Lumbricus Extract Prevents LPS-Induced Inflammatory Activation of BV2 Microglia and Glutamate-Induced Hippocampal HT22 Cell Death by Suppressing MAPK/NF-κB/NLRP3 Signaling and Oxidative Stress
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials and Reagents
2.2. Preparation of Lumbricus Water Extract (LWE) and Lumbricus Ethanol Extract (LEE)
2.3. Cell Culture and Drug Treatment
2.4. Cell Viability
2.5. Analysis of NO Secretion
2.6. ELISA for Cytokine Determination
2.7. Total RNA Extraction, DNA Synthesis, and RT-qPCR
2.8. Preparation of Whole-Cell, Cytosolic, and Nuclear Lysates
2.9. Western Blot Analysis
2.10. LDH Assay for Cytotoxicity
2.11. Intracellular ROS Determination
2.12. Measurement of MDA
2.13. Apoptotic Cell Death Assessment by Flow Cytometry
2.14. Preparation of Extracts and Standards for HPLC
2.15. Chromatographic Conditions
2.16. Validation of the Method
2.17. Statistical Analysis
3. Results
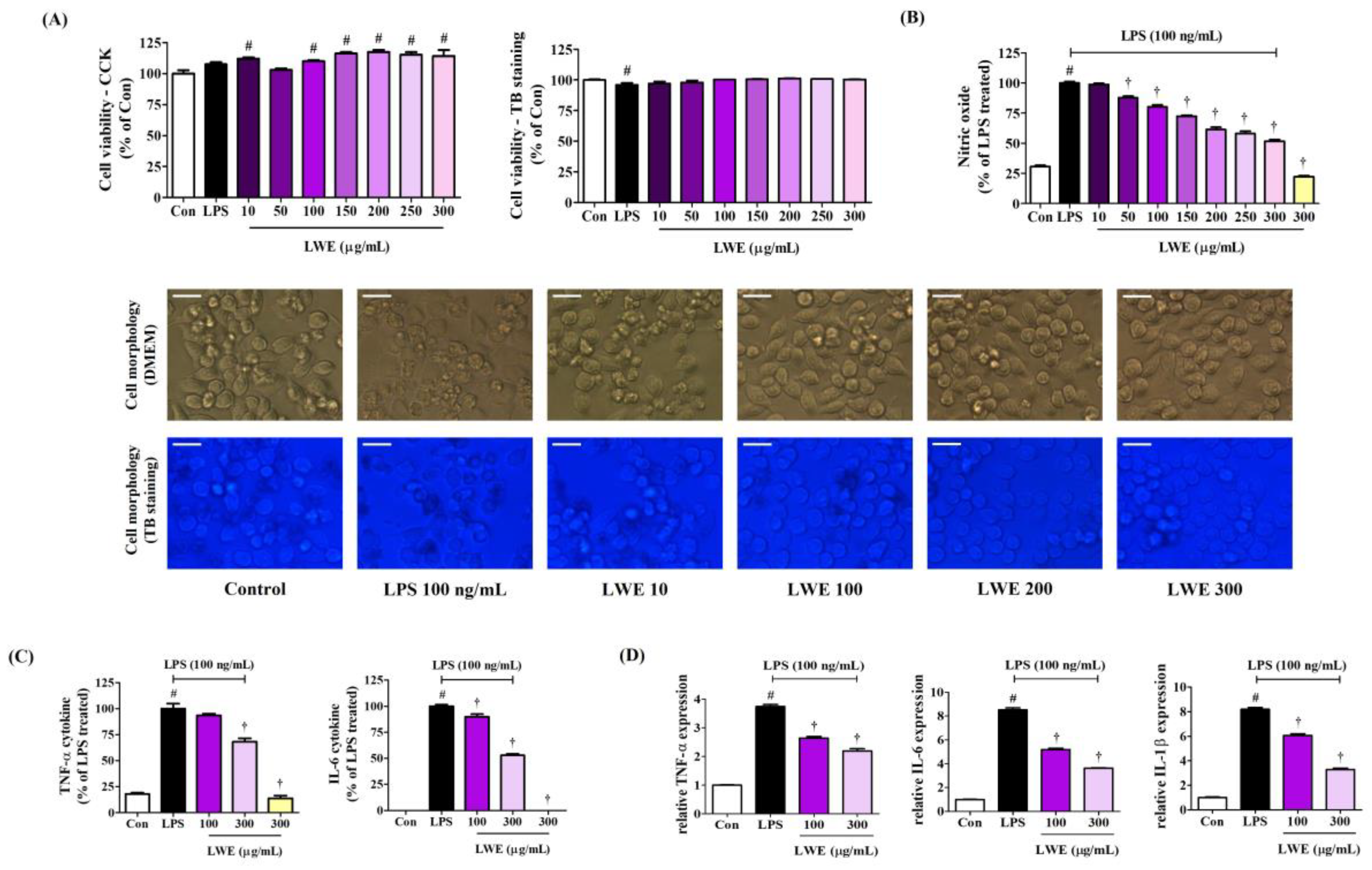
3.1. Effects of LWE on Microglial Cell Viability
3.2. LWE Dose-Dependently Inhibited the Secretion of NO and the Production of Inflammatory Cytokines by LPS-Stimulated BV2 Microglia
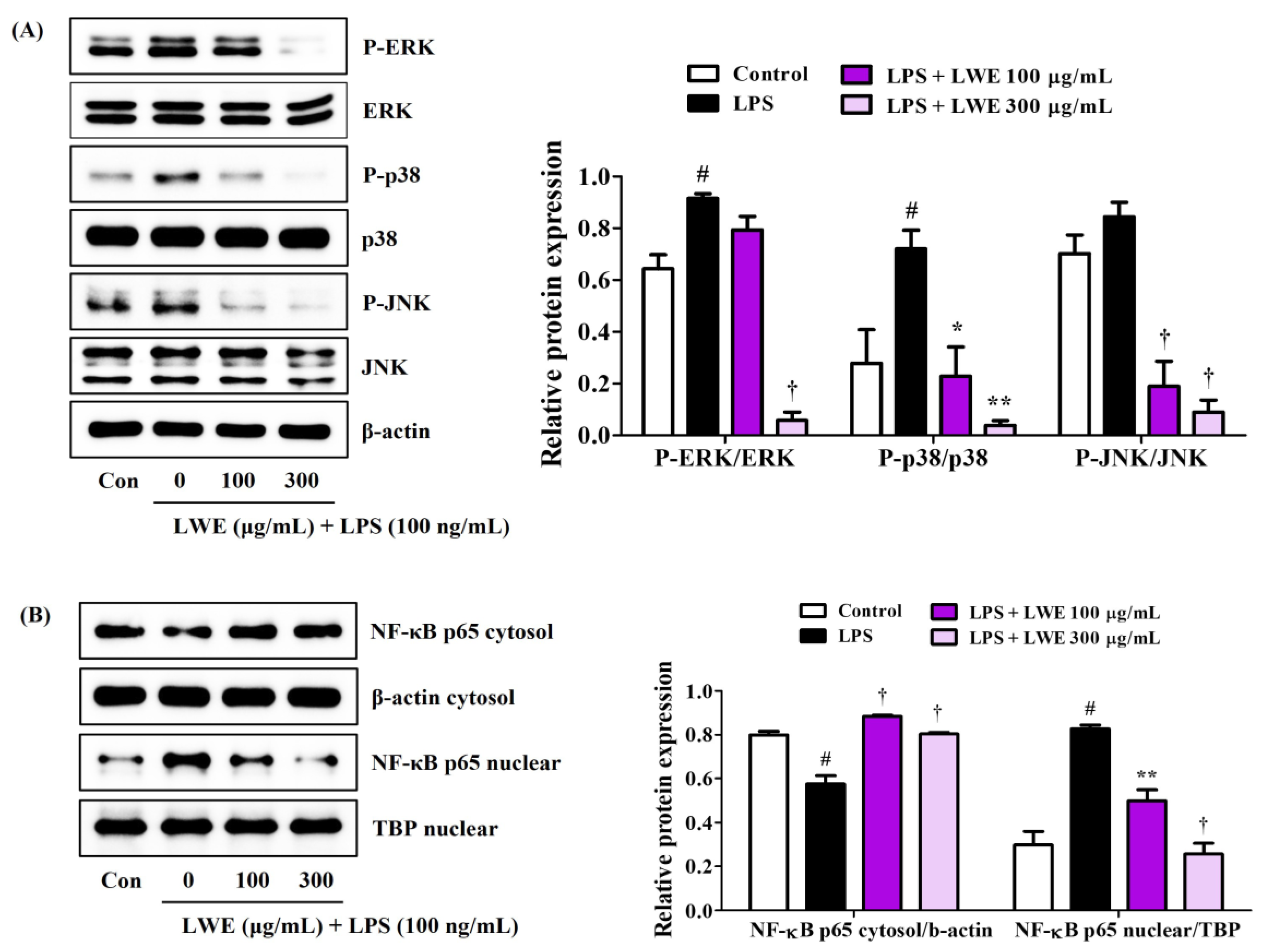
3.3. LWE Reduced MAPK Phosphorylation and NF-κB Nuclear Translocation in LPS-Stimulated BV2 Cells
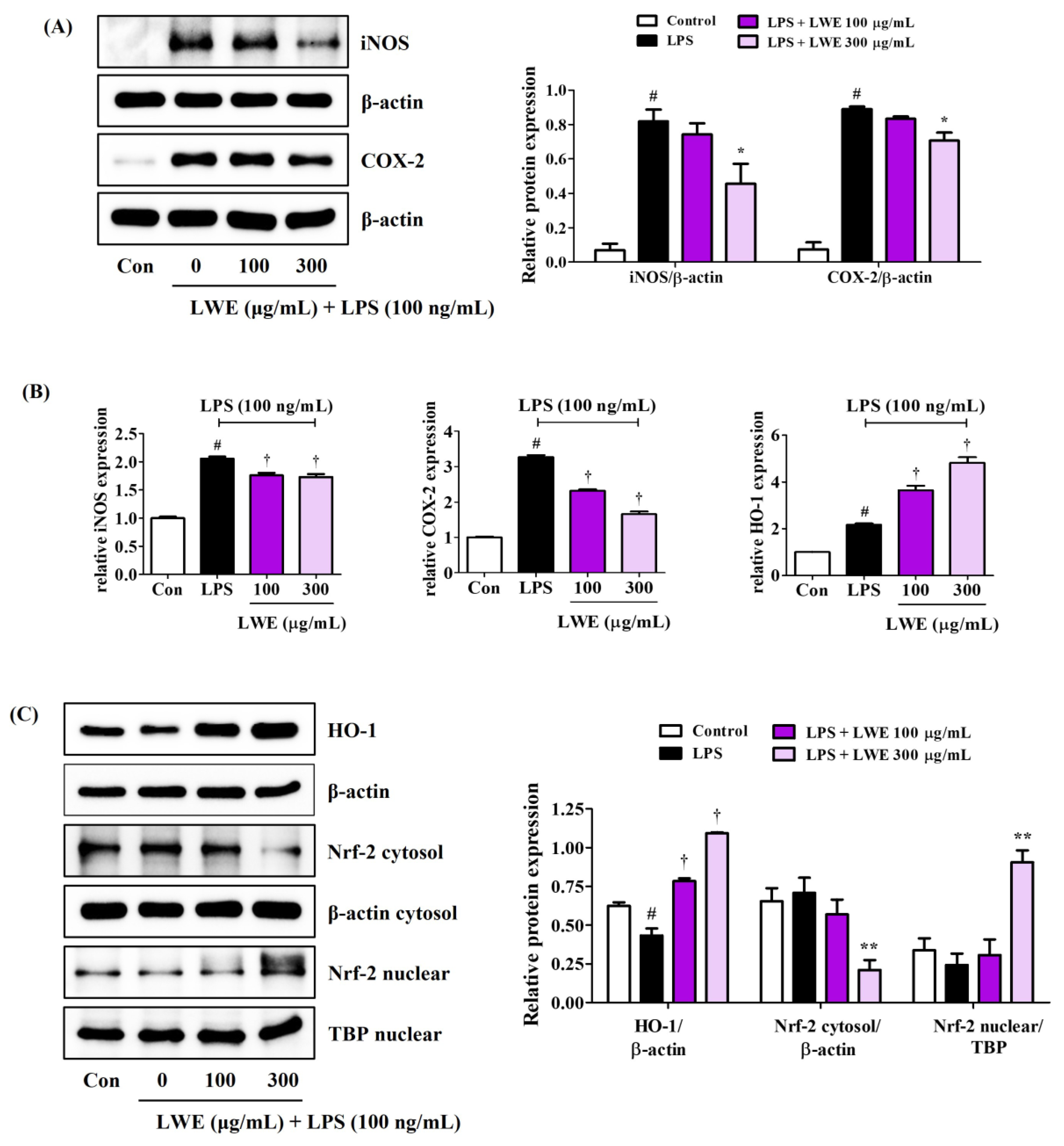
3.4. LWE Pretreatment Suppressed LPS-Induced Expression of iNOS and COX-2
3.5. LWE Upregulated HO-1 and Nuclear Translocation of Nrf-2 in LPS-Stimulated BV2 Microglia
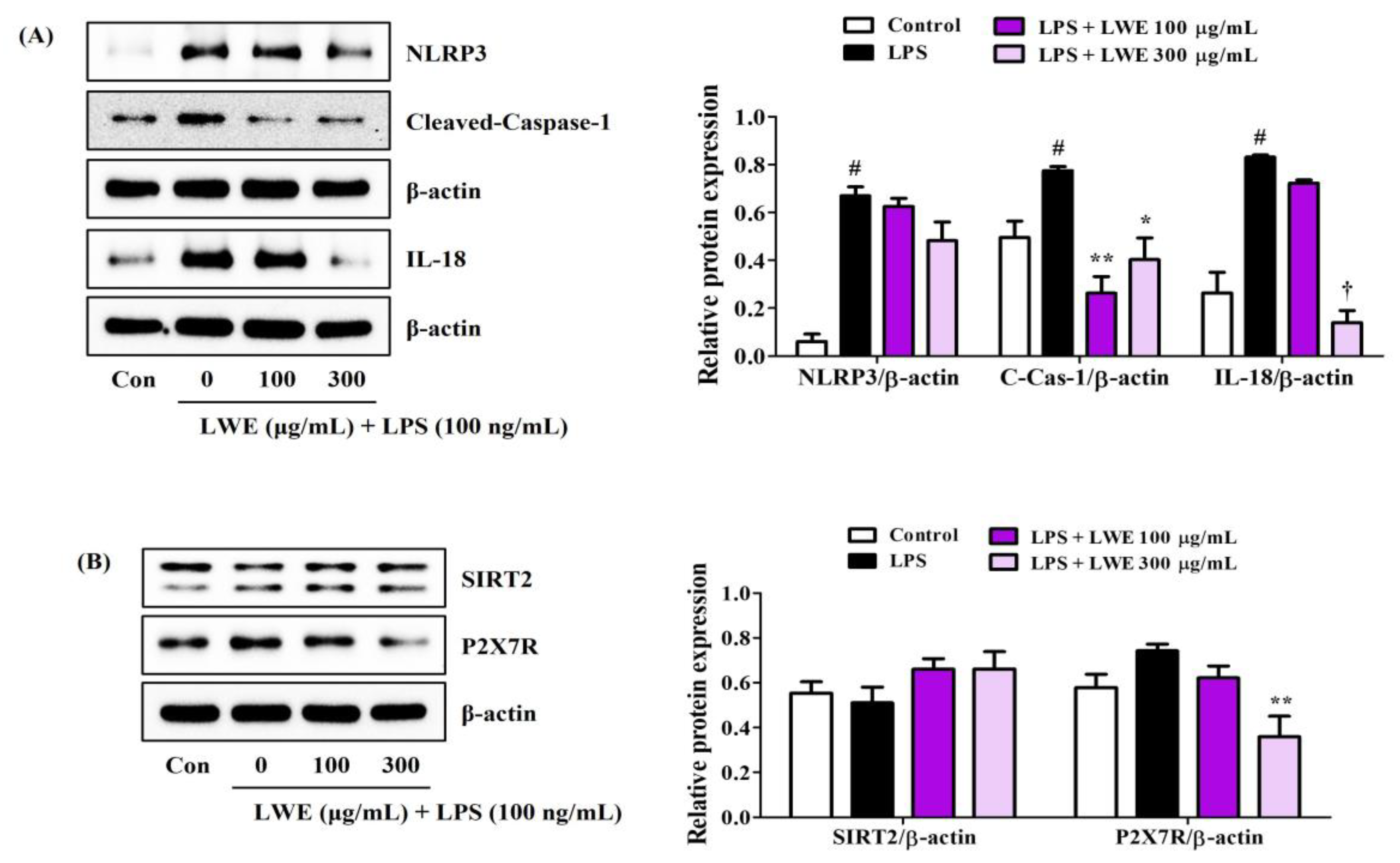
3.6. LWE Inhibited LPS-Induced Expression of NLRP3 Inflammasome-Related Proteins in BV2 Cells
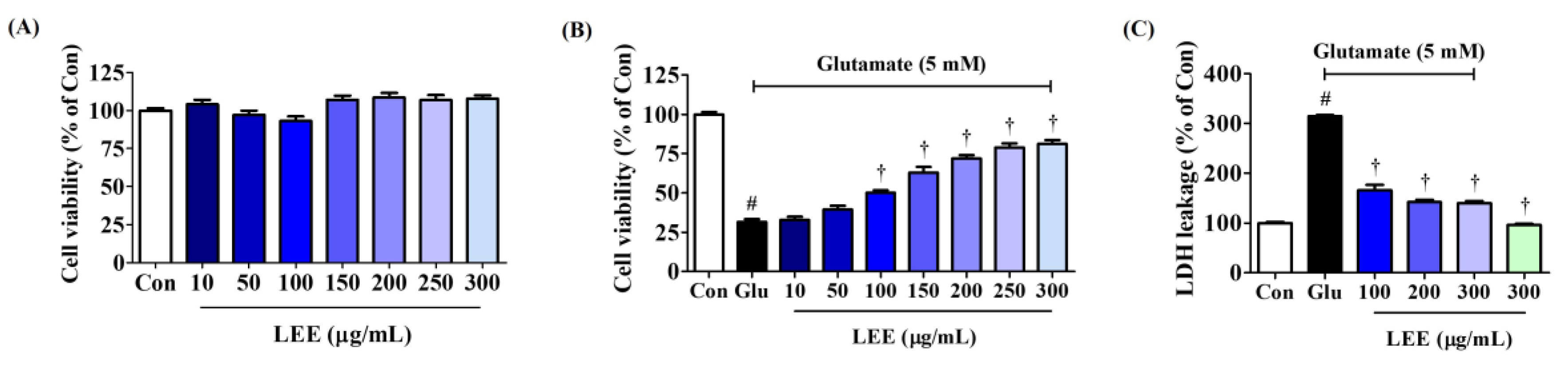
3.7. LEE Protected Hippocampal HT22 Cells against Glutamate-Induced Death
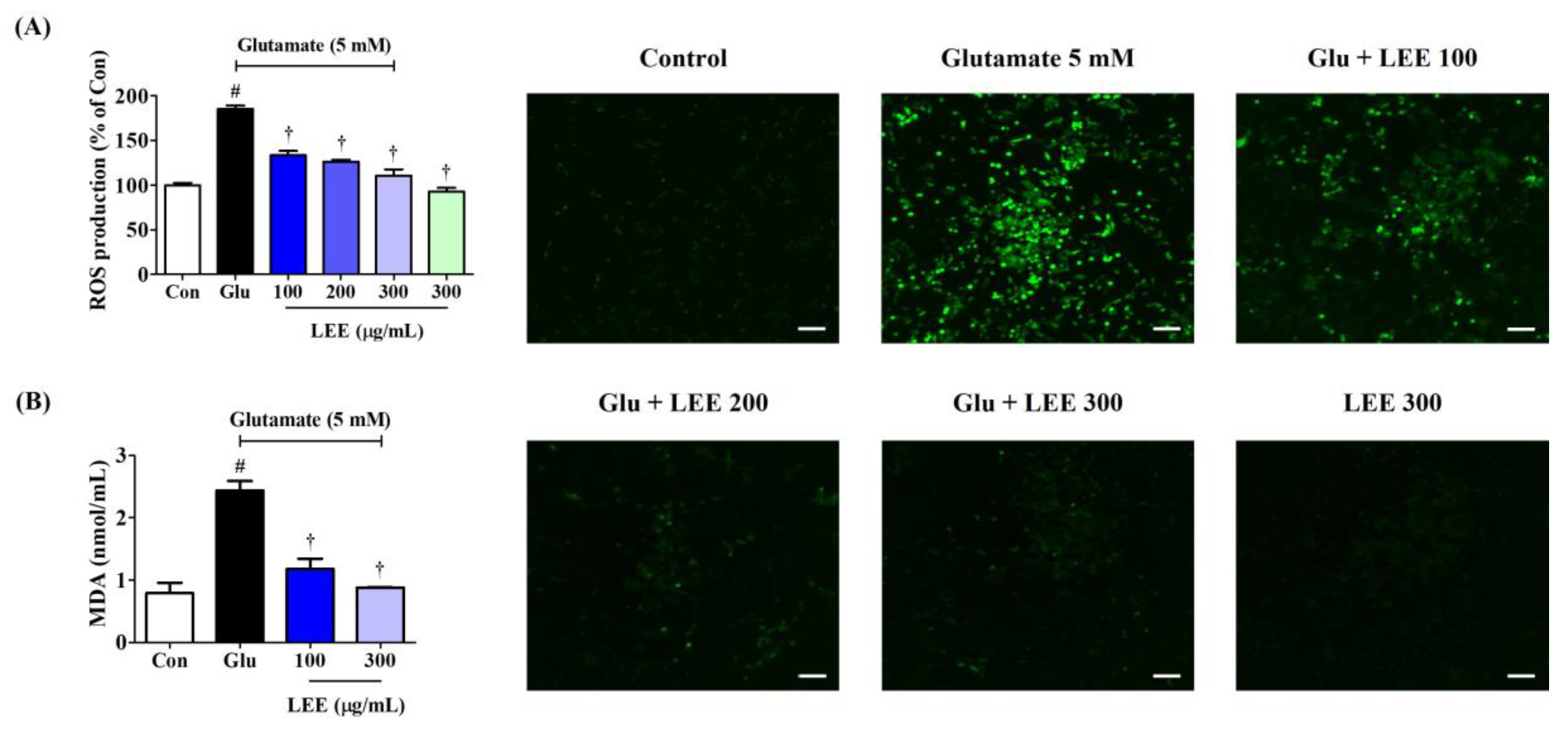
3.8. LEE Reduced Glutamate-Induced Intracellular ROS Generation and MDA Expression in HT22 Cells
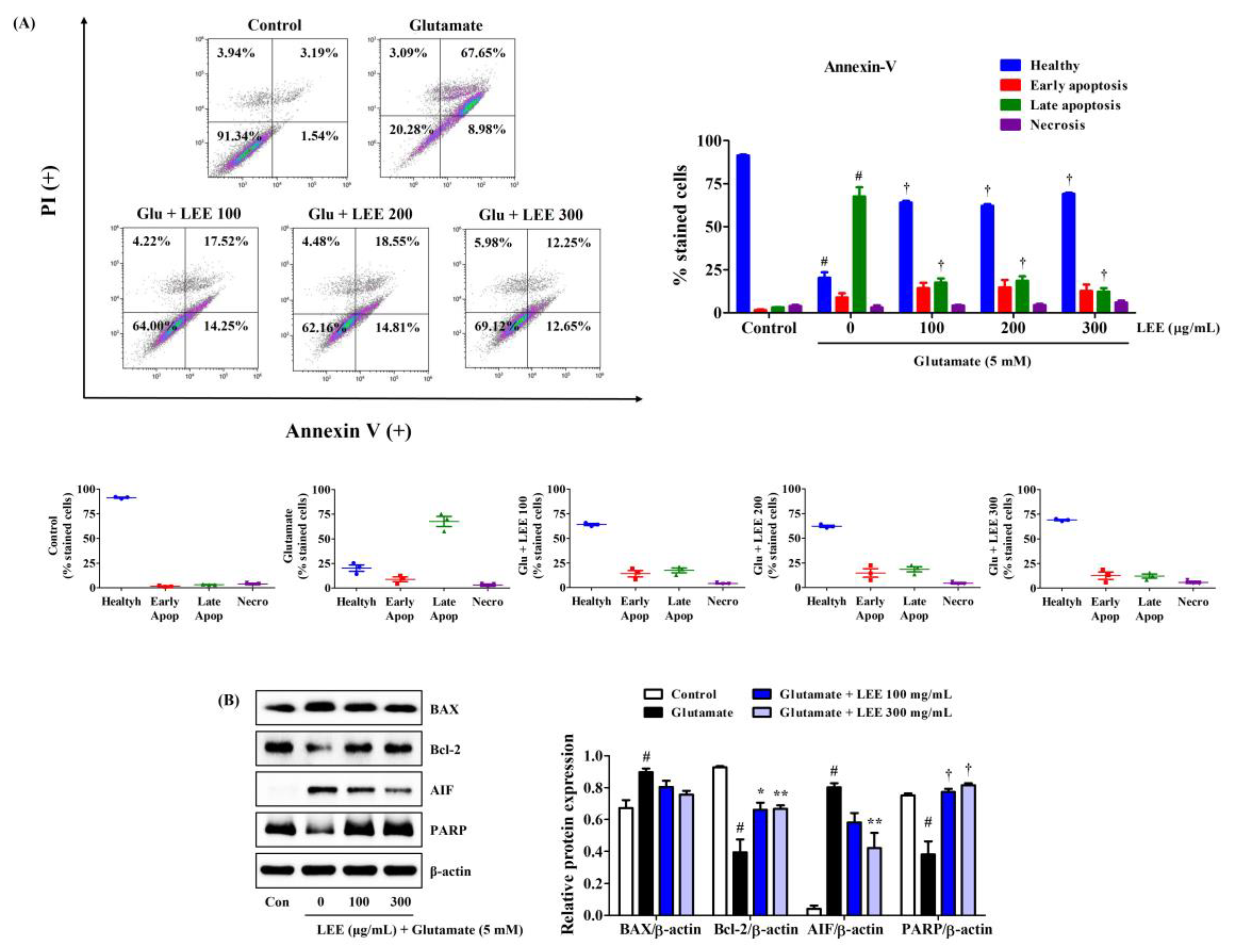
3.9. LEE Suppressed Glutamate-Induced Apoptosis of HT22 Cells
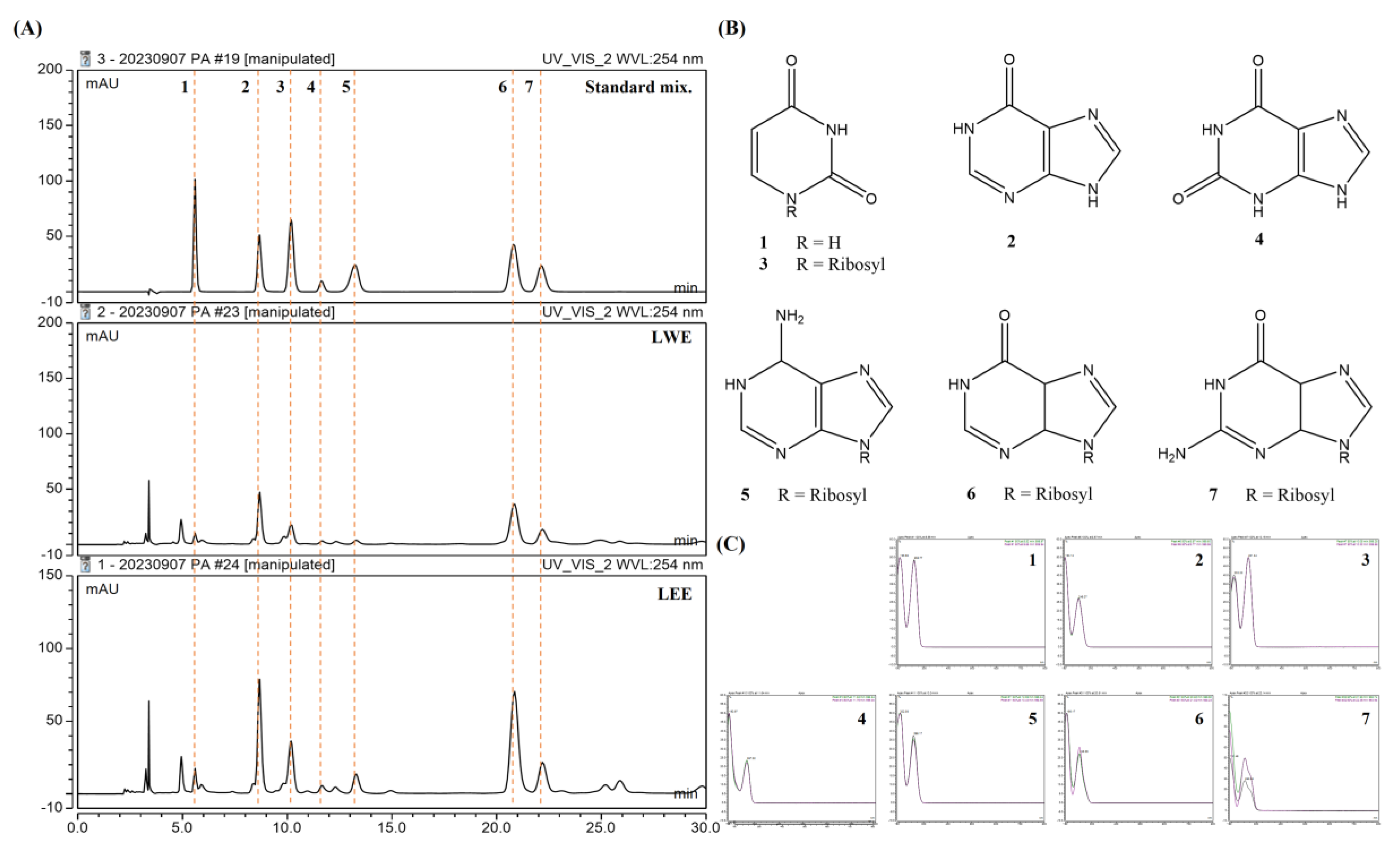
3.10. Identification of Potential Bioactive Components in LWE and LEE Using HPLC-DAD
3.11. Validation of the Analytical HPLC Method
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Swerdlow, R.H.; Burns, J.M.; Khan, S.M. The Alzheimer’s Disease Mitochondrial Cascade Hypothesis. J. Alzheimers Dis. 2010, 20, S265–S279. [Google Scholar] [CrossRef]
