Electrophilic Agonists Modulate the Transient Receptor Potential Ankyrin-1 Channels Mediated by Insulin and Glucagon-like Peptide-1 Secretion for Glucose Homeostasis
Abstract
1. Introduction
2. Results
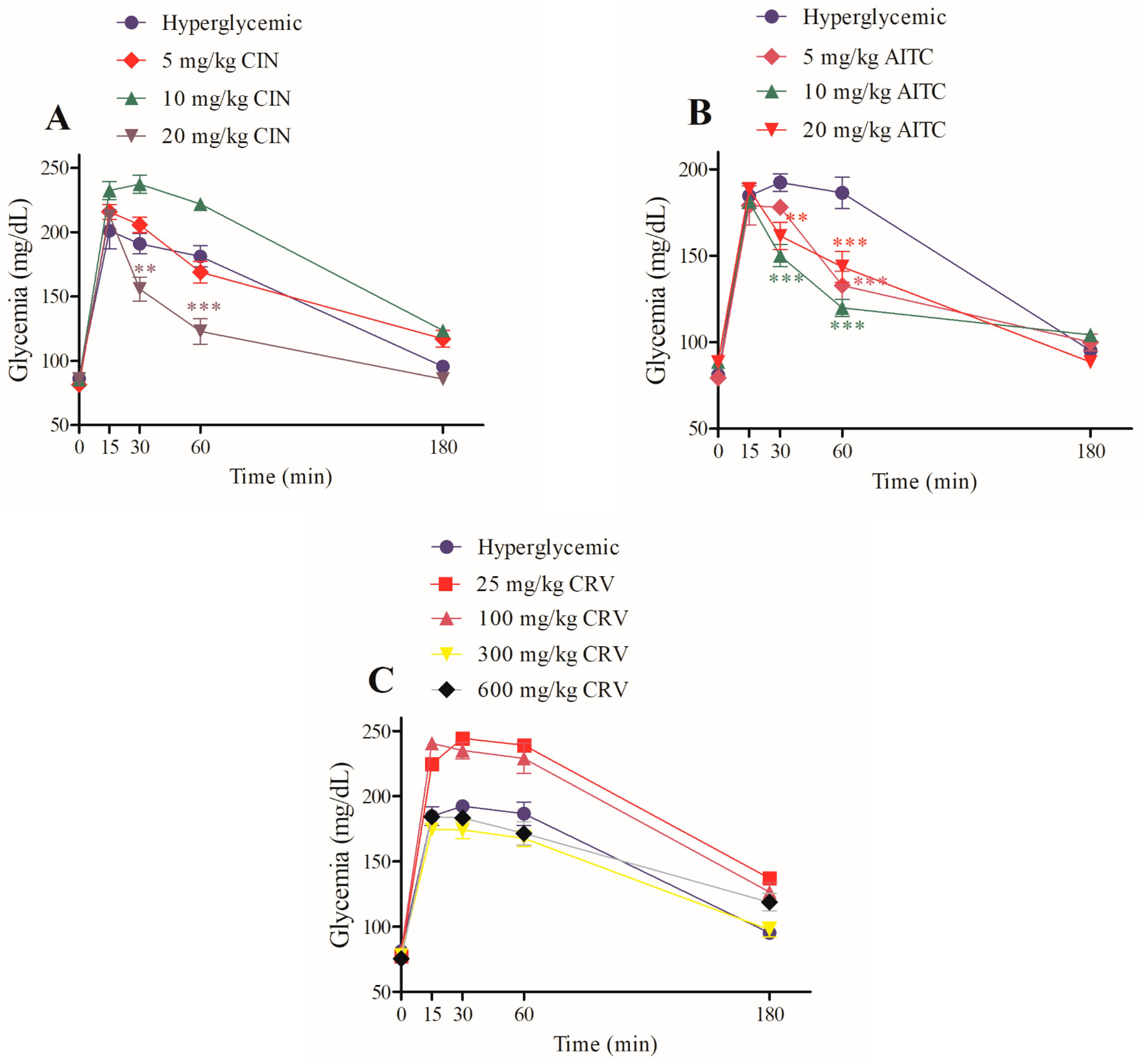
2.1. Role of Transient Receptor Potential Ankyrin-1 in Maintaining Glucose Tolerance
2.2. Influence of Transient Receptor Potential Ankyrin-1 Agonists on the Activity of Intestinal Disaccharides
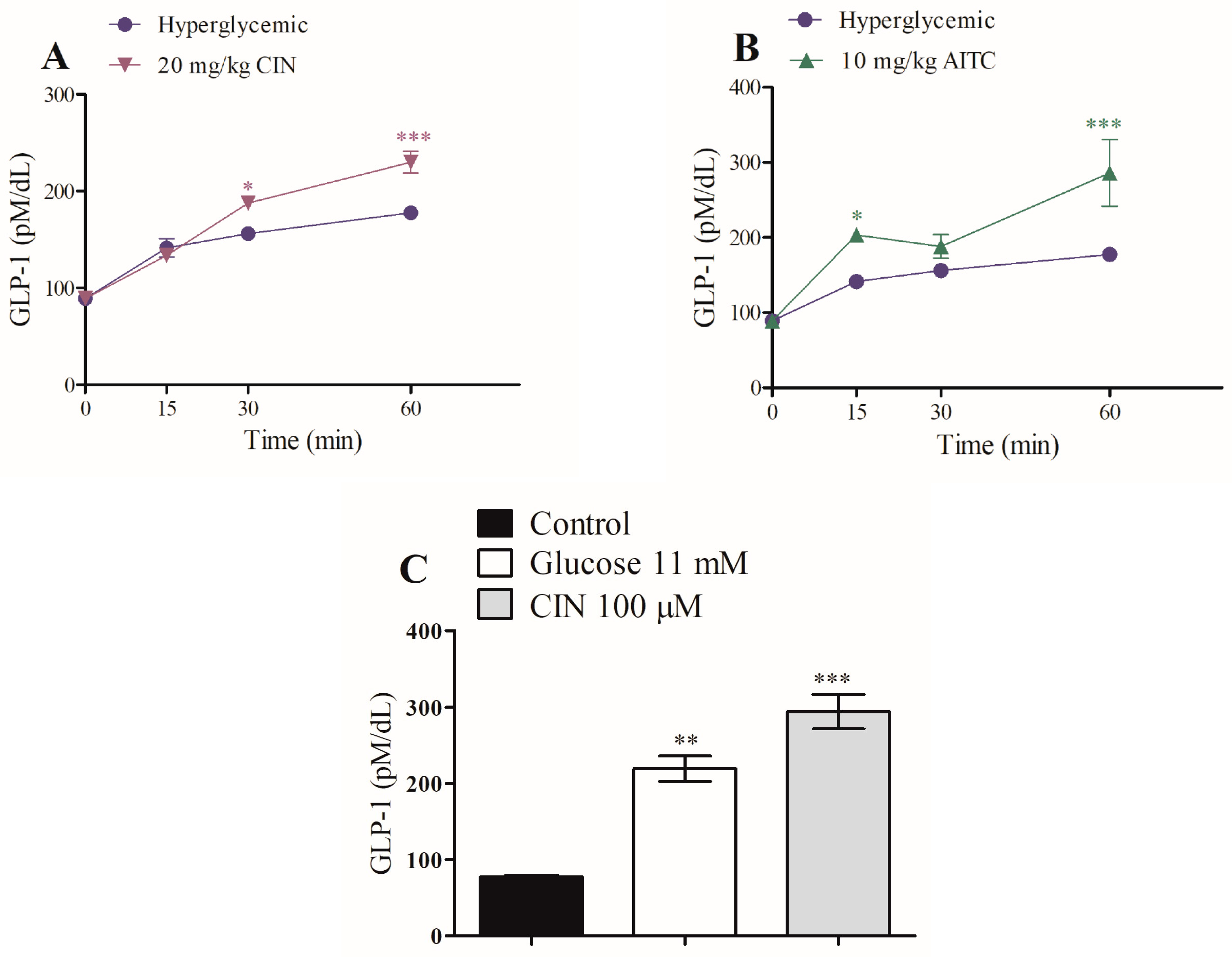
2.3. Effects of Transient Receptor Potential Ankyrin-1 Agonists on Glucagon-like Peptide-1 Secretion
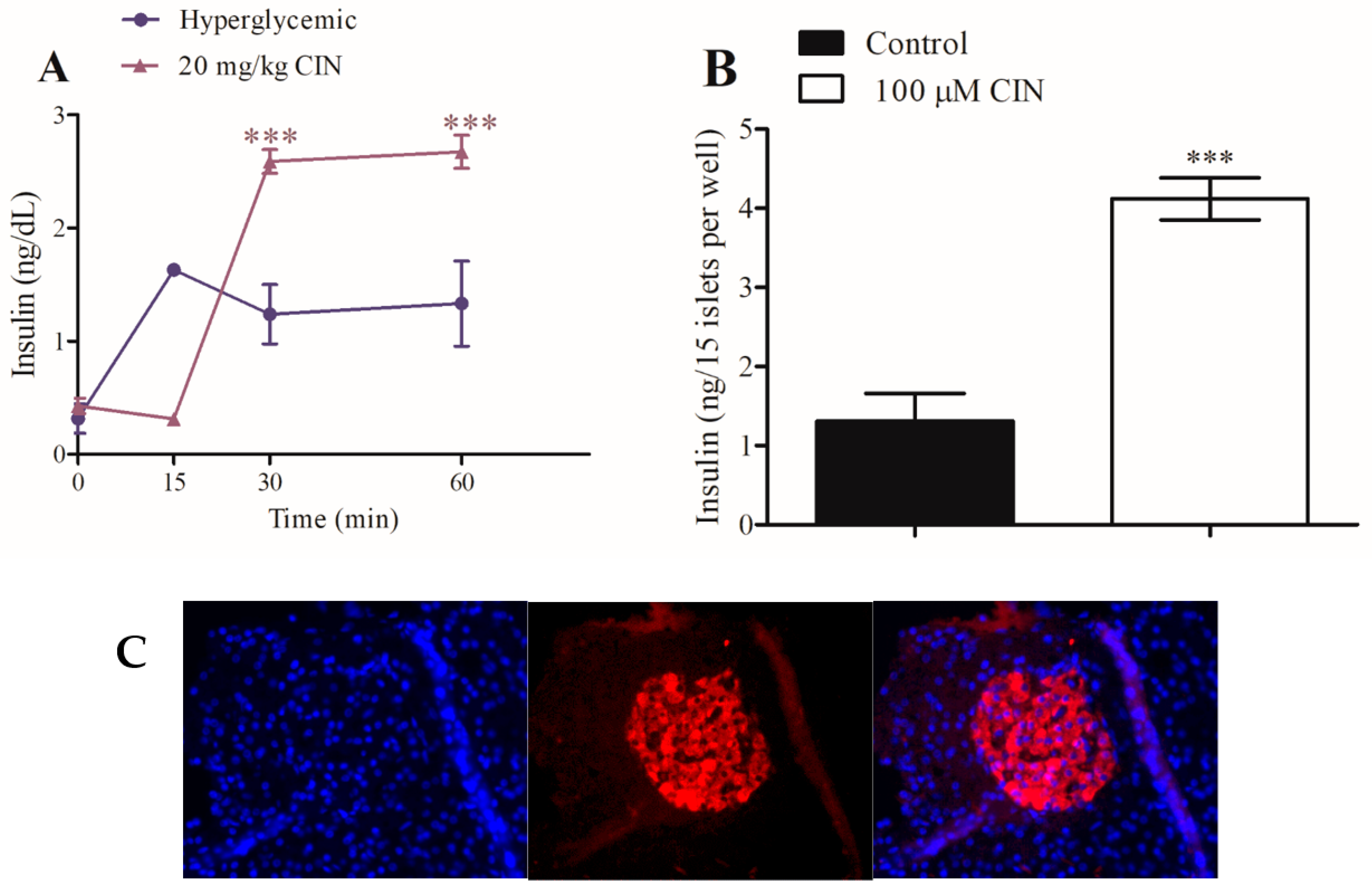
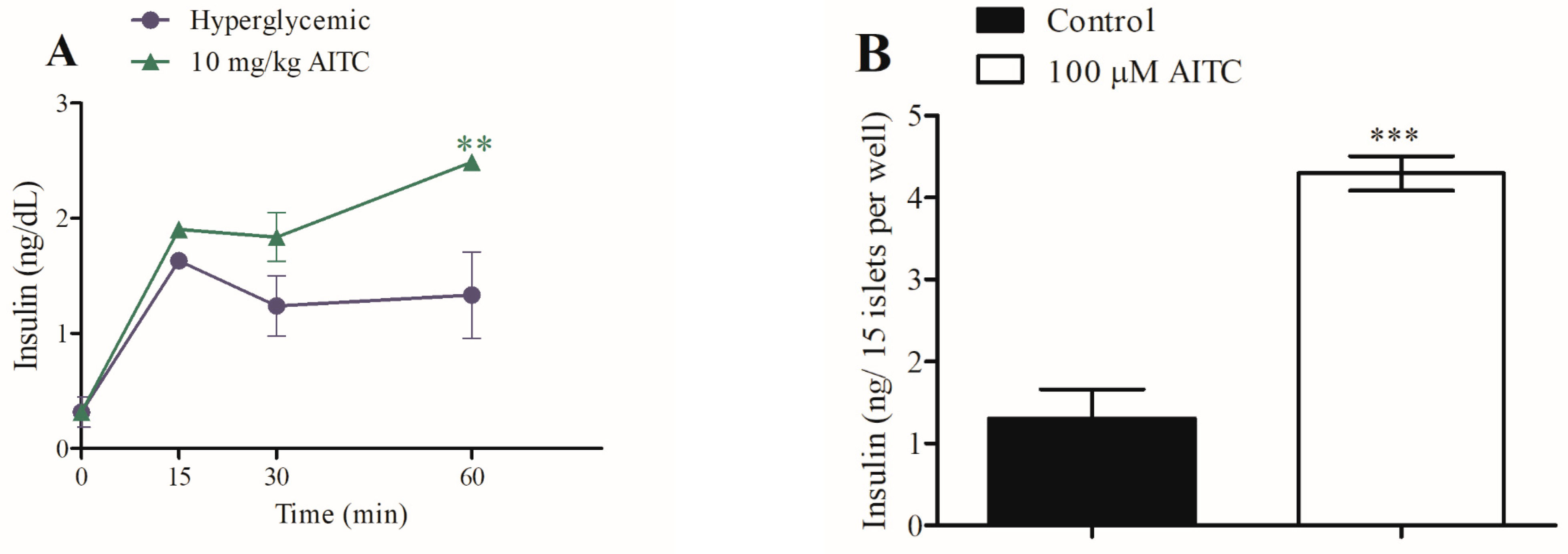
2.4. Role of Transient Receptor Potential Ankyrin-1 on In Vivo and In Vitro Insulin Secretion
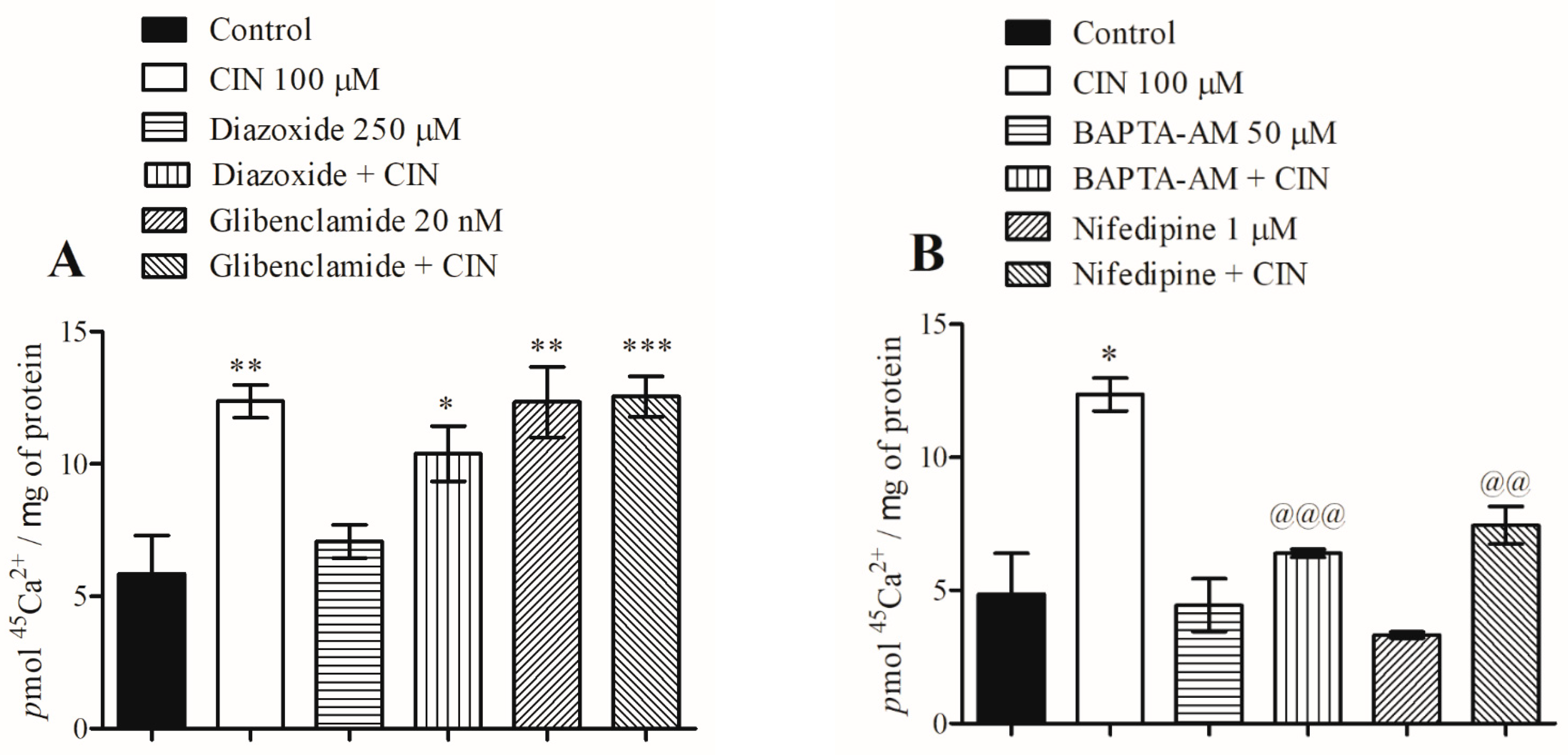
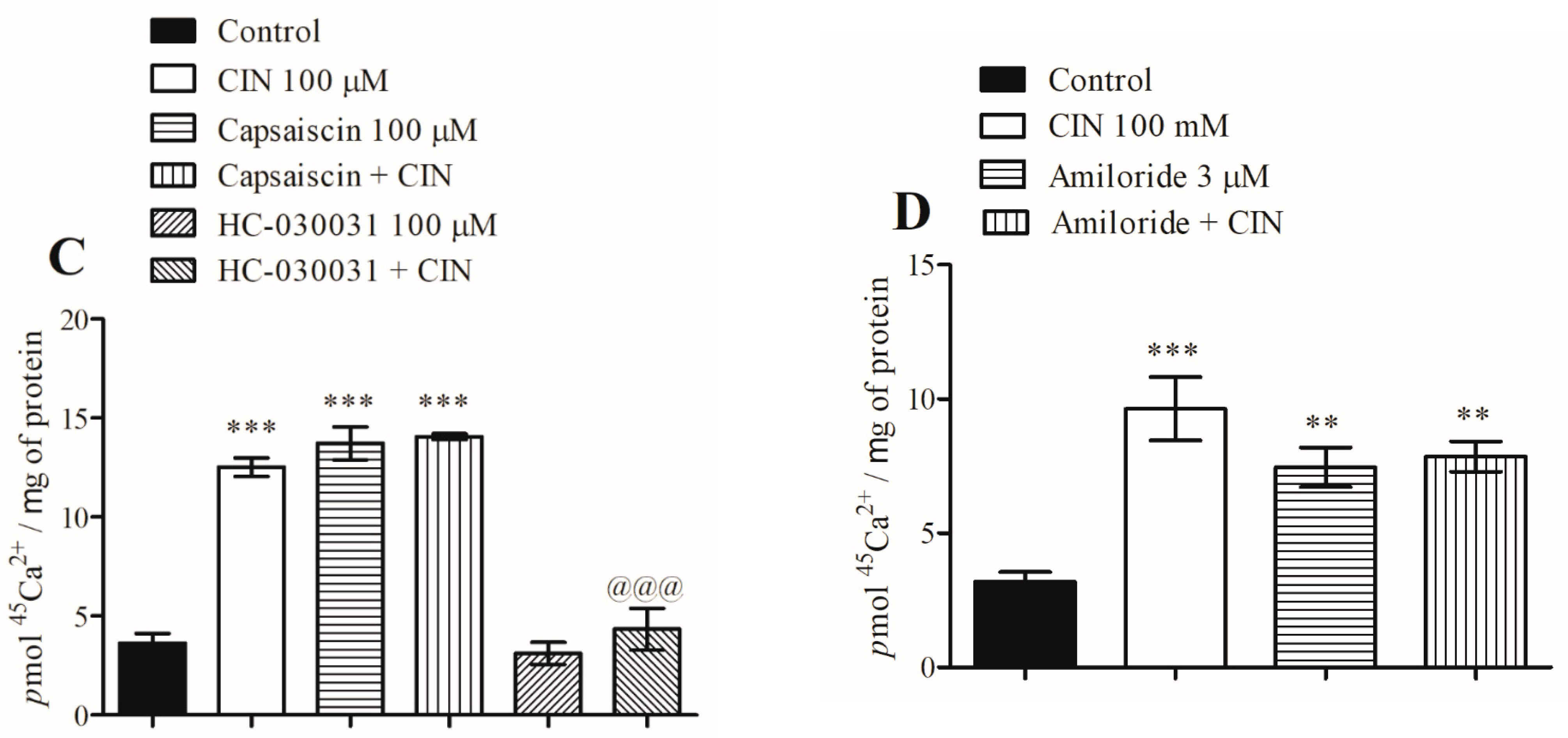
2.5. Mechanism by Which Transient Receptor Potential Ankyrin-1 Agonists Modulate Calcium Influx Signaling Pathways during Insulin Secretion
3. Discussion
4. Materials and Methods
4.1. Animals
4.2. Effects of Cinnamaldehyde, Allylisothiocyanate and Carvacrol on Glucose Tolerance, Serum Glucagon-like Peptide-1, and Insulin Secretion
4.3. Effects of Cinnamaldehyde, Allylisothiocyanate and Carvacrol on Intestinal Disaccharidase Activity (In Vitro)
4.4. Isolation of Intestinal Colon Slices for Static Glucagon-like Peptide-1 Measurement
4.5. Insulin and Glucagon-like Peptide-1 Measurements
4.6. Immunofluorescence Images of the Islet Architecture for β-Cell Staining
4.7. Isolation of Pancreatic Islets for Studies on Calcium Influx and Static Insulin Measurement
4.8. Study of the Effects of Transient Receptor Potential Ankyrin-1 Agonists/Antagonists on the Stimulatory Effect of Cinnamaldehyde on Calcium Influx in Pancreatic Islets
4.9. Statistical Analyzes
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Calcaterra, V.; Vandoni, M.; Pellino, V.C.; Cena, H. Special Attention to Diet and Physical Activity in Children and Adolescents with Obesity During the Coronavirus Disease-2019 Pandemic. Front. Pediatr. 2020, 8, 407. [Google Scholar] [CrossRef] [PubMed]
