Development of Scaffolds with Chitosan Magnetically Activated with Cobalt Nanoferrite: A Study on Physical-Chemical, Mechanical, Cytotoxic and Antimicrobial Behavior
Abstract
1. Introduction
2. Results and Discussion
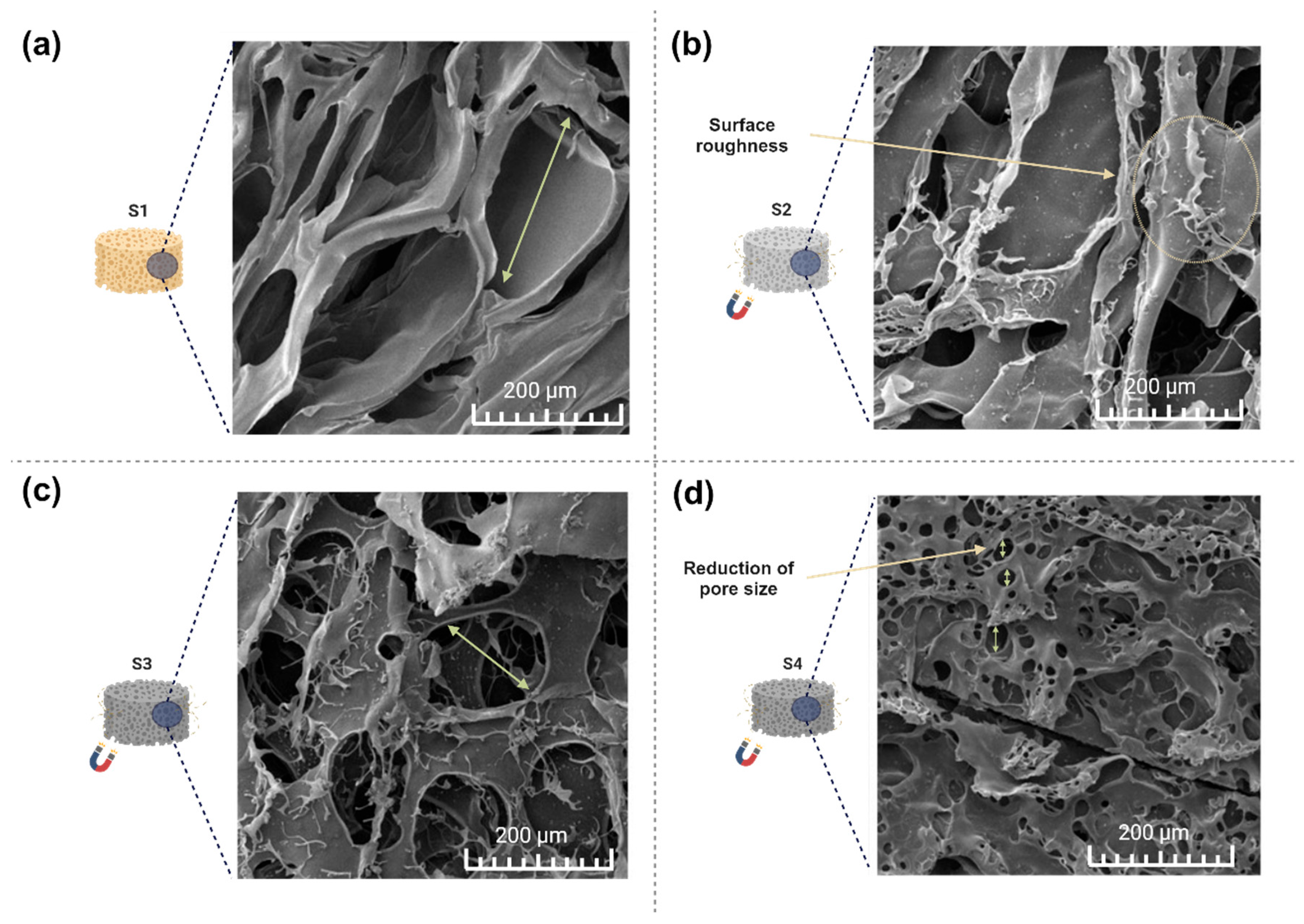
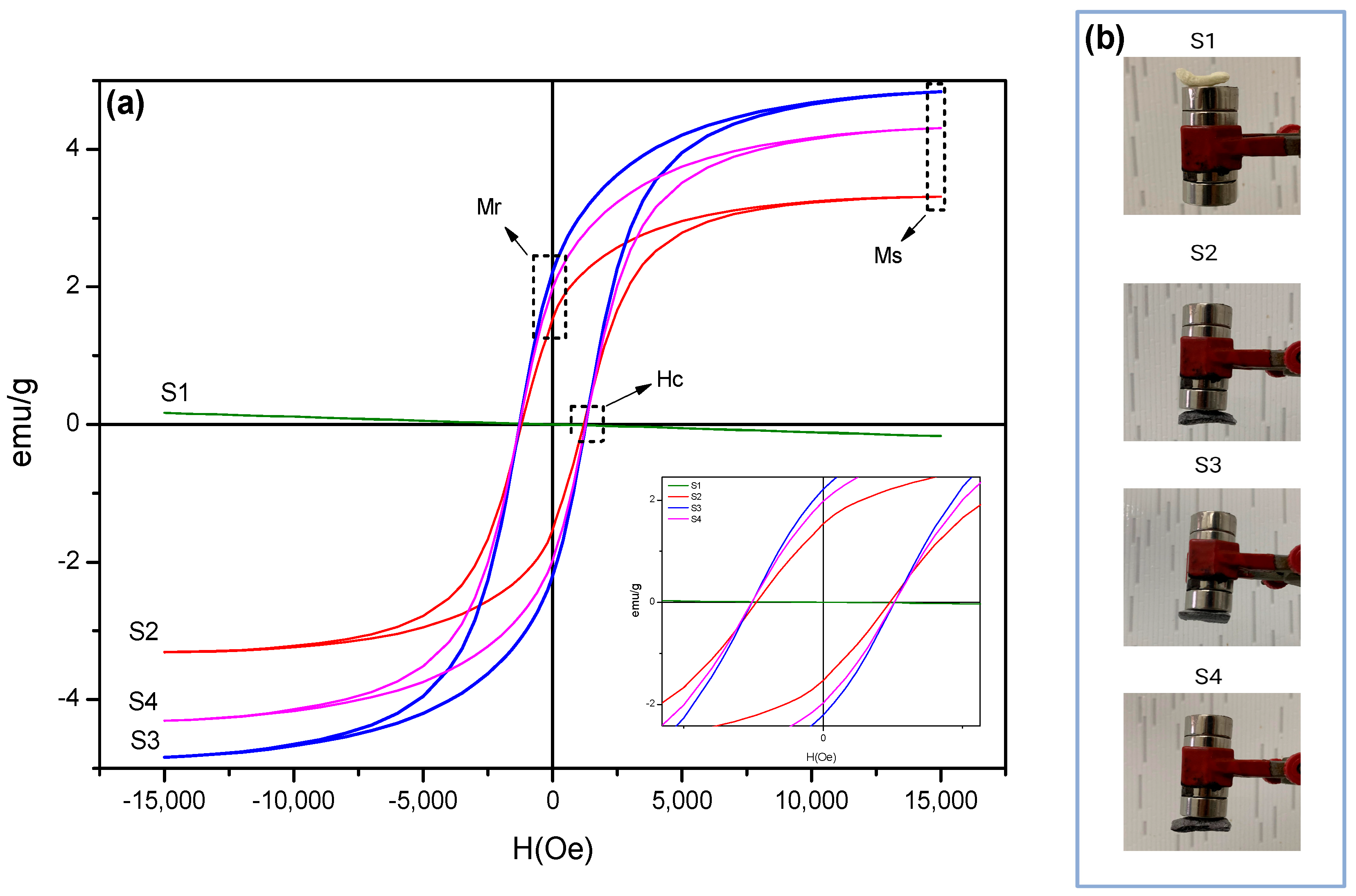
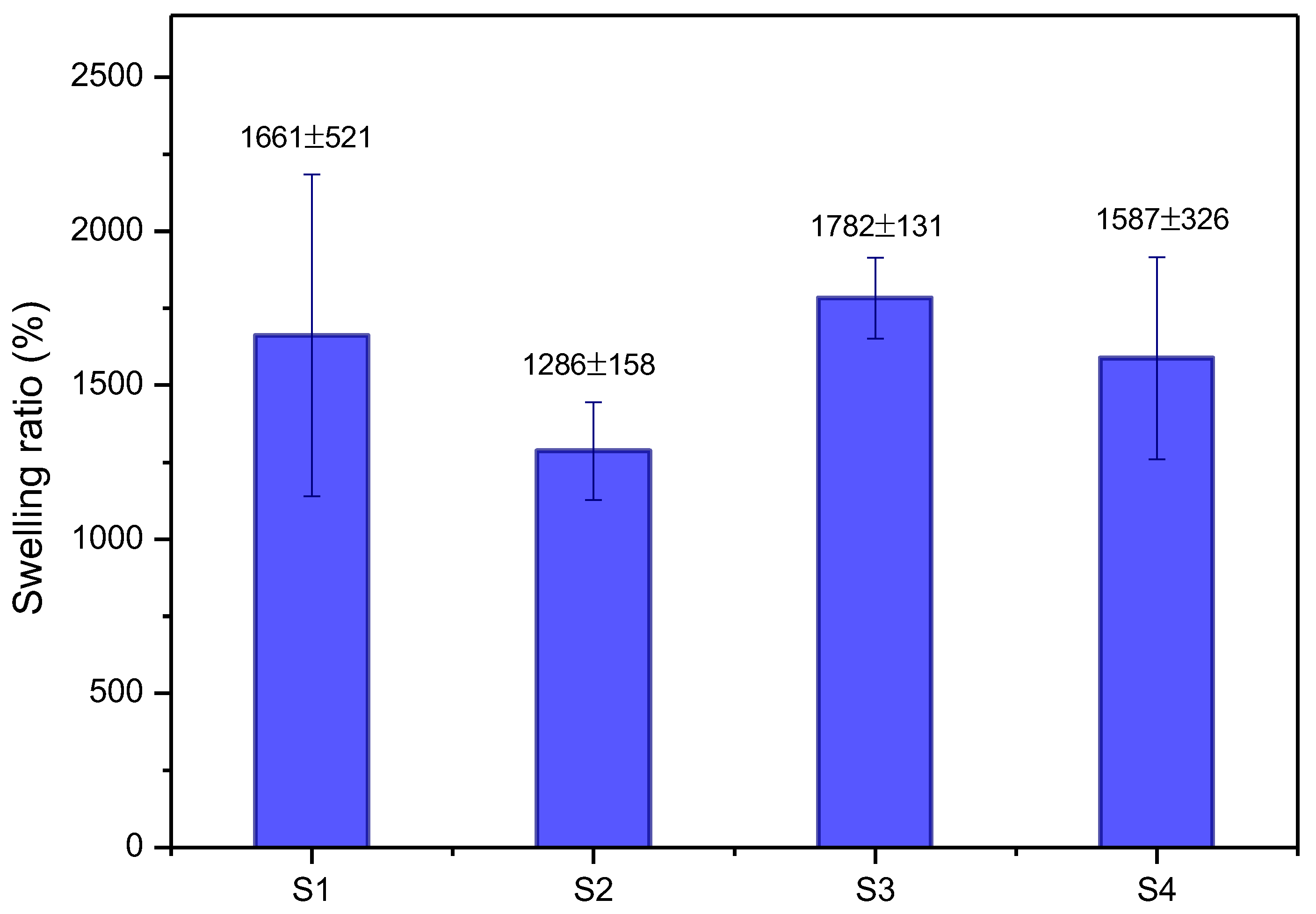
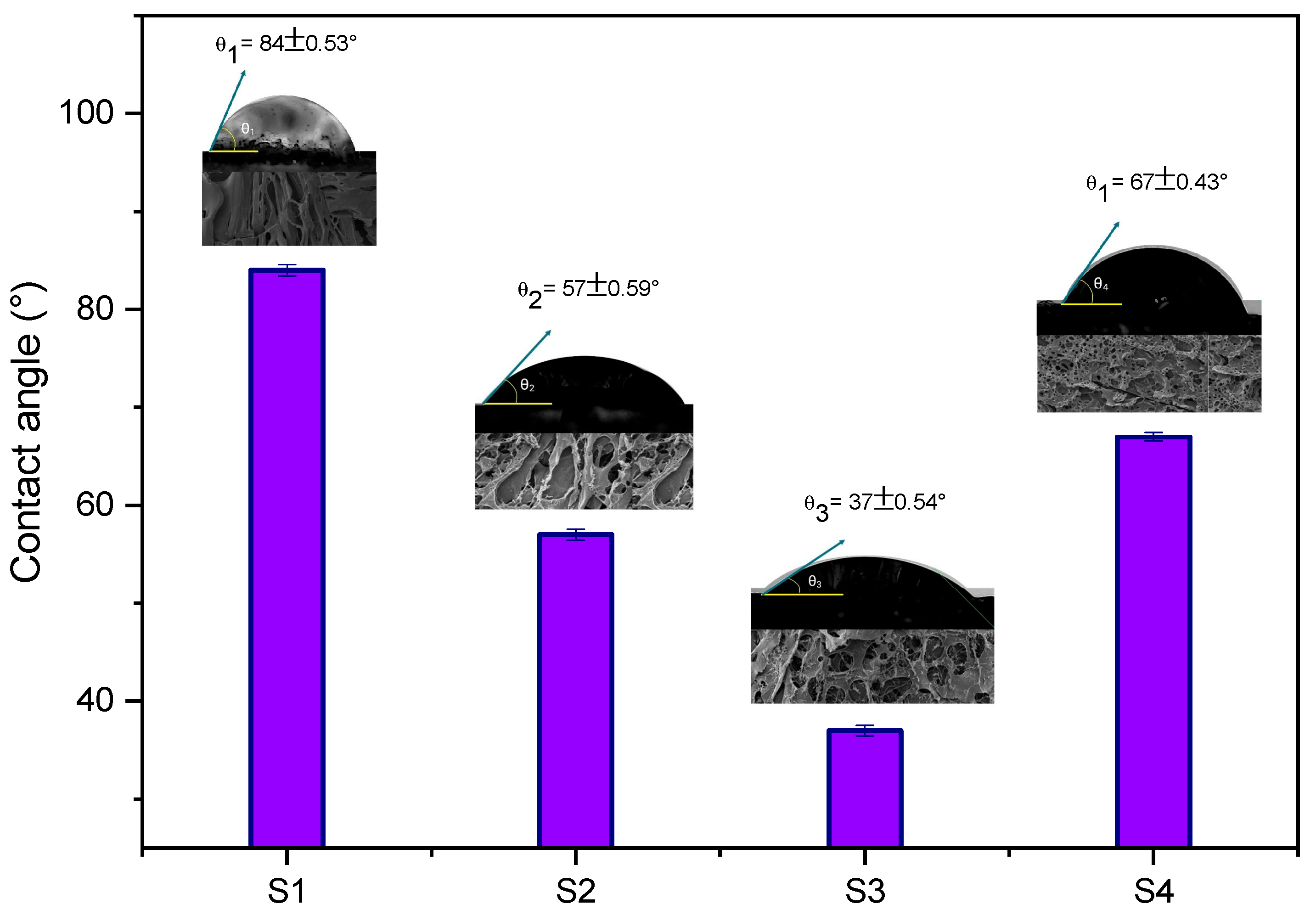
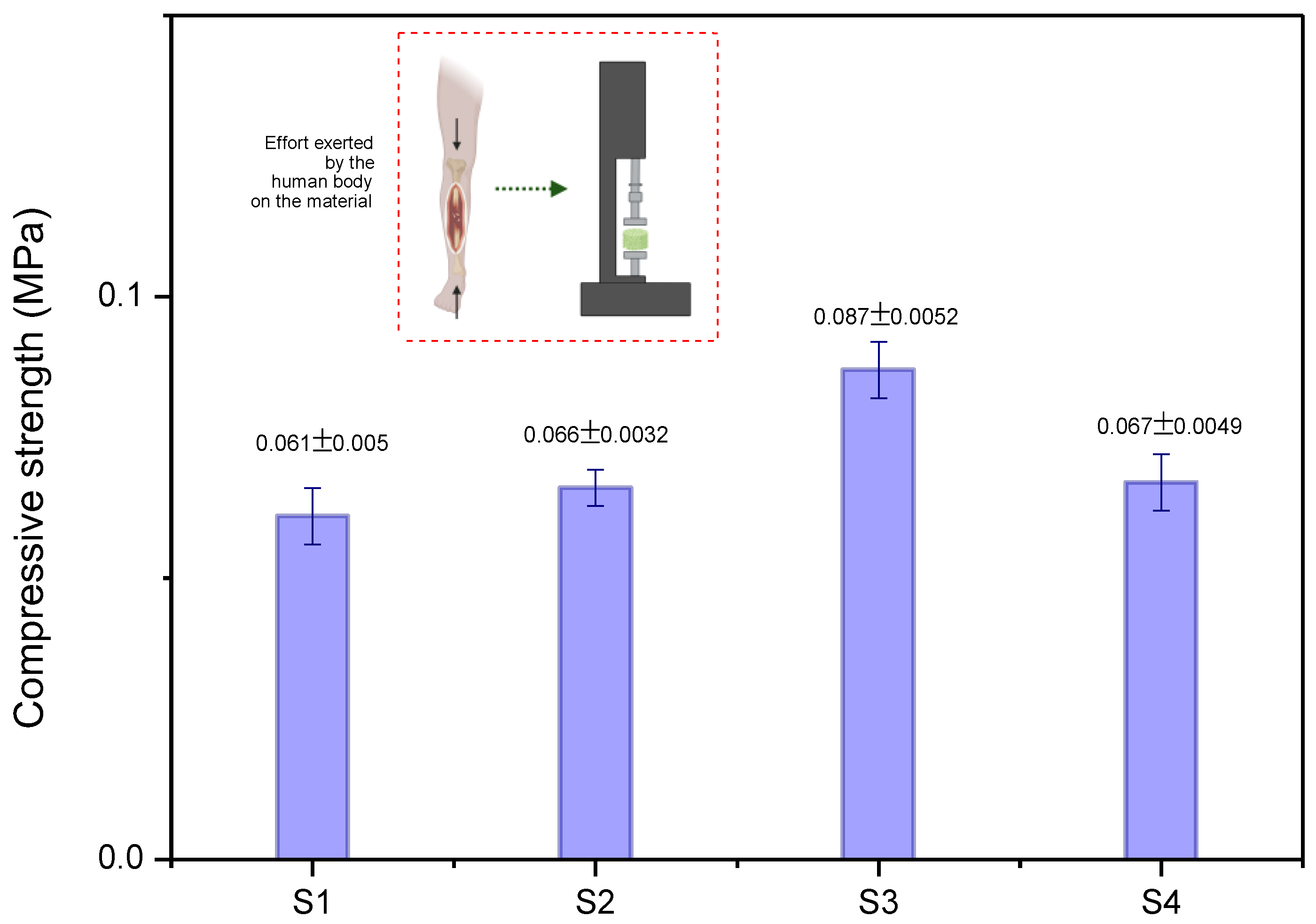
2.1. Physicochemical Results
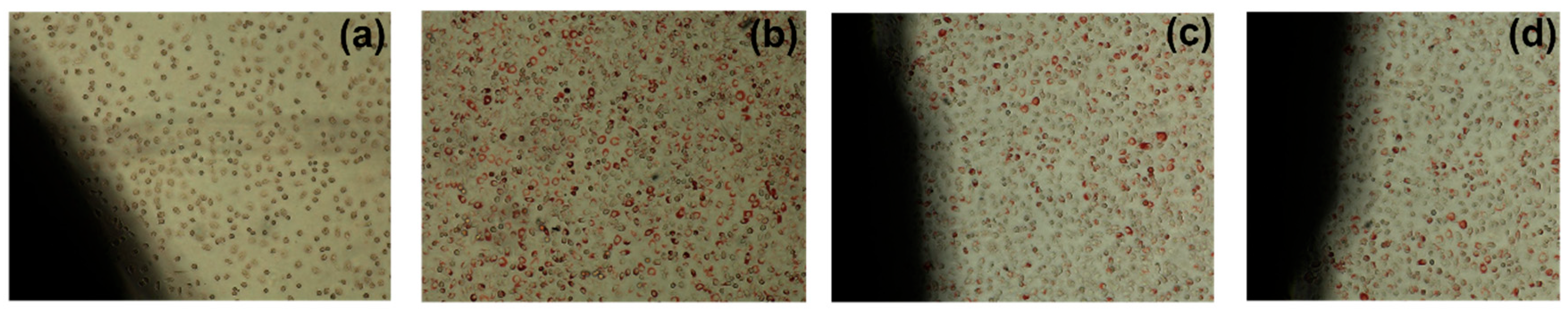
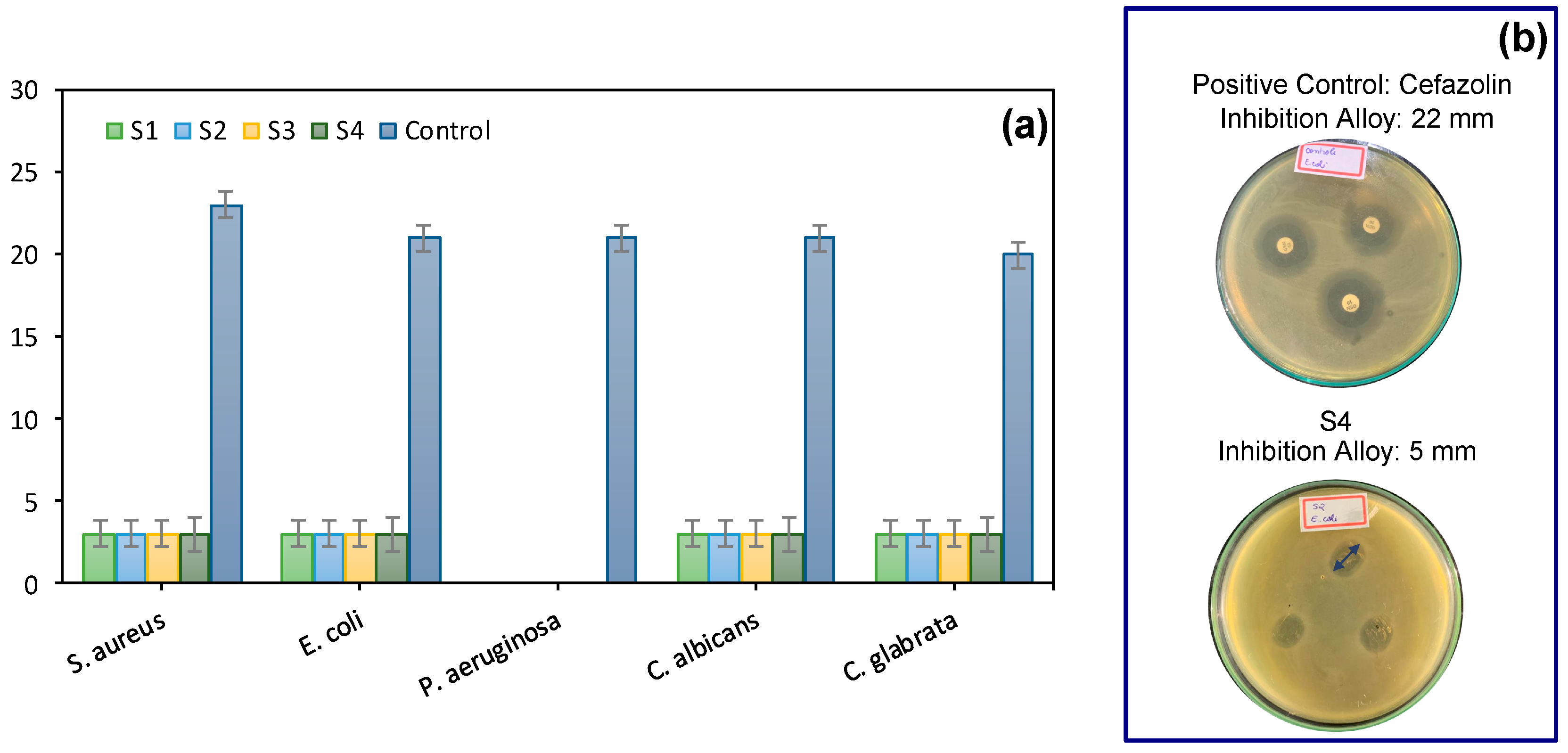
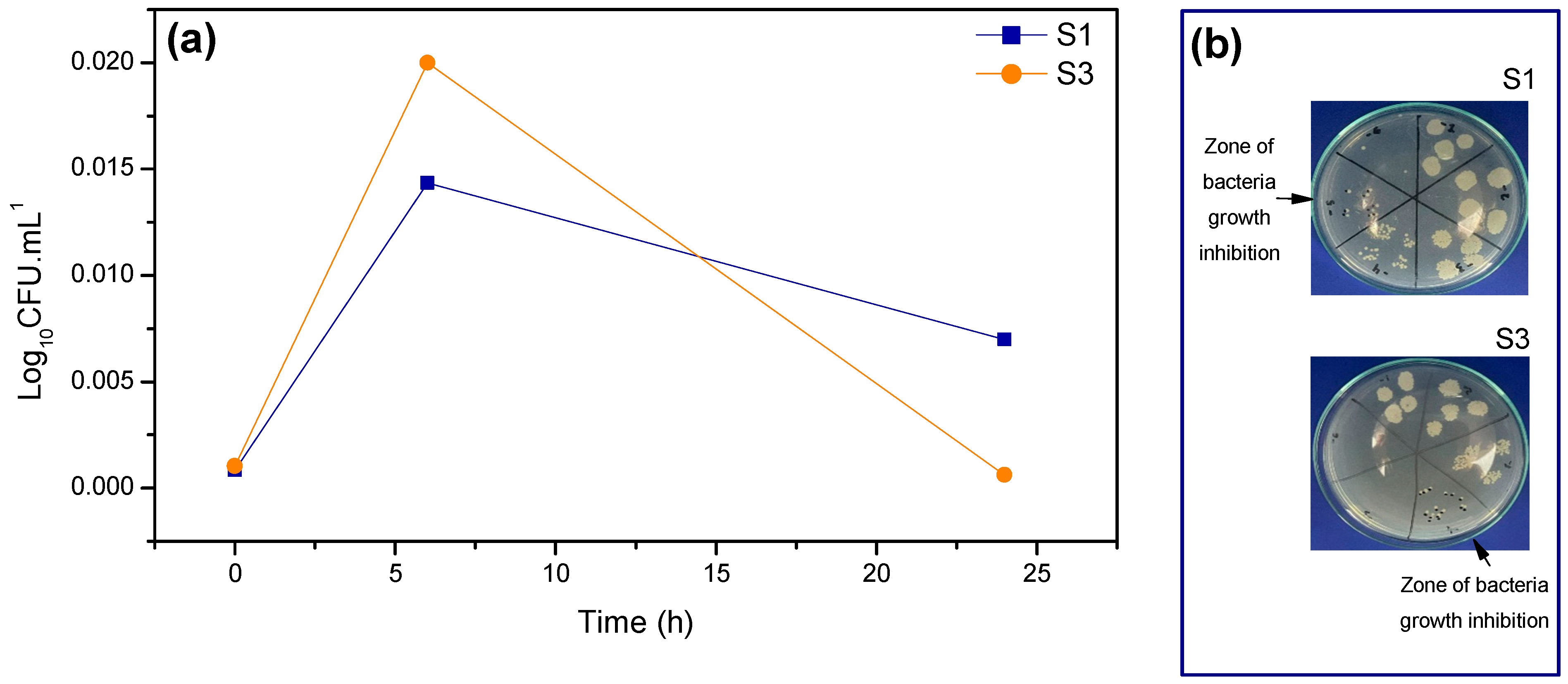
2.2. Biological Response
3. Experimental Section
3.1. Materials
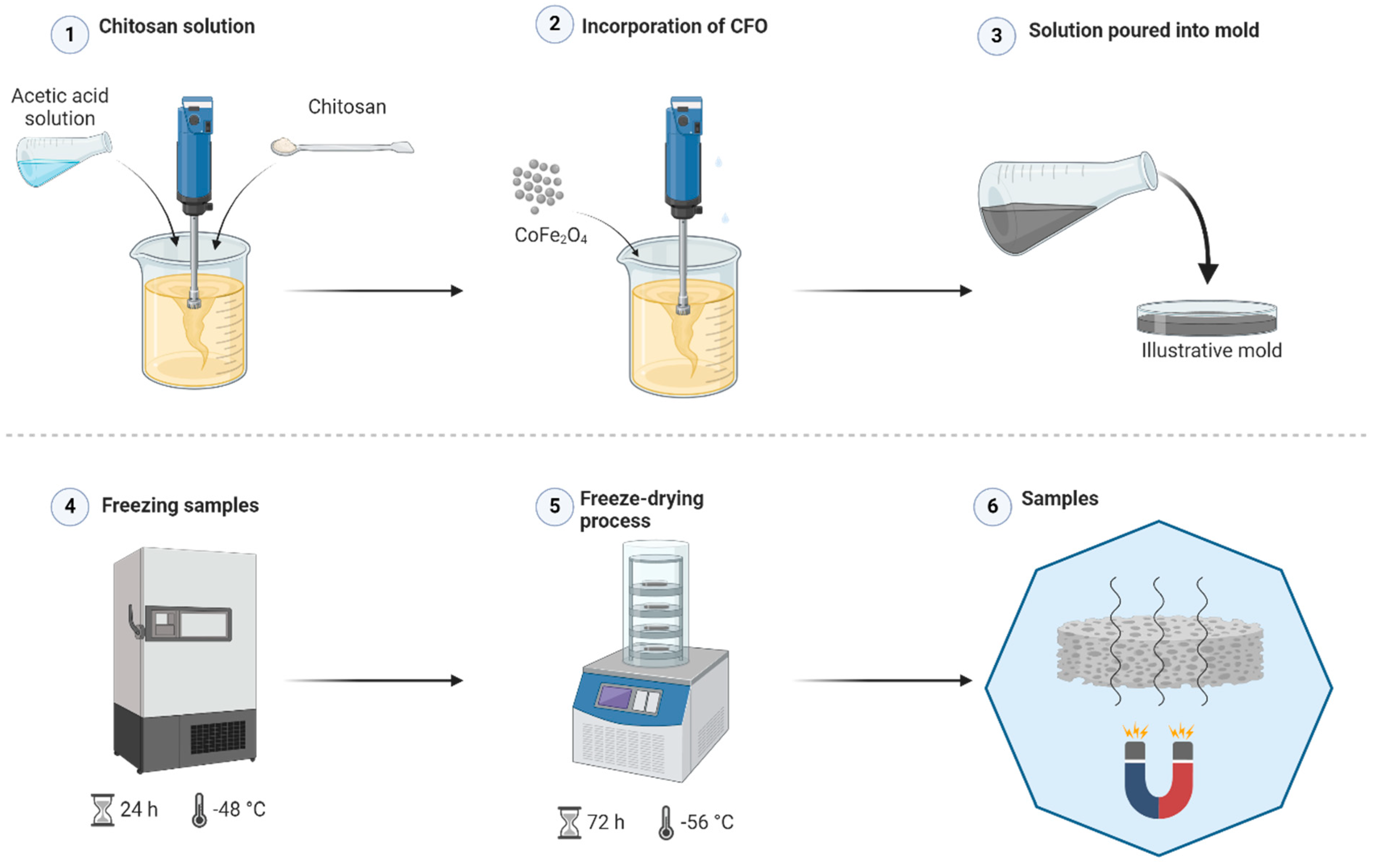
3.2. Methods
3.2.1. Synthesis of Cobalt Ferrite (CoFe2O4) via Combustion Reaction
3.2.2. Scaffolds Preparation
3.3. Physicochemical Characterization
3.4. Biological Analyses
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Percival, K.M.; Paul, V.; Husseini, G.A. Recent Advancements in Bone Tissue Engineering: Integrating Smart Scaffold Technologies and Bio-Responsive Systems for Enhanced Regeneration. Int. J. Mol. Sci. 2024, 25, 6012. [Google Scholar] [CrossRef] [PubMed]
- Zelinka, A.; Roelofs, A.J.; Kandel, R.A.; De Bari, C. Cellular therapy and tissue engineering for cartilage repair. Osteoarthr. Cartil. 2022, 30, 1547–1560. [Google Scholar] [CrossRef]
- Park, S.; Rahaman, K.A.; Kim, Y.C.; Jeon, H.; Han, H.S. Fostering tissue engineering and regenerative medicine to treat musculoskeletal disorders in bone and muscle. Bioact. Mater. 2024, 40, 345–365. [Google Scholar] [CrossRef]
- Ghosh, S.; Dhiman, M.; Gupta, S.; Roy, P.; Lahiri, D. Electro-conductive chitosan/graphene bio-nanocomposite Scaffold for tissue engineering of the central nervous system. Biomater. Adv. 2023, 154, 213596. [Google Scholar] [CrossRef]
- Sufiyan, M.; Kushwaha, P.; Ahmad, M.; Mandal, P.; Vishwakarma, K.K. Scaffold-Mediated Drug Delivery for Enhanced Wound Healing: A Review. Am. Assoc. Pharm. Sci. 2024, 25, 137. [Google Scholar] [CrossRef]
- Zhang, L.; Yang, G.; Johnson, B.N.; Jia, X. Three-dimensional (3D) printed Scaffold and material selection for bone repair. Acta Biomater. 2019, 84, 16–33. [Google Scholar] [CrossRef] [PubMed]
- De Witte, T.M.; Fratila-Apachitei, L.E.; Zadpoor, A.A.; Peppas, N.A. Bone tissue engineering via growth factor delivery: From Scaffoldsto complex matrices. Regen. Mater. 2018, 5, 197–211. [Google Scholar] [CrossRef] [PubMed]
- Maglio, M.; Sartori, M.; Gambardella, A.; Shelyakova, T.; Dediu, V.A.; Santin, M.; Piñeiro, Y.; López, M.B.; Rivas, J.; Tampieri, A.; et al. Bone Regeneration Guided by a Magnetized Scaffold in an Ovine Defect Model. Int. J. Mol. Sci. 2023, 24, 747. [Google Scholar] [CrossRef] [PubMed]
