First In Vivo Applicational Data of Foam-Based Intrathoracic Chemotherapy (FBiTC) in a Swine Model
Abstract
:1. Introduction
2. Results
2.1. Clinical Evaluation
2.2. Evaluation of CT Scan
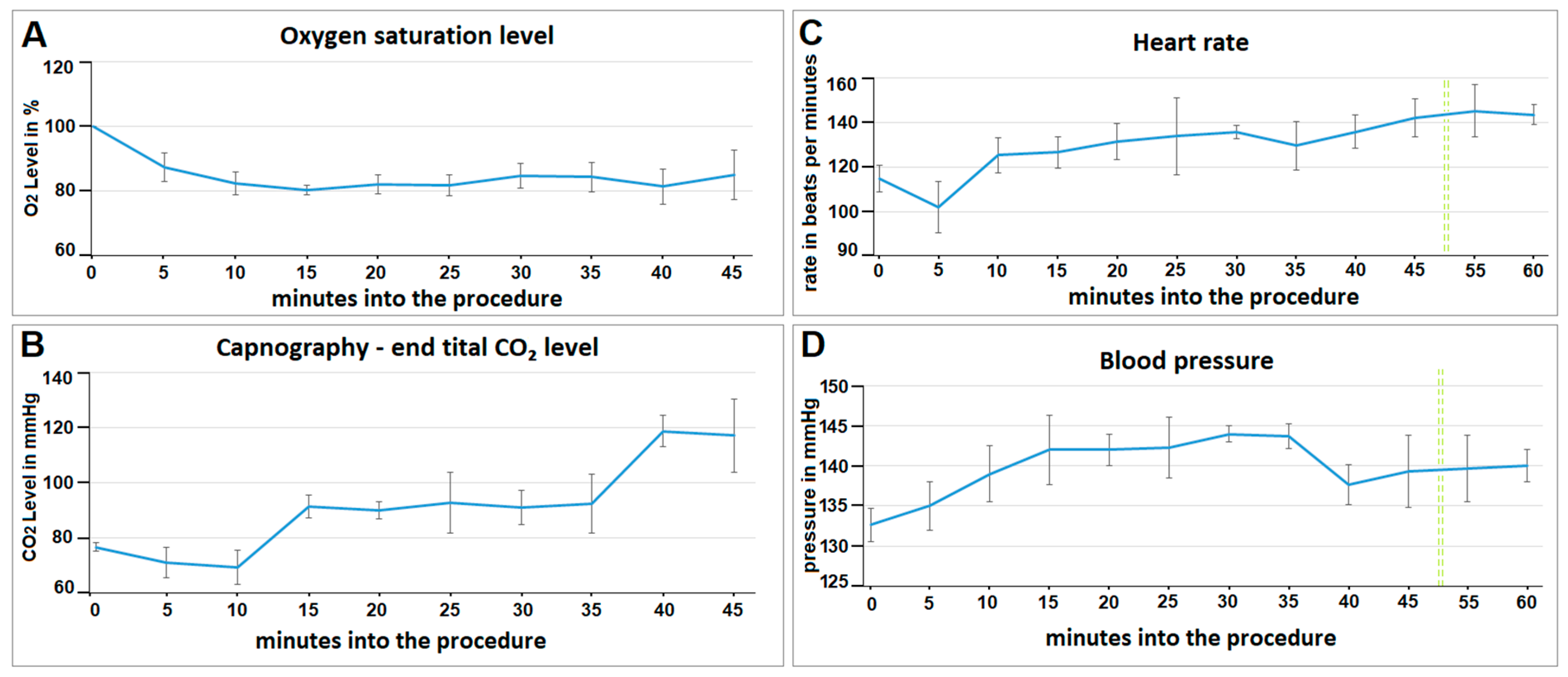
2.3. Evaluation of Vital Parameters
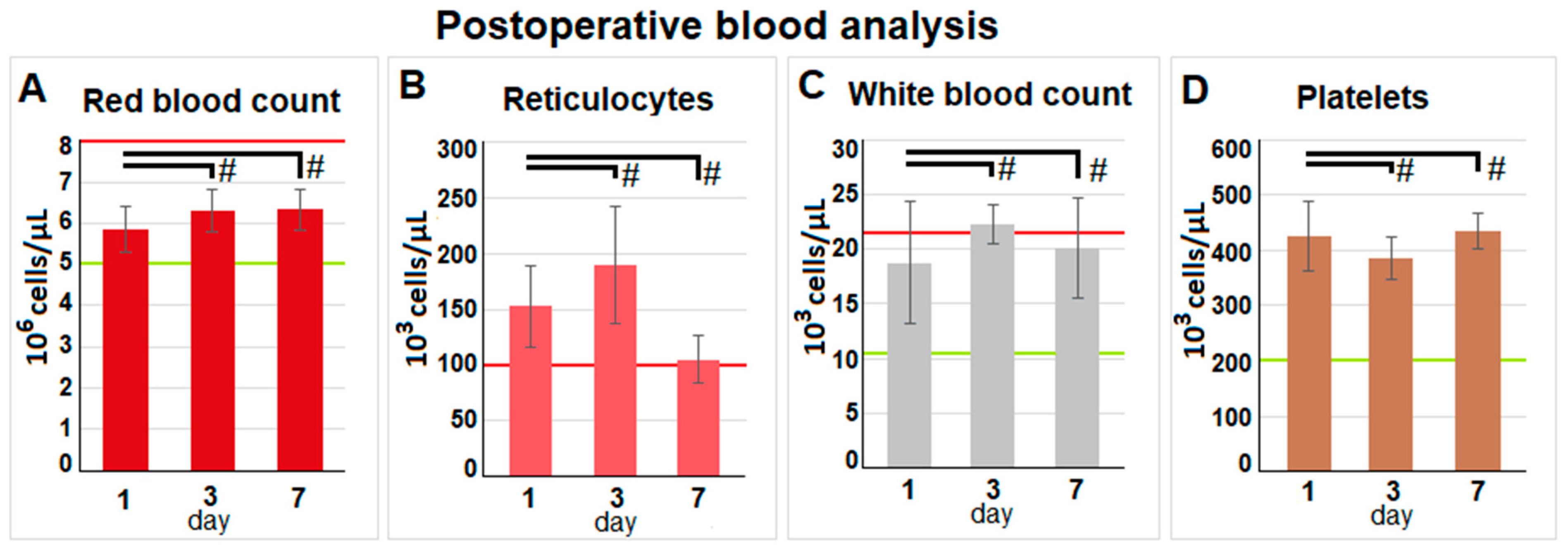
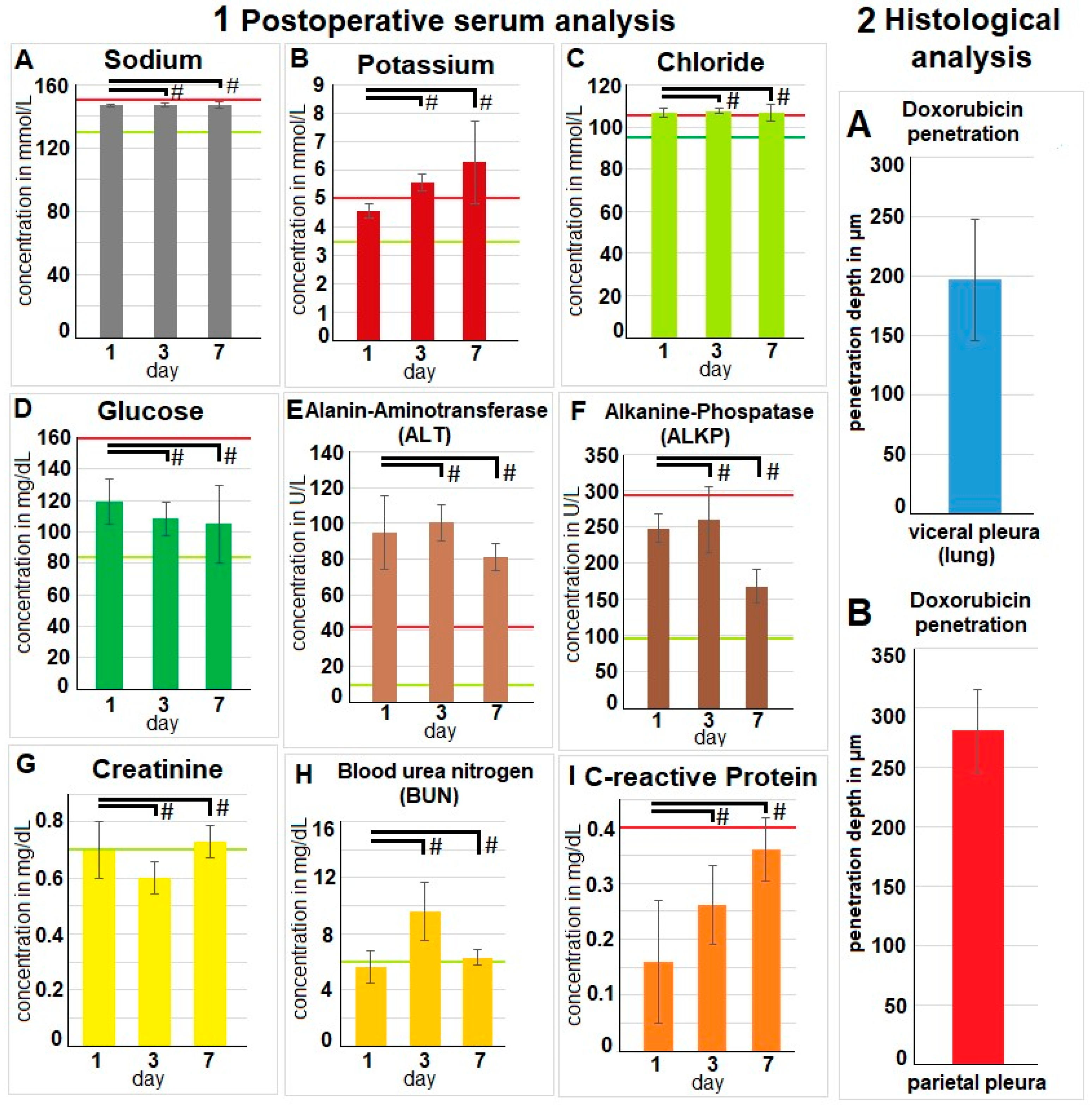
2.4. Evaluation of Postoperative Laboratory Parameters
2.5. Fluorescence Histology
3. Discussion
4. Materials and Methods
4.1. Sequence of Procedures
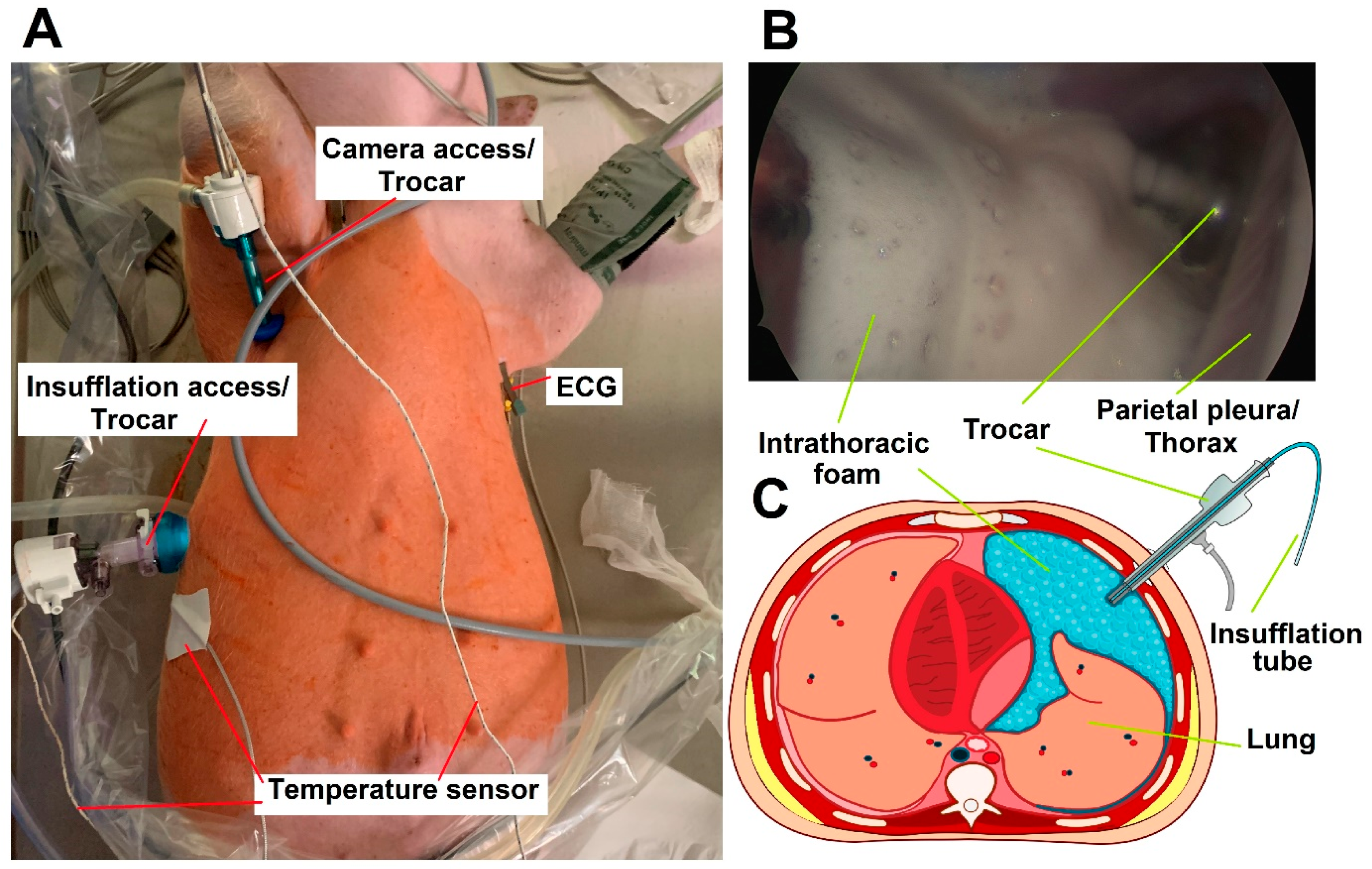
4.2. Video-Assisted Thoracoscopic (VAT) for FBiTC Application in an In Vivo Swine Model
4.3. Postoperative Monitoring
4.4. Euthanization
4.5. Microscopic Analysis of the Pleural Tissue
4.6. The Bicarbonate-Based Foam Carrier
4.7. Environmental Control and Housing Standards
4.8. Statistical Data Analyses
4.9. Ethical Approval and Regulations
4.10. Graphic Design
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Sadeghi, B.; Arvieux, C.; Glehen, O.; Beaujard, A.C.; Rivoire, M.; Baulieux, J.; Fontaumard, E.; Brachet, A.; Caillot, J.L.; Faure, J.L.; et al. Peritoneal carcinomatosis from non-gynecologic malignancies: Results of the EVOCAPE 1 multicentric prospective study. Cancer 2000, 88, 358–363. [Google Scholar] [CrossRef]
