Effects of Metformin on Ischemia/Reperfusion Injury: New Evidence and Mechanisms
Abstract
1. Introduction
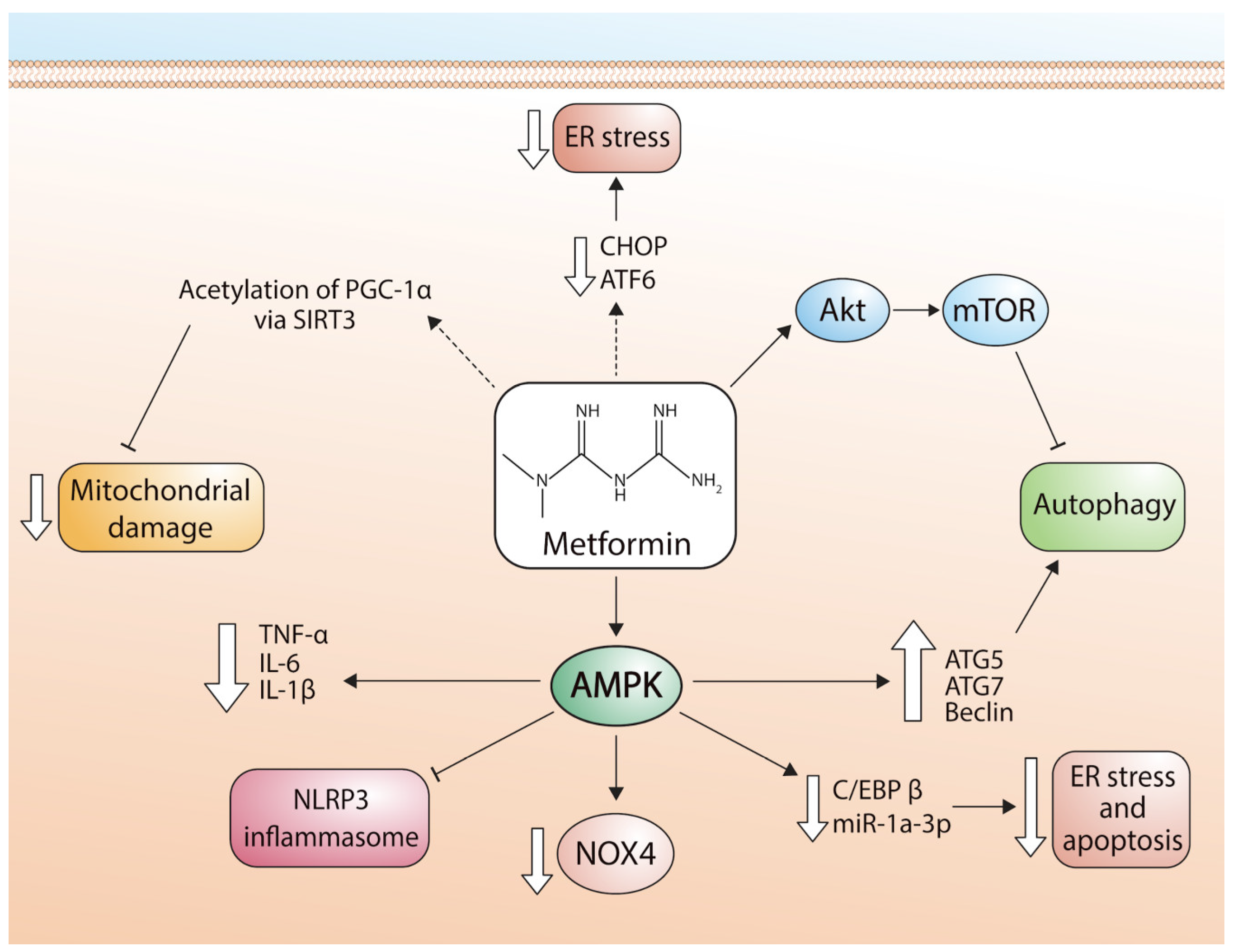
2. Metformin
3. Classical Effects of Metformin
4. Myocardial Ischemia/Reperfusion (I/R) Injury
5. Cardioprotective Effects of Metformin on Myocardial I/R
5.1. Cardioprotective Effects of Metformin via Inhibition of Apoptosis
5.2. Cardioprotective Effects of Metformin on I/R Injury via Modulation of ROS
5.3. Cardioprotective Effects of Metformin on I/R Injury via Autophagy
5.4. Cardioprotective Effects of Metformin via Mitochondrial Function
5.5. Effects of Metformin on Cardiac Function after I/R Injury
6. Clinical Trials
7. Perspectives and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ADP | Adenosine Diphosphate |
| AMP | Adenosine Monophosphate |
| AMPK | AMP-Activated Protein Kinase |
| ATG5 | Autophagy Related 5 |
| ATG7 | Autophagy Related 7 |
| ATP | Adenosine Triphosphate |
| CVD | Cardiovascular Diseases |
| DM | Diabetes Mellitus |
| eGFR | Estimated Glomerular Filtration Rates |
| HDL-cholesterol | High Density Lipoprotein—Cholesterol |
| HOMA-IR | Homeostatic Model Assessment of Insulin Resistance |
| hTERT | Telomerase Reverse Transcriptase—Human |
| I/R | Ischemia-Reperfusion |
| IL-1 | Interleukin 6 |
| IL-6 | Interleukin-6 |
| KLF2 | Krueppel-Like Factor 2 |
| LC3I | Light Chain 3 I |
| LC3-II | Light Chain 3 II |
| LDL-cholesterol | Low Density Lipoprotein Cholesterol |
| MMPs | Matrix Metalloproteinases |
| mtDNA | Mitochondrial DNA |
| mTOR | Mammalian Target Of Rapamycin |
| NADH | Reduced Nicotinamide Adenine Dinucleotide |
| NF-kB | Nuclear Factor-Κb |
| NLRP3 | NLR Family Pyrin Domain Containing 3 |
| NO | Nitric Oxide |
| NOX4 | NADPH Oxidase 4 |
| NRF-1 | Nuclear Respiratory Factor 1 |
| NRF-2 | Nuclear Respiratory Factor 2 |
| p62 | P62 Protein |
| PDK4 | Pyruvate Dehydrogenase Lipoamide Kinase Isozyme 4 |
| PGC-1α | Peroxisome Proliferator-Activated Receptor Γ Co-Activator 1 A |
| PI3K | Phosphatidylinositol-3-Kinase |
| RISK | Reperfusion Injury Salvage Kinase |
| ROS | Reactive Oxygen Species |
| SIRT-1 | Sirtuin 1 |
| SIRT3 | Sirtuin 3 |
| SQSTM1 | Sequestosome 1 |
| STAT 3 | Signal Transducer and Activator of Transcription 3 |
| TNF-α | Tumor Necrosis Factor Alpha |
| WHO | World Health Organization |
| mPTP | Mitochondrial permeability transition pore |
| MI | Myocardial infarction |
| CAD | Coronary artery disease |
| IL-6 | Interleukin 6 |
| BECLIN-1 | Beclin 1 Polyclonal Antibody |
| TSPO | Translocator Protein |
| ER | Endoplasmic reticulum |
| EF | Ejection fraction |
| LV | Left ventricular |
| LVEF | Left ventricular ejection fraction |
| C/EBP | CCAAT enhancer binding protein |
| β/miR-1a-3p/GRPQ4 | beta/miR-1a-3p/grpq4 |
| Akt | Protein kinase B |
References
- World Health Organization. Cardiovascular Diseases. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 3 January 2022).
- Pan American Health Organization. Cardiovascular Disease Burden. Available online: https://www.paho.org/en/enlace/cardiovascular-disease-burden (accessed on 3 January 2022).
- Khan, M.; Hashim, M.; Mustafa, H.; Baniyas, M.; Suwaidi, S.; Alkatheeri, R.; Alblooshi, F.; Almatrooshi, M.; Alzaabi, M.; Al Darmaki, R.S.; et al. Global Epidemiology of Ischemic Heart Disease: Results from the Global Burden of Disease Study. Cureus 2020, 12, 9349. [Google Scholar] [CrossRef]