- Glezer, I.; Simard, A.R.; Rivest, S. Neuroprotective role of the innate immune system by microglia. Neuroscience 2007, 147, 867–883. [Google Scholar] [CrossRef]
- Ryter, S.W.; Kim, H.P.; Hoetzel, A.; Park, J.W.; Nakahira, K.; Wang, X.; Choi, A.M.K. Mechanisms of cell death in oxidative stress. Antioxid. Redox Signal. 2007, 9, 49–89. [Google Scholar] [CrossRef] [PubMed]
- Baillet, A.; Chanteperdrix, V.; Trocme, C.; Casez, P.; Garrel, C.; Besson, G. The Role of Oxidative Stress in Amyotrophic Lateral Sclerosis and Parkinson’s Disease. Neurochem. Res. 2010, 35, 1530–1537. [Google Scholar] [CrossRef] [PubMed]
- Niranjan, R. The role of inflammatory and oxidative stress mechanisms in the pathogenesis of Parkinson’s disease: Focus on astrocytes. Mol. Neurobiol. 2014, 49, 28–38. [Google Scholar] [CrossRef] [PubMed]
- Chang, L.; Karin, M. Mammalian MAP kinase signalling cascades. Nature 2001, 410, 37–40. [Google Scholar] [CrossRef] [PubMed]
- Cho, K.H.; Kim, D.C.; Yoon, C.S.; Ko, W.M.; Lee, S.J.; Sohn, J.H.; Jang, J.H.; Ahn, J.S.; Kim, Y.C.; Oh, H. Anti-neuroinflammatory effects of citreohybridonol involving TLR4-MyD88-mediated inhibition of NF-small ka, CyrillicB and MAPK signaling pathways in lipopolysaccharide-stimulated BV2 cells. Neurochem. Int. 2016, 95, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Zucoloto, A.Z.; Manchope, M.F.; Staurengo-Ferrari, L.; Pinho-Ribeiro, F.A.; Zarpelon, A.C.; Saraiva, A.L.L.; Cecílio, N.T.; Alves-Filho, J.C.; Cunha, T.M.; Menezes, G.B.; et al. Probucol attenuates lipopolysaccharide-induced leukocyte recruitment and inflammatory hyperalgesia: Effect on NF-кB activation and cytokine production. Eur. J. Pharmacol. 2017, 809, 52–63. [Google Scholar] [CrossRef] [PubMed]
- Otterbein, L.E.; Bach, F.H.; Alam, J.; Soares, M.; Tao Lu, H.; Wysk, M.; Davis, R.J.; Flavell, R.A.; Choi, A.M. Carbon monoxide has anti-inflammatory effects involving the mitogen-activated protein kinase pathway. Nat. Med. 2000, 6, 422–428. [Google Scholar] [CrossRef]
- Lim, C.S.; Jin, D.Q.; Mok, H.; Oh, S.J.; Lee, J.U.; Hwang, J.K.; Ha, I.; Han, J.S. Antioxidant and antiinflammatory activities of xanthorrhizol in hippocampal neurons and primary cultured microglia. J. Neurosci. Res. 2005, 82, 831–838. [Google Scholar] [CrossRef]