- Goéré, D.; Passot, G.; Gelli, M.; Levine, E.A.; Bartlett, D.L.; Sugarbaker, P.H.; Glehen, O. Complete cytoreductive surgery plus HIPEC for peritoneal metastases from unusual cancer sites of origin: Results from a worldwide analysis issue of the Peritoneal Surface Oncology Group International (PSOGI). Int. J. Hyperth. 2017, 33, 520–527. [Google Scholar] [CrossRef]
- Gelli, M.; Huguenin, J.F.; de Baere, T.; Benhaim, L.; Mariani, A.; Boige, V.; Malka, D.; Sourouille, I.; Ducreux, M.; Elias, D.; et al. Peritoneal and extraperitoneal relapse after previous curative treatment of peritoneal metastases from colorectal cancer: What survival can we expect? Eur. J. Cancer 2018, 100, 94–103. [Google Scholar] [CrossRef] [PubMed]
- Epelbaum, O.; Rahman, N.M. Contemporary approach to the patient with malignant pleural effusion complicating lung cancer. Ann. Transl. Med. 2019, 7, 352. [Google Scholar] [CrossRef] [PubMed]
- Akulian, J.; Feller-Kopman, D. The past, current and future of diagnosis and management of pleural disease. J. Thorac. Dis. 2015, 7 (Suppl. S4), S329–S338. [Google Scholar] [CrossRef]
- DeBiasi, E.; Puchalski, J. Pleural effusions as markers of mortality and disease severity: A state-of-the-art review. Curr. Opin. Pulm. Med. 2016, 22, 386–391. [Google Scholar] [CrossRef]
- Jiang, L.; Li, P.; Gong, Z.; Hu, B.; Ma, J.; Wang, J.; Chu, H.; Zhang, L.; Sun, P.; Chen, J. Effective treatment for malignant pleural effusion and ascites with combined therapy of bevacizumab and cisplatin. Anticancer Res. 2016, 36, 1313–1318. [Google Scholar]
