Sodium Glucose Cotransporter-2 Inhibitors in Non-Diabetic Kidney Disease: Evidence in Experimental Models
Abstract
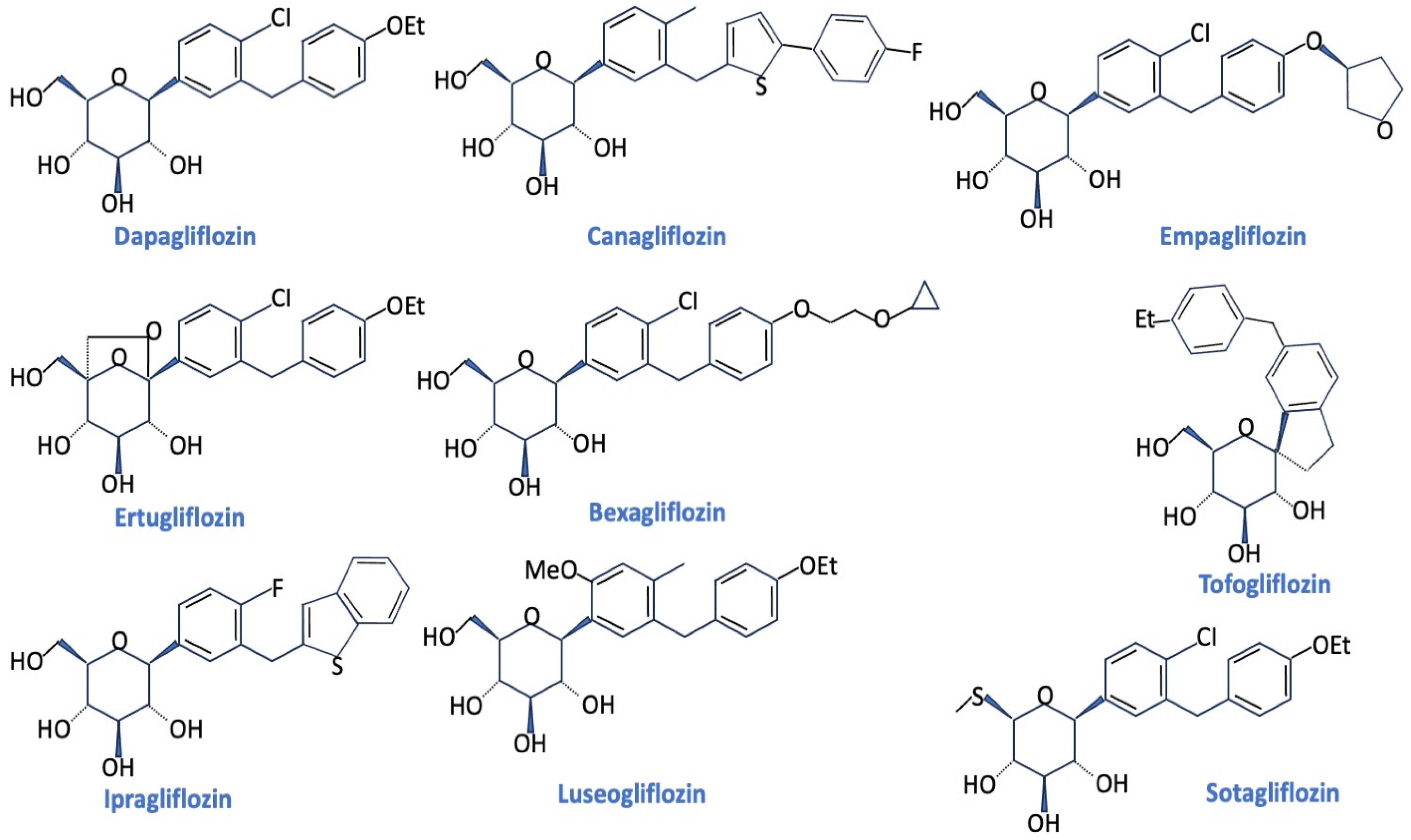
1. Introduction
2. SGLT2 Inhibitors in Experimental Models of Non-Diabetic Kidney Disease
2.1. Hypertensive Nephropathy
2.2. Salt-Sensitive Hypertension and Uninephrectomy DOCA Salt Models
2.3. Polycystic Kidney Disease
2.4. Obesity and Insulin Resistance
2.5. Cisplatin-Induced Nephropathy
2.6. Gentamicin-Induced Nephropathy
2.7. Adenine-Induced Nephropathy
2.8. Protein-Overload Nephropathy
2.9. Oxalate-Induced Nephrocalcinosis
2.10. Cyclosporin Nephropathy
2.11. Adriamycin-Induced Kidney-Injury
2.12. Renal Ischemia-Reperfusion Injury
2.13. Unilateral Ureteric Obstruction
2.14. Subtotal 5/6 Nephrectomy
2.15. Isoprenaline Sympathetic Nervous System Stimulation
2.16. Cardiorenal Syndrome
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zinman, B.; Wanner, C.; Lachin, J.M.; Fitchett, D.; Bluhmki, E.; Hantel, S.; Mattheus, M.; Devins, T.; Johansen, O.E.; Woerle, H.J.; et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N. Engl. J. Med. 2015, 373, 2117–2128. [Google Scholar] [CrossRef] [PubMed]
- Wanner, C.; Inzucchi, S.E.; Lachin, J.M.; Fitchett, D.; von Eynatten, M.; Mattheus, M.; Johansen, O.E.; Woerle, H.J.; Broedl, U.C.; Zinman, B.; et al. Empagliflozin and progression of kidney disease in type 2 diabetes. N. Engl. J. Med. 2016, 375, 323–334. [Google Scholar] [CrossRef] [PubMed]
- Neal, B.; Perkovic, V.; Mahaffey, K.W.; De Zeeuw, D.; Fulcher, G.; Erondu, N.; Shaw, W.; Law, G.; Desai, M.; Matthews, D.R. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N. Engl. J. Med. 2017, 377, 644–657. [Google Scholar] [CrossRef]
- Aguillón, A.R.; Mascarello, A.; Segretti, N.D.; de Azevedo, H.F.Z.; Guimaraes, C.R.W.; Miranda, L.S.M.; de Souza, R.O.M.A. Synthetic Strategies toward SGLT2 Inhibitors. Org. Process Res. Dev. 2018, 22, 467–488. [Google Scholar] [CrossRef]
- Bisignano, P.; Ghezzi, C.; Jo, H.; Polizzi, N.F.; Althoff, T.; Kalyanaraman, C.; Friemann, R.; Jacobson, M.P.; Wright, E.M.; Grabe, M. Inhibitor binding mode and allosteric regulation of Na+-glucose symporters. Nat. Commun. 2018, 9, 5245. [Google Scholar] [CrossRef] [PubMed]
- Thomas, M.C.; Cherney, D.Z.I. The action of SGLT2 inhibitors on metabolism, renal function and blood pressure. Diabetologia 2018, 61, 2098–2107. [Google Scholar] [CrossRef]
- Wanner, C. EMPA-REG Outcome: The nephrologist’s point of view. Am. J. Cardiol. 2017, 120, S59–S67. [Google Scholar] [CrossRef]
- Bonora, B.M.; Avogaro, A.; Fadini, G.P. Extraglycemic effects of SGLT2 Inhibitors: A review of the evidence. Diabetes Metab. Syndrome Obes. Targets Ther. 2020, 13, 161–174. [Google Scholar] [CrossRef]