- Kumar, H.; Koppula, S.; Kim, I.S.; More, S.V.; Kim, B.W.; Choi, D.K. Nuclear factor erythroid 2-related factor 2 signaling in Parkinson disease: A promising multi therapeutic target against oxidative stress, neuroinflammation and cell death. CNS Neurol. Disord. Drug Targets 2012, 11, 1015–1029. [Google Scholar] [CrossRef]
- Bian, F.; Xiao, Y.; Zaheer, M.; Volpe, E.A.; Pflugfelder, S.C.; Li, D.Q.; De Paiva, C.S. Inhibition of NLRP3 Inflammasome Pathway by Butyrate Improves Corneal Wound Healing in Corneal Alkali Burn. Int. J. Mol. Sci. 2017, 18, 562. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.W.; Yang, S.J.; Na, J.M.; Hahn, H.G.; Cho, S.W. 3-(Naphthalen-2-yl(propoxy)methyl)azetidine hydrochloride attenuates NLRP3 inflammasome-mediated signaling pathway in lipopolysaccharide-stimulated BV2 microglial cells. Biochem. Biophys. Res. Commun. 2018, 495, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Dostert, C.; Mayor, A.; Martinon, F.; Tschopp, J. Activation of the NALP3 inflammasome is triggered by low intracellular potassium concentration. Cell Death Differ. 2007, 14, 1583–1589. [Google Scholar]
- Watroba, M.; Dudek, I.; Skoda, M.; Stangret, A.; Rzodkiewicz, P.; Szukiewicz, D. Sirtuins, epigenetics and longevity. Ageing Res. Rev. 2017, 40, 11–19. [Google Scholar] [CrossRef]
- He, M.; Chiang, H.H.; Luo, H.; Zheng, Z.; Qiao, Q.; Wang, L.; Tan, M.; Ohkubo, R.; Mu, W.C.; Zhao, S.; et al. An acetylation switch of the NLRP3 inflammasome regulates aging-associated chronic inflammation and insulin resistance. Cell Metab. 2020, 31, 580–591. [Google Scholar] [CrossRef]
- Youm, Y.H.; Nguyen, K.Y.; Grant, R.W.; Goldberg, E.L.; Bodogai, M.; Kim, D.; D’Agostino, D.; Planavsky, N.; Lupfer, C.; Kanneganti, T.D.; et al. The ketone metabolite beta-hydroxybutyrate blocks NLRP3 inflammasome-mediated inflammatory disease. Nat. Med. 2015, 21, 263–269. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Zhou, X.; Cheng, X.; Lin, L.; Wang, Q.; Zhan, R.; Wu, Q.; Liu, S. Protective Effect of Ferulic Acid on Lipopolysaccharide-Induced BV2 Microglia Inflammation via AMPK/mTOR Signaling Pathway. Molecules 2023, 28, 3482. [Google Scholar] [CrossRef]
- Paula-Lima, A.C.; Brito-Moreira, J.; Ferreira, S.T. Deregulation of excitatory neurotransmission underlying synapse failure in Alzheimer’s disease. J. Neurochem. 2013, 126, 191–202. [Google Scholar] [CrossRef]