- Buse, J.B.; Davies, M.J.; Frier, B.M.; Philis-Tsimikas, A. 100 Years on: The Impact of the Discovery of Insulin on Clinical Outcomes. BMJ Open Diabetes Res. Care 2021, 9, e002373. [Google Scholar] [CrossRef] [PubMed]
- Cao, D.S.; Zhong, L.; Hsieh, T.H.; Abooj, M.; Bishnoi, M.; Hughes, L.; Premkumar, L.S. Expression of Transient Receptor Potential Ankyrin 1 (TRPA1) and Its Role in Insulin Release from Rat Pancreatic Beta Cells. PLoS ONE 2012, 7, e38005. [Google Scholar] [CrossRef] [PubMed]
- Togashi, K.; Hara, Y.; Tominaga, T.; Higashi, T.; Konishi, Y.; Mori, Y.; Tominaga, M. TRPM2 Activation by Cyclic ADP-Ribose at Body Temperature Is Involved in Insulin Secretion. EMBO J. 2006, 25, 1804–1815. [Google Scholar] [CrossRef]
- Cheng, H.; Beck, A.; Launay, P.; Gross, S.A.; Stokes, A.J.; Kinet, J.P.; Fleig, A.; Penner, R. TRPM4 Controls Insulin Secretion in Pancreatic Beta-Cells. Cell. Calcium 2007, 41, 51–61. [Google Scholar] [CrossRef]
- Purhonen, A.K.; Louhivuori, L.M.; Kiehne, K.; Kerman, K.E.; Herzig, K.H. TRPA1 Channel Activation Induces Cholecystokinin Release via Extracellular Calcium. FEBS Lett. 2008, 582, 229–232. [Google Scholar] [CrossRef]
- Macpherson, L.J.; Dubin, A.E.; Evans, M.J.; Marr, F.; Schultz, P.G.; Cravatt, B.F.; Patapoutian, A. Noxious Compounds Activate TRPA1 Ion Channels through Covalent Modification of Cysteines. Nature 2007, 445, 541–545. [Google Scholar] [CrossRef]
- Del Prete, D.; Caprioglio, D.; Appendino, G.; Minassi, A.; Schiano-Moriello, A.; Di Marzo, V.; De Petrocellis, L. Discovery of Non-Electrophilic Capsaicinoid-Type TRPA1 Ligands. Bioorg. Med. Chem. Lett. 2015, 25, 1009–1011. [Google Scholar] [CrossRef]
- Fajardo, O.; Meseguer, V.; Belmonte, C.; Viana, F. TRPA1 Channels: Novel Targets of 1,4-Dihydropyridines. Channels 2008, 2, 429–438. [Google Scholar] [CrossRef]
- Alpizar, Y.A.; Gees, M.; Sanchez, A.; Apetrei, A.; Voets, T.; Nilius, B.; Talavera, K. Bimodal Effects of Cinnamaldehyde and Camphor on Mouse TRPA1. Pflügers Arch. Eur. J. Physiol. 2013, 465, 853–864. [Google Scholar] [CrossRef]
