A Novel Hypoxia-Immune Signature for Gastric Cancer Prognosis and Immunotherapy: Insights from Bulk and Single-Cell RNA-Seq
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients’ Cohort and Preparation
2.2. Identification of Hypoxia- and Immune-Related Genes and Development Risk Signature
2.3. Identification of the Relationship Between Risk Scores and Clinical Factors
2.4. In-Depth Analysis of Molecular and Immunological Features in Different Risk Score Groups
2.5. The Ability of Gene Signatures to Predict Immunotherapy Response
2.6. Single Cell RNA-Sequencing (scRNA-Seq) Analysis of Gene Signature
2.7. Statistical Analysis
3. Results
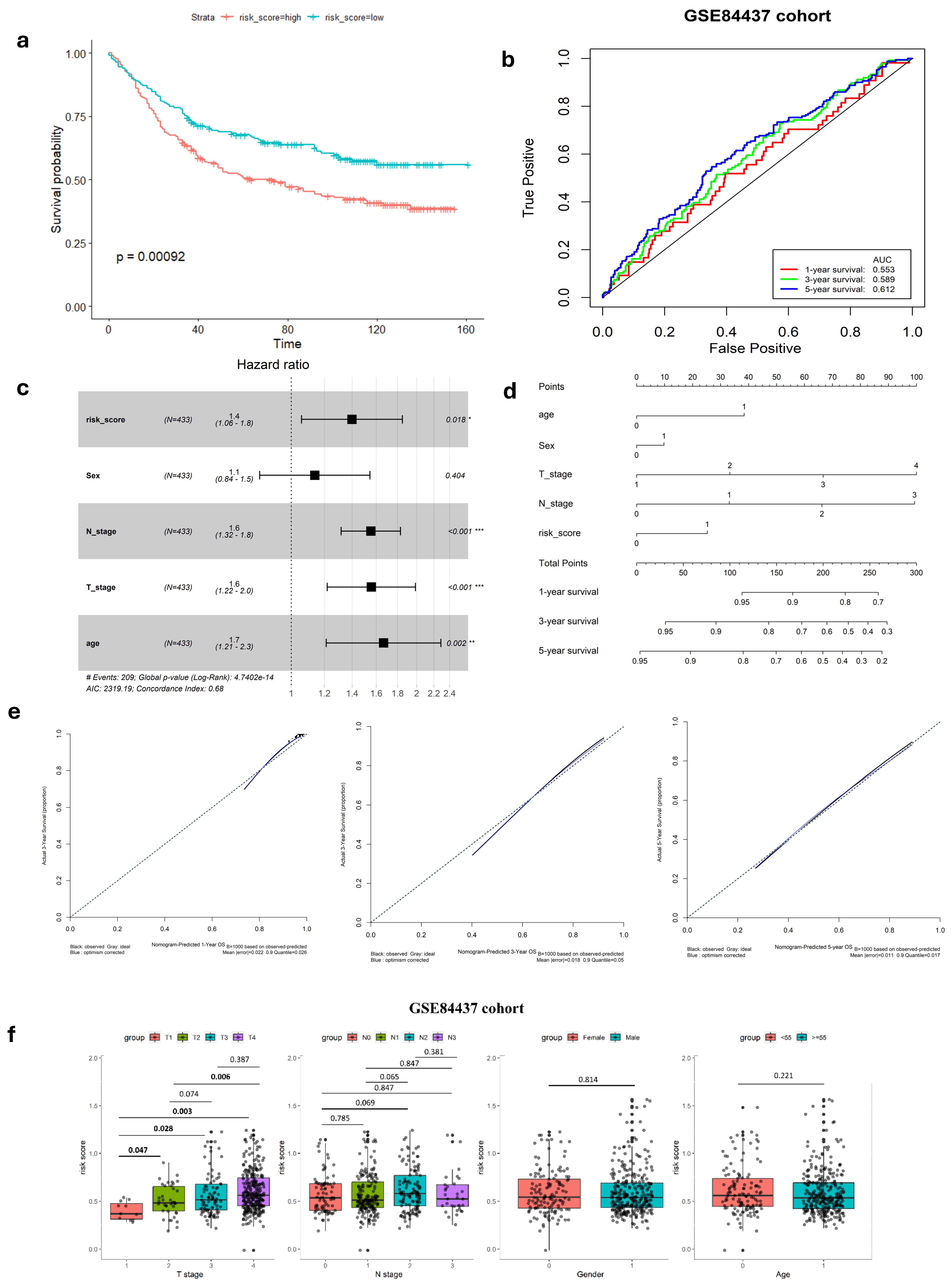
3.1. Development and Validation of Hypoxia- and Immune-Related Gene Signatures
[Expression level of SERPINE1 × 7.965 × 10−6] + [Expression level of GPC3 × 6.999 × 10−6] + [Expression level
of SRPX × 6.395 × 10−5].
