Static Magnetic Field Reduces the Anticancer Effect of Hinokitiol on Melanoma Malignant Cells—Gene Expression and Redox Homeostasis Studies
Abstract
1. Introduction
2. Results
2.1. Cytotoxicity of Hinokitiol
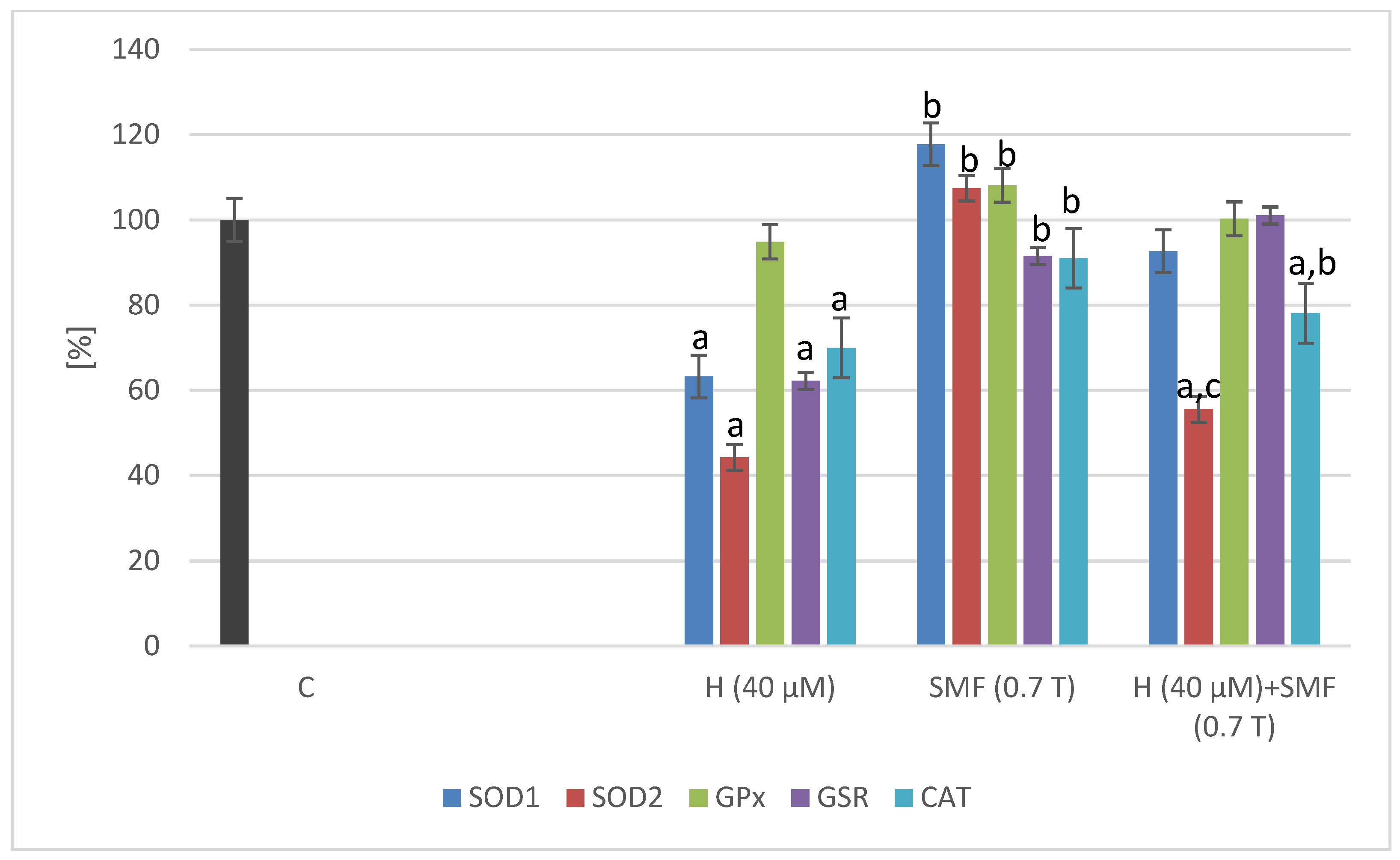
2.2. Effect of Hinokitiol and SMF on the Antioxidant Gene Expression
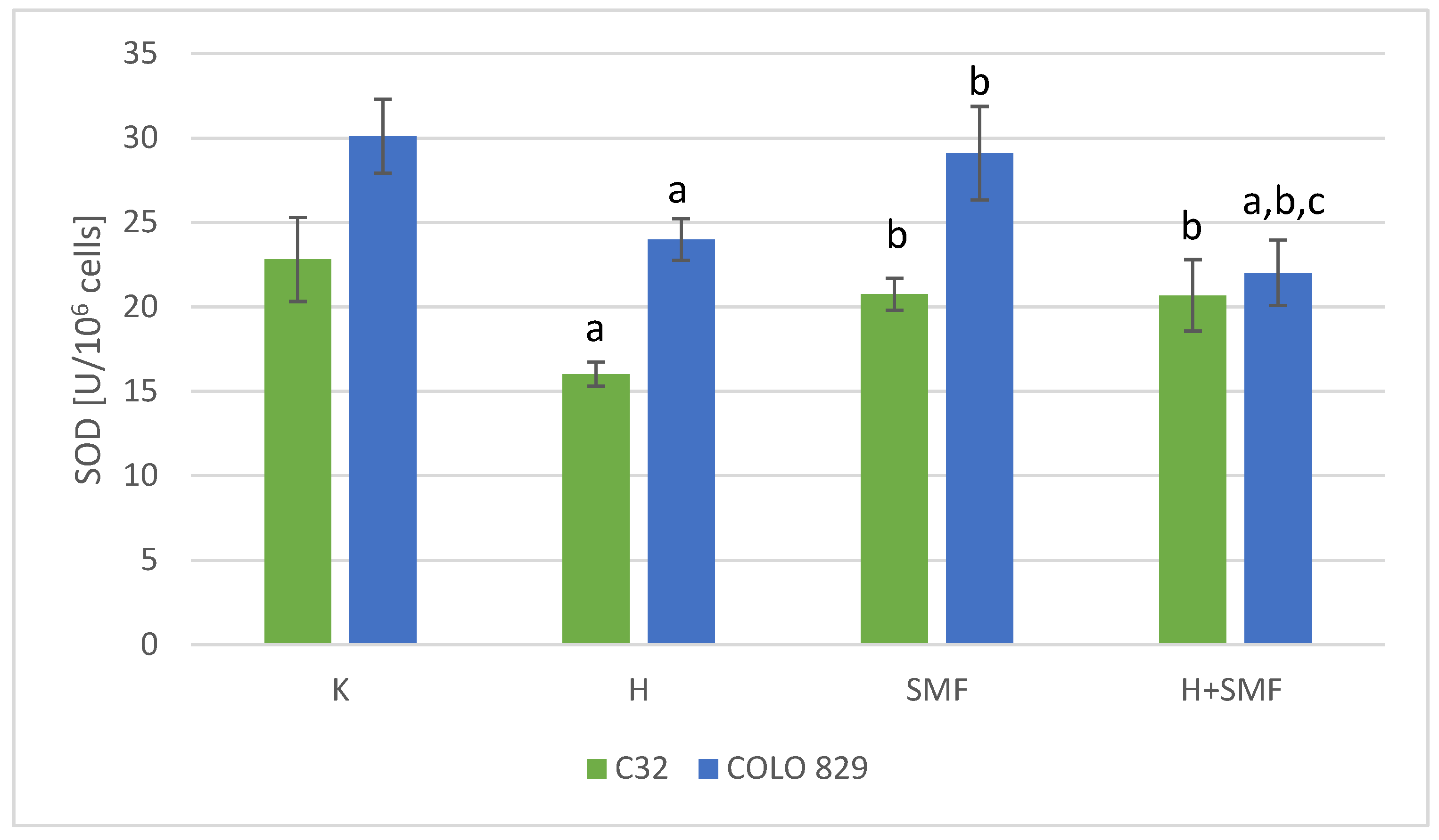
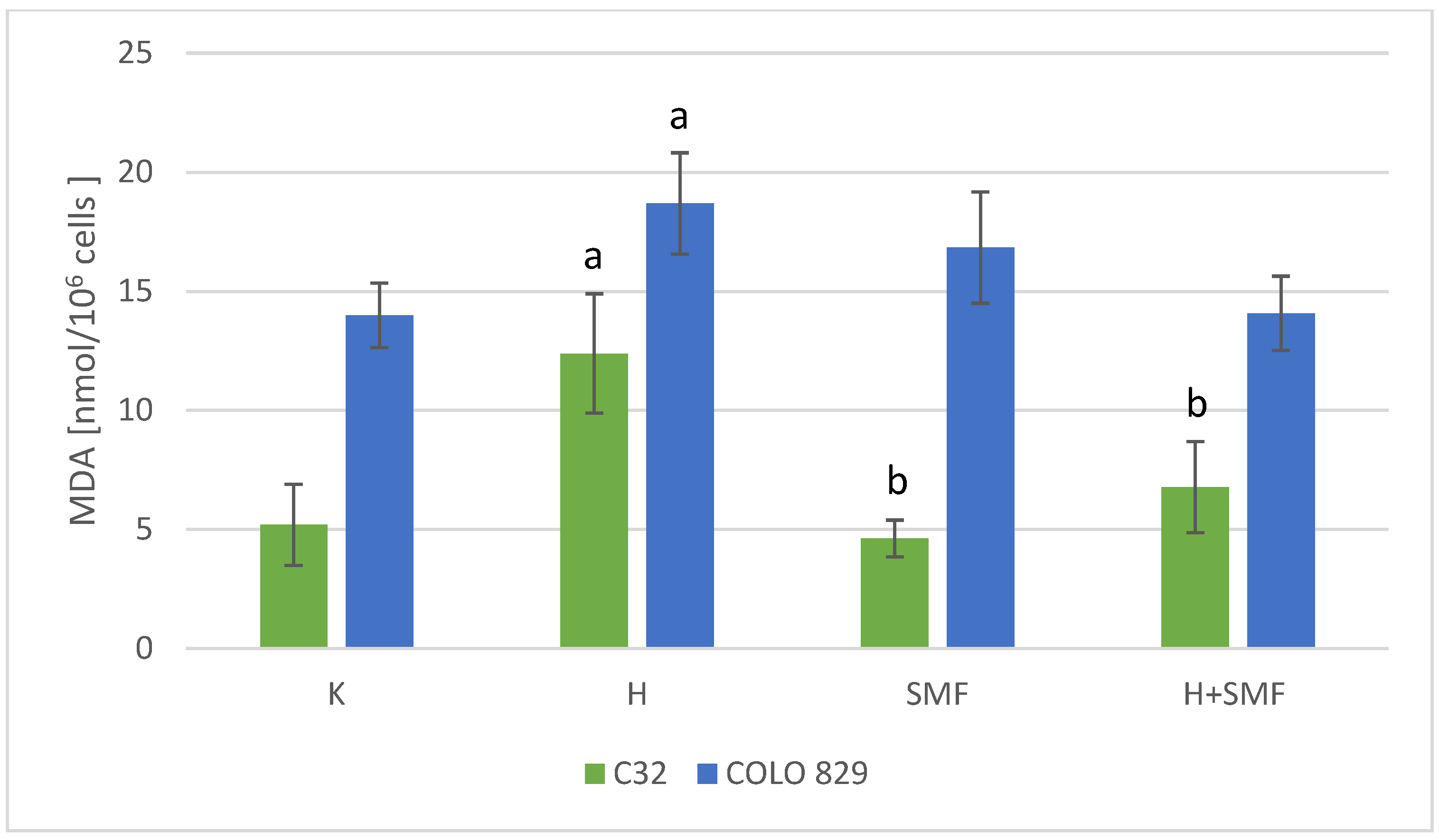
2.3. Effect of Hinokitiol and SMF on the Parameters of Redox Homeostasis
3. Discussion
4. Materials and Methods
4.1. Chemicals
4.2. Melanoma Cell Culture
4.3. Hinokitiol Cytotoxicity
4.4. Static Magnetic Field Exposure
4.5. Preparing the Cell Lysates
4.6. Biochemical Assays
4.6.1. Determination of the Activity of Antioxidant Enzymes
4.6.2. Lipid Peroxidation Assay
4.7. RNA Extraction
Quantitative Real-Time RT-qPCR Assay
4.8. Statistical Analyses
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chiriboga, L.; Meehan, S.; Osman, I.; Glick, M.; de la Cruz, G.; Howell, B.S.; Friedman-Jiménez, G.; Schneider, R.J.; Jamal, S. Endothelin-1 in the tumor microenvironment correlates with melanoma invasion. Melanoma Res. 2016, 26, 236–244. [Google Scholar] [CrossRef] [PubMed]
- Qin, M.; Shao, B.; Lin, L.; Zhang, Z.-Q.; Sheng, Z.-G.; Qin, L.; Shao, J.; Zhu, B.-Z. Molecular mechanism of the unusual biphasic effects of the natural compound hinokitiol on iron-induced cellular DNA damage. Free Rad. Biol. Med. 2023, 194, 163–171. [Google Scholar] [CrossRef] [PubMed]
- Byeon, S.E.; Lee, Y.G.; Kim, J.-C.; Han, J.G.; Lee, H.Y.; Cho, J.Y. Hinokitiol, a natural tropolone derivative, inhibits TNF-α production in LPS-activated macrophages via suppression of NF-κB. Planta Med. 2008, 74, 828–833. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.