- Komatsu, M.; Takei, M.; Ishii, H.; Sato, Y. Glucose-Stimulated Insulin Secretion: A Newer Perspective. J. Diabetes Investig. 2013, 4, 511–516. [Google Scholar] [CrossRef] [PubMed]
- Kichko, T.I.; Kobal, G.; Reeh, P.W. Cigarette Smoke Has Sensory Effects through Nicotinic and TRPA1 but Not TRPV1 Receptors on the Isolated Mouse Trachea and Larynx. Am. J. Physiol. Lung Cell. Mol. Physiol. 2015, 309, L812–L820. [Google Scholar] [CrossRef] [PubMed]
- Xiao, B.; Dubin, A.E.; Bursulaya, B.; Viswanath, V.; Jegla, T.J.; Patapoutian, A. Identification of Transmembrane Domain 5 as a Critical Molecular Determinant of Menthol Sensitivity in Mammalian TRPA1 Channels. J. Neurosci. 2008, 28, 9640–9651. [Google Scholar] [CrossRef]
- Srivastava, S.; Shree, P.; Tripathi, Y.B. Active Phytochemicals of Pueraria Tuberosa for DPP-IV Inhibition: In Silico and Experimental Approach. J. Diabetes Metab. Disord. 2017, 16, 46. [Google Scholar] [CrossRef]
- Kahn, S.E.; Lachin, J.M.; Zinman, B.; Haffner, S.M.; Aftring, R.P.; Paul, G.; Kravitz, B.G.; Herman, W.H.; Viberti, G.; Holman, R.R.; et al. Effects of Rosiglitazone, Glyburide, and Metformin on β-Cell Function and Insulin Sensitivity in ADOPT. Diabetes 2011, 60, 1552–1560. [Google Scholar] [CrossRef] [PubMed]
- Ashcroft, F.M.; Rorsman, P. K(ATP) Channels and Islet Hormone Secretion: New Insights and Controversies. Nat. Rev. Endocrinol. 2013, 9, 660–669. [Google Scholar] [CrossRef]
- Gram, D.X.; Ahrén, B.; Nagy, I.; Olsen, U.B.; Brand, C.L.; Sundler, F.; Tabanera, R.; Svendsen, O.; Carr, R.D.; Santha, P.; et al. Capsaicin-Sensitive Sensory Fibers in the Islets of Langerhans Contribute to Defective Insulin Secretion in Zucker Diabetic Rat, an Animal Model for Some Aspects of Human Type 2 Diabetes. Eur. J. Neurosci. 2007, 25, 213–223. [Google Scholar] [CrossRef]
- Hafizur, R.M.; Hameed, A.; Shukrana, M.; Raza, S.A.; Chishti, S.; Kabir, N.; Siddiqui, R.A. Cinnamic Acid Exerts Anti-Diabetic Activity by Improving Glucose Tolerance in Vivo and by Stimulating Insulin Secretion in Vitro. Phytomedicine 2015, 22, 297–300. [Google Scholar] [CrossRef]