- Shruthi, P.A.; Pushpadass, H.A.; Franklin, M.E.E.; Battula, S.N.; Naik, N.L. Resveratrol-loaded proniosomes: Formulation, characterization and fortification. LWT 2020, 134, 110127. [Google Scholar] [CrossRef]
- Paltanea, G.; Manescu, V.; Antoniac, I.; Antoniac, A.; Nemoianu, I.V.; Robu, A.; Dura, H. A Review of Biomimetic and Biodegradable Magnetic Scaffoldsfor Bone Tissue Engineering and Oncology. Int. J. Mol. Sci. 2023, 24, 4312. [Google Scholar] [CrossRef]
- Li, Z.; Xue, L.; Wang, P.; Ren, X.; Zhang, Y.; Wang, C.; Sun, J. Biological ScaffoldsAssembled with Magnetic Nanoparticles for Bone Tissue Engineering: A Review. Materials 2023, 16, 1429. [Google Scholar] [CrossRef] [PubMed]
- Lukin, I.; Erezuma, I.; Desimone, M.F.; Zhang, Y.S.; Dolatshahi-Pirouz, A.; Orive, G. Nanomaterial-based drug delivery of immunomodulatory factors for bone and cartilage tissue engineering. Biomater. Adv. 2023, 154, 213637. [Google Scholar] [CrossRef]
- Bi, M.; Yang, K.; Yu, T.; Wu, G.; Li, Q. Cell-based mechanisms and strategies of co-culture system both in vivo and vitro for bone tissue engineering. Biomed. Pharmacother. 2023, 169, 115907. [Google Scholar] [CrossRef]
- Kudiyarasu, S.; Karuppan Perumal, M.K.; Rajan Renuka, R.; Manickam Natrajan, P. Chitosan composite with mesenchymal stem cells: Properties, mechanism, and its application in bone regeneration. Int. J. Biol. Macromol. 2024, 275, 133502. [Google Scholar] [CrossRef]
- Meshkini, A.; Sistanipour, E.; Izadi, A. Mg.ATP-decorated ultrafine magnetic nanofibers: A bone Scaffold with high osteogenic and antibacterial properties in the presence of an electromagnetic field. Colloids Surf. B Biointerfaces 2022, 210, 112256. [Google Scholar] [CrossRef]
- Harugade, A.; Sherje, A.P.; Pethe, A. Chitosan: A review on properties, biological activities and recent progress in biomedical applications. React. Funct. Polym. 2023, 191, 105634. [Google Scholar] [CrossRef]
- Wong, S.K.; Yee, M.M.F.; Chin, K.Y.; Ima-Nirwana, S. A Review of the Application of Natural and Synthetic Scaffoldsin Bone Regeneration. J. Funct. Biomater. 2023, 14, 286. [Google Scholar] [CrossRef] [PubMed]
- Valverde, T.M.; dos Santos, V.M.; Viana, P.I.; Costa, G.M.; de Goes, A.M.; Sousa, L.R.; Xavier, V.F.; Vieira, P.M.; de Lima Silva, D.; Domingues, R.Z.; et al. Novel Fe3O4 Nanoparticles with Bioactive Glass–Naproxen Coating: Synthesis, Characterization, and In Vitro Evaluation of Bioactivity. Int. J. Mol. Sci. 2024, 25, 4270. [Google Scholar] [CrossRef]
- Vasić, K.; Knez, Ž.; Leitgeb, M. Multifunctional Iron Oxide Nanoparticles as Promising Magnetic Biomaterials in Drug Delivery: A Review. J. Funct. Biomater. 2024, 15, 227. [Google Scholar] [CrossRef]
