Genetic Signatures for Distinguishing Chemo-Sensitive from Chemo-Resistant Responders in Prostate Cancer Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Archived Biopsy Samples
2.2. Conducting Microtomy and RNA Extraction
2.3. Quantitative Reverse Transcription-Polymerase Chain Reaction (qRT-PCR)
2.4. Signaling Pathway Enrichment
2.5. Protein–Protein Interaction Network Analysis
2.6. Molecular Docking Analysis
2.7. Statistical Analysis
3. Results
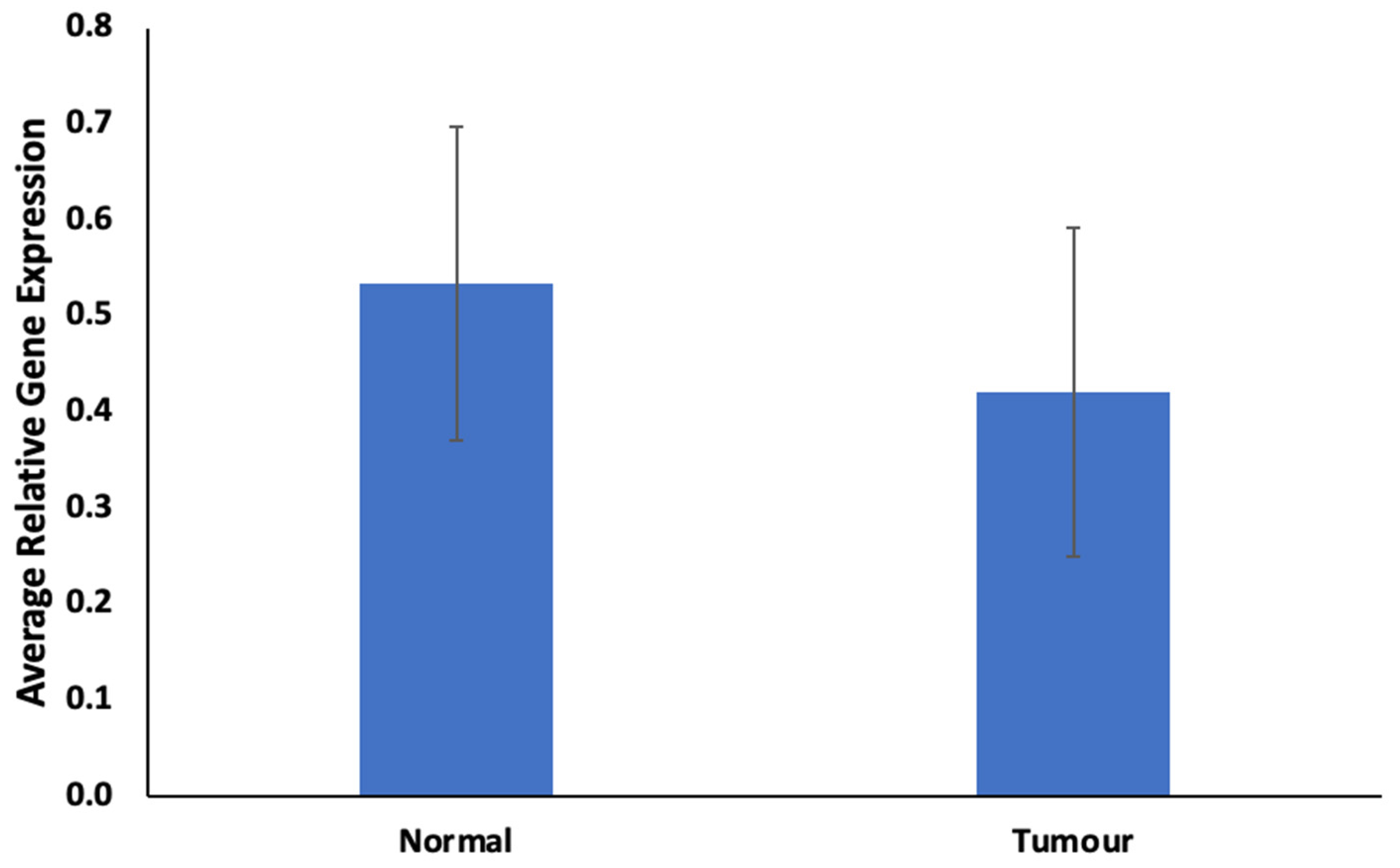
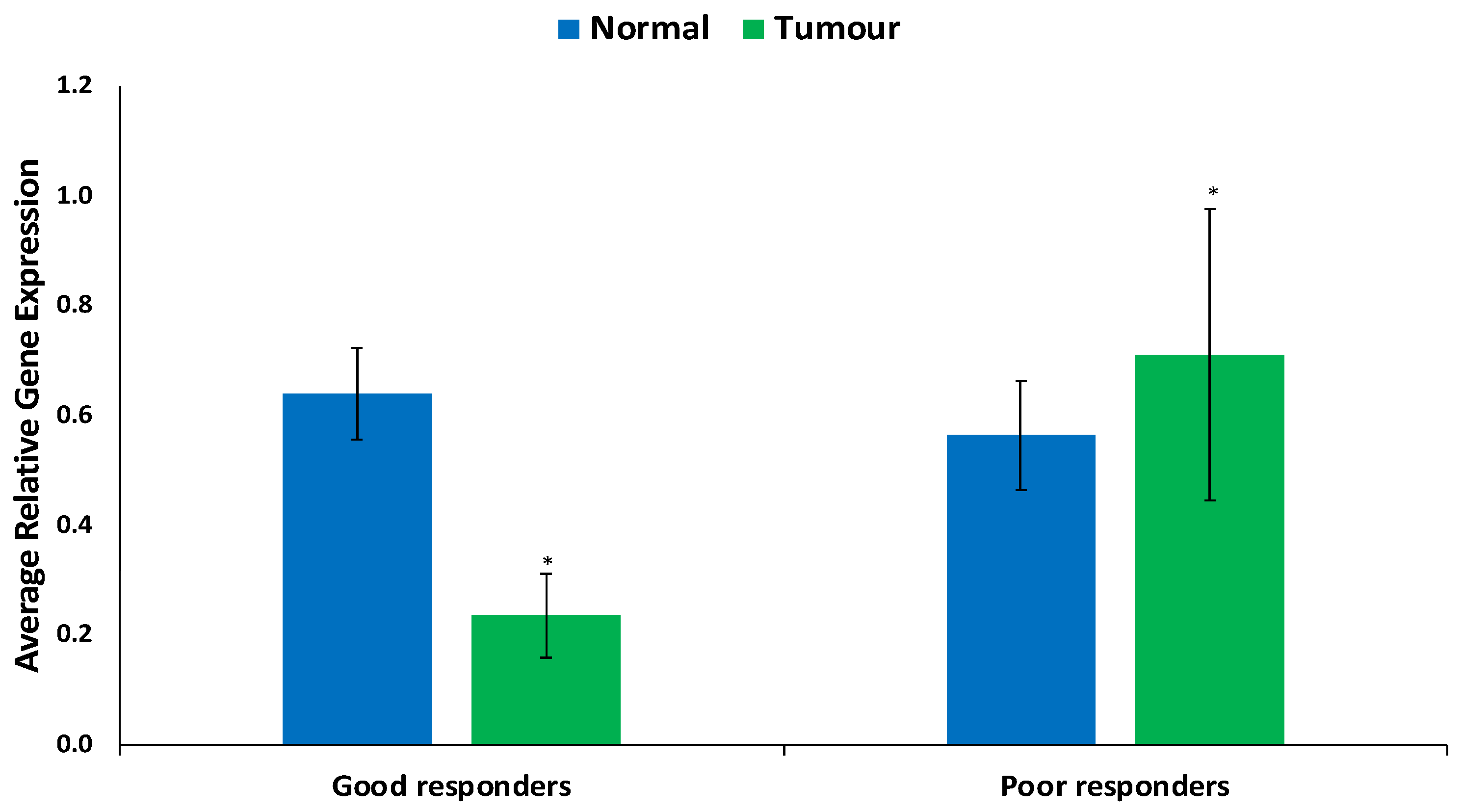
3.1. Relative Gene Expression of ABCB1
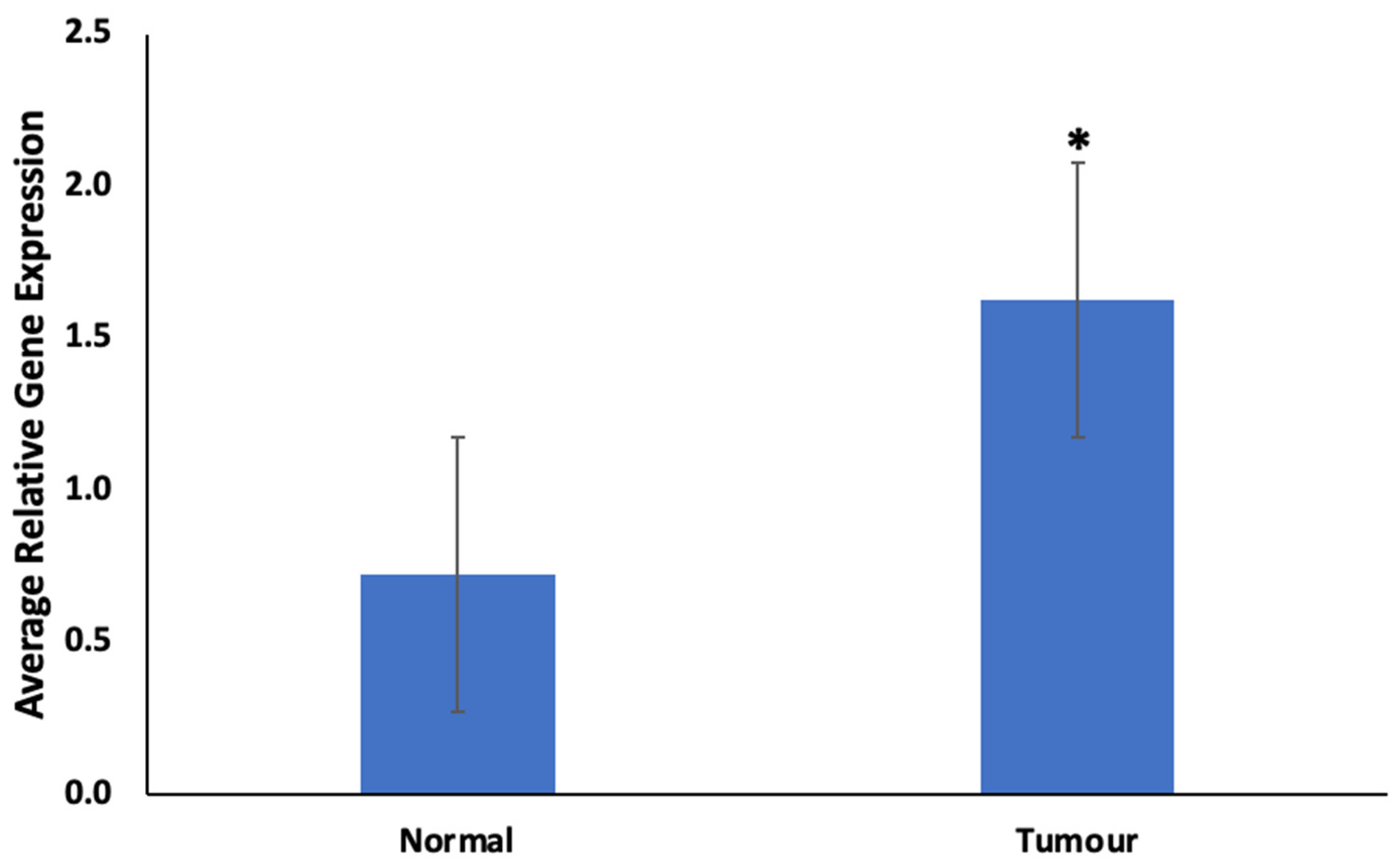
3.2. Relative Gene Expression of CYP1B1
3.3. Signaling Pathway Enrichment of CYP1B1 and ABCB1 Expression
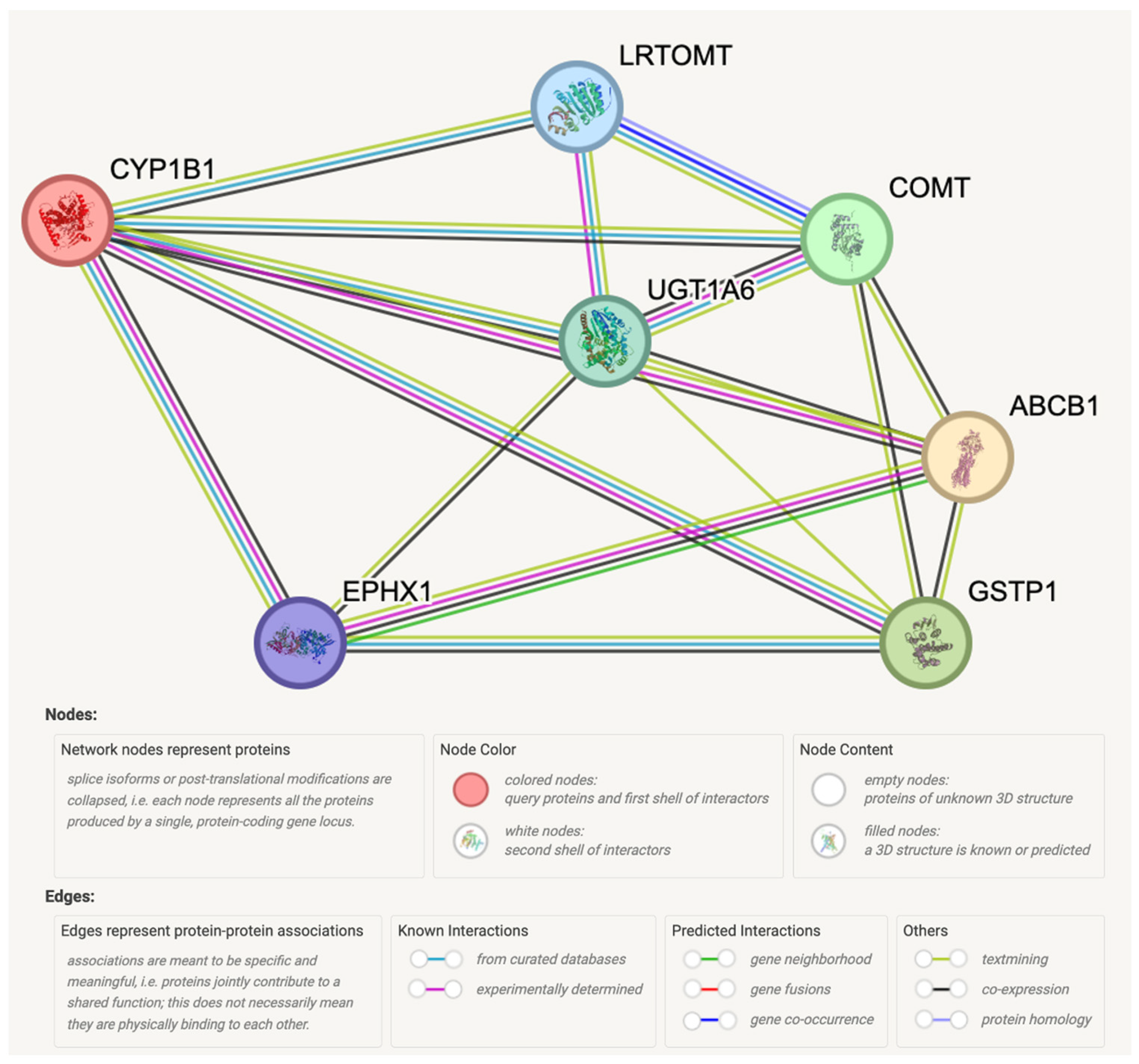
3.4. Protein–Protein Interaction Network Analysis of CYP1B1 and ABCB1
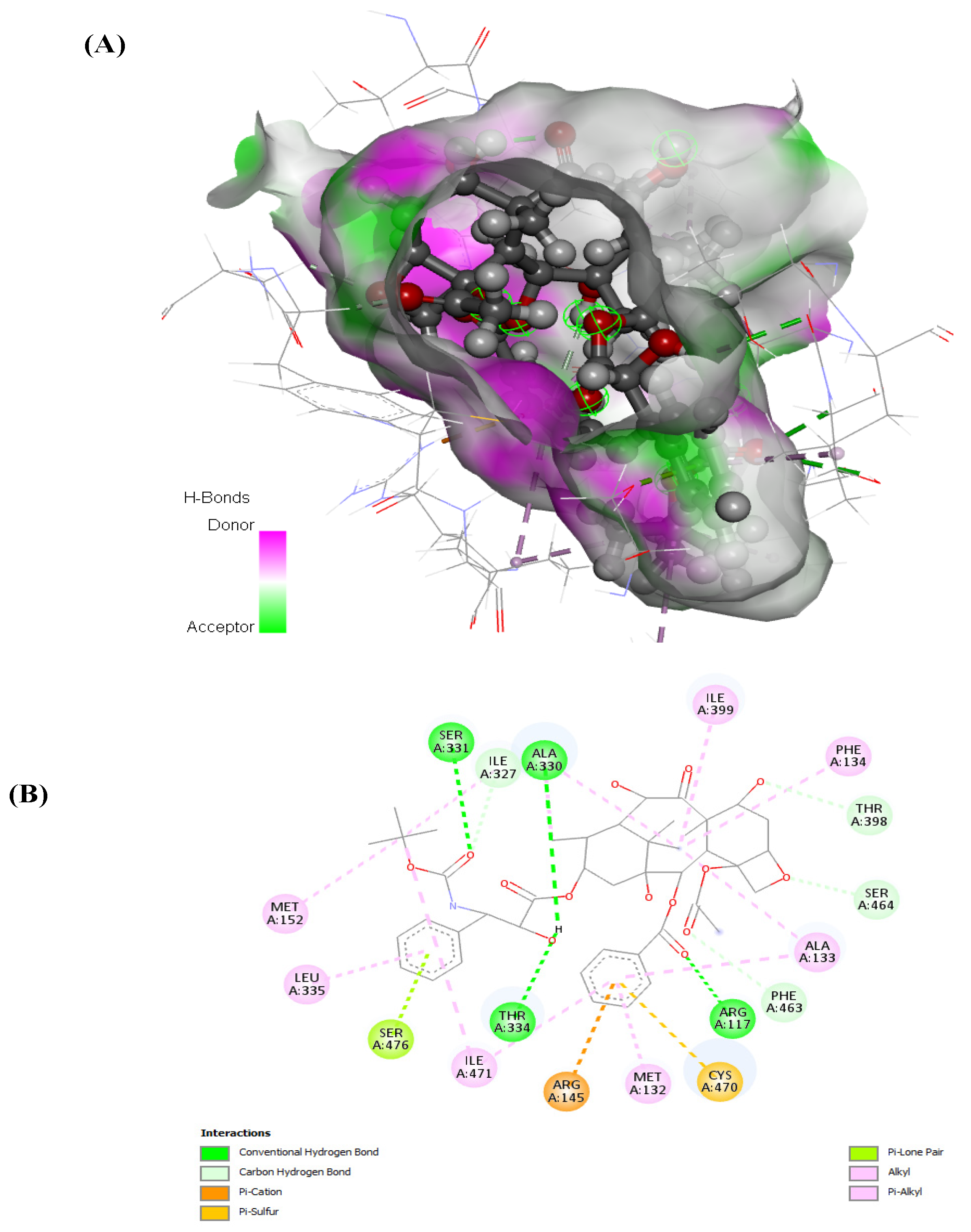
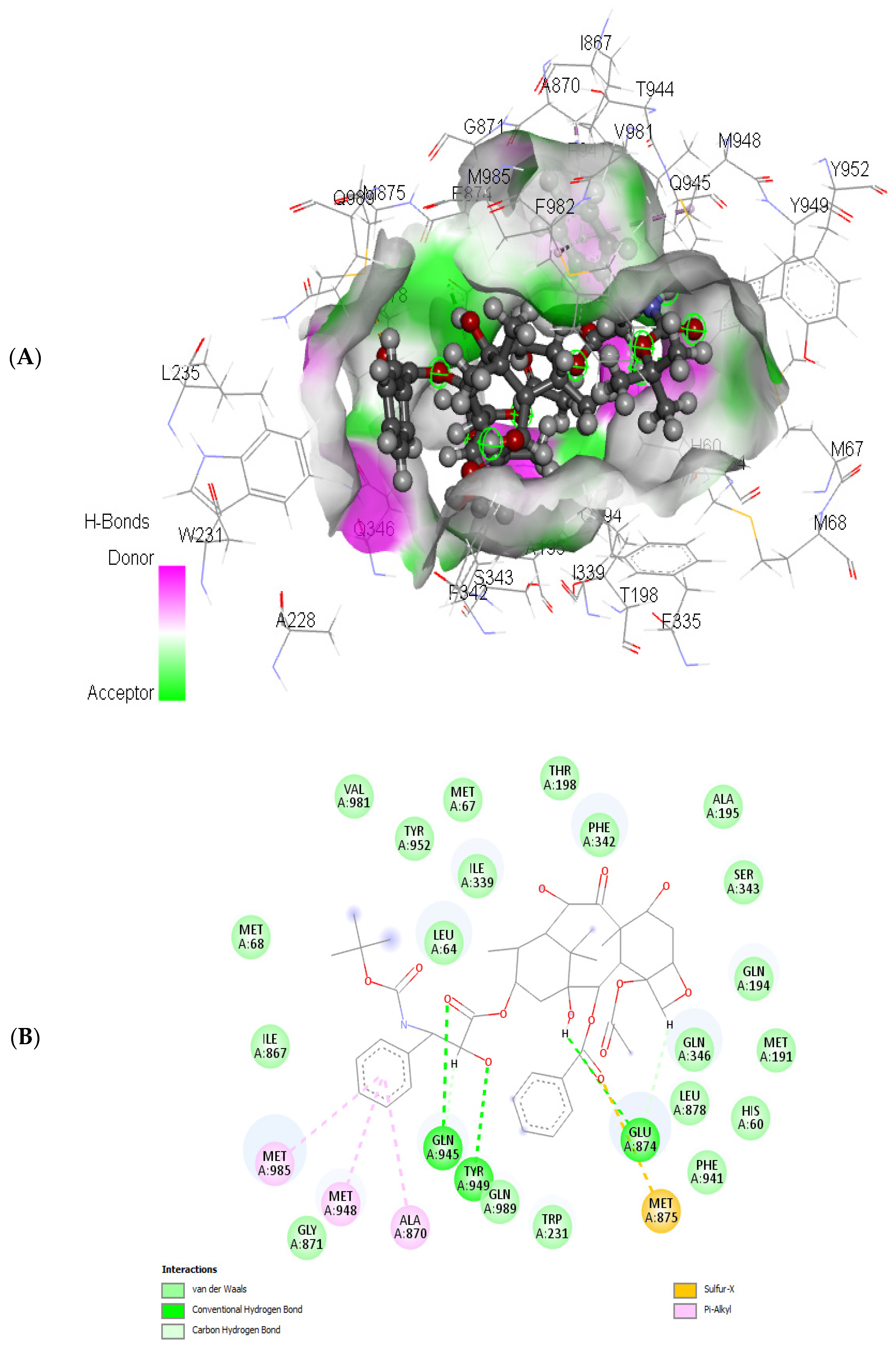
3.5. Molecular Docking Analysis of ABCB1 and CYP1B1
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Berenguer, C.V.; Pereira, F.; Câmara, J.S.; Pereira, J.A.M. Underlying Features of Prostate Cancer—Statistics, Risk Factors, and Emerging Methods for Its Diagnosis. Curr. Oncol. 2023, 30, 2300–2321. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.; Zhang, A.-H.; Qiu, S.; Zhang, T.-L.; Li, X.-N.; Yan, G.-L.; Sun, H.; Liu, L.; Wang, X.-J. Identification of the perturbed metabolic pathways associating with prostate cancer cells and anticancer affects of obacunone. J. Proteom. 2019, 206, 103447. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.H.; Yu, A.-M. ABC Transporters in Multidrug Resistance and Pharmacokinetics, and Strategies for Drug Development. Curr. Pharm. Des. 2014, 20, 793–807. [Google Scholar] [CrossRef] [PubMed]
