Inflammatory Cytokine and Chemokine Patterns in Paediatric Patients with Suspected Serious Bacterial Infection
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Thompson, M.; Van den Bruel, A.; Verbakel, J.; Lakhanpaul, M.; Haj-Hassan, T.; Stevens, R.; Moll, H.; Buntinx, F.; Berger, M.; Aertgeerts, B.; et al. Systematic review and validation of prediction rules for identifying children with serious infections in emergency departments and urgent-access primary care. Health Technol. Assess. 2012, 16, 1–100. [Google Scholar] [CrossRef] [PubMed]
- Verbakel, J.Y.; Van den Bruel, A.; Thompson, M.; Stevens, R.; Aertgeerts, B.; Oostenbrink, R.; Moll, H.A.; Berger, M.Y.; Lakhanpaul, M.; Mant, D.; et al. How well do clinical prediction rules perform in identifying serious infections in acutely ill children across an international network of ambulatory care datasets? BMC Med. 2013, 11, 10. [Google Scholar] [CrossRef] [PubMed]
- Van den Bruel, A.; Thompson, M.J.; Haj-Hassan, T.; Stevens, R.; Moll, H.; Lakhanpaul, M.; Mant, D. Diagnostic value of laboratory tests in identifying serious infections in febrile children: Systematic review. BMJ 2011, 342, d3082. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, B.; Giroir, B.; Randolph, A. International pediatric sepsis consensus conference: Definitions for sepsis and organ dysfunction in pediatrics. Pediatr. Crit. Care Med. 2005, 6, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Seymour, C.W.; Liu, V.X.; Iwashyna, T.J.; Brunkhorst, F.M.; Rea, T.D.; Scherag, A.; Rubenfeld, G.; Kahn, J.M.; Shankar-Hari, M.; Singer, M.; et al. Assessment of Clinical Criteria for Sepsis. JAMA 2016, 315, 762. [Google Scholar] [CrossRef] [PubMed]
- Meem, M.; Modak, J.K.; Mortuza, R.; Morshed, M.; Islam, M.S.; Saha, S.K. Biomarkers for diagnosis of neonatal infections: A systematic analysis of their potential as a point-of-care diagnostics. J. Glob. Health 2011, 1, 201–209. [Google Scholar] [PubMed]
- Pierrakos, C.; Vincent, J.-L. Sepsis biomarkers: A review. Crit. Care 2010, 14, R15. [Google Scholar] [CrossRef] [PubMed]
- Nelson, G.E.; Mave, V.; Gupta, A. Biomarkers for sepsis: A review with special attention to India. Biomed. Res. Int. 2014, 2014, 264351. [Google Scholar] [CrossRef] [PubMed]
- Stensballe, L.G.; Sørup, S.; Aaby, P.; Benn, C.S.; Greisen, G.; Jeppesen, D.L.; Birk, N.M.; Kjærgaard, J.; Nissen, T.N.; Pihl, G.T.; et al. BCG vaccination at birth and early childhood hospitalisation: A randomised clinical multicentre trial. Arch. Dis. Child. 2017, 102, 224–231. [Google Scholar] [CrossRef] [PubMed]