- Babakhani, A.; Peighambardoust, S.J.; Olad, A. Fabrication of magnetic nanocomposite Scaffoldsbased on polyvinyl alcohol-chitosan containing hydroxyapatite and clay modified with graphene oxide: Evaluation of their properties for bone tissue engineering applications. J. Mech. Behav. Biomed. Mater. 2024, 150, 106263. [Google Scholar] [CrossRef]
- Azadani, R.N.; Karbasi, S.; Poursamar, A. Chitosan/MWCNTs nanocomposite coating on 3D printed Scaffold of poly 3-hydroxybutyrate/magnetic mesoporous bioactive glass: A new approach for bone regeneration. Int. J. Biol. Macromol. 2024, 260, 129407. [Google Scholar] [CrossRef] [PubMed]
- Nag, S.; Mohanto, S.; Ahmed, M.G.; Subramaniyan, V. “Smart” stimuli-responsive biomaterials revolutionizing the theranostic landscape of inflammatory arthritis. Mater. Today Chem. 2024, 39, 102178. [Google Scholar] [CrossRef]
- Xu, Z.; Zhang, Y.; Zheng, L.; Cai, H.; Yang, X.; Xue, Y.; Wan, Q.; Chen, J.; Li, Y. Magnetic Scaffold constructing by micro-injection for bone tissue engineering under static magnetic field. J. Mater. Res. Technol. 2024, 29, 3554–3565. [Google Scholar] [CrossRef]
- Salmanpour, Z.; Abolmaali, S.S.; Farahavar, G.; Salmanpour, M.; Tamaddon, A.M. Magnetic nanoparticles and their hybrid biomaterials for drug delivery and theranostic applications in cardiovascular diseases. J. Drug Deliv. Sci. Technol. 2024, 96, 105676. [Google Scholar] [CrossRef]
- Laurent, S.; Forge, D.; Port, M.; Roch, A.; Robic, C.; Vander Elst, L.; Muller, R.N. Magnetic Iron Oxide Nanoparticles: Synthesis, Stabilization, Vectorization, Physicochemical Characterizations, and Biological Applications. Chem. Rev. 2008, 108, 2064–2110. [Google Scholar] [CrossRef]
- Barani, M.; Rahdar, A.; Mukhtar, M.; Razzaq, S.; Qindeel, M.; Hosseini Olam, S.A.; Paiva-Santos, A.C.; Ajalli, N.; Sargazi, S.; Balakrishnan, D.; et al. Recent application of cobalt ferrite nanoparticles as a theranostic agent. Mater. Today Chem. 2022, 26, 101131. [Google Scholar] [CrossRef]
- Gupta, A.; Anjali; Sahni, M. Structural and magnetic properties of cobalt ferrite nano-particles. Mater. Today Proc. 2023, 322, 3470–3475. [Google Scholar] [CrossRef]
- Leal, E.; Dantas, J.; Santos, P.T.A.D.; Bicalho, S.M.D.C.M.; Kiminami, R.H.G.A.; da Silva, M.R.; Costa, A.C.F.D.M. Effect of the surface treatment on the structural, morphological, magnetic and biological properties of MFe2O4 iron spinels (M = Cu, Ni, Co, Mn and Fe). Appl. Surf. Sci. 2018, 455, 635–645. [Google Scholar] [CrossRef]