3.2. Relationship Between Gene Signature and Clinicopathological Parameters
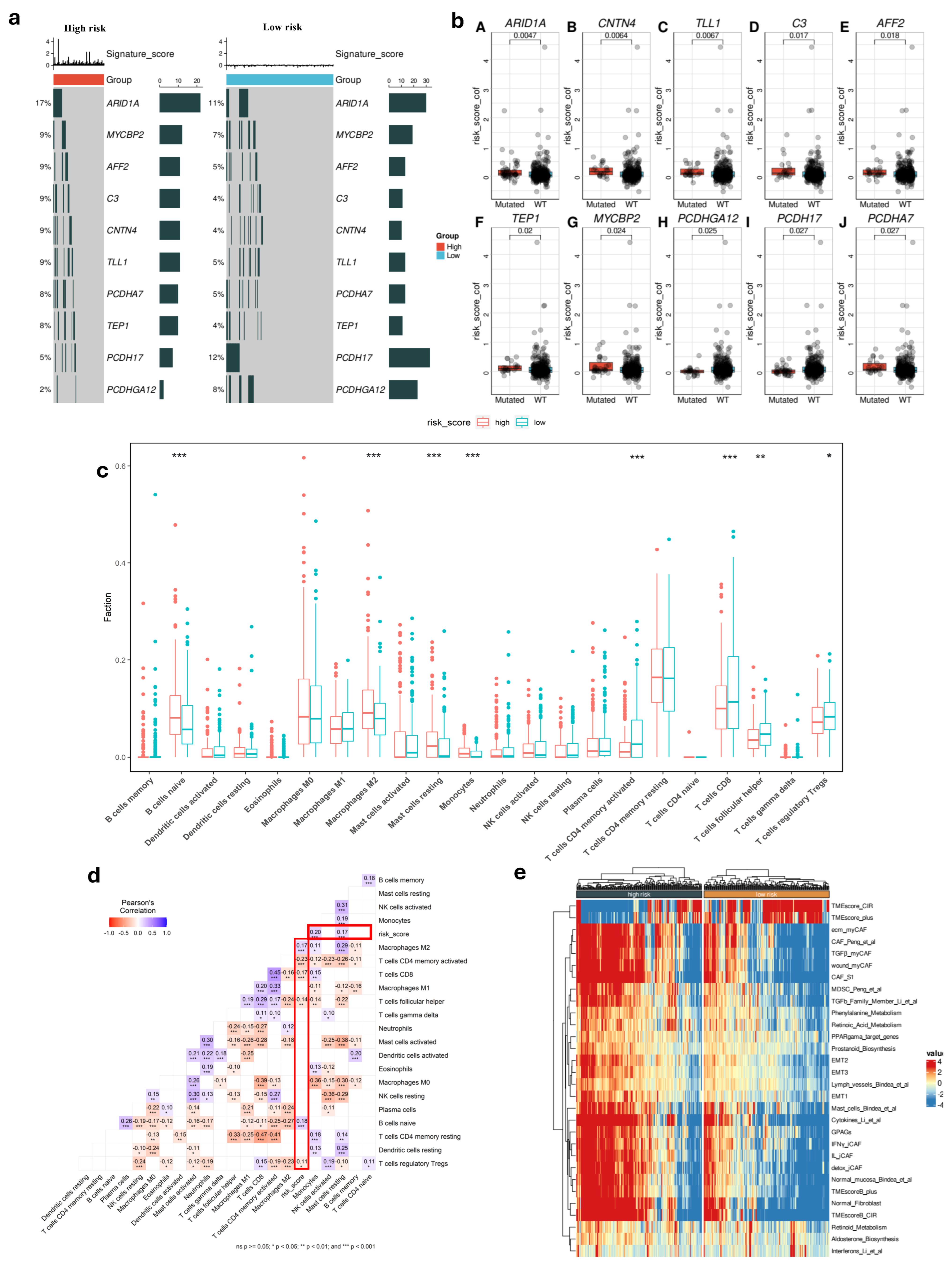
3.3. Microenvironment of Different Risk-Score Groups
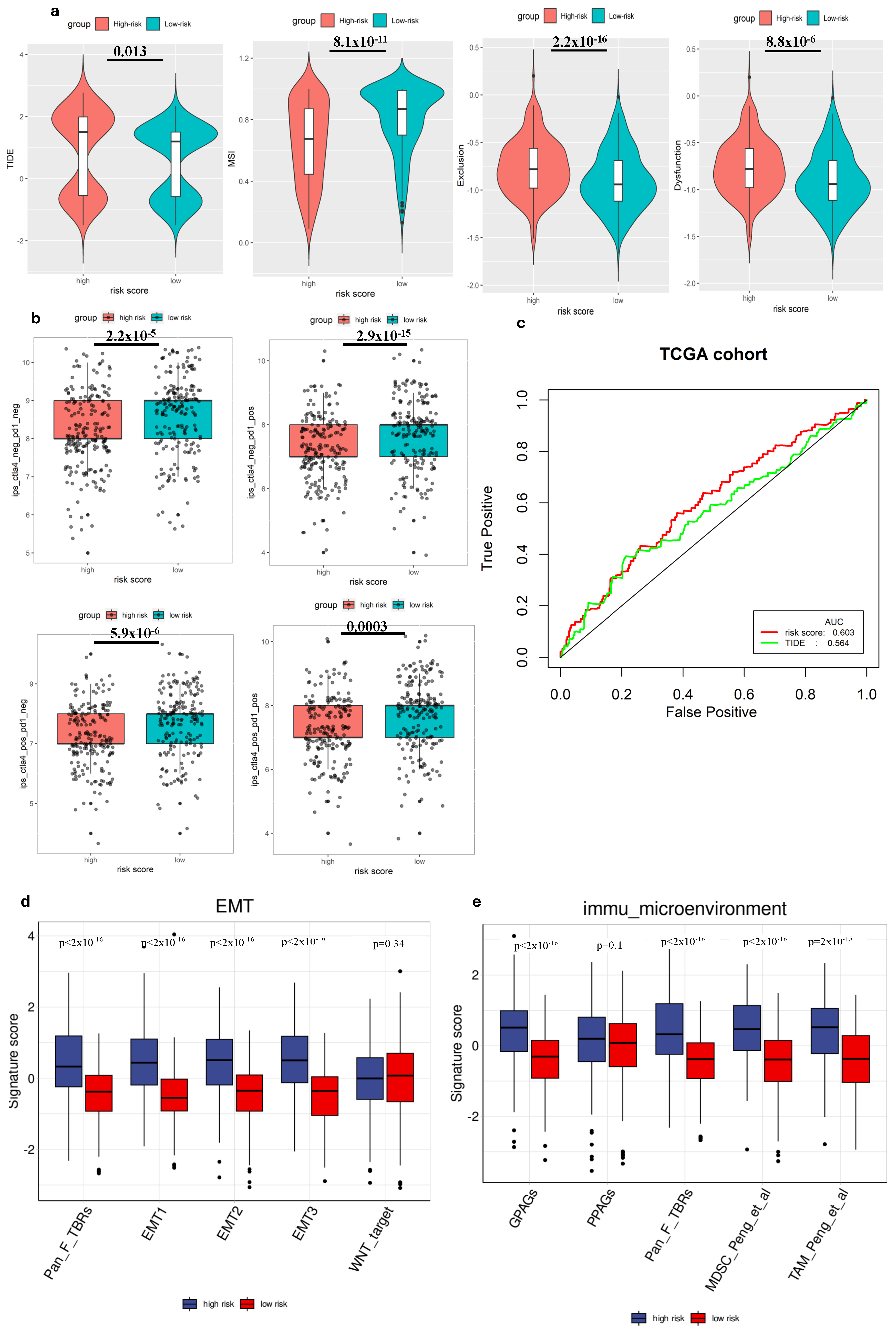
3.4. The Ability to Predict Immunotherapy Response of Gene Signature
3.5. Gene Signature and Tumor Biology
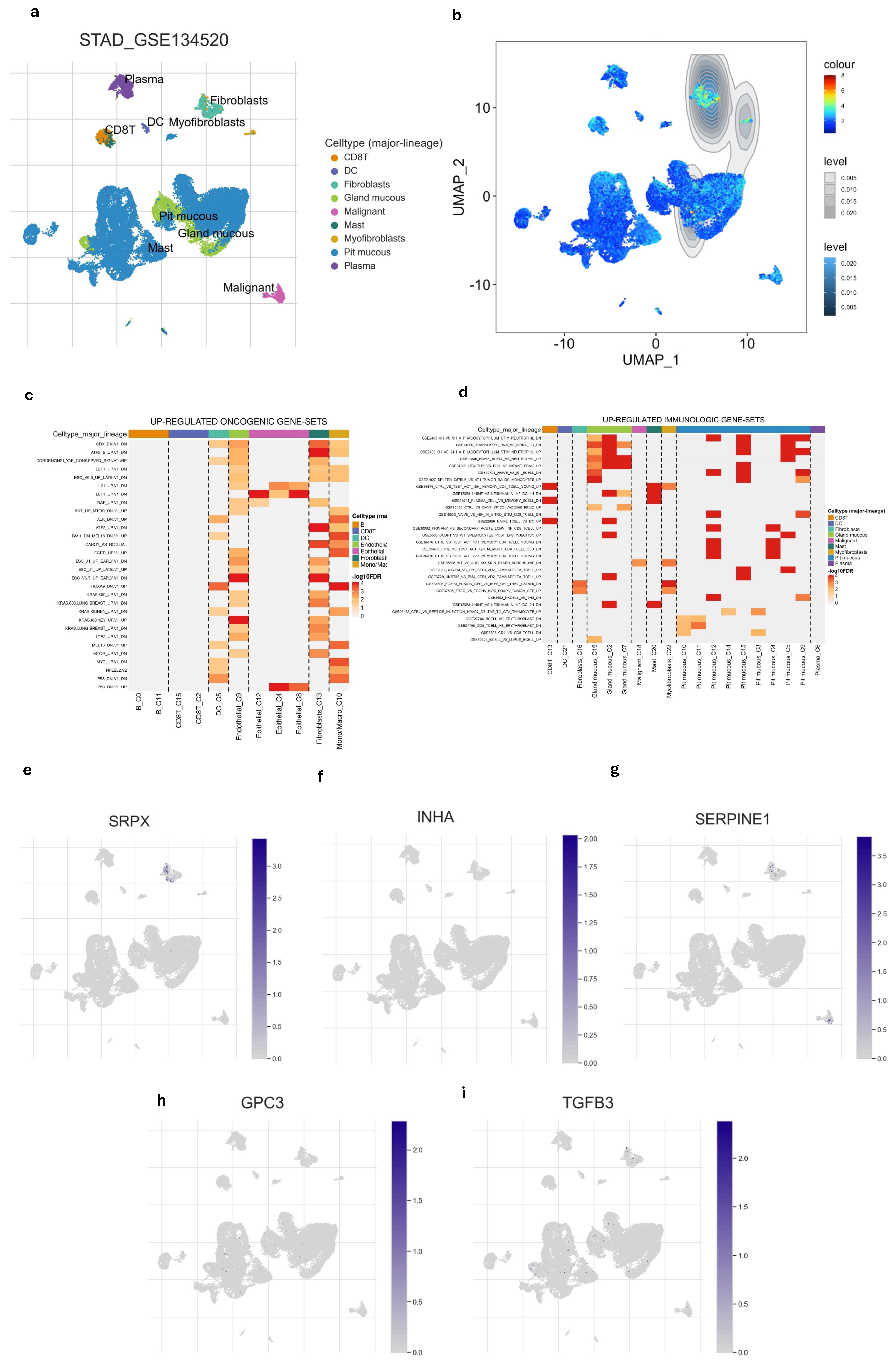
3.6. Single-Cell Profiling of Gene Signature
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Thrift, A.P.; El-Serag, H.B. Burden of Gastric Cancer. Clin. Gastroenterol. Hepatol. 2020, 18, 534–542. [Google Scholar] [CrossRef] [PubMed]
- Smyth, E.C.; Nilsson, M.; Grabsch, H.I.; van Grieken, N.C.; Lordick, F. Gastric cancer. Lancet 2020, 396, 635–648. [Google Scholar] [CrossRef] [PubMed]
- Guan, W.-L.; He, Y.; Xu, R.-H. Gastric cancer treatment: Recent progress and future perspectives. J. Hematol. Oncol. 2023, 16, 57. [Google Scholar] [CrossRef]
- Sharma, P.; Hu-Lieskovan, S.; Wargo, J.A.; Ribas, A. Primary, adaptive, and acquired resistance to cancer immunotherapy. Cell 2017, 168, 707–723. [Google Scholar] [CrossRef]
- Ivan, M.; Fishel, M.L.; Tudoran, O.M.; Pollok, K.E.; Wu, X.; Smith, P.J. Hypoxia signaling: Challenges and opportunities for cancer therapy. Semin. Cancer Biol. 2022, 85, 185–195. [Google Scholar] [CrossRef]
- Muz, B.; de la Puente, P.; Azab, F.; Azab, A.K. The role of hypoxia in cancer progression, angiogenesis, metastasis, and resistance to therapy. Hypoxia 2015, 3, 83–92. [Google Scholar] [CrossRef]
- Harris, A.L. Hypoxia—A key regulatory factor in tumour growth. Nat. Rev. Cancer 2002, 2, 38–47. [Google Scholar] [CrossRef]
- Gilkes, D.M.; Semenza, G.L.; Wirtz, D. Hypoxia and the extracellular matrix: Drivers of tumour metastasis. Nat. Rev. Cancer 2014, 14, 430–439. [Google Scholar] [CrossRef]
- Wicks, E.E.; Semenza, G.L. Hypoxia-inducible factors: Cancer progression and clinical translation. J. Clin. Investig. 2022, 132, e159839. [Google Scholar] [CrossRef]
- Li, M.; Li, G.; Yang, X.; Yin, W.; Lv, G.; Wang, S. HIF in Gastric Cancer: Regulation and Therapeutic Target. Molecules 2022, 27, 4893. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Xu, J.; Xie, J.; Yang, W. Research progress in targeted therapy and immunotherapy for gastric cancer. Chin. Med. J. 2022, 135, 1299–1313. [Google Scholar] [CrossRef] [PubMed]