- Criscuolo, D.; Morra, F.; Giannella, R.; Cerrato, A.; Celetti, A. Identification of Novel Biomarkers of Homologous Recombination Defect in DNA Repair to Predict Sensitivity of Prostate Cancer Cells to PARP-Inhibitors. Int. J. Mol. Sci. 2019, 20, 3100. [Google Scholar] [CrossRef] [PubMed]
- Sokolova, A.O.; Cheng, H.H. Genetic Testing in Prostate Cancer. Curr. Oncol. Rep. 2020, 22, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Abidi, A. Cabazitaxel: A novel taxane for metastatic castration-resistant prostate cancer-current implications and future prospects. J. Pharmacol. Pharmacother. 2013, 4, 230–237. [Google Scholar] [CrossRef]
- Giacinti, S.; Poti, G.; Roberto, M.; Macrini, S.; Bassanelli, M.; Di Pietro, F.; Aschelter, A.M.; Ceribelli, A.; Ruggeri, E.M.; Marchetti, P. Molecular Basis of Drug Resistance and Insights for New Treatment Approaches in mCRPC. Anticancer Res. 2018, 38, 6029–6039. [Google Scholar] [CrossRef]
- Obligacion, R.; Murray, M.; Ramzan, I. Drug-Metabolizing Enzymes and Transporters: Expression in the Human Prostate and Roles in Prostate Drug Disposition. J. Androl. 2006, 27, 138–150. [Google Scholar] [CrossRef]
- Demidenko, R.; Razanauskas, D.; Daniunaite, K.; Lazutka, J.R.; Jankevicius, F.; Jarmalaite, S. Frequent down-regulation of ABC transporter genes in prostate cancer. BMC Cancer 2015, 15, 683. [Google Scholar] [CrossRef]
- Cookson, M.S.; Roth, B.J.; Dahm, P.; Engstrom, C.; Freedland, S.J.; Hussain, M.; Lin, D.W.; Lowrance, W.T.; Murad, M.H.; Oh, W.K.; et al. Castration-Resistant Prostate Cancer: AUA Guideline. J. Urol. 2013, 190, 429–438. [Google Scholar] [CrossRef] [PubMed]
- Oyama, T.; Kagawa, N.; Kunugita, N.; Kitagawa, K.; Ogawa, M.; Yamaguchi, T.; Suzuki, R.; Kinaga, T.; Yashima, Y.; Ozaki, S.; et al. Expression of cytochrome P450 in tumor tissues and its association with cancer development. Front. Biosci. 2004, 9, 1967–1976. [Google Scholar] [CrossRef]