- Cintra, C.C.V.; Ferreira-Ermita, D.A.C.; Loures, F.H.; Araújo, P.; Ribeiro, I.M.; Araújo, F.R.; Valente, F.L.; Reis, E.C.C.; Costa, A.; Bicalho, S.; et al. In vitro characterization of hydroxyapatite and cobalt ferrite nanoparticles compounds and their biocompatibility in vivo. J. Mater. Sci. Mater. Med. 2022, 33, 21. [Google Scholar] [CrossRef]
- Leal, E.; Basílio, S.T.; Dantas, J.; Richa, P.; Lima, R.d.C.; Kiminami, R.H.G.A.; Costa, A.C.F.d.M. Structural, textural, morphological, magnetic and electromagnetic study of Cu-doped NiZn ferrite synthesized by pilot-scale combustion for RAM application. Arab. J. Chem. 2020, 13, 8100–8118. [Google Scholar] [CrossRef]
- Bigham, A.; Aghajanian, A.H.; Saudi, A.; Rafienia, M. Hierarchical porous Mg2SiO4-CoFe2O4 nanomagnetic Scaffold for bone cancer therapy and regeneration: Surface modification and in vitro studies. Mater. Sci. Eng. C 2020, 109, 110579. [Google Scholar] [CrossRef] [PubMed]
- Vinayak, M.N.; Jana, S.; Datta, P.; Das, H.; Chakraborty, B.; Mukherjee, P.; Mondal, S.; Kundu, B.; Nandi, S.K. Accelerating full-thickness skin wound healing using Zinc and Cobalt doped-bioactive glass-coated eggshell membrane. J. Drug Deliv. Sci. Technol. 2023, 81, 104273. [Google Scholar] [CrossRef]
- Baino, F.; Montazerian, M.; Verné, E. Cobalt-Doped Bioactive Glasses for Biomedical Applications: A Review. Materials 2023, 16, 4994. [Google Scholar] [CrossRef]
- Liu, L.; Huang, R.; Zhang, L. Cobalt Element Doping for Biomedical Use: A Review. Mater. Sci. Forum 2020, 993, 811–819. [Google Scholar] [CrossRef]
- Guedes, D.G.; Cunha, M.E.; Gomes Araújo, R.; Silva, A.L.d.; Guedes de Lima, M.; Gondim Nepomuceno, F.; Figueiredo de Melo Costa, A.C. Scaffoldsmagnéticos de quitosana e/ou hidroxiapatita para regeneração de tecido ósseo: Uma revisão sistemática. Materials 2023, 4, e432936. [Google Scholar] [CrossRef]
- Anila, I.; Lahiri, B.B.; John, S.P.; Jacob Mathew, M.; Philip, J. Preparation, physicochemical characterization, and AC induction heating properties of colloidal aggregates of ferrimagnetic cobalt ferrite nanoparticles coated with a bio-compatible polymer. Ceram. Int. 2023, 49, 15183–15199. [Google Scholar] [CrossRef]
- Zhang, Y.; Yan, T.; Yan, L.; Guo, X.; Cui, L.; Wei, Q.; Du, B. Preparation of novel cobalt ferrite/chitosan grafted with graphene composite as effective adsorbents for mercury ions. J. Mol. Liq. 2014, 198, 381–387. [Google Scholar] [CrossRef]
- Han, X.; Zheng, Z.; Yu, C.; Deng, Y.; Ye, Q.; Niu, F.; Chen, Q.; Pan, W.; Wang, Y. Preparation, characterization and antibacterial activity of new ionized chitosan. Carbohydr. Polym. 2022, 290, 119490. [Google Scholar] [CrossRef]