- de Albuquerque Rocha, N.; Neeland, I.J.; McCullough, P.A.; Toto, R.D.; McGuire, D.K. Effects of sodium glucose co-transporter 2 inhibitors on the kidney. Diabetes Vasc. Dis. Res. 2018, 15, 375–386. [Google Scholar] [CrossRef]
- Jerums, G.; Premaratne, E.; Panagiotopoulos, S.; MacIsaac, R.J. The clinical significance of hyperfiltration in diabetes. Diabetologia 2010, 53, 2093–2104. [Google Scholar] [CrossRef]
- Low, S.; Zhang, X.; Wang, J.; Yeoh, L.Y.; Liu, Y.L.; Ang, K.K.L.; Tang, W.E.; Kwan, P.Y.; Tavintharan, S.; Sum, C.F.; et al. Long-term prospective observation suggests that glomerular hyperfiltration is associated with rapid decline in renal filtration function: A multiethnic study. Diabetes Vasc. Dis. Res. 2018, 15, 417–423. [Google Scholar] [CrossRef]
- Oh, S.W.; Yang, J.H.; Kim, M.G.; Cho, W.Y.; Jo, S.K. Renal hyperfiltration as a risk factor for chronic kidney disease: A health checkup cohort study. PLoS ONE 2020, 15, e0238177. [Google Scholar] [CrossRef]
- Chen, X.; Hocher, C.-F.; Shen, L.; Kramer, B.K.; Hocher, B. Reno-and cardioprotective molecular mechanisms of SGLT2 inhibitors beyond glycemic control: From bedside to bench. Am. J. Physiol. Cell. Physiol. 2023, 325, C661–C681. [Google Scholar] [CrossRef]
- The EMPA-KIDNEY Collaborative Group. Empagliflozin in Patients with Chronic Kidney Disease. N. Engl. J. Med. 2023, 388, 117–127. [Google Scholar] [CrossRef]
- Heerspink, H.J.L.; Stefánsson, B.V.; Correa-Rotter, R.; Chertow, G.M.; Greene, T.; Hou, F.F.; Mann, J.F.E.; McMurray, J.J.V.; Lindberg, M.; Rossing, P.; et al. DAPA-CKD Trial Committees and Investigators. Dapagliflozin in Patients with Chronic Kidney Disease. N. Engl. J. Med. 2020, 383, 1436–1446. [Google Scholar] [CrossRef] [PubMed]
- Heerspink, H.J.L.; Kosiborod, M.; Inzucchi, S.E.; Cherney, D.Z.I. Renoprotective effects of sodium-glucose cotransporter-2 inhibitors. Kidney Int. 2018, 94, 26–39. [Google Scholar] [CrossRef] [PubMed]
- Nespoux, J.; Vallon, V. Renal effects of SGLT2 inhibitors: An update. Curr. Opin. Nephrol. Hypertens. 2020, 29, 190–198. [Google Scholar] [CrossRef] [PubMed]
- Castoldi, G.; Carletti, R.; Ippolito, S.; Colzani, M.; Pelucchi, S.; Zerbini, G.; Perseghin, G.; Zatti, G.; di Gioia, C.R.T. Cardioprotective effects of sodium glucose cotransporter 2 inhibition in angiotensin II-dependent hypertension are mediated by the local reduction of sympathetic activity and inflammation. Int. J. Mol. Sci. 2023, 24, 10710. [Google Scholar] [CrossRef]
- Ashfaq, A.; Meineck, M.; Pautz, A.; Arioglu-Inan, E.; Weinmann-Menke, J.; Michel, M.C. A systematic review on renal effects of SGLT2 inhibitors in rodent models of diabetic nephropathy. Pharmacol. Ther. 2023, 249, 108503. [Google Scholar] [CrossRef]
- Castoldi, G.; Carletti, R.; Ippolito, S.; Colzani, M.; Barzaghi, F.; Stella, A.; Zerbini, G.; Perseghin, G.; di Gioia, C.R.T. Renal anti-fibrotic effect of sodium-glucose cotransporter 2 inhibition in angiotensin II-dependent hypertension. Am. J. Nephrol. 2020, 51, 119–129. [Google Scholar] [CrossRef]