- Kuznetsov, A.; Javadov, S.; Margreiter, R.; Grimm, M.; Hagenbuchner, J.; Ausserlechner, M. The Role of Mitochondria in the Mechanisms of Cardiac Ischemia-Reperfusion Injury. Antioxidants 2019, 8, 454. [Google Scholar] [CrossRef]
- Dunker, D.; Canty, J. Coronary Blood Flow and Myocardial Ischemia. In Braunwald´s Heart Disease, 12th ed.; Elseiver: Philadelphia, PA, USA, 2022. [Google Scholar]
- Henning, R. Obesity and obesity-induced inflammatory disease contribute to aterosclerosis: A review of the pathophysiology and treatment of obesity. Am. J. Cardiovasc. Dis. 2021, 11, 504–529. [Google Scholar] [PubMed]
- Hauet, T.; Pisani, D. New Strategies Protecting from Ischemia/Reperfusion. Int. J. Mol. Sci. 2022, 23, 15867. [Google Scholar] [CrossRef] [PubMed]
- Daiber, A.; Chlopicki, S. Revisiting pharmacology of oxidative stress and endotelial dysfunction in cardiovascular disease: Evidence for redox-based thrreapies. Free Radic. Biol. Med. 2020, 157, 15–37. [Google Scholar] [CrossRef] [PubMed]
- Steven, S.; Frenis, K.; Oelze, M.; Kalinovic, S.; Kuntic, M.; Bayo, M.; Vujacic-Mirski, K.; Helmstädter, J.; Kröller-Schön, S.; Münzel, T.; et al. Vascular Inflammation and Oxidativ Stress: Major Triggers for Cardiovascular Disease. Oxid. Med. Cell. Longev. 2019, 2019, 7092151. [Google Scholar] [CrossRef]
- Ridker, P.M.; Everett, B.M.; Thuren, T.; MacFadyen, J.G.; Chang, W.H.; Ballantyne, C.; Fonseca, F.; Nicolau, J.; Koenig, W.; Anker, S.D.; et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N. Engl. J. Med. 2017, 377, 1119–1131. [Google Scholar] [CrossRef]
- Driver, C.; Bamitale, K.; Kazi, A.; Olla, M.; Nyane, N.; Owira, P. Cardioprotective Effects of Metformin. J. Cardiovasc. Pharmacol. 2018, 72, 121–127. [Google Scholar] [CrossRef]
- Zhang, J.; Huang, L.; Shi, X.; Yang, L.; Hua, F.; Ma, J.; Zhu, W.; Liu, X.; Xuan, R.; Shen, Y.; et al. Metformin protects against myocardial ischemia-reperfusion injury and cell pyroptosis via AMPK/NLRP3 inflammasome pathway. Aging 2020, 12, 24270–24287. [Google Scholar] [CrossRef]
- Saisho, Y. Metformin and Inflammation: Its Potential Beyond Glucose-lowering Effect. Endocr. Metab. Immune Disord. Drug Targets 2015, 15, 196–205. [Google Scholar] [CrossRef]
- Cameron, A.; Morrison, V.; Levin, D.; Mohan, M.; Forteath, C.; Beall, C.; McNeilly, A.; Balfour, D.; Savinko, T.; Wong, A.; et al. Anti-Inflammatory Effects of Metformin Irrespective of Diabetes Status. Circ. Res. 2016, 119, 652–665. [Google Scholar] [CrossRef] [PubMed]
- Rena, G.; Hardie, D.; Pearson, E.R. The mechanisms of action of metformin. Diabetologia 2017, 60, 1577–1585. [Google Scholar] [CrossRef]
- Wang, X.; Yang, L.; Kang, L.; Li, J.; Yang, L.; Zhang, J.; Liu, J.; Zhu, M.; Zhang, Q.; Shen, Y.; et al. Metformin attenuates myocardial ischemia-reperfusion injury via up-regulation of antioxidant enzymes. PLoS ONE 2017, 12, e0182777. [Google Scholar] [CrossRef]
- Yan, Y.; Li, T.; Li, Z.; He, M.; Wang, D.; Xu, Y.; Yang, X.; Bai, Y.; Lao, Y.; Zhang, Z.; et al. Metformin Suppresses the Progress of Diabetes-Accelerated Atherosclerosis by Inhibition of Vascular Smooth Muscle Cell Migration Through AMPK-Pdlim5 Pathway. Front. Cardiovasc. Med. 2021, 8, 690627. [Google Scholar] [CrossRef] [PubMed]