- Kinoshita, Y.; Singh, A.; Rovito, P.M.; Wang, C.Y.; Haas, G.P. Double Primary Cancers of the Prostate and Bladder: A Literature Review. Clin. Prostate Cancer 2004, 3, 83–86. [Google Scholar] [CrossRef]
- Tokizane, T.; Shiina, H.; Igawa, M.; Enokida, H.; Urakami, S.; Kawakami, T.; Ogishima, T.; Okino, S.T.; Li, L.-C.; Tanaka, Y.; et al. Cytochrome P450 1B1 Is Overexpressed and Regulated by Hypomethylation in Prostate Cancer. Clin. Cancer Res. 2005, 11, 5793–5801. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.; Powers, J.; Schaffer, K.; Sartor, O. Practical Methods for Integrating Genetic Testing into Clinical Practice for Advanced Prostate Cancer. Am. Soc. Clin. Oncol. Educ. Book 2018, 38, 372–381. [Google Scholar] [CrossRef]
- Zhen, J.T.; Syed, J.; Nguyen, K.A.; Leapman, M.S.; Agarwal, N.; Brierley, K.; Llor, X.; Hofstatter, E.; Shuch, B. Genetic testing for hereditary prostate cancer: Current status and limitations. Cancer 2018, 124, 3105–3117. [Google Scholar] [CrossRef]
- Giri, V.N.; Morgan, T.M.; Morris, D.S.; Berchuck, J.E.; Hyatt, C.; Morris, F.D.S.; Hyatt, C.C.; Taplin, M.-E. Genetic testing in prostate cancer management: Considerations informing primary care. CA Cancer J. Clin. 2022, 72, 360–371. [Google Scholar] [CrossRef]
- Walsh, P.C. Docetaxel and Estramustine Compared With Mitoxantrone and Prednisone for Advanced Refractory Prostate Cancer. J. Urol. 2005, 173, 457. [Google Scholar] [CrossRef]
- Sy, J.; Ang, L.-C. Microtomy: Cutting formalin-fixed, paraffin-embedded sections. In Biobanking. Methods in Molecular Biology; Humana Press: New York, NY, USA, 2019; pp. 269–278. [Google Scholar] [CrossRef]
- Kuleshov, M.V.; Jones, M.R.; Rouillard, A.D.; Fernandez, N.F.; Duan, Q.; Wang, Z.; Koplev, S.; Jenkins, S.L.; Jagodnik, K.M.; Lachmann, A.; et al. Enrichr: A comprehensive gene set enrichment analysis web server 2016 update. Nucleic Acids Res. 2016, 44, W90–W97. [Google Scholar] [CrossRef]
