Identification of Drug Targets and Their Inhibitors in Yersinia pestis Strain 91001 through Subtractive Genomics, Machine Learning, and MD Simulation Approaches
Abstract
1. Introduction
2. Results and Discussion
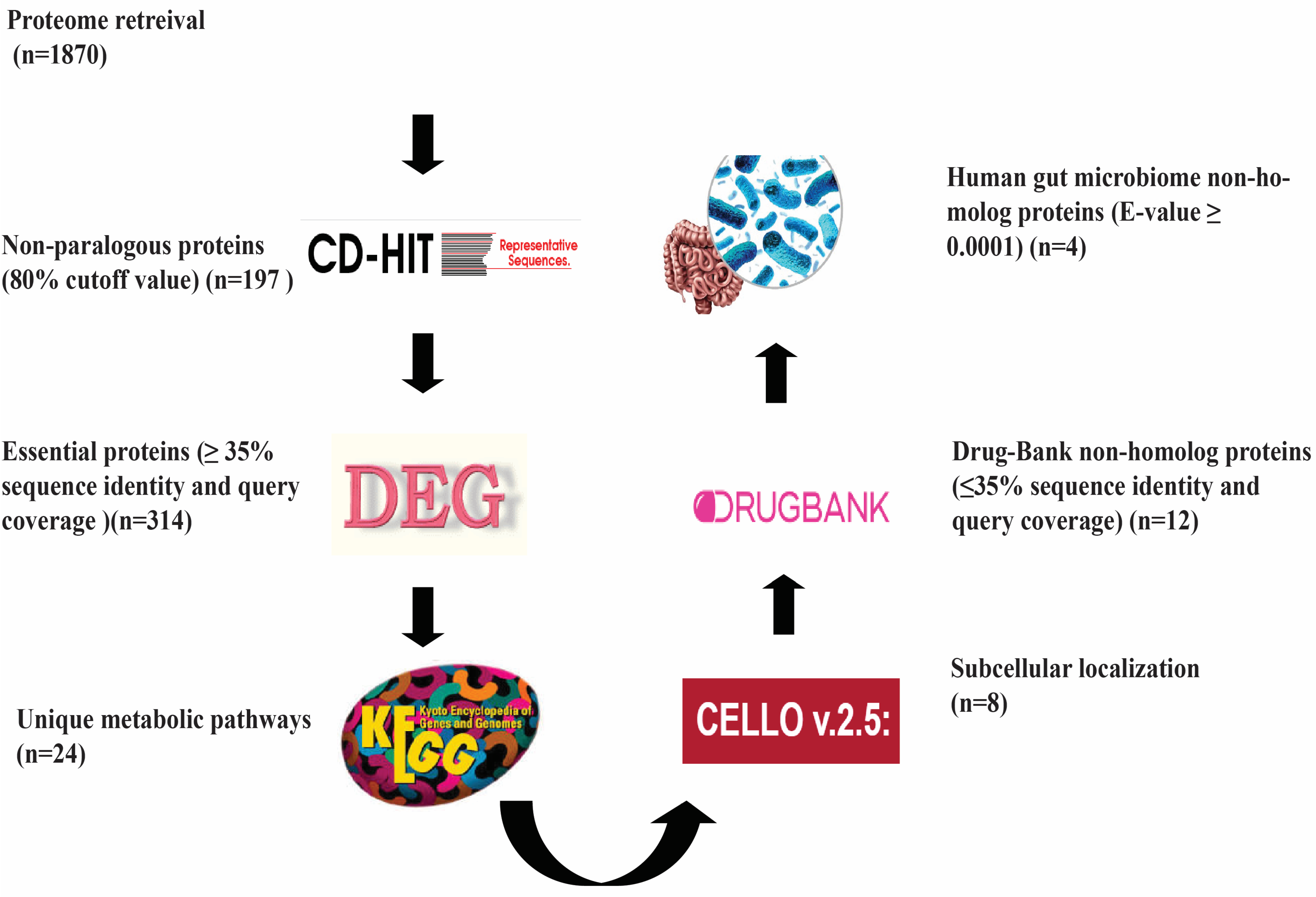
2.1. Subtractive Genomics
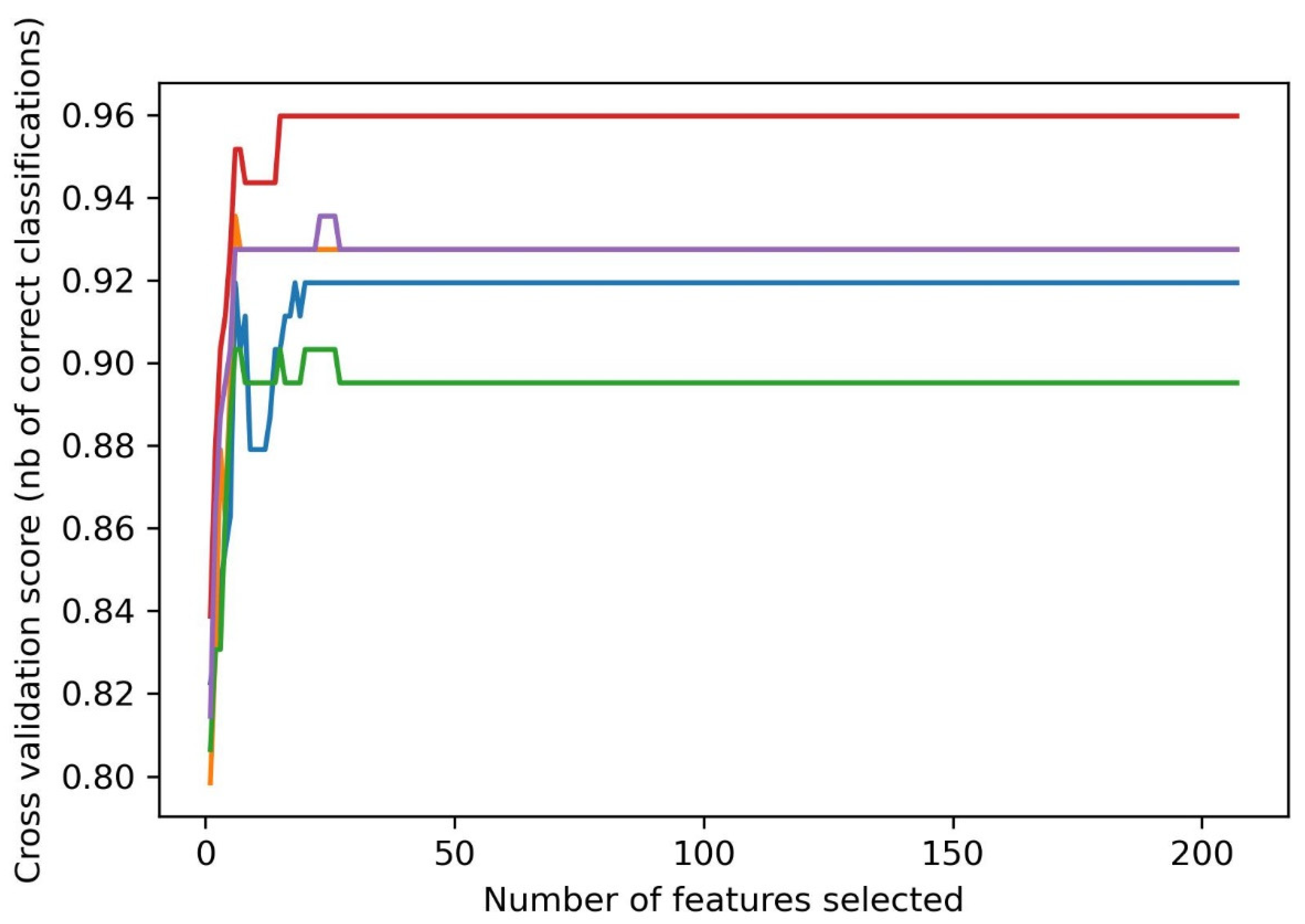
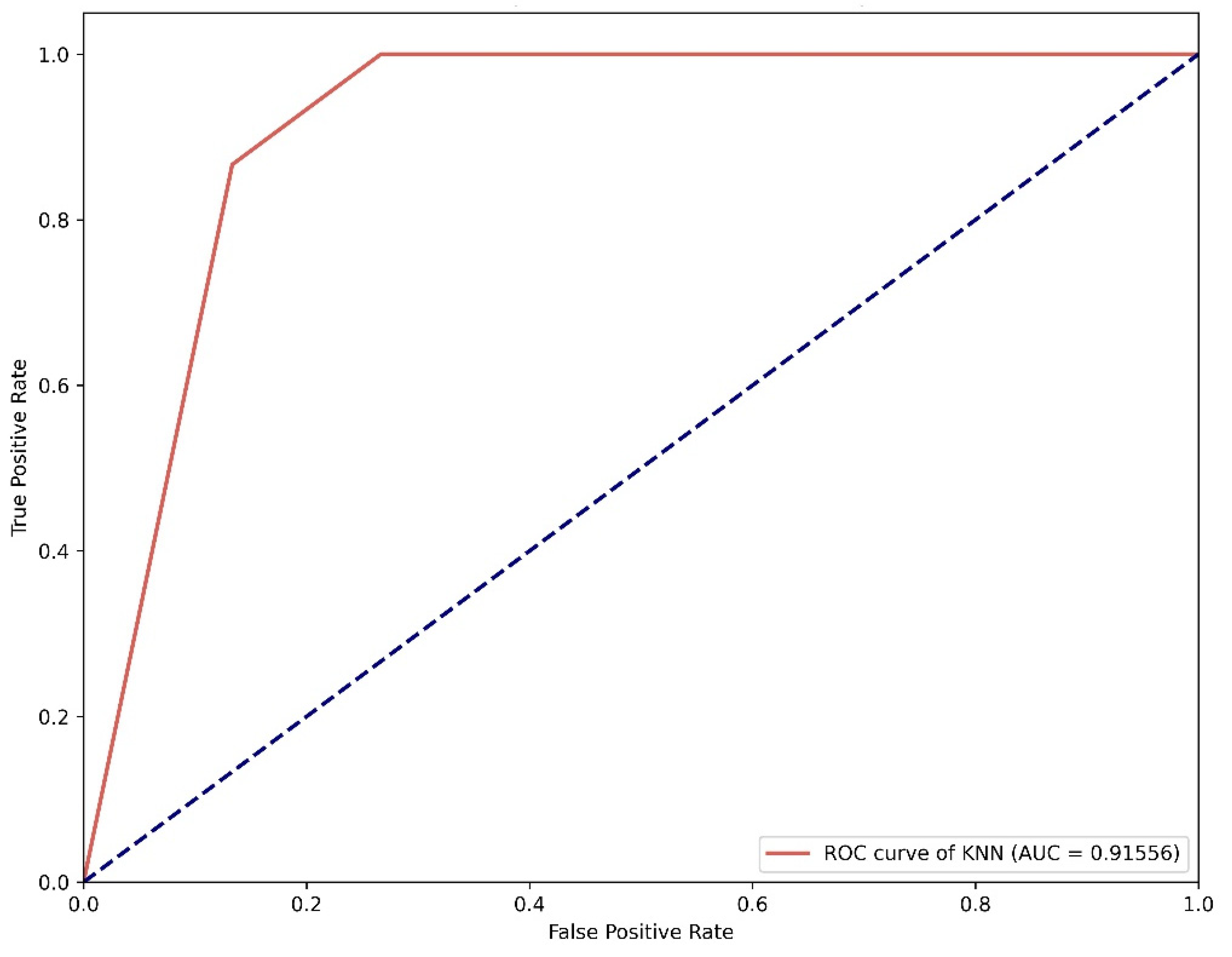
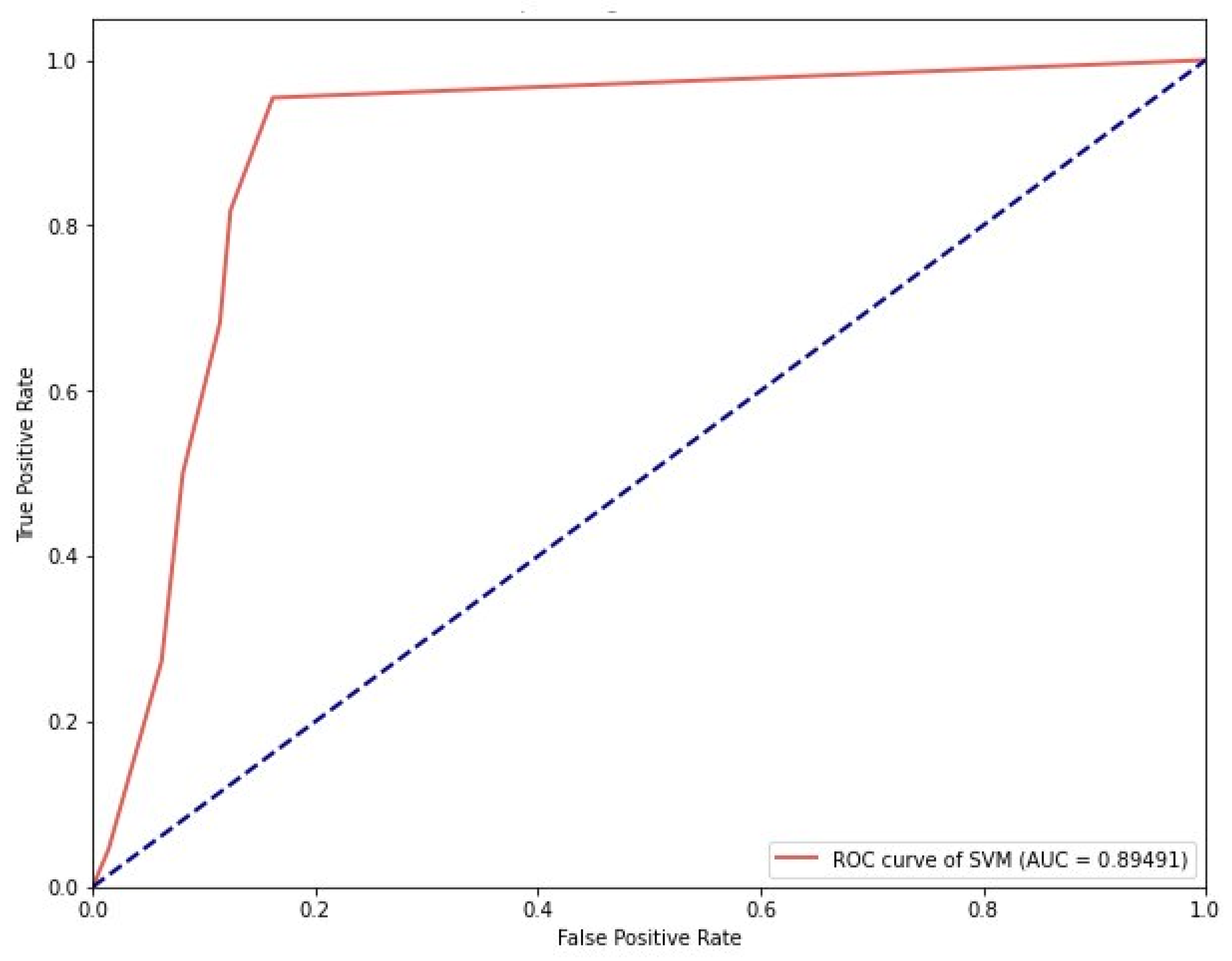
2.2. Machine Learning-Based Virtual Screening
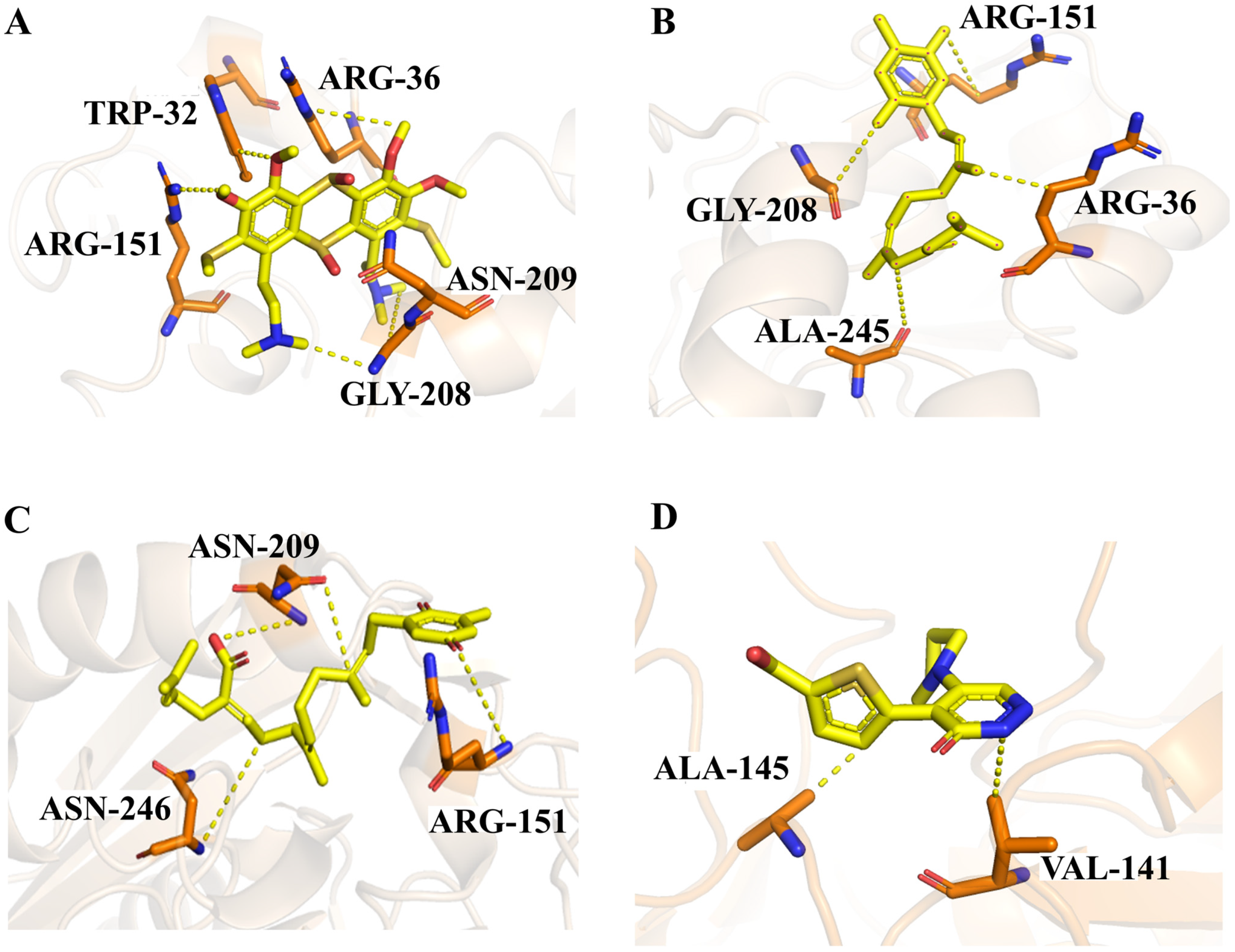
2.3. Docking Analysis
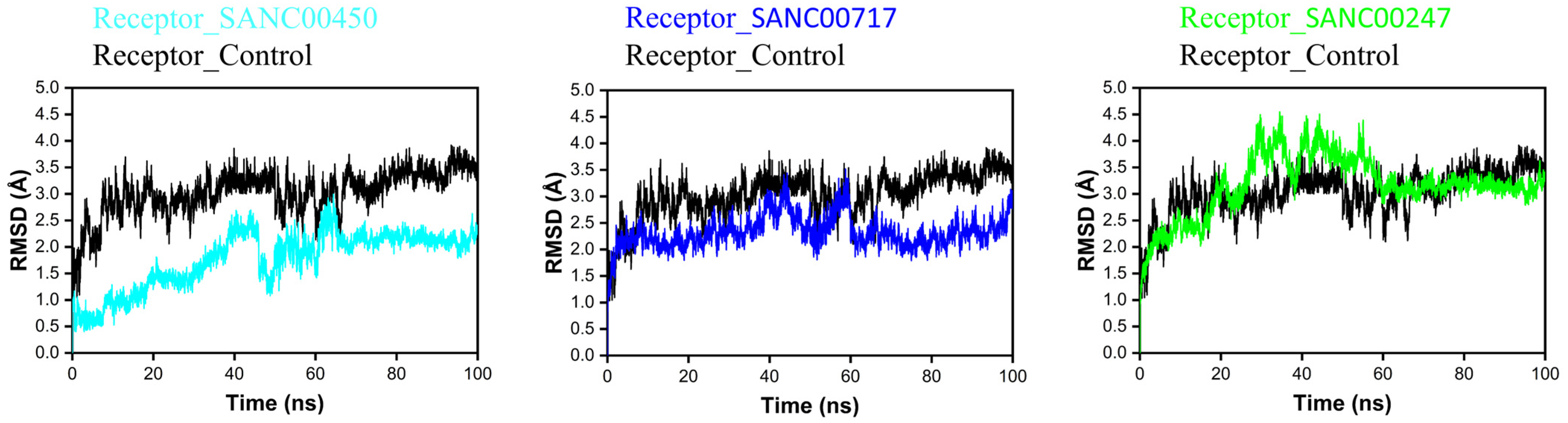
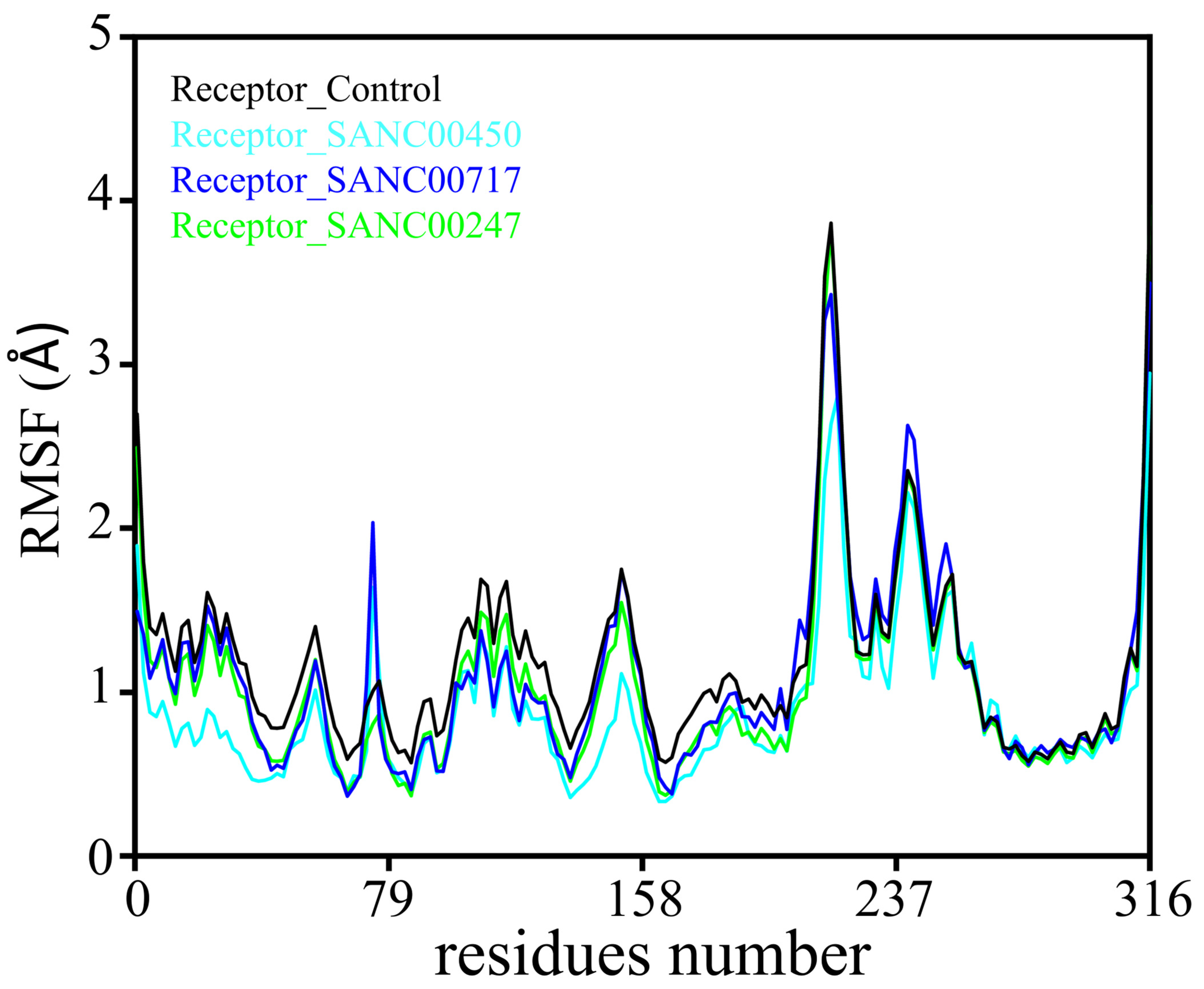
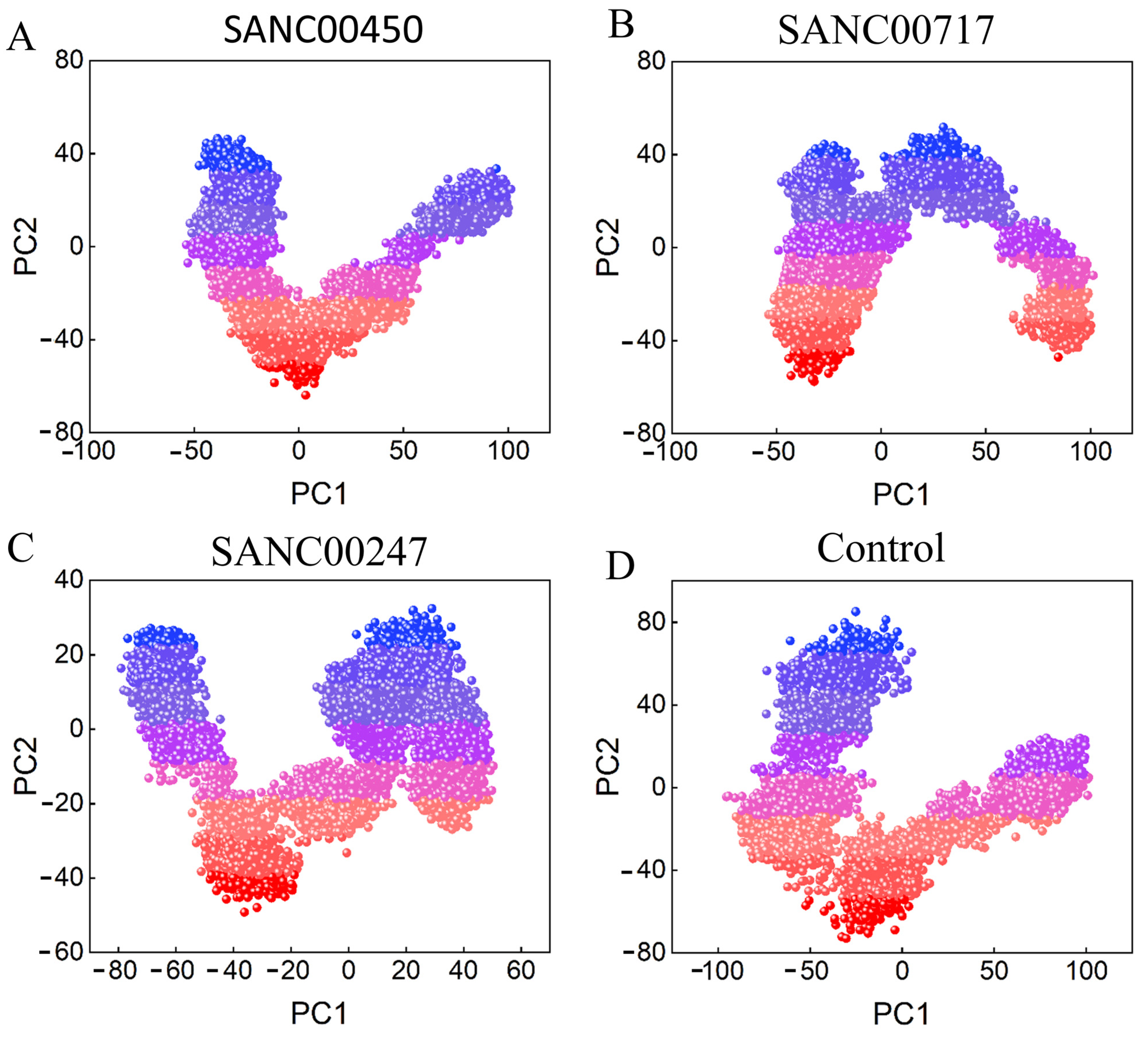
2.4. Post Simulation Analysis
2.4.1. RMSD Analysis
2.4.2. RMSF Analysis
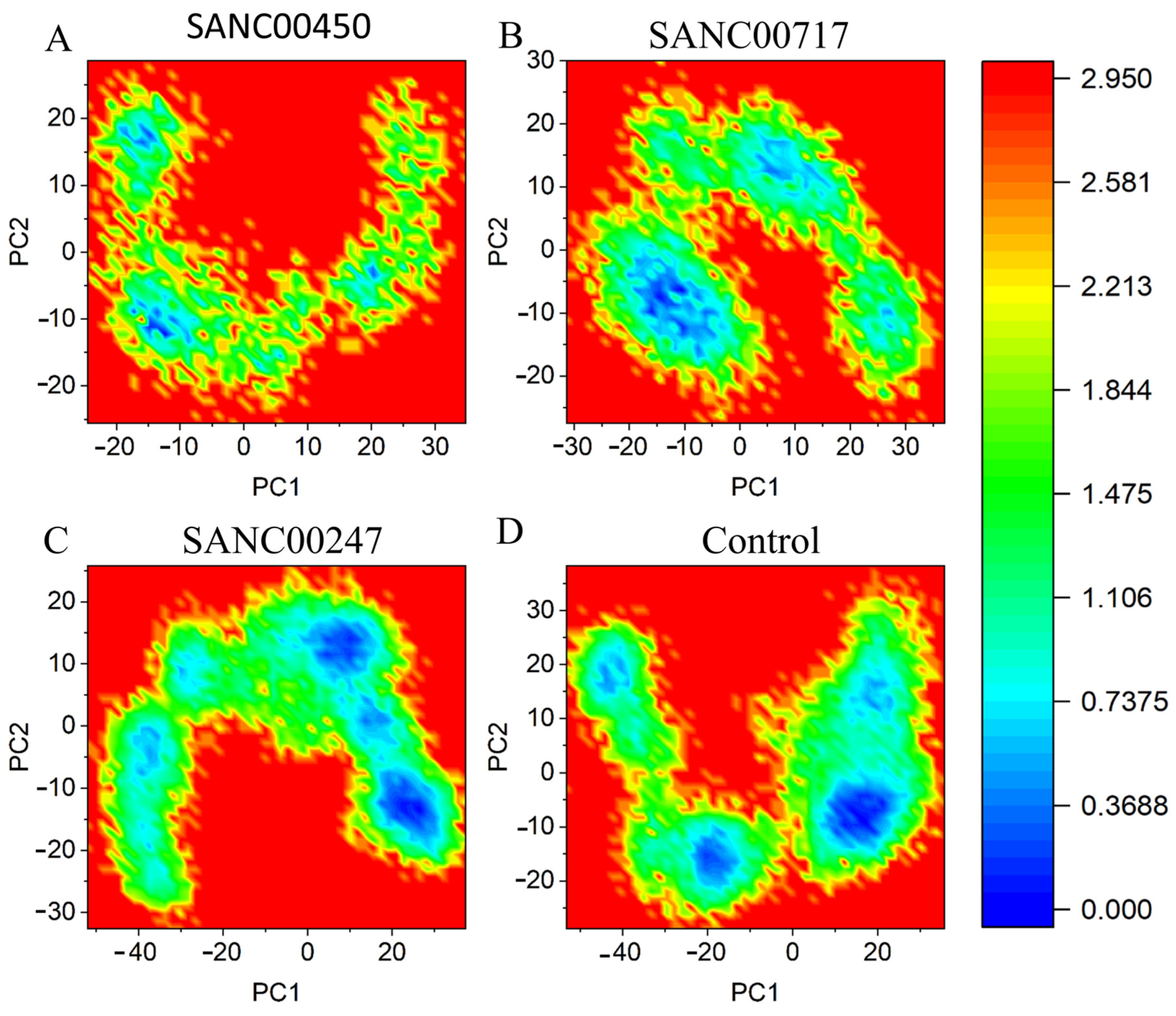
2.4.3. Principal Component Analysis and Free Energy Landscape
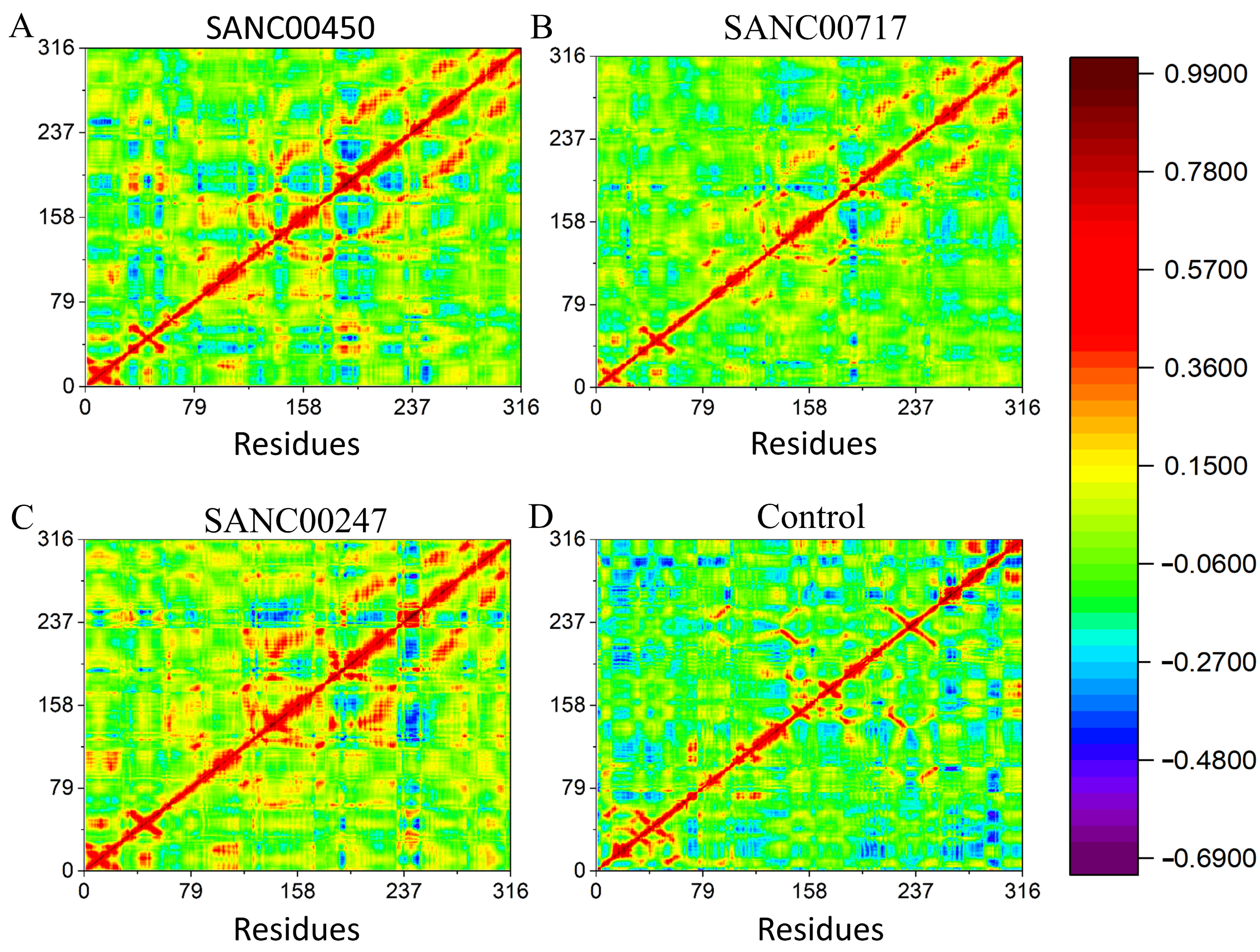
2.4.4. Dynamics Cross Correlation Matrix (DCCM)
3. Materials and Methods
3.1. Pathogen Proteome Retrieval
3.2. Paralogs Proteins Identification
3.3. Human Non-Homologous Proteins Identification
