritoneal cavity | 1.71 ± 0.73 | 1.78 ± 0.88 | 1.69 ± 0.68 | 0.65 | 0.03 | 0.80 |
| Suturing the port sites | 1.63 ± 0.86 | 1.33 ± 0.49 | 1.74 ± 0.94 | 0.09 | 0.05 | 0.67 |
| Stage of the Operation | Overall Degree of Difficulty on a Scale 1−5 (Mean ± SD) | Degree of Difficulty Among Residents (Mean ± SD) | Degree of Difficulty Among Surgeons (Mean ± SD) | p | Correlation Between Degree of Difficulty and Years of Experience in General Surgery | |
|---|---|---|---|---|---|---|
| r | p | |||||
| Creation of pneumoperitoneum | 1.69 ± 0.82 | 1.65 ± 0.86 | 1.71 ± 0.82 | 0.79 | 0.08 | 0.53 |
| Visualization of the operative field | 1.88 ± 0.83 | 2.12 ± 0.93 | 1,8 ± 0.79 | 0.18 | −0.18 | 0.17 |
| Release of adhesions | 2.33 ± 0.93 | 2.41 ± 1 | 2.3 ± 0.9 | 0.66 | 0.02 | 0.91 |
| Liver retraction | 1.85 ± 0.79 | 2.06 ± 0.75 | 1.78 ± 2.01 | 0.21 | 0.02 | 0.91 |
| Dissection of the fundus of the stomach | 2.56 ± 1.03 | 2.89 ± 0.93 | 2.43 ± 1.04 | 0.12 | −0.11 | 0.41 |
| Creation of the pouch | 3.15 ± 1.03 | 3.38 ± 0.81 | 3.07 ± 1.1 | 0.31 | −0.13 | 0.34 |
| Division of the jejunum into the alimentary and the enzymatic limbs | 3.26 ± 1.1 | 3.88 ± 0.86 | 3.02 ± 1.1 | <0.01 | −0.31 | 0.01 |
| Creation of the gastrojejunostomy | 3.68 ± 1.16 | 4.18 ± 0.88 | 3.49 ± 1.2 | 0.04 | −0.12 | 0.37 |
| Dissection of the greater omentum | 2.27 ± 0.88 | 2.59 ± 0.87 | 2.14 ± 0.86 | 0.08 | -0.06 | 0.67 |
| Measuring the length of jejunum to create appropriate jejunojejunostomy | 2.87 ± 1.02 | 3.29 ± 1.11 | 2.71 ± 1.06 | 0.06 | −0.22 | 0.08 |
| Creation of the jejunojejunostomy | 3.6 ± 1.02 | 4 ± 0.79 | 3.4 ± 1.06 | 0.05 | −0.11 | 0.39 |
| Closure of the Petersen space and the intermesenteric space | 3.18 ± 1.1 | 3.23 ± 0.97 | 3.16 ± 1.15 | 0.82 | 0.06 | 0.67 |
| Suturing the port sites | 1.7 ± 0.86 | 1.41 ± 0.51 | 1.82 ± 0.94 | 0.09 | 0.01 | 0.96 |
| Stage of the Operation | Overall Degree of Difficulty on a Scale 1–5 (Mean ± SD) | Degree of Difficulty Among Residents (Mean ± SD) | Degree of Difficulty Among Surgeons (Mean ± SD) | p | Correlation Between Degree of Difficulty and Years of Experience in General Surgery | |
|---|---|---|---|---|---|---|
| r | p | |||||
| Creation of pneumoperitoneum | 1.69 ± 0.82 | 1.39 ± 0.51 | 1.77 ± 0.82 | 0.13 | 0.09 | 0.56 |
| Visualization of the operative field | 1.87 ± 0.83 | 1.83 ± 0.84 | 1.88 ± 0.94 | 0.92 | −0.15 | 0.34 |
| Release of adhesions | 2.33 ± 0.9 | 2.39 ± 0.87 | 2.31 ± 0.93 | 0.81 | −0.17 | 0.29 |
| Liver retraction | 1.85 ± 0.79 | 2.08 ± 0.76 | 1.77 ± 0.82 | 0.25 | −0.25 | 0.11 |
| Dissection of the fundus of the stomach | 2.56 ± 1.03 | 2.77 ± 0.73 | 2.37 ± 0.89 | 0.16 | −0.32 | 0.04 |
| Creation of the pouch | 3.15 ± 1.03 | 3.31 ± 0.75 | 2.63 ± 1.03 | 0.04 | −0.41 | <0.01 |
| Measuring the length of jejunum to create appropriate gastrojejunostomy | 3.26 ± 1.1 | 3.54 ± 1.05 | 2.6 ± 1.16 | 0.02 | −0.41 | <0.01 |
| Creation of the gastrojejunostomy | 3.68 ± 1.16 | 4.08 ± 0.76 | 3.1 ± 1.13 | <0.01 | −0.49 | <0.01 |
| Closure of the Petersen space and the intermesenteric space | 3.18 ± 1.1 | 3.15 ± 0.9 | 2.74 ± 1.06 | 0.23 | 0.27 | 0.10 |
| Suturing the port sites | 1.7 ± 0.86 | 1.69 ± 0.95 | 1.83 ± 0.91 | 0.65 | −0.04 | 0.78 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Major, P.; Stefura, T.; Walędziak, M.; Janik, M.; Pędziwiatr, M.; Wysocki, M.; Rubinkiewicz, M.; Witowski, J.; Szeliga, J.; Budzyński, A. What Makes Bariatric Operations Difficult–Results of a National Survey. Medicina 2019, 55, 218. https://doi.org/10.3390/medicina55060218
Major P, Stefura T, Walędziak M, Janik M, Pędziwiatr M, Wysocki M, Rubinkiewicz M, Witowski J, Szeliga J, Budzyński A. What Makes Bariatric Operations Difficult–Results of a National Survey. Medicina. 2019; 55(6):218. https://doi.org/10.3390/medicina55060218
Chicago/Turabian StyleMajor, Piotr, Tomasz Stefura, Maciej Walędziak, Michał Janik, Michał Pędziwiatr, Michał Wysocki, Mateusz Rubinkiewicz, Jan Witowski, Jacek Szeliga, and Andrzej Budzyński. 2019. "What Makes Bariatric Operations Difficult–Results of a National Survey" Medicina 55, no. 6: 218. https://doi.org/10.3390/medicina55060218
APA StyleMajor, P., Stefura, T., Walędziak, M., Janik, M., Pędziwiatr, M., Wysocki, M., Rubinkiewicz, M., Witowski, J., Szeliga, J., & Budzyński, A. (2019). What Makes Bariatric Operations Difficult–Results of a National Survey. Medicina, 55(6), 218. https://doi.org/10.3390/medicina55060218