- Khosrawipour, V.; Mikolajczyk, A.; Paslawski, R.; Plociennik, M.; Nowak, K.; Kulas, J.; Arafkas, M.; Khosrawipour, T. Intrathoracic aerosol chemotherapy via spray-catheter. Mol. Clin. Oncol. 2020, 12, 350–354. [Google Scholar] [CrossRef]
- Giger-Pabst, U.; Bucur, P.; Roger, S.; Falkenstein, T.A.; Tabchouri, N.; Le Pape, A.; Lerondel, S.; Demtröder, C.; Salamé, E.; Ouaissi, M. Comparison of Tissue and Blood Concentrations of Oxaliplatin Administrated by Different Modalities of Intraperitoneal Chemotherapy. Ann. Surg. Oncol. 2019, 26, 4445–4451. [Google Scholar] [CrossRef]
- Nadiradze, G.; Horvath, P.; Sautkin, Y.; Archid, R.; Weinreich, F.-J.; Königsrainer, A.; Reymond, M.A. Overcoming Drug Resistance by Taking Advantage of Physical Principles: Pressurized Intraperitoneal Aerosol Chemotherapy (PIPAC). Cancers 2019, 12, 34. [Google Scholar] [CrossRef]
- Tempfer, C.B.; Hilal, Z.; Dogan, A.; Petersen, M.; Rezniczek, G.A. Concentrations of cisplatin and doxorubicin in ascites and peritoneal tumor nodules before and after pressurized intraperitoneal aerosol chemotherapy (PIPAC) in patients with peritoneal metastasis. Eur. J. Surg. Oncol. 2018, 44, 1112–1117. [Google Scholar] [CrossRef] [PubMed]
- Eveno, C.; Haidara, A.; Ali, I.; Pimpie, C.; Mirshahi, M.; Pocard, M. Experimental pharmacokinetics evaluation of chemotherapy delivery by PIPAC for colon cancer: First evidence for efficacy. Pleura Peritoneum 2017, 2, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Piao, J.; Park, S.J.; Lee, H.; Kim, J.; Park, S.; Lee, N.; Kim, S.I.; Lee, M.; Song, G.; Lee, J.C.; et al. Ideal Nozzle Position During Pressurized Intraperitoneal Aerosol Chemotherapy in an Ex Vivo Model. Anticancer Res. 2021, 41, 5489–5498. [Google Scholar] [CrossRef] [PubMed]
- Schubert, J.; Khosrawipour, T.; Reinhard, S.; Arafkas, M.; Martino, A.; Bania, J.; Pieczka, M.; Pigazzi, A.; Khosrawipour, V. The concept of foam as a drug carrier for intraperitoneal chemotherapy, feasibility, cytotoxicity and characteristics. Sci. Rep. 2020, 10, 10341. [Google Scholar] [CrossRef] [PubMed]
- Diakun, A.; Khosrawipour, T.; Mikolajczyk-Martinez, A.; Nicpoń, J.; Thelen, S.; Kiełbowicz, Z.; Prządka, P.; Liszka, B.; Kulas, J.; Zielinski, K.; et al. Safety, feasibility, and application of intraperitoneal gas-based hyperthermia beyond 43 °C in the treatment of peritoneal metastasis: An in-vivo pilot study. Front. Oncol. 2022, 12, 953920. [Google Scholar] [CrossRef]
- Monchi, M. Citrate pathophysiology and metabolism. Transfus. Apher. Sci. 2017, 56, 28–30. [Google Scholar] [CrossRef]
- Kozik-Jaromin, J.; Nier, V.; Heemann, U.; Kreymann, B.; Böhler, J. Citrate pharmacokinetics and calcium levels during high-flux dialysis with regional citrate anticoagulation. Nephrol. Dial. Transplant. 2009, 24, 2244–2251. [Google Scholar] [CrossRef]