3.4. Finding Essential Genes
3.5. Pathways Analysis
3.6. Proteins Localization Prediction
3.7. Virulent Proteins Identification
3.8. Druggability Analysis of Shortlisted Proteins
3.9. Analysis of Non-Gut Flora Proteins
3.10. Machine Learning-Based Approaches for Virtual Screening
3.10.1. Dataset Preparation
3.10.2. K-Nearest Neighbor (KNN)
3.10.3. Support Vector Machine (SVM)
3.10.4. Model Validation
3.10.5. Virtual Screening and Molecular Docking
3.11. MD Simulation
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chaaban, T.; Mohsen, Y.; Ezzeddine, Z.; Ghssein, G. Overview of Yersinia pestis Metallophores: Yersiniabactin and Yersinopine. Biology 2023, 12, 598. [Google Scholar] [CrossRef]
- Demeure, C.E.; Dussurget, O.; Mas Fiol, G.; Le Guern, A.-S.; Savin, C.; Pizarro-Cerdá, J. Yersinia pestis and plague: An updated view on evolution, virulence determinants, immune subversion, vaccination, and diagnostics. Genes Immun. 2019, 20, 357–370. [Google Scholar] [CrossRef]
- Anisimov, A.P.; Amoako, K.K. Treatment of plague: Promising alternatives to antibiotics. J. Med. Microbiol. 2006, 55, 1461–1475. [Google Scholar] [CrossRef]
- Yang, R. Plague: Recognition, treatment, and prevention. J. Clin. Microbiol. 2018, 56, e01519-17. [Google Scholar] [CrossRef]
- Sebbane, F.; Jarrett, C.O.; Gardner, D.; Long, D.; Hinnebusch, B. Role of the Yersinia pestis plasminogen activator in the incidence of distinct septicemic and bubonic forms of flea-borne plague. Proc. Natl. Acad. Sci. USA 2006, 103, 5526–5530. [Google Scholar] [CrossRef]
- Miesel, L.; Greene, J.; Black, T.A. Genetic strategies for antibacterial drug discovery. Nat. Rev. Genet. 2003, 4, 442–456. [Google Scholar] [CrossRef]
- Plotkin, S.A. Vaccines: Past, present and future. Nat. Med. 2005, 11, S5–S11. [Google Scholar] [CrossRef]
- Mondal, S.I.; Ferdous, S.; Jewel, N.A.; Akter, A.; Mahmud, Z.; Islam, M.M.; Afrin, T.; Karim, N.J.A. Identification of potential drug targets by subtractive genome analysis of Escherichia coli O157:H7: An in silico approach. Adv. Appl. Bioinform. Chem. 2015, 8, 49–63. [Google Scholar] [CrossRef]