- Dhar, D.; Ghosh, S.; Mukherjee, S.; Dhara, S.; Chatterjee, J.; Das, S. Assessment of chitosan-coated zinc cobalt ferrite nanoparticle as a multifunctional theranostic platform facilitating pH-sensitive drug delivery and OCT image contrast enhancement. Int. J. Pharm. 2024, 654, 123999. [Google Scholar] [CrossRef]
- Zhou, K.; Azaman, F.A.; Cao, Z.; Brennan Fournet, M.; Devine, D.M. Bone Tissue Engineering Scaffold Optimisation through Modification of Chitosan/Ceramic Composition. Macromol 2023, 3, 326–342. [Google Scholar] [CrossRef]
- Tavares, F.J.T.M.; Soares, P.I.P.; Silva, J.C.; Borges, J.P. Preparation and In Vitro Characterization of Magnetic CS/PVA/HA/pSPIONs Scaffoldsfor Magnetic Hyperthermia and Bone Regeneration. Int. J. Mol. Sci. 2023, 24, 1128. [Google Scholar] [CrossRef] [PubMed]
- Farzaneh, S.; Hosseinzadeh, S.; Samanipour, R.; Hatamie, S.; Ranjbari, J.; Khojasteh, A. Fabrication and characterization of cobalt ferrite magnetic hydrogel combined with static magnetic field as a potential bio-composite for bone tissue engineering. J. Drug Deliv. Sci. Technol. 2021, 64, 102525. [Google Scholar] [CrossRef]
- Maia, F.R.; Bastos, A.R.; Oliveira, J.M.; Correlo, V.M.; Reis, R.L. Recent approaches towards bone tissue engineering. Bone 2022, 154, 116256. [Google Scholar] [CrossRef]
- Yadav, P.; Beniwal, G.; Saxena, K.K. A review on pore and porosity in tissue engineering. Mater. Today Proc. 2021, 44, 2623–2628. [Google Scholar] [CrossRef]
- Francis, A.P.; Augustus, A.R.; Chandramohan, S.; Bhat, S.A.; Priya, V.V.; Rajagopalan, R. A review on biomaterials-based Scaffold: An emerging tool for bone tissue engineering. Mater. Today Commun. 2023, 34, 105124. [Google Scholar] [CrossRef]
- Baykara, D.; Pilavci, E.; Ulag, S.; Valentine Okoro, O.; Nie, L.; Shavandi, A.; Ceren Koyuncu, A.; Bingol Ozakpinar, O.; Eroglu, M.; Gunduz, O. In vitro electrically controlled amoxicillin release from 3D-printed chitosan/bismuth ferrite Scaffolds. Eur. Polym. J. 2023, 193, 112105. [Google Scholar] [CrossRef]
- Ge, Y.-W.; Fan, Z.-H.; Ke, Q.-F.; Guo, Y.-P.; Zhang, C.-Q.; Jia, W.-T. SrFe12O19-doped nano-layered double hydroxide/chitosan layered Scaffoldswith a nacre-mimetic architecture guide in situ bone ingrowth and regulate bone homeostasis. Mater. Today Bio 2022, 16, 100362. [Google Scholar] [CrossRef]
- Reizabal, A.; Brito-Pereira, R.; Fernandes, M.M.; Castro, N.; Correia, V.; Ribeiro, C.; Costa, C.M.; Perez, L.; Vilas, J.L.; Lanceros-Méndez, S. Silk fibroin magnetoactive nanocomposite films and membranes for dynamic bone tissue engineering strategies. Materialia 2020, 12, 100709. [Google Scholar] [CrossRef]
- Shuai, C.; Cheng, Y.; Yang, W.; Feng, P.; Yang, Y.; He, C.; Qi, F.; Peng, S. Magnetically actuated bone Scaffold: Microstructure, cell response and osteogenesis. Compos. Part B Eng. 2020, 192, 107986. [Google Scholar] [CrossRef]