- Raju, B.; Verma, H.; Narendra, G.; Sapra, B.; Silakari, O. Multiple machine learning, molecular docking, and ADMET screening approach for identification of selective inhibitors of CYP1B1. J. Biomol. Struct. Dyn. 2021, 40, 7975–7990. [Google Scholar] [CrossRef] [PubMed]
- Iacobas, S.; Iacobas, D.A. Personalized 3-Gene Panel for Prostate Cancer Target Therapy. Curr. Issues Mol. Biol. 2022, 44, 360–382. [Google Scholar] [CrossRef] [PubMed]
- Rees, D.C.; Johnson, E.; Lewinson, O. ABC transporters: The power to change. Nat. Rev. Mol. Cell Biol. 2009, 10, 218–227. [Google Scholar] [CrossRef] [PubMed]
- Angel, J.M.; DiGiovanni, J. Genetic determinants of cancer susceptibility. In Comprehensive Toxicology, 3rd ed.; McQueen, C.A., Ed.; Elsevier: Amsterdam, The Netherlands, 2018; pp. 330–360. [Google Scholar] [CrossRef]
- Lin, Q.; Cao, J.; Du, X.; Yang, K.; Yang, X.; Liang, Z.; Shi, J.; Zhang, J. CYP1B1-catalyzed 4-OHE2 promotes the castration resistance of prostate cancer stem cells by estrogen receptor α-mediated IL6 activation. Cell Commun. Signal. 2022, 20, 31. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Zhao, Z.; Zhang, Z.; Zhang, Y.; Guan, W. Tryptophan metabolism induced by TDO2 promotes prostatic cancer chemotherapy resistance in a AhR/c-Myc dependent manner. BMC Cancer 2021, 21, 1112. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Ding, B.; Ali, M.R.K.; Zhao, L.; Zang, X.; Lv, Z. Dual Effect of Tryptamine on Prostate Cancer Cell Growth Regulation: A Pilot Study. Int. J. Mol. Sci. 2022, 23, 11087. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.; Mao, Y.; Tahreem, S.; Wei, D.-Q.; Wang, Y. Structural and molecular insights into the mechanism of resistance to enzalutamide by the clinical mutants in androgen receptor (AR) in castration-resistant prostate cancer (CRPC) patients. Int. J. Biol. Macromol. 2022, 218, 856–865. [Google Scholar] [CrossRef] [PubMed]