- Reyes-Pardo, H.; Bautista, R.; Vargas-Robles, H.; Rios, A.; Sánchez, D.; Escalante, B. Role of sodium/glucose cotransporter inhibition on a rat model of angiotensin II-dependent kidney damage. BMC Nephrol. 2019, 20, 292. [Google Scholar] [CrossRef]
- Hojná, S.; Kotsaridou, Z.; Vaňourková, Z.; Rauchová, H.; Behuliak, M.; Kujal, P.; Kadlecová, M.; Zicha, J.; Vaněčková, I. Empagliflozin Is Not Renoprotective in Non-Diabetic Rat Models of Chronic Kidney Disease. Biomedicines 2022, 10, 2509. [Google Scholar] [CrossRef]
- Kim, S.; Jo, C.H.; Kim, G.H. Effects of empagliflozin on nondiabetic salt-sensitive hypertension in uninephrectomized rats. Hypertens. Res. 2019, 42, 1905–1915. [Google Scholar] [CrossRef]
- Tauber, P.; Sinha, F.; Berger, R.S.; Gronwald, W.; Dettmer, K.; Kuhn, M.; Trum, M.; Maier, L.S.; Wagner, S.; Schweda, F. Empagliflozin reduces renal hyperfiltration in response to uninephrectomy, but is not nephroprotective in UNx/DOCA/Salt mouse models. Front. Pharmacol. 2021, 12, 761855. [Google Scholar] [CrossRef]
- Mohamed, H.E.; Asker, M.E.; Keshawy, M.M.; Hasan, R.A.; Mahmoud, Y.K. Inhibition of tumor necrosis factor-α enhanced the antifibrotic effect of empagliflozin in an animal model with renal insulin resistance. Mol. Cell. Biochem. 2020, 466, 45–54. [Google Scholar] [CrossRef] [PubMed]
- Ma, Q.; Steiger, S.; Anders, H.J. Sodium glucose transporter-2 inhibition has no renoprotective effects on non-diabetic chronic kidney disease. Physiol. Rep. 2017, 5, e13228. [Google Scholar] [CrossRef] [PubMed]
- Castoldi, G.; Carletti, R.; Ippolito, S.; Colzani, M.; Barzaghi, F.; Stella, A.; Zerbini, G.; Perseghin, G.; Zatti, G.; di Gioia, C.R.T. Sodium-glucose cotransporter 2 inhibition prevents renal fibrosis in cyclosporine nephropathy. Acta Diabetol. 2021, 58, 1059–1070. [Google Scholar] [CrossRef] [PubMed]
- Abbas, N.A.T.; El Salem, A.; Awad, M.M. Empagliflozin, SGLT2 inhibitor, attenuates renal fibrosis in rats exposed to unilateral ureteric obstruction: Potential role of klotho expression. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2018, 391, 1347–1360. [Google Scholar] [CrossRef] [PubMed]
- Zeng, S.; Delic, D.; Chu, C.; Xiong, Y.; Luo, T.; Chen, X.; Gaballa, M.M.S.; Xue, Y.; Chen, X.; Cao, Y.; et al. Antifibrotic effects of low dose SGLT2 Inhibition with empagliflozin in comparison to Ang II receptor blockade with telmisartan in 5/6 nephrectomised rats on high salt diet. Biomed. Pharmacother. 2022, 146, 112606. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.P.; Wu, H.W.; Zhu, T.; Li, X.T.; Zuo, J.; Hasan, A.A.; Reichetzeder, C.; Delic, D.; Yard, B.; Klein, T.; et al. Empagliflozin reduces kidney fibrosis and improves kidney function by alternative macrophage activation in rats with 5/6-nephrectomy. Biomed. Pharmacother. 2022, 156, 113947. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Chen, Y.; Wallace, C.G.; Chen, K.; Cheng, B.; Sung, P.; Li, Y.; Ko, S.; Chang, H.; Yip, H. Early administration of empagliflozin preserved heart function in cardiorenal syndrome in rat. Biomed. Pharmacother. 2019, 109, 658–670. [Google Scholar] [CrossRef]