-H.; Lu, S.-H.; Chang, C.-C.; Thomas, P.A.; Jayakumar, T.; Sheu, J.-R. Hinokitiol, a tropolone derivative, inhibits mouse melanoma (B16-F10) cell migration and in vivo tumor formation. Eur. J. Pharmacol. 2015, 746, 148–157. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.; He, J.; Ye, X.; Zhu, J.; Hu, X.; Shen, M. β-Thujaplicin induces autophagic cell death, apoptosis, and cell cycle arrest through ROS-mediated Akt and p38/ERK MAPK signaling in human hepatocellular carcinoma. Cell Death Dis. 2019, 10, 255. [Google Scholar] [CrossRef]
- Wei, K.-C.; Chen, R.-F.; Chen, Y.F.; Lin, C.-H. Hinokitiol suppresses growth of B16 melanoma by activating ERK/MKP3/proteosome pathway to downregulate survivin expression. Toxicol. Appl. Pharmacol. 2019, 366, 35–45. [Google Scholar] [CrossRef] [PubMed]
- Jayakumar, T.; Liu, C.-H.; Wu, G.Y.; Lee, T.-Y.; Manubolu, M.; Hsieh, C.-Y.; Sheu, J.R. Hinokitiol Inhibits Migration of A549 Lung Cancer Cells via Suppression of MMPs and Induction of Antioxidant Enzymes and Apoptosis. Int. J. Mol. Sci. 2018, 19, 939. [Google Scholar] [CrossRef] [PubMed]
- Lu, S.; Song, Y.; Luo, R.; Li, S.; Li, G.; Wang, K.; Lia, Z.; Wang, B.; Ke, W.; Xiang, Q. Ferroportin-dependent iron homeostasis protects against oxidative stress-induced nucleus pulposus cell ferroptosis and ameliorates intervertebral disc degeneration in vivo. Oxid. Med. Cell. Longev. 2021, 2021, 6670497. [Google Scholar] [CrossRef] [PubMed]
- Hoang, X.; Han, M. A possible application of hinokitiol as a natural zinc ionophore and anti-infective agent for the prevention and treatment of COVID-19 and viral infections. Med. Hypotheses 2020, 145, 110333. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Yuan, X.; Lv, H.; Che, J.; Wang, S.; Shang, P. Biophysical mechanisms underlying the effects of static magnetic fields on biological systems. Prog. Biophys. Mol. Biol. 2023, 177, 14–23. [Google Scholar] [CrossRef] [PubMed]