- Townsend, D.M.; Tew, K.D. The role of glutathione-S-transferase in anti-cancer drug resistance. Oncogene 2003, 22, 7369–7375. [Google Scholar] [CrossRef]
- Allain, E.P.; Rouleau, M.; Lévesque, E.; Guillemette, C. Emerging roles for UDP-glucuronosyltransferases in drug resistance and cancer progression. Br. J. Cancer 2020, 122, 1277–1287. [Google Scholar] [CrossRef]
- Ju, G.; Liu, B.; Ji, M.; Jin, R.; Xu, X.; Xiao, Y.; Li, J.; Xu, D.; Huang, Y.; Hou, J. Folic Acid–Modified miR-491-5p–Loaded ZIF-8 Nanoparticles Inhibit Castration-Resistant Prostate Cancer by Regulating the Expression of EPHX1. Front. Bioeng. Biotechnol. 2021, 9, 706536. [Google Scholar] [CrossRef]
- Jacob, F.; Guertler, R.; Naim, S.; Nixdorf, S.; Fedier, A.; Hacker, N.F.; Heinzelmann-Schwarz, V. Careful Selection of Reference Genes Is Required for Reliable Performance of RT-qPCR in Human Normal and Cancer Cell Lines. PLoS ONE 2013, 8, e59180. [Google Scholar] [CrossRef]
- Puente, J.; Grande, E.; Medina, A.; Maroto, P.; Lainez, N.; Arranz, J.A. Docetaxel in prostate cancer: A familiar face as the new standard in a hormone-sensitive setting. Ther. Adv. Med. Oncol. 2017, 9, 307–318. [Google Scholar] [CrossRef] [PubMed]
- Corcoran, C.; Rani, S.; O’Brien, K.; O’Neill, A.; Prencipe, M.; Sheikh, R.; Webb, G.; McDermott, R.; Watson, W.; Crown, J.; et al. Docetaxel-resistance in prostate cancer: Evaluating associated phenotypic changes and potential for resistance transfer via exosomes. PLoS ONE 2012, 7, e50999. [Google Scholar] [CrossRef] [PubMed]