- Kravtsova, O.; Levchenko, V.; Klemens, C.A.; Rieg, T.; Liu, R.; Staruschenko, A. Effect of SGLT2 inhibition on salt-induced hypertension in female Dahl SS rats. Sci. Rep. 2023, 13, 19231. [Google Scholar] [CrossRef] [PubMed]
- Urbanek, K.; Cappetta, D.; Bellocchio, G.; Coppola, M.A.; Imbrici, P.; Telesca, M.; Donniacuo, M.; Riemma, M.A.; Mele, E.; Cianflone, E.; et al. Dapagliflozin protects the kidney in a non-diabetic model of cardiorenal syndrome. Pharmacol. Res. 2023, 188, 106659. [Google Scholar] [CrossRef] [PubMed]
- Kapoor, S.; Rodriguez, D.; Riwanto, M.; Edenhofer, I.; Segerer, S.; Mitchell, K.; Wüthrich, R.P. Effect of sodium-glucose cotransport inhibition on polycystic kidney disease progression in PCK rats. PLoS ONE 2015, 10, e0125603. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, D.; Kapoor, S.; Edenhofer, I.; Segerer, S.; Riwanto, M.; Kipar, A.; Yang, M.; Mei, C.; Wüthrich, R.P. Inhibition of sodium-glucose cotransporter 2 with dapagliflozin in Han: SPRD rats with polycystic kidney disease. Kidney Blood Press. Res. 2015, 40, 638–647. [Google Scholar] [CrossRef] [PubMed]
- Jaikumkao, K.; Pongchaidecha, A.; Chueakula, N.; Thongnak, L.; Wanchai, K.; Chatsudthipong, V.; Chattipakorn, N.; Lungkaphin, A. Dapagliflozin, a sodium-glucose co-transporter-2 inhibitor, slows the progression of renal complications through the suppression of renal inflammation, endoplasmic reticulum stress and apoptosis in prediabetic rats. Diabetes Obes. Metab. 2018, 20, 2617–2626. [Google Scholar] [CrossRef]
- Thongnak, L.; Chatsudthipong, V.; Kongkaew, A.; Lungkaphin, A. Effects of dapagliflozin and statins attenuate renal injury and liver steatosis in high-fat/high-fructose diet-induced insulin resistant rats. Toxicol. Appl. Pharmacol. 2020, 396, 114997. [Google Scholar] [CrossRef]
- Mohamed, D.I.; Khairy, E.; Saad, S.S.T.; Habib, E.K.; Hamouda, M.A. Potential protective effects of Dapagliflozin in gentamicin induced nephrotoxicity rat model via modulation of apoptosis associated miRNAs. Gene 2019, 707, 198–204. [Google Scholar] [CrossRef]
- Cassis, P.; Locatelli, M.; Cerullo, D.; Corna, D.; Buelli, S.; Zanchi, C.; Villa, S.; Morigi, M.; Remuzzi, G.; Benigni, A.; et al. SGLT2 inhibitor dapagliflozin limits podocyte damage in proteinuric nondiabetic nephropathy. JCI Insight. 2018, 3, e98720. [Google Scholar] [CrossRef]