- Gurhan, H.; Bruzon, R.; Kandala, S.; Greenebaum, B.; Barnes, F. Effects induced by a weak static magnetic field of different intensities on HT-1080 fibrosarcoma cells. Bioelectromagnetics 2021, 42, 212–223. [Google Scholar] [CrossRef] [PubMed]
- Song, C.; Yu, B.; Wang, J.; Ji, X.; Zhang, L.; Tian, X.; Yu, X.; Feng, C.; Wang, X.; Zhang, X. Moderate static magnet fields suppress ovarian cancer metastasis via ROS-mediated oxidative stress. Oxidative Med. Cell Longev. 2021, 2021, 7103345. [Google Scholar] [CrossRef] [PubMed]
- Albuquwrque, W.W.; Costa, R.M.; Fernandes, S.; Porto, A.L. Evidences of the static magnetic field influence on cellular systems. Prog. Biophys. Mol. Biol. 2016, 121, 16–28. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Huyan, T.; Chenge, L.; Shang, P.; Zhang, H. 12 T high static magnetic field suppresses osteosarcoma cells proliferation by regulating intracellular ROS and iron status. Exp. Cell Res. 2022, 417, 113223. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Li, J.; Chen, H.; Cai, Y.; Sheng, T.; Wang, P.; Li, Z.; Yang, F.; Gu, N. Magnet-activatable nanoliposomes as intracellular bubble microreactors to enhance drug delivery efficacy and burst cancer cells. Nanoscale 2019, 11, 18854–18865. [Google Scholar] [CrossRef] [PubMed]
- Pawłowska-Góral, K.; Kimsa-Dudek, M.; Synowiec-Wojtarowicz, A.; Orchel, J.; Glinka, M.; Gawron, S. Effect of static magnetic fields and phloretin on antioxidant defense system of human fibroblasts. Environ. Sci. Pollut. Res. 2016, 23, 14989–14996. [Google Scholar] [CrossRef]