- Kofoed, K.; Andersen, O.; Kronborg, G.; Tvede, M.; Petersen, J.; Eugen-Olsen, J.; Larsen, K. Use of plasma C-reactive protein, procalcitonin, neutrophils, macrophage migration inhibitory factor, soluble urokinase-type plasminogen activator receptor, and soluble triggering receptor expressed on myeloid cells-1 in combination to diagnose infections: A prospective study. Crit. Care 2007, 11, R38. [Google Scholar] [CrossRef] [PubMed]
- Craig, J.C.; Williams, G.J.; Jones, M.; Codarini, M.; Macaskill, P.; Hayen, A.; Irwig, L.; Fitzgerald, D.A.; Isaacs, D.; McCaskill, M. The accuracy of clinical symptoms and signs for the diagnosis of serious bacterial infection in young febrile children: Prospective cohort study of 15 781 febrile illnesses. BMJ 2010, 340, c1594. [Google Scholar] [CrossRef] [PubMed]
- Irwin, A.D.; Marriage, F.; Mankhambo, L.A.; Jeffers, G.; Kolamunnage-Dona, R.; Guiver, M.; Denis, B.; Molyneux, E.M.; Molyneux, M.E.; Day, P.J.; et al. Novel biomarker combination improves the diagnosis of serious bacterial infections in Malawian children. BMC Med. Genom. 2012, 5, 13. [Google Scholar] [CrossRef] [PubMed]
- Geiger, S.M.; Jardim-Botelho, A.; Williams, W.; Alexander, N.; Diemert, D.J.; Bethony, J.M. Serum CCL11 (eotaxin-1) and CCL17 (TARC) are serological indicators of multiple helminth infections and are driven by Schistosoma mansoni infection in humans. Trop. Med. Int. Health 2013, 18, 750–760. [Google Scholar] [CrossRef] [PubMed]
- Sharifabadi, A.R.; Hassanshahi, G.; Ghalebi, S.R.; Arababadi, M.K.; Khorramdelazad, H.; Zainodini, N.; Shabani, Z.I.B.A. All eotaxins CCL11, CCL24 and CCL26 are increased but to various extents in pulmonary tuberculosis patients. Clin. Lab. 2014, 60, 93–97. [Google Scholar] [CrossRef] [PubMed]
- Sumino, K.C.; Walter, M.J.; Mikols, C.L.; Thompson, S.A.; Gaudreault-Keener, M.; Arens, M.Q.; Agapov, E.; Hormozdi, D.; Gaynor, A.M.; Holtzman, M.J.; et al. Detection of respiratory viruses and the associated chemokine responses in serious acute respiratory illness. Thorax 2010, 65, 639–644. [Google Scholar] [CrossRef] [PubMed]
- Gathwala, G.; Walia, M.; Bala, H.; Singh, S. Recombinant Human Granulocyte Colony-stimulating Factor in Preterm Neonates with Sepsis and Relative Neutropenia: A Randomized, Single-Blind, Non-placebo-controlled Trial. J. Trop. Pediatr. 2012, 58, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Gao, M.; Zhang, L.; Liu, Y.; Yang, M.; Wang, N.; Wang, K.; Ou, D.; Liu, M.; Chen, G.; Liu, K.; et al. Use of blood urea nitrogen, creatinine, interleukin-6, granulocyte–macrophage colony stimulating factor in combination to predict the severity and outcome of abdominal sepsis in rats. Inflamm. Res. 2012, 61, 889–897. [Google Scholar] [CrossRef] [PubMed]