- Kumar, S.; Vasudeva, N.; Sharma, S. GC-MS Analysis and Screening of Antidiabetic, Antioxidant and Hypolipidemic Potential of Cinnamomum Tamala Oil in Streptozotocin Induced Diabetes Mellitus in Rats. Cardiovasc. Diabetol. 2012, 11, 95. [Google Scholar] [CrossRef]
- Blevins, S.M.; Leyva, M.J.; Brown, J.; Wright, J.; Scofield, R.H.; Aston, C.E. Effect of Cinnamon on Glucose and Lipid Levels in Non Insulin-Dependent Type 2 Diabetes. Diabetes Care 2007, 30, 2236–2237. [Google Scholar] [CrossRef]
- Vanschoonbeek, K.; Thomassen, B.J.W.; Senden, J.M.; Wodzig, W.K.W.H.; van Loon, L.J.C. Cinnamon Supplementation Does Not Improve Glycemic Control in Postmenopausal Type 2 Diabetes Patients. J. Nutr. 2006, 136, 977–980. [Google Scholar] [CrossRef] [PubMed]
- Wickenberg, J.; Lindstedt, S.; Berntorp, K.; Nilsson, J.; Hlebowicz, J. Ceylon Cinnamon Does Not Affect Postprandial Plasma Glucose or Insulin in Subjects with Impaired Glucose Tolerance. Br. J. Nutr. 2012, 107, 1845–1849. [Google Scholar] [CrossRef] [PubMed]
- Silva, M.L.; Bernardo, M.A.; Singh, J.; de Mesquita, M.F. Cinnamon as a Complementary Therapeutic Approach for Dysglycemia and Dyslipidemia Control in Type 2 Diabetes Mellitus and Its Molecular Mechanism of Action: A Review. Nutrients 2022, 14, 2773. [Google Scholar] [CrossRef]
- Sahin, N.; Orhan, C.; Erten, F.; Tuzcu, M.; Defo Deeh, P.B.; Ozercan, I.H.; Juturu, V.; Kazim, S. Effects of Allyl Isothiocyanate on Insulin Resistance, Oxidative Stress Status, and Transcription Factors in High-Fat Diet/Streptozotocin-Induced Type 2 Diabetes Mellitus in Rats. J. Biochem. Mol. Toxicol. 2019, 33, e22328. [Google Scholar] [CrossRef]
- Ezhumalai, M.; Radhiga, T.; Pugalendi, K.V. Antihyperglycemic Effect of Carvacrol in Combination with Rosiglitazone in High-Fat Diet-Induced Type 2 Diabetic C57BL/6J Mice. Mol. Cell. Biochem. 2014, 385, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Inouye, K.; Shum, K.; Chan, O.; Mathoo, J.; Matthews, S.G.; Vranic, M. Effects of Recurrent Hyperinsulinemia with and without Hypoglycemia on Counterregulation in Diabetic Rats. Am. J. Physiol. Endocrinol. Metab. 2002, 282, E1369–E1379. [Google Scholar] [CrossRef][Green Version]