- Kimsa-Dudek, M.; Krawczyk, A.; Synowiec-Wojtarowicz, A.; Dudek, S.; Pawłowska-Góral, K. The impact of the co-exposure of melanoma cells to chlorogenic acid and a moderate-strength static magnetic field. J. Food Biochem. 2020, 44, e13512. [Google Scholar] [CrossRef] [PubMed]
- Synowiec-Wojtarowicz, A.; Pawłowska-Góral, K.; Krawczyk, A.; Gawron, S.; Kimsa-Dudek, M. The effect of a static magnetic field and baicalin or baicalein interactions on amelanotic melanoma cell cultures (C32). Mol. Biol. Rep. 2022, 49, 3157–31636. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Song, C.H.; Zhang, L.; Wang, J.; Yu, X.; Yu, B.; Zablotskii, V.; Zhang, X. An upward 9.4 T static magnetic field inhibits DNA synthesis and increases ROS-P53 to suppress lung cancer growth. Transl. Oncol. 2021, 14, 101103. [Google Scholar] [CrossRef] [PubMed]
- Ghodbane, S.; Lahbib, A.; Sakly, M.; Abdelmelek, H. Bioeffects of static magnetic fields; Oxidative stress, genotoxic effects and cancer studies. BioMed Res. Int. 2013, 2013, 602987. [Google Scholar] [CrossRef] [PubMed]
- Shih, Y.-H.; Chang, K.-W.; Hsia, S.-M.; Yu, C.-C.; Fuh, L.-J.; Chi, T.-Y.; Shieh, T.-M. In vitro antimicrobial and anticancer potential of hinokitiol against oral pathogens and oral cancer cell lines. Microbiol. Res. 2013, 168, 254–262. [Google Scholar] [CrossRef] [PubMed]
- Eltamany, E.E.; Elhady, S.S.; Ahmed, H.A.; Badr, J.M.; Noor, A.O.; Ahmed, S.A.; Nafie, M.S. Chemical Profiling, Antioxidant, Cytotoxic Activities and Molecular Docking Simulation of Carrichtera annua DC. (Cruciferae). Antioxidants 2020, 9, 1286. [Google Scholar] [CrossRef] [PubMed]