- Hashemi, M.; Zandieh, M.A.; Talebi, Y.; Rahmanian, P.; Shafiee, S.S.; Nejad, M.M.; Babaei, R.; Sadi, F.H.; Rajabi, R.; Abkenar, Z.O.; et al. Paclitaxel and docetaxel resistance in prostate cancer: Molecular mechanisms and possible therapeutic strategies. Biomed. Pharmacother. 2023, 160, 114392. [Google Scholar] [CrossRef]
- Sekino, Y.; Teishima, J. Molecular mechanisms of docetaxel resistance in prostate cancer. Cancer Drug Resist. 2020, 3, 676–685. [Google Scholar] [CrossRef] [PubMed]
- McFadyen, M.C.; McLeod, H.L.; Jackson, F.C.; Melvin, W.T.; Doehmer, J.; Murray, G.I. Cytochrome P450 CYP1B1 protein expression: A novel mechanism of anticancer drug resistance. Biochem. Pharmacol. 2001, 62, 207–212. [Google Scholar] [CrossRef]
- Pastina, I.; Giovannetti, E.; Chioni, A.; Sissung, T.M.; Crea, F.; Orlandini, C.; Price, D.K.; Cianci, C.; Figg, W.D.; Ricci, S.; et al. Cytochrome 450 1B1 (CYP1B1) polymorphisms associated with response to docetaxel in Castration-Resistant Prostate Cancer (CRPC) patients. BMC Cancer 2010, 10, 511. [Google Scholar] [CrossRef]
- Linke, D.; Donix, L.; Peitzsch, C.; Erb, H.H.H.; Dubrovska, A.; Pfeifer, M.; Thomas, C.; Fuessel, S.; Erdmann, K. Comprehensive Evaluation of Multiple Approaches Targeting ABCB1 to Resensitize Docetaxel-Resistant Prostate Cancer Cell Lines. Int. J. Mol. Sci. 2022, 24, 666. [Google Scholar] [CrossRef]
- Seo, H.K.; Lee, S.; Kwon, W.; Jeong, K. Docetaxel-resistant prostate cancer cells become sensitive to gemcitabine due to the upregulation of ABCB1. Prostate 2020, 80, 453–462. [Google Scholar] [CrossRef]
- Martinez, V.G.; O’Connor, R.; Liang, Y.; Clynes, M. CYP1B1 expression is induced by docetaxel: Effect on cell viability and drug resistance. Br. J. Cancer 2008, 98, 564–570. [Google Scholar] [CrossRef]


| Patient Category | Symptomatic Improvement | Gleason Score | Progressive Disease | Serum PSA Level |
|---|---|---|---|---|