- Cha, J.J.; Park, H.J.; Yoo, J.A.; Ghee, J.; Cha, D.R.; Kang, Y.S. Dapagliflozin does not protect against adriamycin-induced kidney injury in mice. Kidney Blood Press. Res. 2024, 49, 81–90. [Google Scholar] [CrossRef]
- Chang, Y.K.; Choi, H.; Jeong, J.Y.; Na, K.R.; Lee, K.W.; Lim, B.J.; Choi, D.E. Dapagliflozin, SGLT2 inhibitor, attenuates renal ischemia-reperfusion injury. PLoS ONE 2016, 11, e0158810. [Google Scholar] [CrossRef]
- Zhang, Y.; Thai, K.; Kepecs, D.M.; Gilbert, R.E. Sodium-glucose linked cotransporter-2 inhibition does not attenuate disease progression in the rat remnant kidney model of chronic kidney disease. PLoS ONE 2016, 11, e0144640. [Google Scholar] [CrossRef]
- Rajasekeran, H.; Reich, H.N.; Hladunewich, M.A.; Cattran, D.; Lovshin, J.A.; Lytvyn, Y.; Bjornstad, P.; Lai, V.; Tse, J.; Cham, L.; et al. Dapagliflozin in focal segmental glomerulosclerosis: A combined human-rodent pilot study. Am. J. Physiol. Renal. Physiol. 2018, 314, F412–F422. [Google Scholar] [CrossRef]
- Wang, X.; Zhang, S.; Liu, Y.; Spichtig, D.; Kapoor, S.; Koepsell, H.; Mohebbi, N.; Segerer, S.; Serra, A.L.; Rodriguez, D.; et al. Targeting of sodium-glucose cotransporters with phlorizin inhibits polycystic kidney disease progression in Han:SPRD rats. Kidney Int. 2013, 84, 962–968. [Google Scholar] [CrossRef] [PubMed]
- Yamato, M.; Kato, N.; Kakino, A.; Yamada, K.; Inoguchi, T. Low dose of sodium-glucose transporter 2 inhibitor ipragliflozin attenuated renal dysfunction and interstitial fibrosis in adenine-induced chronic kidney disease in mice without diabetes. Metabol. Open 2020, 7, 100049. [Google Scholar] [CrossRef] [PubMed]
- Wan, N.; Fujisawa, Y.; Kobara, H.; Masaki, T.; Nakano, D.; Rahman, A.; Nishiyama, A. Effects of an SGLT2 inhibitor on the salt sensitivity of blood pressure and sympathetic nerve activity in a nondiabetic rat model of chronic kidney disease. Hypertens. Res. 2020, 43, 492–499. [Google Scholar] [CrossRef]
- Zhang, Y.; Nakano, D.; Guan, Y.; Hitomi, H.; Uemura, A.; Masaki, T.; Kobara, H.; Sugaya, T.; Nishiyama, A. A sodium-glucose cotransporter 2 inhibitor attenuates renal capillary injury and fibrosis by a vascular endothelial growth factor–dependent pathway after renal injury in mice. Kidney Int. 2018, 94, 524–535. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Konishi, Y.; Morikawa, T.; Zhang, Y.; Kitabayashi, C.; Kobara, H.; Masaki, T.; Nakano, D.; Hitomi, H.; Kobori, H.; et al. Effect of a SGLT2 inhibitor on the systemic and intrarenal renin–angiotensin system in subtotally nephrectomized rats. J. Pharmacol. Sci. 2018, 137, 220–223. [Google Scholar] [CrossRef] [PubMed]