- Gutteridge, J.; Halliwell, B. Mini-Review: Oxidative stress, redox stress or redox success? Biochem. Biophys. Res. Commun. 2018, 502, 183–186. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Yamauchi, H. Hinokitiol, a metal chelator derived from natural plants, suppresses cell growth and disrupts androgen receptor signaling in prostate carcinoma cell lines. Biochem. Biophys. Res. Commun. 2006, 351, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Lin, S.T.; Chang, W.W.; Liu, L.W.; Li, T.; Kuo, C.Y.; Hsieh, J.L.; Lee, C.H. Hinokitiol induces autophagy in murine breast and colorectal cancer cells. Environ. Toxicol. 2016, 31, 77–84. [Google Scholar] [CrossRef]
- Liu, G.; Obeidy, P.; Ford, S.J.; Tselepis, C.; Sharp, D.M.; Jansson, P.J.; Kalinowski, D.; Kovacevic, Z.; Lovejoy, D.B.; Richardson, D.R. The iron chelator, deferasirox, as a novel strategy for cancer treatment: Oral activity against human lung tumor xenografts and molecular mechanism of action. Mol. Pharmacol. 2013, 83, 179–190. [Google Scholar]
- Deng, Z.Y.; Manz, D.H.; Torti, S.V.; Torti, F.M. Iron-responsive element-binding protein 2 plays an essential role in regulating prostate cancer cell growth. Oncotarget 2017, 8, 82231–82243. [Google Scholar] [CrossRef] [PubMed]
- Synowiec-Wojtarowicz, A.; Krawczyk, A.; Kimsa-Dudek, M. The effect of resveratrol and static magnetic field interactions on the oxidation-reduction parameters of melanoma malignant cells. Appl. Sci. 2023, 13, 8042. [Google Scholar] [CrossRef]
- Tian, W.; Wang, D.; Zha, M.; Yang, X.; Ji, X.; Zhang, L.; Zhang, X. Magnetic field direction differentially impacts the growth of different cell types. Electromagn. Biol. Med. 2018, 37, 114–125. [Google Scholar] [CrossRef] [PubMed]