- Bozza, F.A.; Salluh, J.I.; Japiassu, A.M.; Soares, M.; Assis, E.F.; Gomes, R.N.; Bozza, M.T.; Castro-Faria-Neto, H.C.; Bozza, P.T. Cytokine profiles as markers of disease severity in sepsis: A multiplex analysis. Crit. Care 2007, 11, R49. [Google Scholar] [CrossRef] [PubMed]
- Suguna Narasimhulu, S.; Hendricks-Muñoz, K.D.; Borkowsky, W.; Mally, P. Usefulness of Urinary Immune Biomarkers in the Evaluation of Neonatal Sepsis. Clin. Pediatr. 2013, 52, 520–526. [Google Scholar] [CrossRef] [PubMed]
| Title 1 | Severe Bacterial Infection (SBI) Patients (n = 21) | Patients without SBI (n = 30) |
|---|---|---|
| Age, median, months (±SD) | 43.0 ± 63.9 | 30.5 ± 59.62 |
| Sex, percent (n) | 42.9% (9) males 57.1% (12) females | 63.3% (19) males 36.7% (11) females |
| Inclusion day after symptom onset, median (±SD) | 5 ± 2.48 | 3 ± 3.50 |
| C-reactive protein (CRP), median (±SD), mg/L | 131.95 ± 111.94 | 35.65 ± 61.3 |
| Length of hospitalization, median (±SD) | 8 ± 7.81 | 3 ± 2.33 |
| Antibacterial therapy | 100% (21) | 50% (15) |
| Inflammatory Cytokines, Median (min–max) pg/mL | SBI (n = 21) | Patients without SBI (n = 30) | p Value |
|---|---|---|---|
| Soluble apoptosis-stimulating fragment (sFas) | 3356.23 (1606.69–6791.45) | 3740.37 (1925.82–6832.95) | p = 0.153 |
| Soluble vascular cell adhesion molecule (sVCAM1) | 1306.07 (568.63–5042.88) | 1010.95 (392.91–4197.20) | p = 0.243 |
| Total plasminogen activator inhibitor type 1 (tPAI-1) | 147.80 (72.01–353.81) | 136.43 (56.80–327.74) | p = 0.389 |
| Interleukin 8 (IL-8) | 12.6 (1.56–158.57) | 10.2 (4.00–35.70) | p = 0.723 |
| Interleukin 10 (IL-10) | 30.10 (16.22–7127.79) | 40.35 (9.71–3365.79) | p = 0.841 |
| Interferon gamma (INF-gamma) | 16.9 (0.13–172.36) | 13.6 (0.34–838.20) | p = 0.688 |
| Tumor necrosis factor alpha (TNF-alfa) | 13.97 (0.67–100.41) | 13.99 (6.42–35.24) | p = 0.566 |
| Eotaxin | 50.23 (14.80–107.76) | 73.61 (13.50–107.76) | p = 0.035 |
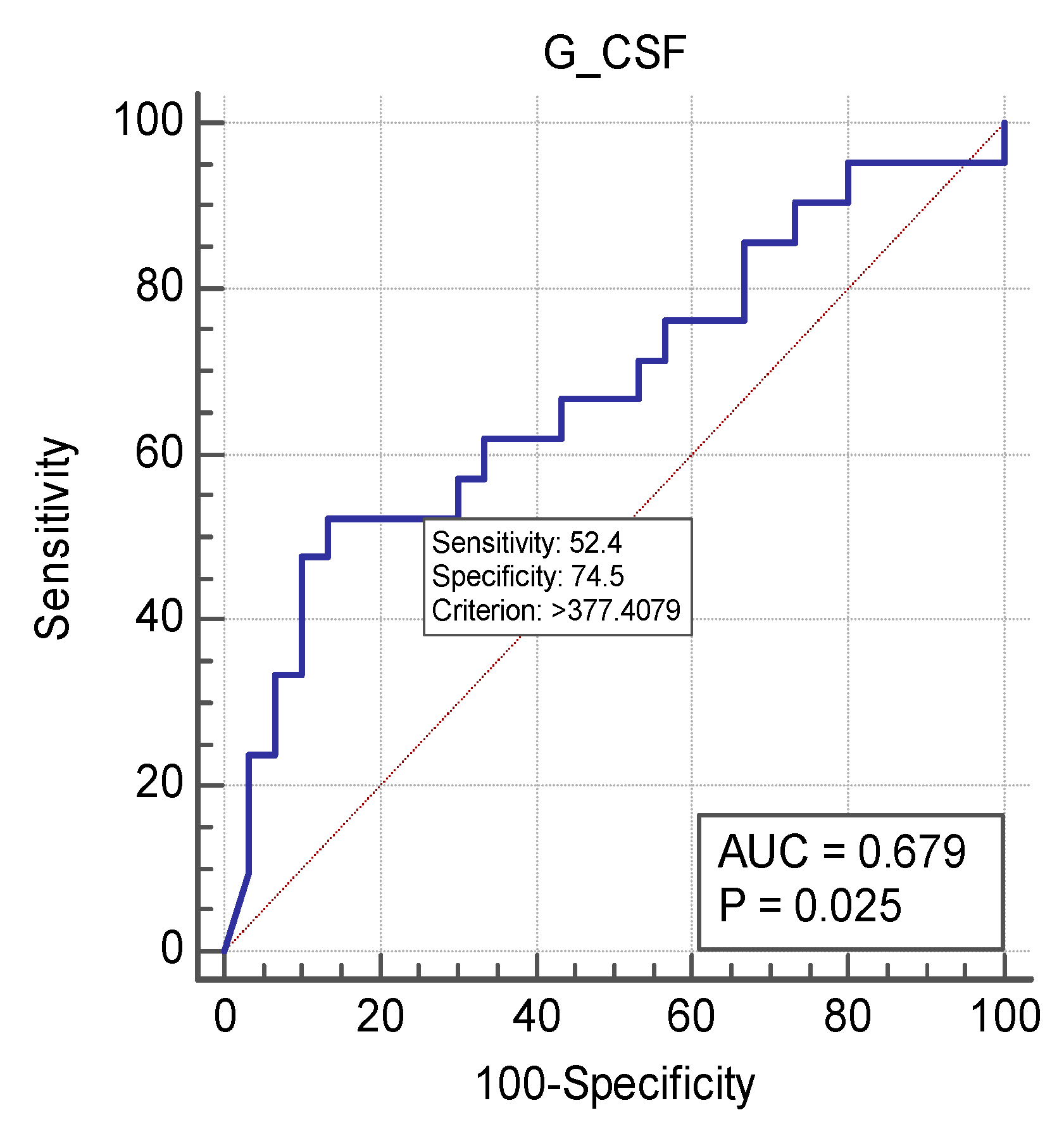
| Granulocyte colony-stimulating factor (G-CSF) | 504.69 (18.88–10,000) | 187.27 (29.19–10,000) | p = 0.031 |
| Interleukin-1 receptor antagonist (IL1ra) | 4.94 (3.20–158.60) | 16.1 (2.00–125.17) | p = 0.601 |
| Interferon-inducible protein-10 (IP10) | 977.78 (218.74–10,000) | 1070.93 (100.60–10,000) | p = 0.836 |