- Nagata, M.; Nakajima, M.; Ishiwata, Y.; Takahashi, Y.; Takahashi, H.; Negishi, K.; Yasuhara, M. Mechanism Underlying Induction of Hyperglycemia in Rats by Single Administration of Olanzapine. Biol. Pharm. Bull. 2016, 39, 754–761. [Google Scholar] [CrossRef] [PubMed]
- Nagata, M.; Kimura, Y.; Ishiwata, Y.; Takahashi, H.; Yasuhara, M. Clozapine-Induced Acute Hyperglycemia Is Accompanied with Elevated Serum Concentrations of Adrenaline and Glucagon in Rats. Biol. Pharm. Bull. 2018, 41, 1286–1290. [Google Scholar] [CrossRef]
- Krasikov, V.V.; Karelov, D.V.; Firsov, L.M. Alpha-Glucosidases. Biochemistry 2001, 66, 267–281. [Google Scholar]
- Liu, L.; Yu, Y.L.; Yang, J.S.; Li, Y.; Liu, Y.W.; Liang, Y.; Liu, X.D.; Xie, L.; Wang, G.J. Berberine Suppresses Intestinal Disaccharidases with Beneficial Metabolic Effects in Diabetic States, Evidences from in Vivo and in Vitro Study. Naunyn. Schmiedebergs. Arch. Pharmacol. 2010, 381, 371–381. [Google Scholar] [CrossRef]
- Campbell, L.K.; Baker, D.E.; Campbell, R.K. Miglitol: Assessment of Its Role in the Treatment of Patients with Diabetes Mellitus. Ann. Pharmacother. 2000, 34, 1291–1301. [Google Scholar] [CrossRef] [PubMed]
- Kaji, I.; Yasuoka, Y.; Karaki, S.; Kuwahara, A. Activation of TRPA1 by Luminal Stimuli Induces EP4-Mediated Anion Secretion in Human and Rat Colon. Am. J. Physiol. Gastrointest. Liver Physiol. 2012, 302, G690–G701. [Google Scholar] [CrossRef] [PubMed]
- Poole, D.P.; Pelayo, J.C.; Cattaruzza, F.; Kuo, Y.M.; Gai, G.; Chiu, J.V.; Bron, R.; Furness, J.B.; Grady, E.F.; Bunnett, N.W. Transient Receptor Potential Ankyrin 1 Is Expressed by Inhibitory Motoneurons of the Mouse Intestine. Gastroenterology 2011, 141, 565–575. [Google Scholar] [CrossRef]
- Kim, M.J.; Son, H.J.; Song, S.H.; Jung, M.; Kim, Y.; Rhyu, M.R. The TRPA1 Agonist, Methyl Syringate Suppresses Food Intake and Gastric Emptying. PLoS ONE 2013, 8, e71603. [Google Scholar] [CrossRef] [PubMed]