- Radulescu, D.-M.; Neacsu, I.A.; Grumezescu, A.-M.; Andronescu, E. New Insights of ScaffoldsBased on Hydrogels in Tissue Engineering. Polymers 2022, 14, 799. [Google Scholar] [CrossRef]
- Öfkeli, F.; Demir, D.; Bölgen, N. Biomimetic mineralization of chitosan/gelatin cryogels and in vivo biocompatibility assessments for bone tissue engineering. J. Appl. Polym. Sci. 2021, 138, 50337. [Google Scholar] [CrossRef]
- Kiumarsi, N.; Najmoddin, N. Systematically engineered GO with magnetic CuFe2O4 to enhance bone regeneration on 3D printed PCL Scaffold. Surf. Interfaces 2023, 39, 102973. [Google Scholar] [CrossRef]
- Mahmoodiyan Najafabadi, F.; Karbasi, S.; Benisi, S.Z.; Shojaei, S.; Poursamar, S.A.; Nasr Azadani, R. Evaluation of the effects of alumina nanowire on 3D printed polycaprolactone / magnetic mesoporous bioactive glass Scaffold for bone tissue engineering applications. Mater. Chem. Phys. 2023, 303, 127616. [Google Scholar] [CrossRef]
- Yan, Z.; Sun, T.; Tan, W.; Wang, Z.; Yan, J.; Miao, J.; Wu, X.; Feng, P.; Deng, Y. Magnetic Field Boosts the Transmembrane Transport Efficiency of Magnesium Ions from PLLA Bone Scaffold. Small 2023, 19, 2301426. [Google Scholar] [CrossRef]
- Chakachaka, V.M.; Tshangana, C.S.; Mahlangu, O.T.; Mamba, B.B.; Muleja, A.A. Remediation of a non-steroidal anti-inflammatory drug from aqueous solutions using cobalt ferrite-photocatalytic membranes. Catal. Commun. 2024, 187, 106855. [Google Scholar] [CrossRef]
- Hadela, A.; Lakić, M.; Potočnik, M.; Košak, A.; Gutmaher, A.; Lobnik, A. Novel reusable functionalized magnetic cobalt ferrite nanoparticles as oil adsorbents. Adsorpt. Sci. Technol. 2020, 38, 168–190. [Google Scholar] [CrossRef]
- Chen, Y.; Etxabide, A.; Seyfoddin, A.; Ramezani, M. Fabrication and characterisation of poly(vinyl alcohol)/chitosan Scaffoldsfor tissue engineering applications. Mater. Today Proc. 2023. [Google Scholar] [CrossRef]
- Liu, D.; Nie, W.; Li, D.; Wang, W.; Zheng, L.; Zhang, J.; Zhang, J.; Peng, C.; Mo, X.; He, C. 3D printed PCL/SrHA Scaffold for enhanced bone regeneration. Chem. Eng. J. 2019, 362, 269–279. [Google Scholar] [CrossRef]
- Azueta-Aguayo, P.H.; Chuc-Gamboa, M.G.; Aguilar-Pérez, F.J.; Aguilar-Ayala, F.J.; Rodas-Junco, B.A.; Vargas-Coronado, R.F.; Cauich-Rodríguez, J.V. Effects of Neutralization on the Physicochemical, Mechanical, and Biological Properties of Ammonium-Hydroxide-Crosslinked Chitosan Scaffolds. Int. J. Mol. Sci. 2022, 23, 14822. [Google Scholar] [CrossRef]
- Tesfamariam, B. Bioresorbable vascular Scaffolds: Biodegradation, drug delivery and vascular remodeling. Pharmacol. Res. 2016, 107, 163–171. [Google Scholar] [CrossRef]