- Kritis, A.A.; Stamoula, E.G.; Paniskaki, K.A.; Vavilis, T.D. Researching glutamate-induced cytotoxicity in different cell lines: A comparative/collective analysis/study. Front. Cell. Neurosci. 2015, 9, 91. [Google Scholar] [CrossRef]
- Xu, T.; Liu, X.; Wang, S.; Kong, H.; Yu, X.; Liu, C.; Song, H.; Gao, P.; Zhang, X. Effect of Pheretima aspergillum on reducing fibrosis: A systematic review and meta-analysis. Front. Pharmacol. 2022, 13, 1039553. [Google Scholar] [CrossRef] [PubMed]
- Huang, P.C.; Shibu, M.A.; Kuo, C.H.; Han, C.K.; Chen, Y.S.; Lo, F.Y.; Li, H.; Viswanadha, V.P.; Lai, C.H.; Li, X.; et al. Pheretima aspergillum extract attenuates high-KCl-induced mitochondrial injury and pro-fibrotic events in cardiomyoblast cells. Environ. Toxicol. 2019, 34, 921–927. [Google Scholar] [CrossRef] [PubMed]
- Shi, Q.; Wang, X.; Liu, J.; Xiang, X.; Su, M.; Huang, R.; Song, C. Anti-Asthma Effect of an Active Components Group from Decoction of Pheretima Aspergillum and Its Chemical Composition Characterized by Liquid Chromatography-Quadrupole Time of Flight Mass Spectrometry. Iran J. Pharm. Res. 2019, 18, 867–876. [Google Scholar]
- Jeong, Y.H.; Oh, Y.C.; Cho, W.K.; Yim, N.H.; Ma, J.Y. Anti-inflammatory effect of Rhapontici Radix ethanol extract via inhibition of NF-κB and MAPK and induction of HO-1 in macrophages. Mediators Inflamm. 2016, 2016, 7216912. [Google Scholar] [CrossRef] [PubMed]
- Oh, Y.C.; Jeong, Y.H.; Li, W.; Go, Y. Angelicae Gigantis Radix regulates LPS-induced neuroinflammation in BV2 microglia by inhibiting NF-κB and MAPK activity and inducing Nrf-2 activity. Molecules 2019, 24, 3755. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.S.; Xiang, Y.; Cui, Y.L.; Lin, K.M.; Zhang, X.F. Dietary blue pigments derived from genipin, attenuate inflammation by inhibiting LPS-induced iNOS and COX-2 expression via the NF-κB inactivation. PLoS ONE 2012, 7, e34122. [Google Scholar] [CrossRef]
- Bradford, M.M. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal. Biochem. 1976, 72, 248–254. [Google Scholar] [CrossRef]
- Baek, S.Y.; Kim, M.R. Neuroprotective effect of carotenoid-rich enteromorpha prolifera extract via TrkB/Akt pathway against oxidative stress in hippocampal neuronal cells. Marine Drugs 2020, 18, 372. [Google Scholar] [CrossRef]
- Tan, S.; Sagara, Y.; Liu, Y.; Maher, P.; Schubert, D. The regulation of reactive oxygen species production during programmed cell death. J. Cell Biol. 1998, 141, 1423–1432. [Google Scholar] [CrossRef]