| Good Responders | ||||
| 1 | Yes | 7 (4 + 3) | No | >5000 |
| 2 | Yes | 7 (4 + 3) | No | 7000 |
| 3 | Yes | 8 (4 + 4) | No | 300 |
| 4 | Yes | 7 (3 + 4) | No | >2000 |
| Poor Responders | ||||
| 5 | No | 8 (4 + 4) | Yes | >2000 |
| 6 | No | 9 (4 + 5) | Yes | 209 |
| 7 | No | 7 (4 + 3) | Yes | 75 |
| 8 | No | 7 (4 + 3) | Yes | 103 |
| 9 | No | 7 (4 + 3) | Yes | 4513 |
| Sample Name | Biological Group | CqABCB1 | CqCYP1B1 | CqGAPDH | CqHPRT | CqHSPCB |
|---|---|---|---|---|---|---|
| 5N | Normal | 28.3 | 24.12 | 21.4 | 33.8 | 22.4 |
| 1N-1 | Normal | 30.1 | 23.86 | 17.6 | UND | 19.8 |
| 1N-2 | Normal | 32.8 | 28.92 | 27.2 | 28.2 | 24.0 |
| 6N | Normal | 27.8 | 22.93 | 17.8 | 27.7 | 19.7 |
| 7N | Normal | 26.1 | 20.38 | 15.6 | UND | 17.3 |
| 2N | Normal | 30.1 | 22.01 | 18.1 | 28.2 | 18.3 |
| 3N | Normal | 27.1 | 21.56 | 16.7 | 27.3 | 18.8 |
| 8N | Normal | 30.2 | 25.04 | 24.2 | 27.8 | 22.8 |
| 9N | Normal | UND | 30.42 | 29.1 | 25.4 | 26.5 |
| 4N | Normal | 29.4 | 24.80 | 20.7 | 24.8 | 21.0 |
| 5T | Tumor | UND | 28.18 | 25.9 | 26.8 | 27.2 |
| 1T-1 | Tumor | 31.6 | 23.56 | 17.4 | 26.3 | 19.6 |
| 1T-2 | Tumor | 29.8 | 23.63 | 18.7 | 26.1 | 20.0 |
| 6T | Tumor | 27.0 | 22.08 | 18.5 | UND | 20.0 |
| 7T | Tumor | 25.9 | 20.93 | 15.9 | 29.7 | 17.4 |
| 2T | Tumor | 28.3 | 21.37 | 19.0 | UND | 18.9 |
| 3T | Tumor | 27.9 | 21.73 | 16.9 | 32.6 | 18.8 |
| 8T | Tumor | UND | 24.06 | 20.3 | 29.9 | 20.9 |
| 9T | Tumor | 29.7 | 24.76 | 22.2 | 28.4 | 23.2 |
| 4T | Tumor | 28.9 | 20.59 | 19.6 | 31.6 | 20.1 |
| CTRL | Control Sample | 20.9 | 20.83 | 14.1 | 22.1 | 14.8 |
| Protein | Score |
|---|---|
| GSTP1 | 0.973 |
| COMT | 0.971 |
| UGT1A6 | 0.966 |
| LRTOMT | 0.966 |
| EPHX1 | 0.966 |
| Ligand | Proteins | Hydrogen Bonds between Atoms of Ligands and Amino Acids of Receptor | Score (Binding Energy) (Kcal/mol) | |||||