- Jin, X.; Liu, Z.; Yang, D.; Yin, K.; Chang, X. Recent Progress and Future Perspectives of Immunotherapy in Advanced Gastric Cancer. Front. Immunol. 2022, 13, 948647. [Google Scholar] [CrossRef] [PubMed]
- Leone, R.D.; Powell, J.D. Metabolism of immune cells in cancer. Nat. Rev. Cancer 2020, 20, 516–531. [Google Scholar] [CrossRef]
- Zhang, A.Z.; Yuan, X.; Liang, W.H.; Zhang, H.J.; Li, Y.; Xie, Y.F.; Li, J.F.; Jiang, C.H.; Li, F.P.; Shen, X.H.; et al. Immune infiltration in gastric cancer microenvironment and its clinical significance. Front. Cell Dev. Biol. 2022, 9, 762029. [Google Scholar] [CrossRef]
- Zhang, C.; Liu, T.; Wang, J.; Zhang, J. Development and verification of an immune-related gene prognostic index for gastric cancer. Sci. Rep. 2022, 12, 15693. [Google Scholar] [CrossRef]
- Zhou, K.; Cai, C.; Ding, G.; He, Y.; Hu, D. A signature of six-hypoxia-related genes to evaluate the tumor immune microenvironment and predict prognosis in gastric cancer. BMC Med. Genom. 2022, 15, 261. [Google Scholar] [CrossRef]
- Breuer, K.; Foroushani, A.K.; Laird, M.R.; Chen, C.; Sribnaia, A.; Lo, R.; Winsor, G.L.; Hancock, R.E.W.; Brinkman, F.S.L.; Lynn, D.J. InnateDB: Systems biology of innate immunity and beyond—Recent updates and continuing curation. Nucleic Acids Res. 2013, 41, D1228–D1233. [Google Scholar] [CrossRef]
- Liberzon, A.; Birger, C.; Thorvaldsdóttir, H.; Ghandi, M.; Mesirov, J.P.; Tamayo, P. The Molecular Signatures Database (MSigDB) hallmark gene set collection. Cell Syst. 2015, 1, 417–425. [Google Scholar] [CrossRef]
- Jia, A.; Xu, L.; Wang, Y. Venn diagrams in bioinformatics. Brief. Bioinform. 2021, 22, bbab108. [Google Scholar] [CrossRef]
- Holleczek, B.; Brenner, H. Model based period analysis of absolute and relative survival with R: Data preparation, model fitting and derivation of survival estimates. Comput. Methods Programs Biomed. 2013, 110, 192–202. [Google Scholar] [CrossRef] [PubMed]
- Rich, J.T.; Neely, J.G.; Paniello, R.C.; Voelker, C.C.; Nussenbaum, B.; Wang, E.W. A practical guide to understanding Kaplan-Meier curves. Otolaryngol. Head Neck Surg. 2010, 143, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Heagerty, P.J.; Lumley, T.; Pepe, M.S. Time-dependent ROC curves for censored survival data and a diagnostic marker. Biometrics 2000, 56, 337–344. [Google Scholar] [CrossRef]