- Emery, E.C.; Diakogiannaki, E.; Gentry, C.; Psichas, A.; Habib, A.M.; Bevan, S.; Fischer, M.J.; Reimann, F.; Gribble, F.M. Stimulation of GLP-1 Secretion Downstream of the Ligand-Gated Ion Channel TRPA1. Diabetes 2015, 64, 1202–1210. [Google Scholar] [CrossRef]
- Babes, A.; Fischer, M.J.; Filipovic, M.; Engel, M.A.; Flonta, M.L.; Reeh, P.W. The Anti-Diabetic Drug Glibenclamide Is an Agonist of the Transient Receptor Potential Ankyrin 1 (TRPA1) Ion Channel. Eur. J. Pharmacol. 2013, 704, 15–22. [Google Scholar] [CrossRef]
- Numazawa, S.; Takase, M.; Ahiko, T.; Ishii, M.; Shimizu, S.; Yoshida, T. Possible Involvement of Transient Receptor Potential Channels in Electrophile-Induced Insulin Secretion from RINm5F Cells. Biol. Pharm. Bull. 2012, 35, 346–354. [Google Scholar] [CrossRef][Green Version]
- Akiba, Y.; Kato, S.; Katsube, K.; Nakamura, M.; Takeuchi, K.; Ishii, H.; Hibi, T. Transient Receptor Potential Vanilloid Subfamily 1 Expressed in Pancreatic Islet Beta Cells Modulates Insulin Secretion in Rats. Biochem. Biophys. Res. Commun. 2004, 321, 219–225. [Google Scholar] [CrossRef]
- Gustavsson, N.; Wu, B.; Han, W. Calcium Sensing in Exocytosis. Adv. Exp. Med. Biol. 2012, 740, 731–757. [Google Scholar] [CrossRef]
- Harach, T.; Pols, T.W.; Nomura, M.; Maida, A.; Watanabe, M.; Auwerx, J.; Schoonjans, K. TGR5 Potentiates GLP-1 Secretion in Response to Anionic Exchange Resins. Sci. Rep. 2012, 2, 430. [Google Scholar] [CrossRef]
- Rajakumar, T.; Pugalendhi, P.; Thilagavathi, S. Dose Response Chemopreventive Potential of Allyl Isothiocyanate against 7,12-Dimethylbenz(a)Anthracene Induced Mammary Carcinogenesis in Female Sprague-Dawley Rats. Chem. Biol. Interact. 2015, 231, 35–43. [Google Scholar] [CrossRef]
- Lowry, O.H.; Rosebrough, N.J.; Farr, A.L.; Randall, R.J. Protein Measurement with the Folin Phenol Reagent. J. Biol. Chem. 1951, 193, 265–275. [Google Scholar] [CrossRef] [PubMed]
- Altenhofen, D.; da Luz, G.; Frederico, M.J.S.; Venzke, D.; Brich, M.; Vigil, S.; Fröde, T.S.; Linares, C.E.B.; Pizzolatti, M.G.; Silva, F.R.M.B. Bis-Pyrano Prenyl Isoflavone Improves Glucose Homeostasis by Inhibiting Dipeptidyl Peptidase-4 in Hyperglycemic Rats. J. Cell. Biochem. 2017, 118, 92–103. [Google Scholar] [CrossRef] [PubMed]