- Ghssein, G.; Matar, S.F. Chelating mechanisms of transition metals by bacterial metallophores “pseudopaline and staphylopine”: A quantum chemical assessment. Computation 2018, 6, 56. [Google Scholar] [CrossRef]
- Maurya, R.; Pandey, A.K. Importance of protozoa Tetrahymena in toxicological studies: A review. Sci. Total Environ. 2020, 741, 140058. [Google Scholar] [CrossRef]
- Parkhill, J.; Wren, B.; Thomson, N.; Titball, R.; Holden, M.; Prentice, M.; Sebaihia, M.; James, K.; Churcher, C.; Mungall, K.L.; et al. Genome sequence of Yersinia pestis, the causative agent of plague. Nature 2001, 413, 523–527. [Google Scholar] [CrossRef]
- Huang, Y.; Niu, B.; Gao, Y.; Fu, L.; Li, W. CD-HIT Suite: A web server for clustering and comparing biological sequences. Bioinformatics 2010, 26, 680–682. [Google Scholar] [CrossRef]
- Zhang, R.; Ou, H.Y.; Zhang, C.T. DEG: A database of essential genes. Nucleic Acids Res. 2004, 32, D271–D272. [Google Scholar] [CrossRef]
- Hossain, M.; Mosnaz, A.; Sajib, A.M.; Roy, P.K.; Shakil, S.K.; Ullah, S.; Prodhan, S.H. Biotechnology. Identification of putative drug targets of Listeria monocytogenes F2365 by subtractive genomics approach. J. BioSci. Biotechnol. 2013, 2, 63–71. [Google Scholar]
- Barh, D.; Tiwari, S.; Jain, N.; Ali, A.; Santos, A.R.; Misra, A.N.; Azevedo, V.; Kumar, A. In silico subtractive genomics for target identification in human bacterial pathogens. Drug Dev. Res. 2011, 72, 162–177. [Google Scholar] [CrossRef]
- Yu, C.S.; Chen, Y.C.; Lu, C.H.; Hwang, J.K. Prediction of protein subcellular localization. Proteins: Struct. Funct. Bioinform. 2006, 64, 643–651. [Google Scholar] [CrossRef]
- Fujimura, K.E.; Slusher, N.A.; Cabana, M.D.; Lynch, S.V. Role of the gut microbiota in defining human health. Expert Rev. Anti-Infect. Ther. 2010, 8, 435–454. [Google Scholar] [CrossRef]
- Hamm, C.A.; Costa, F.F. Epigenomes as therapeutic targets. Pharmacol. Ther. 2015, 151, 72–86. [Google Scholar] [CrossRef]