- Hasanpour, A.; Abbaszadeh, A.; Mir, S.; Hasanvand, A. Metformin and its anti-inflammatory and anti-oxidative effects; new concepts. J. Renal Inj. Prev. 2019, 8, 54–61. [Google Scholar]
- Cheng, Y.; Leu, H.; Chen, T.; Chen, C.; Kuo, C.; Lee, S.; Kao, C. Metformin-inclusive therapy reduces the risk of stroke in patients with diabetes: A 4-year follow-up study. J. Stroke Cerebrovasc. Dis. 2014, 23, 99–105. [Google Scholar] [CrossRef]
- Loi, H.; Boal, F.; Tronchere, H.; Cinato, M.; Kramar, S.; Oleshchuk, O.; Korda, M.; Kunduzova, O. Metformin Protects the Heart Against Hypertrophic and Apoptotic Remodeling After Myocardial Infarction. Front. Pharmacol. 2019, 10, 154. [Google Scholar] [CrossRef]
- Petrie, J.; Chaturvedi, N.; Ford, I.; Brouwers, M.; Greenlaw, N.; Tillin, T.; Hramiak, I.; Hughes, A.; Jenkins, A.; Klein, B.; et al. Cardiovascular and metabolic effects of metformin in patients with type 1 diabetes (REMOVAL): A double-blind, randomised, placebo-controlled trial. Lancet Diabetes Endocrinol. 2017, 5, 597–609. [Google Scholar] [CrossRef]
- Bolívar, S.; Noriega, L.; Ortega, S.; Osorio, E.; Rosale, S.W.; Mendoza, X.; Mendoza-Torres, E. Novel Targets of Metformin in Cardioprotection: Beyond the Effects Mediated by AMPK. Curr. Pharm. Des. 2021, 27, 80–90. [Google Scholar] [CrossRef]
- Bhamra, G.; Hausenloy, D.; Davidson, S.; Carr, R.; Paiva, M.; Wynne, A.; Mocanu, M.; Yellon, D. Metformin protects the ischemic heart by the Akt-mediated inhibition of mitochondrial permeability transition pore opening. Basic Res. Cardiol. 2008, 103, 274–284. [Google Scholar] [CrossRef]
- El Messaoudi, S.; Rongen, G.; Riksen, N. Metformin therapy in diabetes: The role of cardioprotection. Curr. Atheroscler. Rep. 2013, 15, 314. [Google Scholar] [CrossRef]
- Ong, S.; Dongworth, R.; Cabrera-Fuentes, H.; Hausenloy, D. Role of the MPTP in conditioning the heart-translatability and mechanism. Br. J. Pharmacol. 2015, 172, 2074–2084. [Google Scholar] [CrossRef] [PubMed]
- An, D.; Kewalramani, J.; Chan, D.; Ghosh, T.; Pulinikunnil, A.; Abrahani, S. Metformin influences cardiomyocyte cell death by pathways that are dependent and independent of caspase-3. Diabetologia 2006, 49, 2174–2184. [Google Scholar] [CrossRef] [PubMed]
- Thomas, I.; Gregg, B. Metformin; a review of its history and future: From lilac to longevity. Pediatr. Diabetes 2017, 18, 10–16. [Google Scholar] [CrossRef] [PubMed]
- Bailey, C.J. Metformin: Historical overview. Diabetologia 2017, 60, 1566–1576. [Google Scholar] [CrossRef] [PubMed]
- De Boer, I.; Caramori, M.; Chan, J.; Heerspink, H.; Hurst, C.; Khunti, K.; Liew, A.; Michos, E.; Navaneethan, S.; Olowu, W.; et al. KDIGO 2020 clinical practice guideline for diabetes management in chronic kidney disease. Kidney Int. 2020, 98, S1–S115. [Google Scholar] [CrossRef]
- He, L. Metformin and Systemic Metabolism. Trends Pharmacol. Sci. 2020, 41, 868–881. [Google Scholar] [CrossRef]
- Musi, N.; Hirshman, M.; Nygren, J.; Svanfeldt, M.; Bavenholm, P.; Rooyackers, O.; Zhou, G.; Williamson, J.; Ljunqvist, O.; Efendic, S.; et al. Metformin increases AMP-activated protein kinase activity in skeletal muscle of subjects with type 2 diabetes. Diabetes 2002, 51, 2074–2081. [Google Scholar] [CrossRef]