- Steyerberg, E.; Frank, E.H., Jr. Regression Modeling Strategies: With Applications, to Linear Models, Logistic and Ordinal Regression, and Survival Analysis, 2nd ed. Heidelberg: Springer. Biometrics 2016, 72, 1006–1007. [Google Scholar] [CrossRef]
- Mayakonda, A.; Lin, D.-C.; Assenov, Y.; Plass, C.; Koeffler, H.P. Maftools: Efficient and comprehensive analysis of somatic variants in cancer. Genome Res. 2018, 28, 1747–1756. [Google Scholar] [CrossRef]
- Colaprico, A.; Silva, T.C.; Olsen, C.; Garofano, L.; Cava, C.; Garolini, D.; Sabedot, T.S.; Malta, T.M.; Pagnotta, S.M.; Castiglioni, I.; et al. TCGAbiolinks: An R/Bioconductor package for integrative analysis of TCGA data. Nucleic Acids Res. 2016, 44, e71. [Google Scholar] [CrossRef]
- Charoentong, P.; Finotello, F.; Angelova, M.; Mayer, C.; Efremova, M.; Rieder, D.; Hackl, H.; Trajanoski, Z. Pan-cancer Immunogenomic Analyses Reveal Genotype-Immunophenotype Relationships and Predictors of Response to Checkpoint Blockade. Cell Rep. 2017, 18, 248–262. [Google Scholar] [CrossRef]
- Jiang, P.; Gu, S.; Pan, D.; Fu, J.; Sahu, A.; Hu, X.; Li, Z.; Traugh, N.; Bu, X.; Li, B.; et al. Signatures of T cell dysfunction and exclusion predict cancer immunotherapy response. Nat. Med. 2018, 24, 1550–1558. [Google Scholar] [CrossRef]
- Huang, Q.; Liu, Y.; Du, Y.; Garmire, L.X. Evaluation of cell type annotation R packages on single-cell RNA-seq data. Genom. Proteom. Bioinform. 2021, 19, 267–281. [Google Scholar] [CrossRef]
- Dai, Y.; Qiang, W.; Lin, K.; Gui, Y.; Lan, X.; Wang, D. An immune-related gene signature for predicting survival and immunotherapy efficacy in hepatocellular carcinoma. Cancer Immunol Immunother. 2021, 70, 967–979. [Google Scholar] [CrossRef]
- Thrift, A.P.; Wenker, T.N.; El-Serag, H.B. Global burden of gastric cancer: Epidemiological trends, risk factors, screening and prevention. Nat. Rev. Clin. Oncol. 2023, 20, 338–349. [Google Scholar] [CrossRef]