- Anila, I.; Mathew, M.J. Study on the physico-chemical properties, magnetic phase resolution and cytotoxicity behavior of chitosan-coated cobalt ferrite nanocubes. Appl. Surf. Sci. 2021, 556, 149791. [Google Scholar] [CrossRef]
- Miri, A.; Sarani, M.; Najafidoust, A.; Mehrabani, M.; Zadeh, F.A.; Varma, R.S. Photocatalytic performance and cytotoxic activity of green-synthesized cobalt ferrite nanoparticles. Mater. Res. Bull. 2022, 149, 111706. [Google Scholar] [CrossRef]
- Rao, J.; Chen, B.; McClements, D.J. Improving the Efficacy of Essential Oils as Antimicrobials in Foods: Mechanisms of Action. Annu. Rev. Food Sci. Technol. 2019, 10, 365–387. [Google Scholar] [CrossRef]
- Anand, S.; Rajinikanth, P.S.; Arya, D.K.; Pandey, P.; Gupta, R.K.; Sankhwar, R.; Chidambaram, K. Multifunctional Biomimetic Nanofibrous Scaffold Loaded with Asiaticoside for Rapid Diabetic Wound Healing. Pharmaceutics 2022, 14, 273. [Google Scholar] [CrossRef]
- Gole, D.; Kapatkar, S.; Mathad, S.; Chavan, R. In vitro antimicrobial activity of cobalt ferrite nanoparticles synthesized by Co-precipitation method. Acta Chem. Iasi 2020, 28, 225–236. [Google Scholar] [CrossRef]
- Gingasu, D.; Mindru, I.; Patron, L.; Ianculescu, A.; Vasile, E.; Marinescu, G.; Preda, S.; Diamandescu, L.; Oprea, O.; Popa, M.; et al. Synthesis and Characterization of Chitosan-Coated Cobalt Ferrite Nanoparticles and Their Antimicrobial Activity. J. Inorg. Organomet. Polym. Mater. 2018, 28, 1932–1941. [Google Scholar] [CrossRef]
- El-Shahawy, A.A.G.; Abo El-Ela, F.I.; Mohamed, N.A.; Eldine, Z.E.; El Rouby, W.M.A. Synthesis and evaluation of layered double hydroxide/doxycycline and cobalt ferrite/chitosan nanohybrid efficacy on gram positive and gram negative bacteria. Mater. Sci. Eng. C 2018, 91, 361–371. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Adiga, K.; Verneker, V.P. A new approach to thermochemical calculations of condensed fuel-oxidizer mixtures. Combust. Flame 1981, 40, 71–79. [Google Scholar] [CrossRef]
- Guedes, D.G.; Costa, A.C.F.d.M.; Barbosa, R.C.; Fook, M.V.L.; Silva, A.L.; Vasconcelos, H.P. Scaffold de Quitosana Ativado Magneticamente com Partículas de Ferrita de Cobalto Sintetizadas por Reação de Combustão para Engenharia de Tecidos. BR 10 2023 009515 1, 2023. Filed with INPI. [Google Scholar]
- Klug, H.P.; Alexander, L.E. X-ray diffraction procedures: For polycrystalline and amorphous materials. Am. Chem. Soc. 1974, 77, 2030–2031. [Google Scholar]
- ISO:10993-5; Biological Evaluation of Medical Devices. Part 5: Tests for In Vitro Cytotoxicity. International Organization for Standardization: Geneva, Switzerland, 2009.