- Hunter, R.; Hughey, C.; Lantier, L.; Sundelin, E.; Peggie, M.; Zeqiraj, E.; Sicheri, F.; Jessen, N.; Wasserman, D.; Sakamoto, K. Metformin reduces liver glucose production by inhibition of fructose-1–6-bisphosphatase. Nat. Med. 2018, 24, 1395–1406. [Google Scholar] [CrossRef]
- Ouyang, J.; Parakhia, R.; Ochs, R. Metformin Activates AMP Kinase through Inhibition of AMP Deaminase. J. Biol. Chem. 2011, 286, 1–11. [Google Scholar] [CrossRef]
- Lu, G.; Wu, Z.; Shang, J.; Xie, Z.; Chen, C.; Zhang, C. The effects of metformin on autophagy. Biomed. Pharmacother. 2021, 137, 111286. [Google Scholar] [CrossRef] [PubMed]
- Hostalek, U.; Gwilt, M.; Hildemann, S. Therapeutic Use of Metformin in Prediabetes and Diabetes Prevention. Drugs 2015, 75, 1071–1094. [Google Scholar] [CrossRef]
- Podhorecka, M.; Ibanez, B.; Dmoszyńska, A. Metformin—Its potential anti-cancer and anti-aging effects. Postepy Hig. Med. Dosw. 2017, 71, 170–175. [Google Scholar] [CrossRef] [PubMed]
- Kita, Y.; Takamura, T.; Misu, H.; Ota, T.; Kurita, S.; Takeshita, Y.; Uno, M.; Matsuzawa-Nagata, N.; Kato, K.; Ando, H.; et al. Metformin prevents and reverses inflammation in a non-diabetic mouse model of nonalcoholic steatohepatitis. PLoS ONE 2012, 7, e43056. [Google Scholar] [CrossRef]
- Woo, S.; Xu, H.; Li, H.; Zhao, Y.; Hu, X.; Zhao, J.; Guo, X.; Guo, T.; Botchlett, R.; Qi, T.; et al. Metformin ameliorates hepatic steatosis and inflammation without altering adipose phenotype in diet-induced obesity. PLoS ONE 2014, 9, e91111. [Google Scholar] [CrossRef] [PubMed]
- Fullerton, M.; Galic, S.; Marcinko, K.; Sikkema, S.; Pulinilkunnil, T.; Chen, Z.; O’Neill, H.; Ford, R.; Palanivel, R.; O’Brien, M.; et al. Single phosphorylation sites in Acc1 and Acc2 regulate lipid homeostasis and the insulin-sensitizing effects of metformin. Nat. Med. 2013, 19, 1649–1654. [Google Scholar] [CrossRef]
- Emelyanova, L.; Bai, X.; Yan, Y.; Bosnjak, Z.J.; Kress, D.; Warner, C.; Kroboth, S.; Rudic, T.; Kaushik, S.; Stoeckl, E.; et al. Biphasic effect of metformin on human cardiac energetics. Transl. Res. 2021, 229, 5–23. [Google Scholar] [CrossRef]
- Bambagiotti-Alberti, M.; Pinzauti, S.; Vincieri, F.F. Simultaneous capillary gas chromatographic determination of guaifenesin, dextromethorphan and diphenhydramine in cough-cold syrup. Pharm. Acta Helv. 1987, 62, 175–176. [Google Scholar]
- Zhu, X.; Shen, W.; Liu, Z.; Sheng, S.; Xiong, W.; He, R.; Zhang, X.; Ma, L.; Ju, Z. Effect of Metformin on Cardiac Metabolism and Longevity in Aged Female Mice. Front. Cell Dev. Biol. 2021, 8, 626011. [Google Scholar] [CrossRef]
- Kralj, V.; Brkic Bilos, I. Morbidity and mortality from cardiovascular diseases. Cardiol. Croat. 2013, 8, 373–378. [Google Scholar] [CrossRef]
- Malakar, A.; Choudhury, D.; Halder, B.; Paul, P.; Uddin, A.; Chakraborty, S. A review on coronary artery disease, its risk factors, and therapeutics. J. Cell. Physiol 2019, 234, 16812–16823. [Google Scholar] [CrossRef] [PubMed]
- Mack, M.; Gopal, A. Epidemiology, Traditional and Novel Risk Factors in Coronary Artery Disease. Heart Fail Clin. 2016, 12, 1–10. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Top 10 Causes of Death. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed on 3 January 2022).