- Ozcan, G. The hypoxia-inducible factor-1α in stemness and resistance to chemotherapy in gastric cancer: Future directions for therapeutic targeting. Front. Cell Dev. Biol. 2023, 11, 1082057. [Google Scholar] [CrossRef] [PubMed]
- Ucaryilmaz Metin, C.; Ozcan, G. The HIF-1α as a Potent Inducer of the Hallmarks in Gastric Cancer. Cancers 2022, 14, 2711. [Google Scholar] [CrossRef] [PubMed]
- Taylor, C.T.; Scholz, C.C. The effect of HIF on metabolism and immunity. Nat. Rev. Nephrol. 2022, 18, 573–587. [Google Scholar] [CrossRef]
- Corrado, C.; Fontana, S. Hypoxia and HIF Signaling: One Axis with Divergent Effects. Int. J. Mol. Sci. 2020, 21, 5611. [Google Scholar] [CrossRef]
- Han, Y.K.; Park, G.Y.; Bae, M.J.; Kim, J.S.; Jo, W.S.; Lee, C.G. Hypoxia induces immunogenic cell death of cancer cells by enhancing the exposure of cell surface calreticulin in an endoplasmic reticulum stress-dependent manner. Oncol. Lett. 2019, 18, 6269–6274. [Google Scholar] [CrossRef]
- Liu, Y.; Wu, J.; Huang, W.; Weng, S.; Wang, B.; Chen, Y.; Wang, H. Development and validation of a hypoxia-immune-based microenvironment gene signature for risk stratification in gastric cancer. J. Transl. Med. 2020, 18, 201. [Google Scholar] [CrossRef]
- Sukri, A.; Hanafiah, A.; Kosai, N.R. The Roles of Immune Cells in Gastric Cancer: Anti-Cancer or Pro-Cancer? Cancers 2022, 14, 3922. [Google Scholar] [CrossRef]
- Xie, Q.; Ding, J.; Chen, Y. Role of CD8+ T lymphocyte cells: Interplay with stromal cells in tumor microenvironment. Acta Pharm. Sin. B 2021, 11, 1365–1378. [Google Scholar] [CrossRef]
- van der Leun, A.M.; Thommen, D.S.; Schumacher, T.N. CD8+ T cell states in human cancer: Insights from single-cell analysis. Nat. Rev. Cancer 2020, 20, 218–232. [Google Scholar] [CrossRef]
- Matsumoto, H.; Thike, A.A.; Li, H.; Yeong, J.; Koo, S.-L.; Dent, R.A.; Tan, P.H.; Iqbal, J. Increased CD4 and CD8-positive T cell infiltrate signifies good prognosis in a subset of triple-negative breast cancer. Breast Cancer Res. Treat. 2016, 156, 237–247. [Google Scholar] [CrossRef] [PubMed]