- Montanya, E.; Téllez, N. Pancreatic Remodeling: Beta-Cell Apoptosis, Proliferation and Neogenesis, and the Measurement of Beta-Cell Mass and of Individual Beta-Cell Size. Methods Mol. Biol. 2009, 560, 137–158. [Google Scholar] [CrossRef] [PubMed]
- Gomes Castro, A.J.; Silva Frederico, M.J.; Cazarolli, L.H.; Bretanha, L.C.; Tavares, L.D.C.; Buss, Z.D.S.; Dutra, M.F.; Pacheco De Souza, A.Z.; Pizzolatti, M.G.; Silva, F.R.M.B. Betulinic Acid and 1,25(OH)2 Vitamin D3 Share Intracellular Signal Transduction in Glucose Homeostasis in Soleus Muscle. Int. J. Biochem. Cell. Biol. 2014, 48, 18–27. [Google Scholar] [CrossRef]
- Lacy, P.E.; Kostianovsky, M. Method for the Isolation of Intact Islets of Langerhans from the Rat Pancreas. Diabetes 1967, 16, 35–39. [Google Scholar] [CrossRef]
- Horaguchi, A.; Merrell, R.C. Preparation of Viable Islet Cells from Dogs by a New Method. Diabetes 1981, 30, 455–458. [Google Scholar] [CrossRef][Green Version]
- Sołobodowska, S.; Giebułtowicz, J.; Wolinowska, R.; Wroczyński, P. Contribution of ALDH1A1 Isozyme to Detoxification of Aldehydes Present in Food Products. Acta. Pol. Pharm. 2012, 69, 1380–1383. [Google Scholar]
- Frederico, M.J.S.; Castro, A.J.G.; Menegaz, D.; Murat, C.D.B.; Mendes, C.P.; Mascarello, A.; Nunes, R.J.; Silva, F.R.M.B. Mechanism of Action of Novel Glibenclamide Derivatives on Potassium and Calcium Channels for Insulin Secretion. Curr. Drug. Targets 2017, 18, 641–650. [Google Scholar] [CrossRef]
- Krizanova, O.; Steliarova, I.; Csaderova, L.; Pastorek, M.; Hudecova, S. Capsaicin Induces Apoptosis in PC12 Cells through ER Stress. Oncol. Rep. 2014, 31, 581–588. [Google Scholar] [CrossRef]
- Takii, M.; Ishikawa, T.; Tsuda, H.; Kanatani, K.; Sunouchi, T.; Kaneko, Y.; Nakayama, K. Involvement of Stretch-Activated Cation Channels in Hypotonically Induced Insulin Secretion in Rat Pancreatic Beta-Cells. Am. J. Physiol. Cell. Physiol. 2006, 291, C1405–C1411. [Google Scholar] [CrossRef] [PubMed]