- Korkmaz, S.; Zararsiz, G.; Goksuluk, D. MLViS: A web tool for machine learning-based virtual screening in early-phase of drug discovery and development. PLoS ONE 2015, 10, e0124600. [Google Scholar] [CrossRef]
- Cai, C.; Wu, Q.; Luo, Y.; Ma, H.; Shen, J.; Zhang, Y.; Yang, L.; Chen, Y.; Wen, Z.; Wang, Q. In silico prediction of ROCK II inhibitors by different classification approaches. Mol. Divers. 2017, 21, 791–807. [Google Scholar] [CrossRef]
- Islam, M.M.; Karray, F.; Alhajj, R.; Zeng, J. A review on deep learning techniques for the diagnosis of novel coronavirus (COVID-19). IEEE Access 2021, 9, 30551–30572. [Google Scholar] [CrossRef] [PubMed]
- Wadood, A.; Ajmal, A.; Junaid, M.; Rehman, A.U.; Uddin, R.; Azam, S.S.; Khan, A.Z.; Ali, A. Machine Learning-based Virtual Screening for STAT3 Anticancer Drug Target. Curr. Pharm. Des. 2022, 28, 3023–3032. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Kolcz, A. Large-scale machine learning at twitter. In Proceedings of the 2012 ACM SIGMOD International Conference on Management of Data, Scottsdale, AZ, USA, 20–24 May 2022; pp. 793–804.