|---|---|---|---|---|---|---|---|---|
| Ligand Atoms | Receptor | Type | Distance (Å) | Energy (Kcal/mol) | ||||
| Atoms | Residues | |||||||
| Docetaxel | ABCB1 | O4 | OE1 | GLU874 | H-donor | 2.92 | −1.2 | −15.25 |
| O10 | SD | MET875 | H-donor | 3.18 | −0.3 | |||
| C41 | OE1 | GLN945 | H-donor | 3.37 | −0.9 | |||
| O12 | OH | TYR949 | H-acceptor | 2.69 | −1.6 | |||
| CY1B1 | O5 | N | ILE399 | H-acceptor | 2.76 | −1.6 | −20.37 | |
| O9 | CA | PHE463 | H-acceptor | 2.95 | −0.7 | |||
| 6-ring | CA | SER331 | Pi-H | 3.92 | −0.8 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gumenku, L.; Sekhoacha, M.; Abrahams, B.; Mashele, S.; Shoko, A.; Erukainure, O.L. Genetic Signatures for Distinguishing Chemo-Sensitive from Chemo-Resistant Responders in Prostate Cancer Patients. Curr. Issues Mol. Biol. 2024, 46, 2263-2277. https://doi.org/10.3390/cimb46030145
Gumenku L, Sekhoacha M, Abrahams B, Mashele S, Shoko A, Erukainure OL. Genetic Signatures for Distinguishing Chemo-Sensitive from Chemo-Resistant Responders in Prostate Cancer Patients. Current Issues in Molecular Biology. 2024; 46(3):2263-2277. https://doi.org/10.3390/cimb46030145
Chicago/Turabian StyleGumenku, Lemohang, Mamello Sekhoacha, Beynon Abrahams, Samson Mashele, Aubrey Shoko, and Ochuko L. Erukainure. 2024. "Genetic Signatures for Distinguishing Chemo-Sensitive from Chemo-Resistant Responders in Prostate Cancer Patients" Current Issues in Molecular Biology 46, no. 3: 2263-2277. https://doi.org/10.3390/cimb46030145
APA StyleGumenku, L., Sekhoacha, M., Abrahams, B., Mashele, S., Shoko, A., & Erukainure, O. L. (2024). Genetic Signatures for Distinguishing Chemo-Sensitive from Chemo-Resistant Responders in Prostate Cancer Patients. Current Issues in Molecular Biology, 46(3), 2263-2277. https://doi.org/10.3390/cimb46030145