- Eikelenboom, P.; Veerhuis, R. The importance of inflammatory mechanisms for the development of Alzheimer’s disease. Exp. Gerontol. 1999, 34, 453–461. [Google Scholar] [CrossRef]
- Brown, J.; Wang, H.; Hajishengallis, G.N.; Martin, M. TLR-signaling networks: An integration of adaptor molecules, kinases, and cross-talk. J. Dent. Res. 2011, 90, 417–427. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Tian, F.; Zhang, Y.; Wu, M.; Mao, R.; Le, Z.; Xu, D.; Cao, H.; Ma, Z. Chromatographic Fingerprint and Quantitative Analysis of Commercial Pheretima aspergillum (Guang Dilong) and Its Adulterants by UPLC-DAD. Int. J. Anal. Chem. 2019, 2019, 4531092. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Liu, H.; Zhang, C.; Wei, A.; Ao, H.; Liu, F.; Li, M.; Guo, L.; Ye, Q. Combination of c oxidase subunit I based deoxyribonucleic acid barcoding and HPLC techniques for the identification and quality evaluation of Pheretima aspergillum. J. Sep. Sci. 2020, 43, 2989–2995. [Google Scholar] [CrossRef] [PubMed]
- Stone, T.W. Adenosine, neurodegeneration and neuroprotection. Neurol. Res. 2005, 27, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, J.A.; Sebastiao, A.M.; de Mendonca, A. Participation of adenosine receptors in neuroprotection. Drug News Perspect. 2003, 16, 80–86. [Google Scholar] [CrossRef]
- Datta, A.; Suthar, P.; Sarmah, D.; Jadhav, P.; Shah, J.; Katamneni, M.; Bhosale, N.; Gupta, V.; Bohra, M.; Baidya, F.; et al. Inosine attenuates post-stroke neuroinflammation by modulating inflammasome mediated microglial activation and polarization. Biochim. Biophys. Acta Mol. Basis Dis. 2023, 1869, 166771. [Google Scholar] [CrossRef]
- Ruhal, P.; Dhingra, D. Inosine improves cognitive function and decreases aging-induced oxidative stress and neuroinflammation in aged female rats. Inflammopharmacology 2018, 26, 1317–1329. [Google Scholar] [CrossRef]
- Shen, H.; Chen, G.J.; Harvey, B.K.; Bickford, P.C.; Wang, Y. Inosine reduces ischemic brain injury in rats. Stroke 2005, 36, 654–659. [Google Scholar] [CrossRef]
- Dal-Cim, T.; Ludka, F.K.; Martins, W.C.; Reginato, C.; Parada, E.; Egea, J.; López, M.G.; Tasca, C.I. Guanosine controls inflammatory pathways to afford neuroprotection of hippocampal slices under oxygen and glucose deprivation conditions. J. Neurochem. 2013, 126, 437–450. [Google Scholar] [CrossRef]