- Virani, S.; Alonso, A.; Aparicio, H.; Benjamin, E.; Bittencourt, M.; Callaway, C.; Carson, A.; Chamberlain, A.; Cheng, S.; Delling, F.; et al. Heart Disease and Stroke Statistics—2021 Update: A Report From the American Heart Association. Circulation 2021, 143, 254–743. [Google Scholar] [CrossRef] [PubMed]
- Duggan, J.; Peters, A.; Trachiotis, G.; Antevil, J. Epidemiology of Coronary Artery Disease. Surg. Clin. North. Am. 2022, 102, 499–516. [Google Scholar] [CrossRef]
- Férez, S.; Márquez, M.; Ocaranza, R. Daño miocárdico por reperfusión (Myocardial Reperfusion Injury). Rev. Esp. Cardiol. 2004, 57, 9–21. [Google Scholar] [CrossRef]
- Wang, L.; Niu, H.; Zhang, J. Homocysteine induces mitochondrial dysfunction and oxidative stress in myocardial ischemia/reperfusion injury through stimulating ROS production and the ERK1/2 Signaling Pathway. Exp. Ther. Med. 2020, 20, 938–944. [Google Scholar] [CrossRef]
- Dai, H.; Much, A.; Maor, E.; Asher, E.; Younis, A.; Xu, Y.; Lu, Y.; Liu, X.; Shu, J.; Bragazzi, N. Global, regional, and national burden of ischemic heart disease and its attributable risk factors, 1990–2017: Results from the global burden of disease study 2017. Eur. Heart J. Qual. Care Clin. Outcomes 2020, 8, 50–60. [Google Scholar] [CrossRef]
- Kanamori, H.; Naruse, G.; Yoshida, A.; Minatoguchi, S.; Watanabe, T.; Kawaguchi, T.; Yamada, Y.; Mikami, A.; Kawasaki, M.; Takemura, G.; et al. Metformin Enhances Autophagy and Provides Cardioprotection in δ-Sarcoglycan Deficiency-Induced Dilated Cardiomyopathy. Circ. Heart Fail. 2019, 12, e005418. [Google Scholar] [CrossRef]
- Land, W.G. The Role of Damage-Associated Molecular Patterns in Human Diseases: Part I—Promoting inflammation and immunity. Sultan Qaboos Univ. Med. J. 2015, 15, e9–e21. [Google Scholar]
- Gibson, M. Reperfusion Injury of the Heart. UpToDate. Last Update 19 November 2021. Available online: https://www.uptodate.com/contents/reperfusion-injury-of-the-heart (accessed on 26 January 2023).
- Beaulieu, J.; Grimm, C.; Hassoun, T. Ischemia-Reperfusion. In Rutherford’s Vascular Surgery and Endovascular Therapy, 9th ed.; Elsevier: Philadelphia, PA, USA, 2019; Volume 2, pp. 64–71. [Google Scholar]
- Dzwierzynski, W. Replantation and revascularization. In Plastic Surgery: Hand and Upper Extremity, 4th ed.; Elsevier: Philadelphia, PA, USA, 2018; Volume 6, pp. 247–270. [Google Scholar]
- Abella, B.S.; Bobrow, B.J. Síndrome posterior al paro cardiaco. In Tintinalli Medicina de Urgencias, 8th ed.; Tintinalli, J., Stapczynski, J., Ma, O., Yealy, D., Meckler, G., Cline, D., Eds.; McGraw Hill Medical: Ciudad de México, México, 2018; Volume 1. [Google Scholar]
- Kalogeris, T.; Baines, C.; Krenz, M.; Korthuis, R. Cell biology of ischemia/reperfusion injury. Int. Rev. Cell Mol. Biol. 2012, 298, 229–317. [Google Scholar]
- Kvietys, P.; Granger, D. Role of reactive oxygen and nitrogen species in the vascular responses to inflammation. Free Radic. Biol. Med. 2012, 52, 556–592. [Google Scholar] [CrossRef] [PubMed]
- Przykaza, Ł. Understanding the Connection Between Common Stroke Comorbidities, Their Associated Inflammation, and the Course of the Cerebral Ischemia/Reperfusion Cascade. Front. Immunol. 2021, 12, 782569. [Google Scholar] [CrossRef] [PubMed]
- Rajendran, P.; Rengarajan, T.; Thangavel, J.; Nishigaki, Y.; Sakthisekaran, D.; Sethi, G.; Nishigaki, I. The vascular endothelium and human diseases. Int. J. Biol. Sci. 2013, 9, 1057–1069. [Google Scholar] [CrossRef] [PubMed]
- Palee, S.; Maneechote, C.; Kerdphoo, S.; Jaiwongkam, T.; Chattipakorn, S.; Chattipakorn, N. Differential temporal inhibition of mitochondrial fission by Mdivi–1 exerts effective cardioprotection in cardic ischemia/reperfusion injury. Clin. Sci. 2018, 132, 1669–1683. [Google Scholar]
- Lu, T.; Zeng, X.; Yang, W.; Zhang, Y. Treatment with metformin prevents myocardial ischemia-reperfusion injury via STEAP4 signaling pathway. Anatol. J. Cardiol. 2019, 21, 261–271. [Google Scholar] [CrossRef]
- Shi, Y.; Hou, S. Protective effects of metformin against myocardial ischemia-reperfusion injury via AMPK-dependent suppression of NOX4. Mol. Med. Rep. 2021, 24, 712. [Google Scholar] [CrossRef]
- Huang, K.; Que, J.; Hu, Z.; Yu, Y.; Zhou, Y.; Wang, L.; Xue, Y.; Ji, K.; Zhang, X. Metformin suppresses inflammation and apoptosis of myocardiocytes by inhibiting autophagy in a model of ischemia-reperfusion injury. Int. J. Biol. Sci. 2020, 16, 2559–2579. [Google Scholar] [CrossRef]