| Monocyte chemoattractant protein-1 (MCP1) | 319.05 (126.35–4788.12) | 411.28 (39.15–5763.23) | p = 0.168 |
| Inflammatory Cytokines, Median (min-max) pg/mL | Time of Inclusion | After 24 h | p Value |
|---|---|---|---|
| Soluble apoptosis-stimulating fragment (sFas) | 3356.23 (1606.69–6791.45) | 3530.31 (1925.82–7553.48) | p = 0.041 |
| Soluble vascular cell adhesion molecule (sVCAM1) | 1306.07 (568.63–5042.88) | 919.10 (628.18–4859.74) | p = 0.078 |
| Total plasminogen activator inhibitor type 1 (tPAI-1) | 147.80 (72.01–353.81) | 154.99 (92.44–286.00) | p = 0.383 |
| Interleukin 8 (IL-8) | 12.6 (1.56–158.57) | 8.78 (2.89–105.36) | p = 0.0383 |
| Interleukin 10 (IL-10) | 30.10 (16.22–7127.79) | 26.12 (6.47–3385.94) | p = 0.027 |
| Interferon gamma (INF-gamma) | 16.9 (0.13–172.36) | 5.18 (0.13–120.94) | p = 0.016 |
| Tumor necrosis factor alpha (TNF-alfa) | 13.97 (0.67–100.41) | 12.42 (4.74–73.12) | p = 1.000 |
| Eotaxin | 50.23 (14.80–107.76) | 64.02 (20.49–122.77) | p = 0.027 |
| Granulocyte colony-stimulating factor (G-CSF) | 504.69 (18.88–10,000) | 129.75 (29.19–2074.56) | p < 0.001 |
| Interleukin-1 receptor antagonist (IL1ra) | 4.94 (3.20–158.60) | 3.20 (1.66–77.85) | p = 0.146 |
| Interferon-inducible protein-10 (IP10) | 977.78 (218.74–10,000) | 576.579 (161.67–10,000) | p = 0.012 |
| Monocyte chemoattractant protein-1 (MCP1) | 319.05 (126.35–4788.12) | 309.16 (65.71–4327.81) | p = 0.383 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rautiainen, L.; Pavare, J.; Grope, I.; Tretjakovs, P.; Gardovska, D. Inflammatory Cytokine and Chemokine Patterns in Paediatric Patients with Suspected Serious Bacterial Infection. Medicina 2019, 55, 4. https://doi.org/10.3390/medicina55010004
Rautiainen L, Pavare J, Grope I, Tretjakovs P, Gardovska D. Inflammatory Cytokine and Chemokine Patterns in Paediatric Patients with Suspected Serious Bacterial Infection. Medicina. 2019; 55(1):4. https://doi.org/10.3390/medicina55010004
Chicago/Turabian StyleRautiainen, Linda, Jana Pavare, Ilze Grope, Peteris Tretjakovs, and Dace Gardovska. 2019. "Inflammatory Cytokine and Chemokine Patterns in Paediatric Patients with Suspected Serious Bacterial Infection" Medicina 55, no. 1: 4. https://doi.org/10.3390/medicina55010004
APA StyleRautiainen, L., Pavare, J., Grope, I., Tretjakovs, P., & Gardovska, D. (2019). Inflammatory Cytokine and Chemokine Patterns in Paediatric Patients with Suspected Serious Bacterial Infection. Medicina, 55(1), 4. https://doi.org/10.3390/medicina55010004