- Dal-Cim, T.; Martins, W.C.; Thomaz, D.T.; Coelho, V.; Poluceno, G.G.; Lanznaster, D.; Vandresen-Filho, S.; Tasca, C.I. Neuroprotection Promoted by Guanosine Depends on Glutamine Synthetase and Glutamate Transporters Activity in Hippocampal Slices Subjected to Oxygen/Glucose Deprivation. Neurotox. Res. 2016, 29, 460–468. [Google Scholar] [CrossRef]
- Haskó, G.; Kuhel, D.G.; Németh, Z.H.; Mabley, J.G.; Stachlewitz, R.F.; Virág, L.; Lohinai, Z.; Southan, G.J.; Salzman, A.L.; Szabó, C. Inosine inhibits inflammatory cytokine production by a posttranscriptional mechanism and protects against endotoxin-induced shock. J. Immunol. 2000, 164, 1013–1019. [Google Scholar]
- Souza, D.G.; Bellaver, B.; Bobermin, L.D.; Souza, D.O.; Quincozes-Santos, A. Anti-aging effects of guanosine in glial cells. Purinergic Signal. 2016, 12, 697–706. [Google Scholar] [CrossRef] [PubMed]
- Bellaver, B.; Souza, D.G.; Bobermin, L.D.; Gonçalves, C.A.; Souza, D.O.; Quincozes-Santos, A. Guanosine inhibits LPS-induced pro-inflammatory response and oxidative stress in hippocampal astrocytes through the heme oxygenase-1 pathway. Purinergic Signal. 2015, 11, 571–580. [Google Scholar] [CrossRef]
- Sturm, C.D.; Frisella, W.A.; Yoon, K.W. Attenuation of potassium cyanide-mediated neuronal cell death by adenosine. J. Neurosurg. 1993, 79, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Khanal, S.; Bok, E.; Kim, J.; Park, G.H.; Choi, D.Y. Dopaminergic neuroprotective effects of inosine in MPTP-induced parkinsonian mice via brain-derived neurotrophic factor upregulation. Neuropharmacology 2023, 238, 109652. [Google Scholar] [CrossRef]
- Albrecht, P.; Henke, N.; Tien, M.L.; Issberner, A.; Bouchachia, I.; Maher, P.; Lewerenz, J.; Methner, A. Extracellular cyclic GMP and its derivatives GMP and guanosine protect from oxidative glutamate toxicity. Neurochem. Int. 2013, 62, 610–619. [Google Scholar] [CrossRef] [PubMed]
- Spector, R. Hypoxanthine transport through the blood-brain barrier. Neurochem. Res. 1987, 12, 791–796. [Google Scholar] [CrossRef]
- Cornford, E.M.; Oldendorf, W.H. Independent blood-brain barrier transport systems for nucleic acid precursors. Biochim. Biophys. Acta 1975, 394, 211–219. [Google Scholar] [CrossRef]
| Target Gene | Primer Sequence |
|---|---|
| TNF-α | F: 5′-TTCTGTCTACTGAACTTCGGGGTGATCGGTCC-3′ |