- Pepe, J.; Colangelo, L.; Biamonte, F.; Sonato, C.; Danese, V.C.; Cecchetti, V.; Occhiuto, M.; Piazzolla, V.; De Martino, V.; Ferrone, F.; et al. Diagnosis and management of hypocalcemia. Endocrine 2020, 69, 485–495. [Google Scholar] [CrossRef]
- Martin, H.E.; Wertman, M. Clinical potassium problems. Calif. Med. 1950, 72, 133–141. [Google Scholar]
- Aronson, P.S.; Giebisch, G. Effects of pH on Potassium: New explanations for old observations. J. Am. Soc. Nephrol. 2011, 22, 1981–1989. [Google Scholar] [CrossRef]
- Perez, G.O.; Oster, J.R.; Vaamonde, C.A. Serum potassium concentration in acidemic states. Nephron 1981, 27, 233–243. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Tanojo, H.; Lenn, J.; Deng, C.H.; Krochmal, L. A novel foam vehicle for delivery of topical corticosteroids. J. Am. Acad. Dermatol. 2005, 53 (Suppl. S1), S26–S38. [Google Scholar] [CrossRef] [PubMed]
- Mei, L.; Chen, J.; Yu, S.; Huang, Y.; Xie, Y.; Wang, H.; Pan, X.; Wu, C. Expansible thermal gelling foam aerosol for vaginal drug delivery. Drug Deliv. 2017, 24, 1325–1337. [Google Scholar] [CrossRef] [PubMed]
- Loew, B.J.; Siegel, C.A. Foam preparations for the treatment of ulcerative colitis. Curr. Drug Deliv. 2012, 9, 338–344. [Google Scholar] [CrossRef] [PubMed]
- Griffis, C.D.; Metcalfe, S.; Bowling, F.L.; Boulton, A.J.; Armstrong, D.G. The use of gentamicin-impregnated foam in the management of diabetic foot infections: A promising delivery system? Expert Opin. Drug Deliv. 2009, 6, 639–642. [Google Scholar] [CrossRef]