- Asensio-Lopez, M.D.C.; Lax, A.; Fernandez Del Palacio, M.J.; Sassi, Y.; Hajjar, R.J.; Pascual-Figal, D.A. Pharmacological inhibition of the mitochondrial NADPH oxidase 4/PKCα/Gal-3 pathway reduces left ventricular fibrosis following myocardial infarction. Transl. Res. 2018, 199, 4–23. [Google Scholar] [CrossRef]
- Wu, S.; Zhang, H.; Chen, N.; Zhang, C.; Guo, X. Metformin protects cardiomyocytes against oxygen-glucose deprivation injury by promoting autophagic flux through AMPK pathway. J. Drug Target. 2021, 29, 551–561. [Google Scholar] [CrossRef]
- Fei, Q.; Ma, H.; Zou, J.; Wang, W.; Zhu, L.; Deng, H.; Meng, M.; Tan, S.; Zhang, H.; Xiao, X.; et al. Metformin protects against ischaemic myocardial injury by alleviating autophagy-ros-NLRP3-mediated inflammatory response in macrophages. J. Mol. Cell. Cardiol. 2020, 145, 1–13. [Google Scholar] [CrossRef]
- Zhang, Y.; Liu, X.; Zhang, L.; Li, X.; Zhou, Z.; Jiao, L.; Shao, Y.; Li, M.; Leng, B.; Zhou, Y.; et al. Metformin Protects against H2O2-Induced Cardiomyocyte Injury by Inhibiting the miR-1a-3p/GRP94 Pathway. Mol. Ther. Nucleic Acids 2018, 13, 189–197. [Google Scholar] [CrossRef] [PubMed]
- Tian, J.; Zheng, Y.; Mou, T.; Yun, M.; Tian, Y.; Lu, Y.; Bai, Y.; Zhou, Y.; Hacker, M.; Zhang, X.; et al. Metformin confers longitudinal cardiac protection by preserving mitochondrial homeostasis following myocardial ischemia/reperfusion injury. Eur. J. Nucl. Med. Mol. Imaging 2023, 50, 825–838. [Google Scholar] [CrossRef]
- Chen, Q.; Thompson, J.; Hu, Y.; Lesnefsky, E. Chronic metformin treatment decreases cardiac injury during ischemia-reperfusion by attenuating endoplasmic reticulum stress with improved mitochondrial function. Aging 2021, 13, 7828–7845. [Google Scholar] [CrossRef] [PubMed]
- Arinno, A.; Maneechote, C.; Khuanjing, T.; Ongnok, B.; Prathumsap, N.; Chunchai, T.; Arunsak, B.; Kerdphoo, S.; Shinlapawittayatorn, K.; Chattipakorn, S.; et al. Cardioprotective effects of melatonin and metformin against doxorubicin-induced cardiotoxicity in rats are through preserving mitochondrial function and dynamics. Biochem. Pharmacol. 2021, 192, 114743. [Google Scholar] [CrossRef] [PubMed]
- Su, H.; Lu, D.; Shen, M.; Feng, L.; Xu, C. Evaluating the cardioprotective effect of metformin on myocardial ischemia-reperfusion injury using dynamic 18F-FDG micro-PET/CT imaging. BMC Cardiovasc. Disord. 2022, 22, 310. [Google Scholar] [CrossRef]
- Jo, W.; Kang, K.; Chae, S.; Son, W. Metformin Alleviates Left Ventricular Diastolic Dysfunction in a Rat Myocardial Ischemia Reperfusion Injury Model. Int. J. Mol. Sci. 2020, 21, 1489. [Google Scholar] [CrossRef]
- Palee, S.; Higgins, L.; Leech, T.; Chattipakorn, S.C.; Chattipakorn, N. Acute metformin treatment provides cardioprotection via improved mitochondrial function in cardiac ischemia / reperfusion injury. Biomed. Pharmacother. 2020, 130, 110604. [Google Scholar] [CrossRef] [PubMed]
- Eppinga, R.; Kofink, D.; Dullaart, R.; Dalmeijer, G.; Lipsic, E.; van Veldhuisen, D.; van der Horst, I.; Asselbergs, F.; van der Harst, P. Effect of Metformin on Metabolites and Relation with Myocardial Infarct Size and Left Ventricular Ejection Fraction After Myocardial Infarction. Circ. Cardiovasc. Genet. 2017, 10, 001564. [Google Scholar] [CrossRef]
- Charytan, D.; Solomon, S.; Ivanovich, P.; Remuzzi, G.; Cooper, M.; McGill, J.; Parving, H.; Parfrey, P.; Singh, A.; Burdmann, E.; et al. Metformin use and cardiovascular events in patients with type 2 diabetes and chronic kidney disease. Diabetes Obes. Metab. 2019, 21, 1199–1208. [Google Scholar] [CrossRef]
- Bergmark, B.; Bhatt, D.; McGuire, D.; Cahn, A.; Mosenzon, O.; Steg, P.; Im, K.; Kanevsky, E.; Gurmu, Y.; Raz, I.; et al. Metformin Use and Clinical Outcomes Among Patients With Diabetes Mellitus With or Without Heart Failure or Kidney Dysfunction: Observations From the SAVOR-TIMI 53 Trial. Circulation 2019, 140, 1004–1014. [Google Scholar] [CrossRef]