- Abdelrahman, A.M.; Al Suleimani, Y.; Shalaby, A.; Ashique, M.; Manoj, P.; Nemmar, A.; Ali, B.H. Effect of canagliflozin, a sodium glucose co-transporter 2 inhibitor, on cisplatin-induced nephrotoxicity in mice. Naunyn-Schmiedeberg’s Arch. Pharmcol. 2019, 392, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Song, Z.; Zhu, J.; Wei, Q.; Dong, G.; Dong, Z. Canagliflozin reduces cisplatin uptake and activates Akt to protect against cisplatin-induced nephrotoxicity. Am. J. Physiol. Renal. Physiol. 2020, 318, F1041–F1052. [Google Scholar] [CrossRef]
- Ali, B.H.; Al Salam, S.; Al Suleimani, Y.; Al Za’abi, M.; Abdelrahman, A.M.; Ashique, M.; Manoj, P.; Adham, S.A.; Hartmann, C.; Schupp, N.; et al. Effects of the SGLT-2 inhibitor canagliflozin on adenine-induced chronic kidney disease in rats. Cell. Physiol. Biochem. 2019, 52, 27–39. [Google Scholar] [CrossRef] [PubMed]
- Hasan, R.; Lasker, S.; Hasan, A.; Zerin, F.; Zamila, M.; Parvez, F.; Rahman, M.M.; Khan, F.; Subhan, N.; Alam, M.A. Canagliflozin ameliorates renal oxidative stress and inflammation by stimulating AMPK-Akt-eNOS pathway in the isoprenaline-induced oxidative stress model. Sci. Rep. 2020, 10, 14659. [Google Scholar] [CrossRef] [PubMed]


| Experimental Models of Kidney Disease | SGLT2 Inhibitor | Renal Functional Parameters | Kidney Tissue | References |
|---|---|---|---|---|
| Angiotensin II-dependent hypertension (Sprague Dawley rats) | Empagliflozin | ↔ Glomerular filtration rate | ↓ fibrosis ↓ inflammatory cells ↓ type I, type IV collagen | [20] |
| Angiotensin II-dependent hypertension (Wistar rats) | Empagliflozin +AT1 antagonist | ↑ Glomerular filtration rate ↓ proteinuria | ↑ SGLT2, ↓ ROS | [21] |
| Hypertensive rats (fawn-hooded rats) | Empagliflozin | ↔ plasma creatinine ↔ plasma MCP-1 ↔ proteinuria | ↑ kidney weight ↔ oxidative stress | [22] |
| 2kidney-1clip hypertensive rats (Wistar rats) | Empagliflozin | ↔ plasma creatinine ↔ plasma MCP-1 ↑ proteinuria | ↔ kidney weight ↔ oxidative stress | [22] |
| Salt-sensitive hypertension in uninephrectomized (Hannover Sprague Dawley rats) | Empagliflozin | ↑ plasma MCP-1 ↔ proteinuria | ↑ kidney weight ↔ oxidative stress | [22] |
| Salt-sensitive hypertension in uninephrectomized (Sprague Dawley rats) | Empagliflozin | ↑ Glomerular filtration rate ↑ Proteinuria | ↑ HIF-1 ↓ inflammatory cells | [23] |
| Uninephrectomy-Doca-salt (different mouse strain) | Empagliflozin | ↔ Glomerular filtration rate ↔ albuminuria | ↔ fibrosis | [24] |
| Insulin resistance (Wistar rats) | Empagliflozin | ↔ serum creatinine ↔ serum BUN | ↓ fibrosis | [25] |
| Oxalate-induced nephropathy (C57BL/6N mice) | Empagliflozin | ↔ plasma creatinine ↔ plasma BUN ↔ Glomerular filtration rate | ↔ interstitial fibrosis | [26] |
| Cyclosporine nephropathy (Sprague Dawley rats) | Empagliflozin | ↑ Glomerular filtration rate | ↓ fibrosis ↓ inflammatory cells ↓ type I collagen ↓ type IV collagen | [27] |
| Unilateral ureteric obstruction (Wistar rats) | Empagliflozin | ↓ serum BUN ↓ serum creatinine | ↓ interstitial fibrosis ↓ inflammation ↓ tubular damage ↑ kloto expression | [28] |