- Batra, S.; Sjögren, C. Effect of Estrogen Treatment on Calcium Uptake by the Rat Uterine Smooth Muscle. Life Sci. 1983, 32, 315–319. [Google Scholar] [CrossRef] [PubMed]


| Group | Incretinogenic Index (pM/mg) |
|---|---|
| Hyperglycemic (4 g/kg, i.p.) | 0.8393 |
| CIN (20 mg/kg, i.p.) | 1.1258 *** |
| AITC (10 mg/kg, i.p.) | 1.4306 *** |
| Group | Insulinogenic Index (ng/mg) |
|---|---|
| Hyperglycemic (4 g/kg, i.p.) | 0.4805 |
| CIN (20 mg/kg, i.p.) | 1.0250 *** |
| AITC (10 mg/kg, i.p.) | 1.1888 *** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Frederico, M.J.S.; Cipriani, A.; Heim, J.B.A.; Mendes, A.K.B.; Aragón, M.; Gaspar, J.M.; De Alencar, N.M.N.; Silva, F.R.M.B. Electrophilic Agonists Modulate the Transient Receptor Potential Ankyrin-1 Channels Mediated by Insulin and Glucagon-like Peptide-1 Secretion for Glucose Homeostasis. Pharmaceuticals 2023, 16, 1167. https://doi.org/10.3390/ph16081167
Frederico MJS, Cipriani A, Heim JBA, Mendes AKB, Aragón M, Gaspar JM, De Alencar NMN, Silva FRMB. Electrophilic Agonists Modulate the Transient Receptor Potential Ankyrin-1 Channels Mediated by Insulin and Glucagon-like Peptide-1 Secretion for Glucose Homeostasis. Pharmaceuticals. 2023; 16(8):1167. https://doi.org/10.3390/ph16081167
Chicago/Turabian StyleFrederico, Marisa Jadna Silva, Andreza Cipriani, Jocelyn Brice Alexandre Heim, Ana Karla Bittencourt Mendes, Marcela Aragón, Joana Margarida Gaspar, Nylane Maria Nunes De Alencar, and Fátima Regina Mena Barreto Silva. 2023. "Electrophilic Agonists Modulate the Transient Receptor Potential Ankyrin-1 Channels Mediated by Insulin and Glucagon-like Peptide-1 Secretion for Glucose Homeostasis" Pharmaceuticals 16, no. 8: 1167. https://doi.org/10.3390/ph16081167
APA StyleFrederico, M. J. S., Cipriani, A., Heim, J. B. A., Mendes, A. K. B., Aragón, M., Gaspar, J. M., De Alencar, N. M. N., & Silva, F. R. M. B. (2023). Electrophilic Agonists Modulate the Transient Receptor Potential Ankyrin-1 Channels Mediated by Insulin and Glucagon-like Peptide-1 Secretion for Glucose Homeostasis. Pharmaceuticals, 16(8), 1167. https://doi.org/10.3390/ph16081167