- Van Huizen, A.V.; Morton, J.M.; Kinsey, L.J.; Von Kannon, D.G.; Birkholz, T.R.; Czajka, J.M.; Cyrus, J.; Barnes, F.S.; Beane, W.S. Weak magnetic fields alter stem cell–mediated growth. Sci. Adv. 2019, 5, 7201. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Ma, Y.; Li, N.; Cao, Y.; Zhu, Y. Natural static magnetic field-induced apoptosis in liver cancer cell. Electromagn. Biol. Med. 2014, 33, 47–50. [Google Scholar] [CrossRef] [PubMed]
- Nieminen, V.; Juntunen, M.; Naarala, J.; Luukkonen, J. Static or 50 Hz magnetic fields at 100 µT do not modify the clonogenic survival of doxorubicin-treated MCF-7 cancer cells. Bioelectrochemistry 2022, 147, 108196. [Google Scholar] [CrossRef]
- Stockert, J.C.; Blazquez-Castro, A.; Canete, M.; Horobin, R.W.; Vilanueva, A. MTT assay for cell viability: Intracellular localization of the formazan product is in lipid droplets. Acta Histochem. 2012, 114, 785–796. [Google Scholar] [CrossRef] [PubMed]
- Glinka, M.; Gawron, S.; Sieroń, A.; Pawłowska-Góral, K.; Cieślar, G.; Sieroń-Stołtny, K. Test chambers for cell culture in static magnetic field. J. Magn. Magn. Mater. 2013, 331, 208–215. [Google Scholar] [CrossRef]
- Gawron, S.; Glinka, M.; Wolnik, T. Magnetyczna komora badawcza dedykowana do hodowli komórek. Zesz. Probl. Masz. Elektr. 2012, 4, 11–16. [Google Scholar]
- Chomczyński, P.; Sacchi, N. The single step method of RNA isolation by acid guanidinium thiocyanate-phenol-chloroform extraction: Twenty-something years on. Nat. Protoc. 2006, 1, 581–585. [Google Scholar] [CrossRef] [PubMed]
- Schmittgen, T.D.; Livak, K.J. Analyzing real-time PCR data by the comparative C(T) method. Nat. Protoc. 2008, 3, 1101–1108. [Google Scholar] [CrossRef] [PubMed]




| Gene | Sequence of Primers | Amplicon Length (bp) |
|---|---|---|