- Indhavivadhana, S.; Rattanachaiyanont, M.; Wongwananurak, T.; Techatraisak, K.; Jirattigalachote, A.; Dangrat, C. Effect of metformin on cardiovascular risk factors in middle-aged Thai women with metabolic syndrome: A randomized placebo-controlled trial. J. Obstet. Gynaecol. Res. 2020, 46, 1193–1202. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, S.; Xavier, D.; George, B.; Umesh, S.; Fathima, S.; Bantwal, G. Effect of intensive lifestyle modification & metformin on cardiovascular risk in prediabetes: A pilot randomized control trial. Indian J. Med. Res. 2018, 148, 705–712. [Google Scholar] [PubMed]
- Sardu, C.; Paolisso, P.; Sacra, C.; Mauro, C.; Minicucci, F.; Portoghese, M.; Rizzo, M.; Barbieri, M.; Sasso, F.; D’Onofrio, N.; et al. Effects of Metformin Therapy on Coronary Endothelial Dysfunction in Patients With Prediabetes With Stable Angina and Nonobstructive Coronary Artery Stenosis: The CODYCE Multicenter Prospective Study. Diabetes Care 2019, 42, 1946–1955. [Google Scholar] [CrossRef]
- Lee, C.; Heckman-Stoddard, B.; Dabelea, D.; Gadde, K.; Ehrmann, D.; Ford, L.; Prorok, P.; Boyko, E.; Pi-Sunyer, X.; Wallia, A.; et al. Effect of Metformin and Lifestyle Interventions on Mortality in the Diabetes Prevention Program and Diabetes Prevention Program Outcomes Study. Diabetes Care 2021, 44, 2775–2782. [Google Scholar] [CrossRef] [PubMed]
- Hartman, M.H.; Prins, J.K.; Schurer, R.A.; Lipsic, E.; Lexis, C.P.; van der Horst-Schrivers, A.N.; van Veldhuisen, D.J.; van der Horst, I.C.; van der Harst, P. Two-year follow-up of 4 months metformin treatment vs. placebo in st-elevation myocardial infarction: Data from the gips-III RCT. Clin. Res. Cardiol. 2017, 106, 939–946. [Google Scholar] [CrossRef]
- Goldberg, R.B.; Orchard, T.J.; Crandall, J.P.; Boyko, E.J.; Budoff, M.; Dabelea, D.; Gadde, K.; Knowler, W.; Lee, C.; Nathan, D.; et al. Effects of long-term metformin and lifestyle interventions on cardiovascular events in the diabetes prevention program and its outcome study. Circulation 2022, 145, 1632–1641. [Google Scholar] [CrossRef]

| Models | In Vitro | In Vivo | Dosage | Effects |
|---|---|---|---|---|
| I/R | H9C2 Cells | Sprague Dawley rats | In vitro: 0, 10, 20, 40 u 80 µmol/L In vivo: 250 mg/kg | Metformin reduced infarct size, increased STEAP4 expression and mitigation of myocardial apoptosis, and increased MMP when models underwent H/R or I/R lesions [59]. |
| I/R | - | Sprague Dawley (SD) male rat | 5 mg/kg | Metformin inhibited NOX4 expression through AMPK activation, resulting in decreased myocardial oxidative damage, apoptosis, and infarct size [60]. |
| I/R | Neonatal Rat Ventricular Cardiomyocytes (NRVC) | - | 0, 1, 0, 5, 1, 2, 5 o 10 mM | Metformin attenuated H2O2-induced cardiomyocyte injury via the AMPK/C/EBP β/miR-1a-3p/GRP94 pathway [64]. |
| I/R | H9c2 Cells | C57BL/6 Mice | In vitro: 50 μM In vivo: 125 µg/kg | Metformin protected cardiomyocytes from I/R-induced apoptosis and inflammation through downregulation of autophagy mediated by Akt signaling pathway [65]. |
| I/R | - | Sprague Dawley rats | 400 mg/kg/day | Metformin decreased the size of the infarct in the heart by inducing autophagy through regulation of the mTOR/AMPK pathway [70]. |
| I/R | Male Wistar rats | - | 100, 200 y 400 mg/kg | Metformin reduced mitochondrial fission, apoptosis, arrhythmias, infarct size, and preserved left ventricular function, thus reducing the mortality rate [76]. |
| Title and Authors | Treatment | Main Findings |
|---|---|---|
| Metformin use and cardiovascular events in patients with type 2 diabetes and chronic kidney disease. Charytan et al. (2019) [77]. | 591 individuals who used metformin at baseline and 3447 non-users | Cardiovascular mortality, cardiovascular events and the combined endpoint were lower in metformin users than in non-users. |
| Metformin Use and Clinical Outcomes Among Patients with Diabetes Mellitus With or Without Heart Failure or Kidney Dysfunction: Observations From the SAVOR-TIMI 53 Trial. Bergmark et al. (2019) [78]. | Patients in SAVOR-TIMI 53 (saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus) were classified as ever versus never taking metformin. | Reduction in mortality after the use of metformin in association with other antidiabetic drugs. |
| Effect of metformin on cardiovascular risk factors in middle-aged Thai women with metabolic syndrome: A randomized placebo-controlled trial. Indhavivadhana et al. (2020) [79]. | Double-blind and placebo-controlled study in 40 menopausal women with metabolic syndrome after taking metformin 1700 mg/day for 6 months. | Metformin improved some parameters of metabolic syndrome. Metformin improved body mass index, fasting blood glucose, high-sensitivity C-reactive protein and 10-year risk of coronary heart disease. |