- Fernandes, F.H.A.; Salgado, H.R.N. Antimicrobial Activity of Spondias dulcis Parkinson Extract Leaves Using Microdilution and Agar Diffusion: A Comparative Study. EC Microbiol. 2019, 14, 259–262. [Google Scholar]
- CLSI. Methods for Determining Bactericidal Activity of Antimicrobial Agents. In Time Kill Method; Clinical and Laboratory Standard Institute CLSI: Wayne, PA, USA, 2010; Volume CLSI document M100-S19, p. 32. [Google Scholar]
- Esentürk-Güzel, İ.; Durgun, M.E.; Özsoy, Y.; Güngör, S. Drug Release, Susceptibility and Time-Kill Assays to Develop Novel Anti-Infective Drugs. In Encyclopedia of Infection and Immunity; Rezaei, N., Ed.; Elsevier: Oxford, UK, 2022; pp. 640–651. [Google Scholar] [CrossRef]
- Pankey, G.A.; Ashcraft, D.S. In vitro antibacterial activity of tigecycline against resistant Gram-negative bacilli and enterococci by time–kill assay. Diagn. Microbiol. Infect. Dis. 2009, 64, 300–304. [Google Scholar] [CrossRef]
- Pauw, E.; Eloff, J.N. Which tree orders in southern Africa have the highest antimicrobial activity and selectivity against bacterial and fungal pathogens of animals? BMC Complement. Altern. Med. 2014, 14, 317. [Google Scholar] [CrossRef] [PubMed]
- CLSI. Methods for Dilution Antimicrobial Susceptibiçity Tests for Bacteria That Grow Aerobically; CLSI: Wayne, PA, USA, 2018. [Google Scholar]
- Obiang, C.S.; Misso, R.L.N.M.; Atome, G.R.N.; Obame, R.B.M.; Ondo, J.P.; Engonga, L.C.O.; Emvo, E.N. Antimicrobial, antioxidant, anti-inflammatory and cytotoxic study of extracts of Guibourtia tessmanii (harms) J. Léonard from Gabon. Clin. Phytosci. 2021, 7, 45. [Google Scholar] [CrossRef]
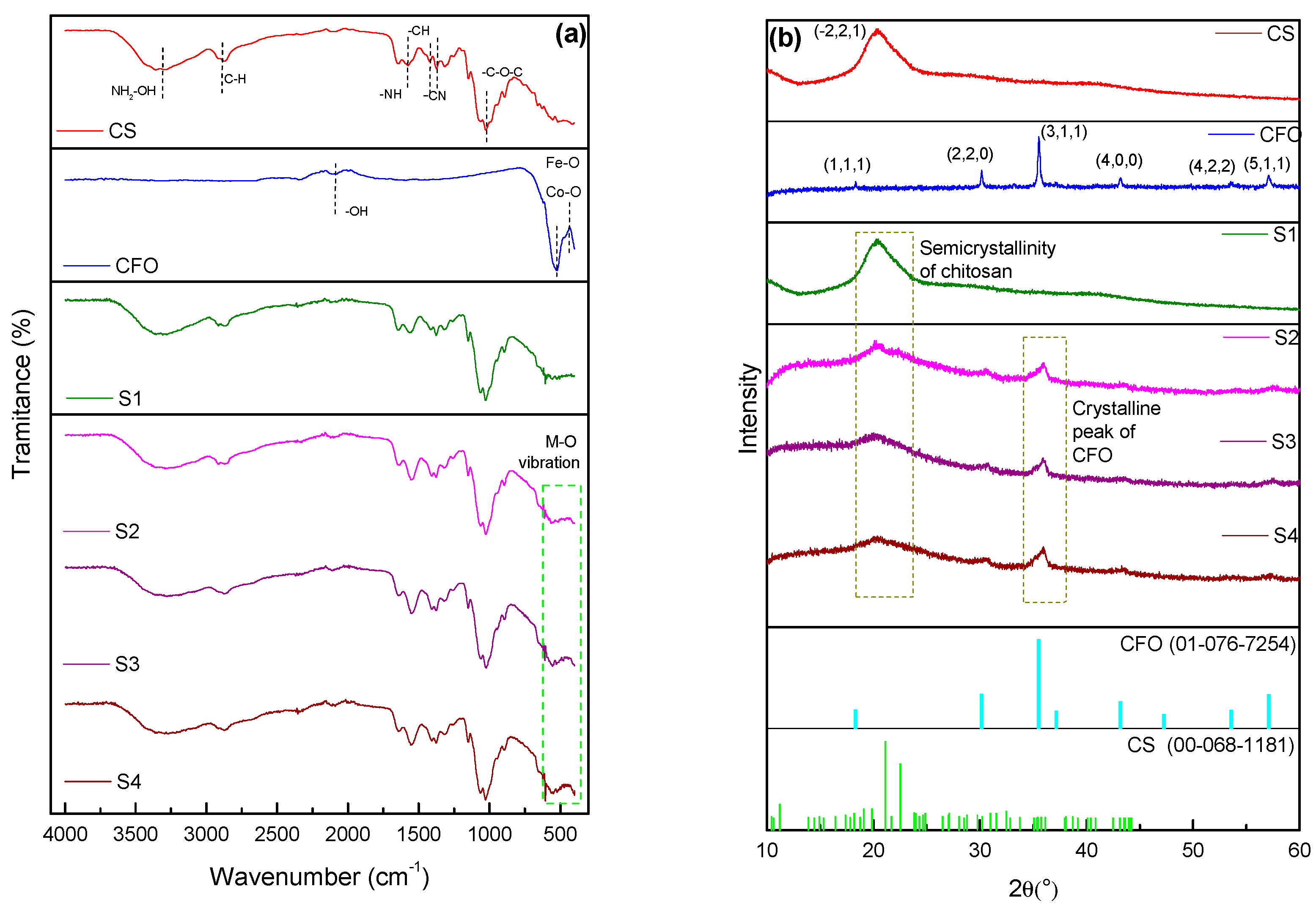



| Observed Frequency (cm−1) | Absorption Band | Assignment | Frequency Reported in the Literature (cm−1) | Reference |
|---|---|---|---|---|
| ~432 | Fe-O stretch | Axial Stretching of Fe–O in Octahedral Sites | 451 | [36] |
| ~518 | Fe-O stretch | Axial Stretching of Fe-O in Tetrahedral Sites | 562 | |
| ~1021 | C–O–C stretch | Axial Stretching of C–O–C | 1065 | [37] |
| ~1367 | C–N stretch | Axial Stretching of C-N in Primary Amines | 1386 | |
| ~1570 | N–H bend | Angular Deformation of N-H in Amide II | 1590 | [38] |
| Sample | Porosity (%) | Average Pore Diameter (µm) |
|---|---|---|
| S1 * | 78 | 104.9 |
| S2 | 79.5 | 131.3 |
| S3 | 80 | 120.5 |
| S4 | 83 | 87 |
| Sample | Ms (emu/g) | Mr (emu/g) | Hc (Oe) |
|---|---|---|---|
| S1 * | 0.16 | 0.002 | 265 |
| S2 | 3.3 | 1.5 | 1095 |
| S3 | 4.8 | 2.2 | 1274 |
| S4 | 4.3 | 2.0 | 1275 |
| Samples | Microrganisms MIC/MBC (μg.mL−1) | |||
|---|---|---|---|---|
| S. aureus MRSA ATCC (43300) | E. coli ATCC (25922) | |||
| MIC | MBC | CIM | CBM | |
| CFO | 6.250 ± 0 | - | 12.500 ± 0 | 12.500 ± 0 |
| S1 | 7.500 ± 0 | - | 7.500 ± 0 | 7.500 ± 0 |
| S3 | 37.500 ± 0 | - | 37.500 ± 0 | 37.500 ± 0 |
| Cefalexin | - | - | 3.125 ± 0 | 50.000 ± 0 |
| Sample | Cobalt Ferrite (CFO) | Chitosan (CS) |
|---|---|---|
| S1 * | 0% | 100% |
| S2 | 5% | 95% |
| S3 | 7.5% | 92.5% |
| S4 | 10% | 90% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guedes, D.G.; Guedes, G.G.; Silva, J.d.O.d.; Silva, A.L.d.; Luna, C.B.B.; Damasceno, B.P.G.d.L.; Costa, A.C.F.d.M. Development of Scaffolds with Chitosan Magnetically Activated with Cobalt Nanoferrite: A Study on Physical-Chemical, Mechanical, Cytotoxic and Antimicrobial Behavior. Pharmaceuticals 2024, 17, 1332. https://doi.org/10.3390/ph17101332
Guedes DG, Guedes GG, Silva JdOd, Silva ALd, Luna CBB, Damasceno BPGdL, Costa ACFdM. Development of Scaffolds with Chitosan Magnetically Activated with Cobalt Nanoferrite: A Study on Physical-Chemical, Mechanical, Cytotoxic and Antimicrobial Behavior. Pharmaceuticals. 2024; 17(10):1332. https://doi.org/10.3390/ph17101332
Chicago/Turabian StyleGuedes, Danyelle Garcia, Gabryella Garcia Guedes, Jessé de Oliveira da Silva, Adriano Lima da Silva, Carlos Bruno Barreto Luna, Bolívar Ponciano Goulart de Lima Damasceno, and Ana Cristina Figueiredo de Melo Costa. 2024. "Development of Scaffolds with Chitosan Magnetically Activated with Cobalt Nanoferrite: A Study on Physical-Chemical, Mechanical, Cytotoxic and Antimicrobial Behavior" Pharmaceuticals 17, no. 10: 1332. https://doi.org/10.3390/ph17101332
APA StyleGuedes, D. G., Guedes, G. G., Silva, J. d. O. d., Silva, A. L. d., Luna, C. B. B., Damasceno, B. P. G. d. L., & Costa, A. C. F. d. M. (2024). Development of Scaffolds with Chitosan Magnetically Activated with Cobalt Nanoferrite: A Study on Physical-Chemical, Mechanical, Cytotoxic and Antimicrobial Behavior. Pharmaceuticals, 17(10), 1332. https://doi.org/10.3390/ph17101332