| SOD1 | Forward: 5′-TTGGGCAATGTGACTGCTGACAAA-3′ Reverse: 5′-GGGCGATCCCAATTACACCACAA-3′ | 208 |
| SOD2 | Forward: 5′-CTGATTTGGACAAGCAGCAA-3′ Reverse: 5′-CTGGACAAACCTCAGCCCTA-3 | 199 |
| GSR | Forward: 5′-AGAAATCATCCGTGGCCATGCA-3′ Reverse: 5′-ACCAACAATGACGCTGCGGC-3 | 214 |
| CAT | Forward: 5′-CCTATCCTGACACTCACCGCCATCG-3′ Reverse: 5′-GGATGCTGTGCTCCAGGGCAGA-3 | 201 |
| GPx1 | Forward: 5′-AATGTGGCGTCCCTCTGAGGCA-3′ Reverse: 5′-GCTCGTTCATCTGGGTGTAGTCCCG-3′ | 55 |
| ACTB | Forward: 5′-TCACCCACACTGTGCCCATCTACGA-3′ Reverse: 5′-CAGCGGAACCGCTCATTGCCAATGG-3′ | 295 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Synowiec-Wojtarowicz, A.; Krawczyk, A.; Kimsa-Dudek, M. Static Magnetic Field Reduces the Anticancer Effect of Hinokitiol on Melanoma Malignant Cells—Gene Expression and Redox Homeostasis Studies. Pharmaceuticals 2024, 17, 430. https://doi.org/10.3390/ph17040430
Synowiec-Wojtarowicz A, Krawczyk A, Kimsa-Dudek M. Static Magnetic Field Reduces the Anticancer Effect of Hinokitiol on Melanoma Malignant Cells—Gene Expression and Redox Homeostasis Studies. Pharmaceuticals. 2024; 17(4):430. https://doi.org/10.3390/ph17040430
Chicago/Turabian StyleSynowiec-Wojtarowicz, Agnieszka, Agata Krawczyk, and Magdalena Kimsa-Dudek. 2024. "Static Magnetic Field Reduces the Anticancer Effect of Hinokitiol on Melanoma Malignant Cells—Gene Expression and Redox Homeostasis Studies" Pharmaceuticals 17, no. 4: 430. https://doi.org/10.3390/ph17040430
APA StyleSynowiec-Wojtarowicz, A., Krawczyk, A., & Kimsa-Dudek, M. (2024). Static Magnetic Field Reduces the Anticancer Effect of Hinokitiol on Melanoma Malignant Cells—Gene Expression and Redox Homeostasis Studies. Pharmaceuticals, 17(4), 430. https://doi.org/10.3390/ph17040430