- Sethi, A.; Joshi, K.; Sasikala, K.; Alvala, M. Molecular docking in modern drug discovery: Principles and recent applications. Drug Discov. Dev. -New Adv. 2019, 2, 1–21. [Google Scholar]
- He, X.; Reeve, A.M.; Desai, U.R.; Kellogg, G.E.; Reynolds, K.A. 1, 2-dithiole-3-ones as potent inhibitors of the bacterial 3-ketoacyl acyl carrier protein synthase III (FabH). Antimicrob. Agents Chemother. 2004, 48, 3093–3102. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.; Randhawa, A.W.; Balouch, A.R.; Mukhtar, N.; Sayaf, A.M.; Suleman, M.; Khan, T.; Ali, S.; Ali, S.S.; Wang, Y. Blocking key mutated hotspot residues in the RBD of the omicron variant (B. 1.1. 529) with medicinal compounds to disrupt the RBD-hACE2 complex using molecular screening and simulation approaches. RSC Adv. 2022, 12, 7318–7327. [Google Scholar] [CrossRef]
- Wei-Ya, L.; Yu-Qing, D.; Yang-Chun, M.; Xin-Hua, L.; Ying, M.; Wang, R.-L.J. Exploring the cause of the inhibitor 4AX attaching to binding site disrupting protein tyrosine phosphatase 4A1 trimerization by molecular dynamic simulation. J. Biomol. Struct. Dyn. 2019, 37, 4840–4851. [Google Scholar] [CrossRef]
- Hasan, M.A.; Khan, M.A.; Sharmin, T.; Mazumder, M.H.H.; Chowdhury, A.S. Identification of putative drug targets in Vancomycin-resistant Staphylococcus aureus (VRSA) using computer aided protein data analysis. Gene 2016, 575, 132–143. [Google Scholar] [CrossRef]
- Gupta, R.; Verma, R.; Pradhan, D.; Jain, A.K.; Umamaheswari, A.; Rai, C.S. An in silico approach towards identification of novel drug targets in pathogenic species of Leptospira. PLoS ONE 2019, 14, e0221446. [Google Scholar] [CrossRef]
- Ahmad, S.; Raza, S.; Uddin, R.; Azam, S.S.J. Comparative subtractive proteomics based ranking for antibiotic targets against the dirtiest superbug: Acinetobacter baumannii. J. Mol. Graph. Model. 2018, 82, 74–92. [Google Scholar] [CrossRef]
- Moriya, Y.; Itoh, M.; Okuda, S.; Yoshizawa, A.C.; Kanehisa, M. KAAS: An automatic genome annotation and pathway reconstruction server. Nucleic Acids Res. 2007, 35, W182–W185. [Google Scholar] [CrossRef]
- Chen, L.; Xiong, Z.; Sun, L.; Yang, J.; Jin, Q. VFDB 2012 update: Toward the genetic diversity and molecular evolution of bacterial virulence factors. Nucleic Acids Res. 2012, 40, D641–D645. [Google Scholar] [CrossRef] [PubMed]
- Knox, C.; Law, V.; Jewison, T.; Liu, P.; Ly, S.; Frolkis, A.; Pon, A.; Banco, K.; Mak, C.; Neveu, V. DrugBank 3.0: A comprehensive resource for ‘omics’ research on drugs. Nucleic Acids Res. 2010, 39, D1035–D1041. [Google Scholar] [CrossRef] [PubMed]
- Rabizadeh, S.; Sears, C. New horizons for the infectious diseases specialist: How gut microflora promote health and disease. Curr. Infect. Dis. Rep. 2008, 10, 92–98. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Willing, B.P.; Russell, S.L.; Finlay, B.B. Shifting the balance: Antibiotic effects on host–microbiota mutualism. Nat. Rev. Genet. 2011, 9, 233–243. [Google Scholar] [CrossRef] [PubMed]
- Kuldeep, J.; Sharma, S.K.; Sharma, T.; Singh, B.N.; Siddiqi, M.I. Targeting Mycobacterium Tuberculosis Enoyl-Acyl Carrier Protein Reductase Using Computational Tools for Identification of Potential Inhibitor and their Biological Activity. Mol. Inform. 2021, 40, 2000211. [Google Scholar] [CrossRef] [PubMed]
- Samad, A.; Ajmal, A.; Mahmood, A.; Khurshid, B.; Li, P.; Jan, S.M.; Rehman, A.U.; He, P.; Abdalla, A.N.; Umair, M. Identification of novel inhibitors for SARS-CoV-2 as therapeutic options using machine learning-based virtual screening, molecular docking and MD simulation. Front. Mol. Biosci. 2023, 10, 1060076. [Google Scholar] [CrossRef]
- Cover, T.; Hart, P. Nearest neighbor pattern classification. IEEE Trans. Inf. Theory 1967, 13, 21–27. [Google Scholar] [CrossRef]
- Inayat, N.; Khan, M.; Iqbal, N.; Khan, S.; Raza, M.; Khan, D.M.; Khan, A.; Wei, D.Q. iEnhancer-DHF: Identification of enhancers and their strengths using optimize deep neural network with multiple features extraction methods. IEEE Access 2021, 9, 40783–40796. [Google Scholar] [CrossRef]
- Diallo, B.; Glenister, M.; Musyoka, T.M.; Lobb, K.; Tastan Bishop, Ö.J. SANCDB: An update on South African natural compounds and their readily available analogs. J. Cheminform. 2021, 13, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Attique, S.A.; Hassan, M.; Usman, M.; Atif, R.M.; Mahboob, S.; Al-Ghanim, K.A.; Bilal, M.; Nawaz, M.Z. A molecular docking approach to evaluate the pharmacological properties of natural and synthetic treatment candidates for use against hypertension. Int. J. Environ. Res. Public Health 2019, 16, 923. [Google Scholar] [CrossRef] [PubMed]
- Rahman, N.; Ajmal, A.; Ali, F.; Rastrelli, L. Core proteome mediated therapeutic target mining and multi-epitope vaccine design for Helicobacter pylori. Genomics 2020, 112, 3473–3483. [Google Scholar] [CrossRef] [PubMed]
- Choudhary, S.; Kesavan, A.K.; Juneja, V.; Thakur, S. Molecular modeling, simulation and docking of Rv1250 protein from Mycobacterium tuberculosis. Front. Bioinform. 2023, 3, 1125479. [Google Scholar] [CrossRef]
- Ullah, A.; Shah, A.A.; Syed, F.; Mahmood, A.; Ur Rehman, H.; Khurshid, B.; Samad, A.; Ahmad, W.; Basit, S. Molecular Dynamic Simulation Analysis of a Novel Missense Variant in CYB5R3 Gene in Patients with Methemoglobinemia. Medicina 2023, 59, 379. [Google Scholar] [CrossRef] [PubMed]
- Singh, M.B.; Sharma, R.; Kumar, D.; Khanna, P.; Khanna, L.; Kumar, V.; Kumari, K.; Gupta, A.; Chaudhary, P.; Kaushik, N.J.; et al. An understanding of coronavirus and exploring the molecular dynamics simulations to find promising candidates against the Mpro of nCoV to combat the COVID-19: A systematic review. J. Infect. Public Health 2022, 15, 1326–1349. [Google Scholar] [CrossRef] [PubMed]


| S. No | Pathway ID | Pathway Name |
|---|---|---|
| 1 | ypm00281 | Geraniol degradation |
| 2 | ypm00332 | Carbapenem biosynthesis |
| 3 | ypm00361 | Chlorocyclohexane and chlorobenzene degradation |
| 4 | ypm00362 | Benzoate degradation |
| 5 | ypm00364 | Fluorobenzoate degradation |
| 6 | ypm00401 | Novobiocin biosynthesis |
| 7 | ypm00540 | Lipopolysaccharide biosynthesis |
| 8 | ypm00550 | Peptidoglycan biosynthesis |
| 9 | ypm00623 | Toluene degradation |
| 10 | ypm00625 | Chloroalkane and chloroalkene degradation |