| Subtotally nephrectomized rats (Wistar rats) | Empagliflozin | ↔ Glomerular filtration rate ↔ albuminuria | ↓ interstitial fibrosis ↓ glomerulosclerosis | [29] |
| Subtotally nephrectomized rats (Wistar rats) | Empagliflozin | ↓ serum creatinine ↓ serum BUN ↓ albuminuria | ↓ glomerulosclerosis ↓ interstitial fibrosis ↓ M2 macrophage polarization | [30] |
| Cardiorenal syndrome (Sprague Dawley rats) | Empagliflozin | ↓ plasma creatinine ↓ proteinuria | ↓ tubular damage ↓ Bowman’s capsule dilatation | [31] |
| Experimental Models of Kidney Disease | SGLT2 Inhibitor | Renal Functional Parameters | Kidney Tissue | References |
|---|---|---|---|---|
| Salt-sensitive hypertension (female Dahl SS rats) | Dapagliflozin | ↔ Glomerular filtration rate | ↓ fibrosis | [32] |
| Salt-sensitive hypertension (Dahl SS rats) | Dapagliflozin | ↓ albuminuria | ↓ fibrosis ↓ inflammation ↓ oxidative stress ↑ protective RAS signaling | [33] |
| Polycystic kidney disease (PKC rats) | Dapagliflozin | ↑ Glomerular filtration rate ↑ albuminuria | ↑ cyst volume | [34] |
| Polycystic kidney disease (Han:SPRD rats) | Dapagliflozin | ↑ Glomerular filtration rate ↓ albuminuria | ↔ cyst volume ↔ fibrosis ↔ inflammatory cells | [35] |
| Prediabetic rats (Wistar rats) | Dapagliflozin | ↓ Glomerular hyperfiltration ↓ albuminuria | ↓ fibrosis ↓ inflammation ↓ endoplasmatic reticulum stress ↓ apoptosis | [36] |
| High-fat/high-fructose-diet-induced insulin resistance (Wistar rats) | Dapagliflozin | ↓ serum creatinine | ↓ fibrosis ↓ inflammation ↓ oxidative stress ↓ apoptosis ↓ triglyceride accumulation | [37] |
| Gentamicin-induced nephrotoxicity (Wistar rats) | Dapagliflozin | ↓ serum creatinine ↓ serum BUN ↓ proteinuria | ↓ tubular and glomerular injury ↓ oxidative stress ↓ apoptosis | [38] |
| Protein overload- proteinuria (C57BL/6N mice) | Dapagliflozin | ↔ Glomerular filtration rate ↓ proteinuria | ↓ glomerular lesions ↓ inflammation | [39] |
| Adriamicin-induced nephropathy (balb/c mice) | Dapagliflozin | ↔ proteinuria | ↔ fibrosis ↔ inflammation ↔ tubular atrophy | [40] |
| Renal ischemia- reperfusion injury (C57BL/6 mice) | Dapagliflozin | ↓ serum creatinine ↓ serum BUN | ↓ tubulointerstitial lesions ↓ apoptosis ↑ HIF-1 expression | [41] |
| Subtotally nephrectomized rats (Sprague Dawley rats) | Dapagliflozin | ↔ Glomerular filtration rate ↔ proteinuria | ↔ glomerulosclerosis ↔ interstitial fibrosis ↔ inflammatory cells | [42] |
| Subtotally nephrectomized rats (Sprague Dawley rats) | Dapagliflozin | ↔ Glomerular filtration rate ↔ proteinuria | ↔ glomerulosclerosis ↔ inflammatory cells | [43] |
| Experimental Models of Kidney Disease | SGLT2 Inhibitor | Renal Functional Parameters | Kidney Tissue | References |
|---|---|---|---|---|