| R: 5′-GTATGAGATAGCAAATCGGCTGACGGTGTGGG-3′ | |
| IL-6 | F: 5′-TCCAGTTGCCTTCTTGGGAC-3′ |
| R: 5′-GTGTAATTAAGCCTCCGACTTG-3′ | |
| IL-1β | F: 5′-ATGGCAACTGTTCCTGAACTCAACT-3′ |
| R: 5′-CAGGACAGGTATAGATTCTTTCCTTT-3′ | |
| iNOS | F: 5′-GGCAGCCTGTGAGACCTTTG-3′ |
| R: 5′-GCATTGGAAGTGAAGCGTTTC-3′ | |
| COX-2 | F: 5′-TGAGTACCGCAAACGCTTCTC-3′ |
| R: 5′-TGGACGAGGTTTTTCCACCAG-3′ | |
| HO-1 | F: 5′-TGAAGGAGGCCACCAAGGAGG-3′ |
| R: 5′-AGAGGTCACCCAGGTAGCGGG-3′ | |
| β-actin | F: 5′-AGAGGGAAATCGTGCGTGAC-3′ |
| R: 5′-CAATAGTGATGACCTGGCCGT-3′ |
| Antibody | Corporation | Product No. | RRID | Dilution Rate |
|---|---|---|---|---|
| P-ERK | Cell Signaling | #4377 | AB_331775 | 1:1000 |
| ERK | Cell Signaling | #9102 | AB_330744 | 1:1000 |
| P-p38 | Cell Signaling | #9211 | AB_331641 | 1:1000 |
| P38 | Cell Signaling | #9212 | AB_330713 | 1:1000 |
| P-JNK | Cell Signaling | #9251 | AB_331659 | 1:1000 |
| JNK | Cell Signaling | #9252 | AB_2250373 | 1:1000 |
| β-actin | Cell Signaling | #4970 | AB_2223172 | 1:1000 |
| NF-κB p65 | Cell Signaling | #8242 | AB_10859369 | 1:1000 |
| TBP | Cell Signaling | #8515 | AB_10949159 | 1:1000 |
| iNOS | Cell Signaling | #2982 | AB_1078202 | 1:1000 |
| COX-2 | Cell Signaling | #4842 | AB_2084968 | 1:5000 |
| HO-1 | Cell Signaling | #82206 | AB_2799989 | 1:1000 |
| Nrf-2 | Cell Signaling | #12721 | AB_2715528 | 1:1000 |
| NLRP3 | Cell Signaling | #15101 | AB_2722591 | 1:1000 |
| C-Caspase-1 | Cell Signaling | #89332 | AB_2923067 | 1:1000 |
| IL-18 | Cell Signaling | #57058 | 1:1000 | |
| SIRT2 | Cell Signaling | #12650 | AB_2716762 | 1:1000 |
| P2X7 | Cell Signaling | #13809 | AB_2798319 | 1:1000 |
| BAX | Cell Signaling | #2772 | AB_10695870 | 1:1000 |
| Bcl-2 | Cell Signaling | #3498 | AB_1903907 | 1:1000 |
| AIF | Cell Signaling | #4642 | AB_2224542 | 1:1000 |
| PARP | Cell Signaling | #9532 | AB_659884 | 1:1000 |
| 2nd anti-mouse | Cell Signaling | #7076 | AB_330924 | 1:5000 |
| 2nd anti-rabbit | Cell Signaling | #7074 | AB_2099233 | 1:5000 |
| Linear Regression Equation a | Correlation Coefficient (n = 5) | LOD b (µg/mL) | LOQ c (µg/mL) | Sample | tR (min) | Measured Amount (µg/mL) | RSD (%) | Contents (μg/mg) | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | y = 0.3665x + 0.0024 | 1.0000 | 0.08 | 0.24 | LWE | 5.63 | 3.77 ± 0.01 | 0.65 | 0.15 |
| LEE | 5.63 | 6.71 ± 0.02 | 0.93 | 0.27 | |||||