| 11 | ypm00626 | Naphthalene degradation |
| 12 | ypm00633 | Nitrotoluene degradation |
| 13 | ypm00930 | Caprolactam degradation |
| 14 | ypm01054 | Nonribosomal peptide structures |
| 15 | ypm01120 | Microbial metabolism in diverse environments |
| 16 | ypm01501 | Vancomycin resistance |
| 17 | ypm01503 | Cationic antimicrobial peptide (CAMP) resistance |
| 18 | ypm05135 | Yersinia infection |
| 19 | ypm03070 | Bacterial secretion system |
| 20 | ypm02020 | Two-component system |
| 21 | ypm02040 | Flagellar assembly |
| 22 | ypm02024 | Quorum sensing |
| 23 | ypm02030 | Bacterial chemotaxis |
| 24 | ypm02060 | Phosphotransferase system (PTS) |
| S. No | Accession No | KO Code | Pathway Name |
|---|---|---|---|
| 1 | WP_002208960.1 | K02988 | Bacterial chemotaxis |
| 2 | WP_002211667.1 | K03070 | Bacterial secretion system |
| 3 | WP_002224818.1 | K07658 | Quorum sensing |
| 4 | WP_002230619.1 | K00349 | Yersinia infection |
| 5 | WP_002211580.1 | K03789 | Vancomycin resistance |
| 6 | WP_002209578.1 | K01736 | Peptidoglycan biosynthesis |
| 7 | WP_002213325.1 | K06958 | Quorum sensing |
| 8 | WP_002213337.1 | K13497 | Flagellar assembly |
| 9 | WP_002222284.1 | K09014 | Two-component system |
| 10 | WP_002218949.1 | K11216 | Bacterial chemotaxis |
| 11 | WP_011906295.1 | K03592 | Two-component system |
| 12 | WP_002213082.1 | K03634 | Quorum sensing |
| 13 | WP_002211073.1 | K01826 | Phosphotransferase system (PTS) |
| 14 | WP_002210412.1 | K19775 | Phosphotransferase system (PTS) |
| 15 | WP_002209326.1 | K03807 | Vancomycin resistance |
| 16 | WP_002211370.1 | K09998 | Vancomycin resistance |
| S. No | Accession No | Drugbank Target | Drugbank ID | Localization |
|---|---|---|---|---|
| 1 | WP_002208960.1 | drugbank_target|P1588040S ribosomal protein S2 | DB09130 | Cytoplasmic |
| 2 | WP_002211667.1 | drugbank_target|P27695 DNA-(apurinic or apyrimidinic site) lyase | DB04967 | Cytoplasmic |
| 3 | WP_002224818.1 | drugbank_target|P13632 C4-dicarboxylate transport transcriptional regulatory protein DctD | DB09462 | InnerMembrane |
| 4 | WP_002230619.1 | drugbank_target|Q9WXS0 Transcriptional regulator, IclR family | DB01942 | Periplasmic |
| 5 | WP_002211580.1 | drugbank_target|O14786 Neuropilin-1 | DB00039 DB04895 | InnerMembrane |
| 6 | WP_002209578.1 | drugbank_target|Q52369 Cytochrome c4 | DB03754 DB09462 | InnerMembrane |
| 7 | WP_002213325.1 | drugbank_target|P52758 Ribonuclease UK114 | DB03793 | Cytoplasmic |
| 8 | WP_002213337.1 | drugbank_target|P0ACQ4 Hydrogen peroxide-inducible genes activator | DB03793 | Cytoplasmic |
| 9 | WP_002222284.1 | drugbank_target|P06971 Ferrichrome-iron receptor | DB03017 DB04160 | Cytoplasmic |
| 10 | WP_002218949.1 | drugbank_target|P12996 Biotin synthase | DB03754 | Cytoplasmic |
| 11 | WP_011906295.1 | drugbank_target|P13632 C4-dicarboxylate transport transcriptional regulatory protein DctD | DB09462 | Cytoplasmic |
| 12 | WP_002213082.1 | drugbank_target|P9WKE1 Thymidylate kinase | DB04160 | Cytoplasmic |
| S. No | Accession No | Similarity with Gut Flora |
|---|---|---|
| 1 | WP_002208960.1 | No |
| 2 | WP_002211667.1 | No |
| 3 | WP_002213325.1 | Yes |
| 4 | WP_002213337.1 | Yes |
| 5 | WP_002222284.1 | No |
| 6 | WP_002218949.1 | Yes |
| 7 | WP_011906295.1 | No |
| 8 | WP_002213082.1 | Yes |
| Model | Accuracy | ROC-AUC Score | F1 | MCC |
|---|---|---|---|---|
| KNN | 97% | 0.91 | 0.98 | 0.97 |
| SVM | 83% | 0.89 | 0.78 | 0.65 |
| Compound ID | Structure | Docking Score |
|---|---|---|
| SANC00450 | 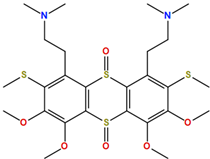 | −7.40 |
| SANC00717 | 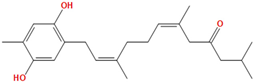 | −7.01 |
| SANC00247 | 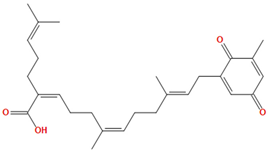 | −6.54 |
| SANC00269 | 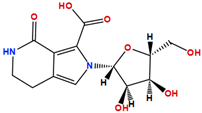 | −6.50 |
| SANC00451 | 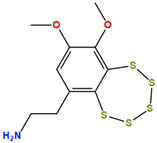 | −6.20 |
| SANC00728 | 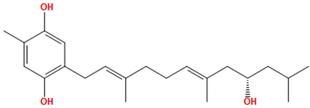 | −6.14 |
| SANC00258 | 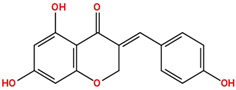 | −5.64 |
| SANC00735 | 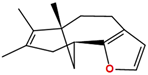 | −4.38 |
| SANC01025 | 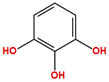 | −4.08 |
| SANC01023 | 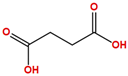 | −4.04 |
| SANC00129 | 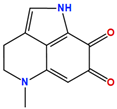 | −5.24 |
| 4,5-dichloro-1,2-dithiole-3 | 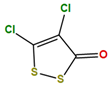 | −5.20 |
| Compound ID | Weight | H-Donor | H-Acceptor | Logp | Toxicity |
|---|---|---|---|---|---|
| SANC00450 | 602.86 | 0 | 6 | 3.90 | No |
| SANC00717 | 340.49 | 2 | 3 | 5.84 | No |
| SANC00247 | 424.58 | 1 | 4 | 7.86 | No |
| SANC00269 | 312.28 | 5 | 7 | 1.10 | No |
| SANC00451 | 339.55 | 1 | 3 | 2.03 | No |
| SANC00728 | 346.51 | 3 | 3 | 5.0 | No |
| SANC00258 | 284.27 | 3 | 5 | 2.47 | No |
| SANC00735 | 216.32 | 0 | 0 | 4.12 | No |
| SANC01025 | 125.11 | 3 | 3 | 0.35 | No |
| SANC01023 | 118.09 | 2 | 4 | -0.77 | No |
| SANC00129 | 202.21 | 1 | 2 | 1.32 | No |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ali, H.; Samad, A.; Ajmal, A.; Ali, A.; Ali, I.; Danial, M.; Kamal, M.; Ullah, M.; Ullah, R.; Kalim, M. Identification of Drug Targets and Their Inhibitors in Yersinia pestis Strain 91001 through Subtractive Genomics, Machine Learning, and MD Simulation Approaches. Pharmaceuticals 2023, 16, 1124. https://doi.org/10.3390/ph16081124
Ali H, Samad A, Ajmal A, Ali A, Ali I, Danial M, Kamal M, Ullah M, Ullah R, Kalim M. Identification of Drug Targets and Their Inhibitors in Yersinia pestis Strain 91001 through Subtractive Genomics, Machine Learning, and MD Simulation Approaches. Pharmaceuticals. 2023; 16(8):1124. https://doi.org/10.3390/ph16081124
Chicago/Turabian StyleAli, Hamid, Abdus Samad, Amar Ajmal, Amjad Ali, Ijaz Ali, Muhammad Danial, Masroor Kamal, Midrar Ullah, Riaz Ullah, and Muhammad Kalim. 2023. "Identification of Drug Targets and Their Inhibitors in Yersinia pestis Strain 91001 through Subtractive Genomics, Machine Learning, and MD Simulation Approaches" Pharmaceuticals 16, no. 8: 1124. https://doi.org/10.3390/ph16081124
APA StyleAli, H., Samad, A., Ajmal, A., Ali, A., Ali, I., Danial, M., Kamal, M., Ullah, M., Ullah, R., & Kalim, M. (2023). Identification of Drug Targets and Their Inhibitors in Yersinia pestis Strain 91001 through Subtractive Genomics, Machine Learning, and MD Simulation Approaches. Pharmaceuticals, 16(8), 1124. https://doi.org/10.3390/ph16081124