- del Castillo-Santaella, T.; Yang, Y.; Martínez-González, I.; Gálvez-Ruiz, M.J.; Cabrerizo-Vílchez, M.; Holgado-Terriza, J.A.; Selles-Galiana, F.; Maldonado-Valderrama, J. Effect of Hyaluronic Acid and Pluronic-F68 on the Surface Properties of Foam as a Delivery System for Polidocanol in Sclerotherapy. Pharmaceutics 2020, 12, 1039. [Google Scholar] [CrossRef]
- Kanai, E.; Matsutani, N.; Watanabe, R.; Yamamoto, Y.; Sakai, T.; Misumi, T.; Fujii, Y.; Takagi, S. Effects of combined one-lung ventilation and intrathoracic carbon dioxide insufflation on intrathoracic working space when performing thoracoscopy in dogs. Am. J. Vet. Res. 2022, 83, ajvr.22.01.0009. [Google Scholar] [CrossRef]
- Ren, Y.; Zhu, X.; Yan, H.; Chen, L.; Mao, Q. Cardiorespiratory impact of intrathoracic pressure overshoot during artificial carbon dioxide pneumothorax: A randomized controlled study. BMC Anesthesiol. 2022, 22, 76. [Google Scholar] [CrossRef]
- Trča, S.; Krška, Z.; Kittnar, O.; Mlček, M.; Demeš, R.; Danzig, V.; Šimek, S.; Bruthans, J.; Fraško, R. Hemodynamic response to thoracoscopy and thoracotomy. Physiol. Res. 2010, 59, 363–371. [Google Scholar] [CrossRef]
- Garber, J.C.; Barbee, R.W.; Bielitzko, J.T.; Clayton, L.A.; Donovan, J.C.; Hendriksen, C.F.M.; Kohn, D.F.; Lipman, P.A.; Locke, P.A.; Melcher, J.; et al. Guide for the Care and Use of Laboratory Animals: Eighth Edition [Internet]; National Academies Press: Washington, DC, USA, 2011; Available online: http://www.nap.edu/catalog/12910 (accessed on 24 October 2023).