| 2 | y = 0.4002x − 0.0423 | 0.9999 | 0.50 | 1.52 | LWE | 8.77 | 24.72 ± 0.01 | 0.06 | 0.99 |
| LEE | 8.77 | 42.55 ± 0.07 | 0.39 | 1.70 | |||||
| 3 | y = 0.1998x − 0.0104 | 1.0000 | 0.33 | 1.00 | LWE | 10.24 | 27.79 ± 0.14 | 2.58 | 1.11 |
| LEE | 10.25 | 57.49 ± 0.11 | 0.94 | 2.30 | |||||
| 4 | y = 0.9758x + 0.0488 | 0.9995 | 0.02 | 0.05 | LWE | 11.81 | 0.87 ± 0.02 | 2.39 | 0.03 |
| LEE | 11.8 | 1.63 ± 0.04 | 2.47 | 0.07 | |||||
| 5 | y = 0.2662x + 0.0414 | 1.0000 | 0.01 | 0.01 | LWE | 13.39 | 4.31 ± 0.02 | 1.77 | 0.17 |
| LEE | 13.39 | 17.67 ± 0.06 | 1.30 | 0.71 | |||||
| 6 | y = 0.2061x + 0.0073 | 1.0000 | 0.51 | 1.54 | LWE | 21.07 | 79.46 ± 0.03 | 0.18 | 3.18 |
| LEE | 21.05 | 150.48 ± 0.26 | 0.83 | 6.02 | |||||
| 7 | y = 0.2612x + 0.0354 | 1.0000 | 0.50 | 1.52 | LWE | 22.42 | 18.65 ± 0.14 | 2.92 | 0.75 |
| LEE | 22.41 | 33.53 ± 0.11 | 1.21 | 1.34 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oh, Y.-C.; Jeong, Y.H.; Yang, H.J.; Li, W.; Ma, J.Y. Lumbricus Extract Prevents LPS-Induced Inflammatory Activation of BV2 Microglia and Glutamate-Induced Hippocampal HT22 Cell Death by Suppressing MAPK/NF-κB/NLRP3 Signaling and Oxidative Stress. Curr. Issues Mol. Biol. 2023, 45, 9926-9942. https://doi.org/10.3390/cimb45120620
Oh Y-C, Jeong YH, Yang HJ, Li W, Ma JY. Lumbricus Extract Prevents LPS-Induced Inflammatory Activation of BV2 Microglia and Glutamate-Induced Hippocampal HT22 Cell Death by Suppressing MAPK/NF-κB/NLRP3 Signaling and Oxidative Stress. Current Issues in Molecular Biology. 2023; 45(12):9926-9942. https://doi.org/10.3390/cimb45120620
Chicago/Turabian StyleOh, You-Chang, Yun Hee Jeong, Hye Jin Yang, Wei Li, and Jin Yeul Ma. 2023. "Lumbricus Extract Prevents LPS-Induced Inflammatory Activation of BV2 Microglia and Glutamate-Induced Hippocampal HT22 Cell Death by Suppressing MAPK/NF-κB/NLRP3 Signaling and Oxidative Stress" Current Issues in Molecular Biology 45, no. 12: 9926-9942. https://doi.org/10.3390/cimb45120620
APA StyleOh, Y.-C., Jeong, Y. H., Yang, H. J., Li, W., & Ma, J. Y. (2023). Lumbricus Extract Prevents LPS-Induced Inflammatory Activation of BV2 Microglia and Glutamate-Induced Hippocampal HT22 Cell Death by Suppressing MAPK/NF-κB/NLRP3 Signaling and Oxidative Stress. Current Issues in Molecular Biology, 45(12), 9926-9942. https://doi.org/10.3390/cimb45120620