| Effect of intensive lifestyle modification & metformin on cardiovascular risk in prediabetes: A pilot randomized control trial. Kulkarni et al. (2018) [80]. | 103 prediabetic patients were randomized into three arms: standard care (STD), intensive lifestyle modification (ILSM) or ILSM and metformin (ILSM + Met), and followed up for six months. | Reduction in weight and fasting blood sugar from baseline in all three arms. No difference in high-sensitivity C-reactive protein and carotid intima-media thickness in the two intervention arms, compared to standard care. |
| Effects of Metformin Therapy on Coronary Endothelial Dysfunction in Patients with Prediabetes With Stable Angina and Nonobstructive Coronary Artery Stenosis: The CODYCE Multicenter Prospective Study. Sardu et. al. (2019) [81]. | 258 propensity score-matched (PSM) patients with stable angina undergoing coronary angiography were classified into three groups: 86 with normoglycemia, 86 with prediabetes, and 86 with prediabetes treated with metformin. | Major cardiovascular events were lower in the group treated with metformin. |
| Effect of Metformin and Lifestyle Interventions on Mortality in the Diabetes Prevention Program and Diabetes Prevention Program Outcomes Study. Lee et al. (2021) [82]. | 3234 healthy patients with risk factors for type 2 diabetes mellitus were randomized and subjected to intensive lifestyle intervention, metformin, or placebo. | Metformin and lifestyle modification prevented diabetes. However, none of these strategies reduced cancer or cardiovascular mortality rates. |
| Two-year follow-up of 4 months metformin treatment vs. placebo in ST-elevation myocardial infarction: data from the GIPS-III RCT. Hartman et al. (2017) [83]. | 379 patients without diabetes undergoing primary percutaneous coronary intervention were randomized to a 4-month treatment with metformin or placebo. | Four months of metformin treatment in STEMI patients without diabetes did not exert favorable long-term effects. |
| Effects of Long-term Metformin and Lifestyle Interventions on Cardiovascular Events in the Diabetes Prevention Program and Its Outcome Study. Goldberg et al. (2022) [84]. | 3.234 people with impaired glucose tolerance were randomly assigned to receive metformin 850 mg twice daily, a strict diet, or a placebo, and were then monitored for three years. The authors also examined whether these interventions reduced the incidence of major cardiovascular events over a 21-year median follow-up. | Neither metformin nor lifestyle reduced major cardiovascular events. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Osorio-Llanes, E.; Villamizar-Villamizar, W.; Ospino Guerra, M.C.; Díaz-Ariza, L.A.; Castiblanco-Arroyave, S.C.; Medrano, L.; Mengual, D.; Belón, R.; Castellar-López, J.; Sepúlveda, Y.; et al. Effects of Metformin on Ischemia/Reperfusion Injury: New Evidence and Mechanisms. Pharmaceuticals 2023, 16, 1121. https://doi.org/10.3390/ph16081121
Osorio-Llanes E, Villamizar-Villamizar W, Ospino Guerra MC, Díaz-Ariza LA, Castiblanco-Arroyave SC, Medrano L, Mengual D, Belón R, Castellar-López J, Sepúlveda Y, et al. Effects of Metformin on Ischemia/Reperfusion Injury: New Evidence and Mechanisms. Pharmaceuticals. 2023; 16(8):1121. https://doi.org/10.3390/ph16081121
Chicago/Turabian StyleOsorio-Llanes, Estefanie, Wendy Villamizar-Villamizar, María Clara Ospino Guerra, Luis Antonio Díaz-Ariza, Sara Camila Castiblanco-Arroyave, Luz Medrano, Daniela Mengual, Ricardo Belón, Jairo Castellar-López, Yanireth Sepúlveda, and et al. 2023. "Effects of Metformin on Ischemia/Reperfusion Injury: New Evidence and Mechanisms" Pharmaceuticals 16, no. 8: 1121. https://doi.org/10.3390/ph16081121
APA StyleOsorio-Llanes, E., Villamizar-Villamizar, W., Ospino Guerra, M. C., Díaz-Ariza, L. A., Castiblanco-Arroyave, S. C., Medrano, L., Mengual, D., Belón, R., Castellar-López, J., Sepúlveda, Y., Vásquez-Trincado, C., Chang, A. Y., Bolívar, S., & Mendoza-Torres, E. (2023). Effects of Metformin on Ischemia/Reperfusion Injury: New Evidence and Mechanisms. Pharmaceuticals, 16(8), 1121. https://doi.org/10.3390/ph16081121