- Angelico, G.; Attanasio, G.; Colarossi, L.; Colarossi, C.; Montalbano, M.; Aiello, E.; Vendra, F.D.; Mare, M.; Orsi, N.; Memeo, L. ARID1A Mutations in Gastric Cancer: A Review with Focus on Clinicopathological Features, Molecular Background and Diagnostic Interpretation. Cancers 2024, 16, 2062. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; Wang, S.C.; Wei, Y.; Luo, X.; Jia, Y.; Li, L.; Gopal, P.; Zhu, M.; Nassour, I.; Chuang, J.-C.; et al. Arid1a has context-dependent oncogenic and tumor suppressor functions in liver cancer. Cancer Cell 2017, 32, 574–589.e6. [Google Scholar] [CrossRef] [PubMed]
- Bu, X.; Chen, Z.; Zhang, A.; Zhou, X.; Zhang, X.; Yuan, H.; Zhang, Y.; Yin, C.; Yan, Y. Circular RNA circAFF2 accelerates gastric cancer development by activating miR-6894–5p and regulating ANTXR 1 expression. Clin. Res. Hepatol. Gastroenterol. 2021, 45, 101671. [Google Scholar] [CrossRef]
- Gong, L.; Xia, Y.; Qian, Z.; Shi, J.; Luo, J.; Song, G.; Xu, J.; Ye, Z. Overexpression of MYC binding protein promotes invasion and migration in gastric cancer. Oncol. Lett. 2018, 15, 5243–5249. [Google Scholar] [CrossRef]
- Yuan, K.; Ye, J.; Liu, Z.; Ren, Y.; He, W.; Xu, J.; He, Y.; Yuan, Y. Complement C3 overexpression activates JAK2/STAT3 pathway and correlates with gastric cancer progression. J. Exp. Clin. Cancer Res. 2020, 39, 9. [Google Scholar] [CrossRef]
- Cai, H.; Li, M.; Deng, R.; Wang, M.; Shi, Y. Advances in molecular biomarkers research and clinical application progress for gastric cancer immunotherapy. Biomark. Res. 2022, 10, 67. [Google Scholar] [CrossRef]
- Shitara, K.; Van Cutsem, E.; Bang, Y.-J.; Fuchs, C.; Wyrwicz, L.; Lee, K.-W.; Kudaba, I.; Garrido, M.; Chung, H.C.; Lee, J.; et al. Efficacy and Safety of Pembrolizumab or Pembrolizumab Plus Chemotherapy vs Chemotherapy Alone for Patients With First-line, Advanced Gastric Cancer: The KEYNOTE-062 Phase 3 Randomized Clinical Trial. JAMA Oncol. 2020, 6, 1571–1580. [Google Scholar] [CrossRef]
- Klempner, S.J.; Fabrizio, D.; Bane, S.; Reinhart, M.; Peoples, T.; Ali, S.M.; Sokol, E.S.; Frampton, G.; Schrock, A.B.; Anhorn, R.; et al. Tumor Mutational Burden as a Predictive Biomarker for Response to Immune Checkpoint Inhibitors: A Review of Current Evidence. Oncologist 2020, 25, e147–e159. [Google Scholar] [CrossRef]
- Hou, W.; Zhao, Y.; Zhu, H. Predictive Biomarkers for Immunotherapy in Gastric Cancer: Current Status and Emerging Prospects. Int. J. Mol. Sci. 2023, 24, 15321. [Google Scholar] [CrossRef] [PubMed]