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khosrawipour, C.; Nicpoń, J.; Kiełbowicz, Z.; Prządka, P.; Liszka, B.; Zielinski, K.; Khosrawipour, V.; Li, S.; Lau, H.; Kulas, J.; et al. First In Vivo Applicational Data of Foam-Based Intrathoracic Chemotherapy (FBiTC) in a Swine Model. Pharmaceuticals 2024, 17, 45. https://doi.org/10.3390/ph17010045
Khosrawipour C, Nicpoń J, Kiełbowicz Z, Prządka P, Liszka B, Zielinski K, Khosrawipour V, Li S, Lau H, Kulas J, et al. First In Vivo Applicational Data of Foam-Based Intrathoracic Chemotherapy (FBiTC) in a Swine Model. Pharmaceuticals. 2024; 17(1):45. https://doi.org/10.3390/ph17010045
Chicago/Turabian StyleKhosrawipour, Carolina, Jakub Nicpoń, Zdzisław Kiełbowicz, Przemysław Prządka, Bartłomiej Liszka, Kacper Zielinski, Veria Khosrawipour, Shiri Li, Hien Lau, Joanna Kulas, and et al. 2024. "First In Vivo Applicational Data of Foam-Based Intrathoracic Chemotherapy (FBiTC) in a Swine Model" Pharmaceuticals 17, no. 1: 45. https://doi.org/10.3390/ph17010045
APA StyleKhosrawipour, C., Nicpoń, J., Kiełbowicz, Z., Prządka, P., Liszka, B., Zielinski, K., Khosrawipour, V., Li, S., Lau, H., Kulas, J., Diakun, A., Kielan, W., Mikolajczk-Martinez, A., & Chabowski, M. (2024). First In Vivo Applicational Data of Foam-Based Intrathoracic Chemotherapy (FBiTC) in a Swine Model. Pharmaceuticals, 17(1), 45. https://doi.org/10.3390/ph17010045