| Polycystic kidney disease (Han:SPRD rats) | Phlorizin | ↑ Glomerular filtration rate ↓ albuminuria | ↓ cyst volume | [44] |
| Adenine-induced chronic kidney disease (C57BL/6JJcl mice) | Ipragliflozin | ↓ plasma creatinine | ↓ fibrosis ↓ tubular dilatation ↓ oxidative stress | [45] |
| Adenine-induced chronic kidney disease (Wistar rats) | Luseogliflozin | ↔ serum BUN | ↔ tubular dilation | [46] |
| Renal ischemia- reperfusion injury (C57BL/6J mice) | Luseogliflozin | ↑ Glomerular filtration rate | ↓ interstitial fibrosis ↓ capillary rarefaction | [47] |
| Subtotally nephrectomized rats (Sprague Dawley rats) | TA-1887 | ↔ plasma creatinine ↔ plasma BUN ↔ Glomerular filtration rate ↔ albuminuria | ↔ interstitial fibrosis ↔ glomerular injury ↔ RAS | [48] |
| Experimental Models of Kidney Disease | SGLT2 Inhibitor | Renal Functional Parameters | Kidney Tissue | References |
|---|---|---|---|---|
| Cisplatin-induced nephrotoxicity (CD1 mice) | Canagliflozin | ↑ Glomerular filtration rate ↓ albuminuria | ↓ tubular and glomerular injury ↓ oxidative stress | [49] |
| Cisplatin-induced nephrotoxicity (C57BL/6 mice) | Canagliflozin | ↓ serum creatinine ↓ serum BUN | ↓ tubular injury ↓ apoptosis | [50] |
| Adenine-induced chronic kidney disease (Wistar rats) | Canagliflozin | ↓ plasma creatinine ↓ plasma BUN ↓ albuminuria | ↓ fibrosis ↓ inflammation ↓ oxidative stress | [51] |
| Isoprenaline-induced renal oxidative damage (Long Evans rats) | Canagliflozin | ↓ plasma creatinine | ↓ fibrosis ↓ inflammatory cells ↓ oxidative stress ↓ apoptosis | [52] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castoldi, G.; Carletti, R.; Barzaghi, F.; Meani, M.; Zatti, G.; Perseghin, G.; Di Gioia, C.R.T.; Zerbini, G. Sodium Glucose Cotransporter-2 Inhibitors in Non-Diabetic Kidney Disease: Evidence in Experimental Models. Pharmaceuticals 2024, 17, 362. https://doi.org/10.3390/ph17030362
Castoldi G, Carletti R, Barzaghi F, Meani M, Zatti G, Perseghin G, Di Gioia CRT, Zerbini G. Sodium Glucose Cotransporter-2 Inhibitors in Non-Diabetic Kidney Disease: Evidence in Experimental Models. Pharmaceuticals. 2024; 17(3):362. https://doi.org/10.3390/ph17030362
Chicago/Turabian StyleCastoldi, Giovanna, Raffaella Carletti, Francesca Barzaghi, Michela Meani, Giovanni Zatti, Gianluca Perseghin, Cira R. T. Di Gioia, and Gianpaolo Zerbini. 2024. "Sodium Glucose Cotransporter-2 Inhibitors in Non-Diabetic Kidney Disease: Evidence in Experimental Models" Pharmaceuticals 17, no. 3: 362. https://doi.org/10.3390/ph17030362
APA StyleCastoldi, G., Carletti, R., Barzaghi, F., Meani, M., Zatti, G., Perseghin, G., Di Gioia, C. R. T., & Zerbini, G. (2024). Sodium Glucose Cotransporter-2 Inhibitors in Non-Diabetic Kidney Disease: Evidence in Experimental Models. Pharmaceuticals, 17(3), 362. https://doi.org/10.3390/ph17030362