- Alkasalias, T.; Moyano-Galceran, L.; Arsenian-Henriksson, M.; Lehti, K. Fibroblasts in the tumor microenvironment: Shield or spear? Int. J. Mol. Sci. 2018, 19, 1532. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, K.; Arao, T.; Maegawa, M.; Matsumoto, K.; Kaneda, H.; Kudo, K.; Fujita, Y.; Yokote, H.; Yanagihara, K.; Yamada, Y.; et al. SRPX2 is overexpressed in gastric cancer and promotes cellular migration and adhesion. Int. J. Cancer 2009, 124, 1072–1080. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Yin, Z.; Song, W.; He, B.; Zhang, W. Sushi-Repeat-Containing Protein X-Linked 2: A Potential Therapeutic Target for Inflammation and Cancer Therapy. J. Immunol. Res. 2022, 2022, 2931214. [Google Scholar] [CrossRef]

| Factors | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|
| HR | 95%CI | p-Value | HR | 95%CI | p-Value | |
| TCGA cohort | ||||||
| Age | 1.52 | 1.094–2.113 | 0.0125 * | 1.773 | 1.2707–2.475 | 0.000754 *** |
| Gender (male vs. female) | 1.232 | 0.8774–1.73 | 0.228 | 1.201 | 0.8532–1.689 | 0.294109 |
| T stage | 1.306 | 1.072–1.591 | 0.00797 ** | 1.238 | 1.0004–1.533 | 0.049602 * |
| N stage | 1.379 | 1.196–1.59 | 9.78 × 10−6 *** | 1.312 | 1.1312–1.521 | 0.000328 *** |
| Risk score (high vs. low) | 1.818 | 1.314–2.514 | 0.000305 *** | 1.854 | 1.3381–2.569 | 0.000208 *** |
| GSE84437 cohort | ||||||
| Age | 1.02 | 1.007–1.032 | 0.00225 ** | 1.023 | 1.0108–1.036 | 0.000244 *** |
| Gender (male vs. female) | 1.256 | 0.9275–1.7 | 0.141 | 1.184 | 0.8726–1.606 | 0.278218 |
| T stage | 1.74 | 1.378–2.198 | 3.31 × 10−6 *** | 1.583 | 1.2385–2.024 | 0.000246 *** |
| N stage | 1.676 | 1.429–1.967 | 2.42 × 10−10 *** | 1.515 | 1.2871–1.782 | 5.72 × 10−7 *** |
| Risk score (high vs. low) | 1.589 | 1.206–2.094 | 0.00101 ** | 1.395 | 1.0562–1.843 | 0.019045 * |
| TCGA Cohort | GSE84437 Cohort | |||||||
|---|---|---|---|---|---|---|---|---|
| Total (N = 404) | Low Risk (N = 202) | High Risk (N = 202) | p-Value | Total (N = 433) | High Risk (N = 216) | Low Risk (N = 217) | p-Value | |
| Gender | ||||||||
| Male | 261 (64.6%) | 134 (66.3%) | 127 (62.9%) | 0.5325 | 296 (68.4%) | 147 (68.1%) | 149 (68.7%) | 0.892 |
| Female | 143 (35.4%) | 68 (33.7%) | 75 (37.1%) | 137 (31.6%) | 69 (31.9%) | 68 (31.3%) | ||
| Age | ||||||||
| <55 | 67 (16.6%) | 30 (14.9%) | 37 (18.2%) | 0.4222 | 129 (28.9%) | 69 (31.9%) | 60 (27.6%) | 0.329 |
| ≥55 | 337 (83.4%) | 172 (85.1%) | 165 (81.7%) | 304 (70.2%) | 147 (68.1%) | 157 (72.4%) | ||
| N stage | ||||||||
| N0 | 125 (30.9%) | 66 (32.7%) | 59 (29.2%) | 0.4545 | 80 (18.5%) | 39 (18.1%) | 41 (18.9%) | 0.011 * |
| N1 | 114 (28.2%) | 59 (29.2%) | 55 (27.2%) | 188 (43.4%) | 80 (37%) | 108 (49.8%) | ||
| N2 | 82 (20.3%) | 42 (20.8%) | 40 (19.8%) | 132 (30.5%) | 81 (37.5%) | 51 (23.5%) | ||
| N3 | 83 (20.5%) | 35 (17.3%) | 48 (23.8%) | 33 (7.6%) | 16 (7.4%) | 17 (7.8%) | ||
| T stage | ||||||||
| T1 | 22 (5.4%) | 16 (7.9%) | 6 (3%) | 0.0222 * | 11 (2.5%) | 1 (0.5%) | 10 (4.6%) | 0.001 *** |
| T2 | 90 (22.3%) | 41 (20.3%) | 49 (24.3%) | 38 (8.8%) | 13 (6.0%) | 25 (11.5%) | ||
| T3 | 182 (45%) | 99 (49%) | 83 (41.1%) | 92 (21.2%) | 40 (18.5%) | 52 (24%) | ||
| T4 | 110 (27.2%) | 46 (22.8%) | 64 (31.7%) | 292 (67.4%) | 162 (75%) | 130 (59.9%) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nguyen, M.H.; Ta, H.D.K.; Nguyen, D.P.Q.; Le, V.H.; Le, N.Q.K. A Novel Hypoxia-Immune Signature for Gastric Cancer Prognosis and Immunotherapy: Insights from Bulk and Single-Cell RNA-Seq. Curr. Issues Mol. Biol. 2025, 47, 552. https://doi.org/10.3390/cimb47070552
Nguyen MH, Ta HDK, Nguyen DPQ, Le VH, Le NQK. A Novel Hypoxia-Immune Signature for Gastric Cancer Prognosis and Immunotherapy: Insights from Bulk and Single-Cell RNA-Seq. Current Issues in Molecular Biology. 2025; 47(7):552. https://doi.org/10.3390/cimb47070552
Chicago/Turabian StyleNguyen, Mai Hanh, Hoang Dang Khoa Ta, Doan Phuong Quy Nguyen, Viet Huan Le, and Nguyen Quoc Khanh Le. 2025. "A Novel Hypoxia-Immune Signature for Gastric Cancer Prognosis and Immunotherapy: Insights from Bulk and Single-Cell RNA-Seq" Current Issues in Molecular Biology 47, no. 7: 552. https://doi.org/10.3390/cimb47070552
APA StyleNguyen, M. H., Ta, H. D. K., Nguyen, D. P. Q., Le, V. H., & Le, N. Q. K. (2025). A Novel Hypoxia-Immune Signature for Gastric Cancer Prognosis and Immunotherapy: Insights from Bulk and Single-Cell RNA-Seq. Current Issues in Molecular Biology, 47(7), 552. https://doi.org/10.3390/cimb47070552






