Prunella vulgaris L.: An Updated Overview of Botany, Chemical Composition, Extraction Methods, and Biological Activities
Abstract
1. Introduction
2. Botany
3. Extracting Methods of PV
| Method | Plant Part | Solvent | Liquid/Solid Ratio | Temperature, °C | Time | References |
|---|---|---|---|---|---|---|
| Reflux | Aerial part | DI water | - | 100 | 2 h | [19] |
| Reflux | Herb | DI water | - | 70 | 5 h | [24] |
| Reflux | Herb | 70% ethanol | 2:19 | - | 1 h | [27] |
| Reflux | Herb | 95% ethanol | - | 60 | 4 h | [28] |
| Stirring | Seed | Methanol | 3 × 10 mL methanol g−1 | - | 30 min | [22] |
| Stirring | Herb | Methanol Hexane Ethyl acetate | 9:1 | Room temperature | 48 h | [29] |
| Maceration | Leaves, stems, flowers | Methanol DI water | 2:1 | Room temperature | 16 h 24 h | [21] |
| Maceration | Aerial part | 80% methanol | - | Room tempersture | - | [25] |
| Maceration | Whole plant | Hexane Cloroform Butanol | - | - | - | [26] |
| Infusing | Leaves of herbal tea | DI water | 1:1 | 80 | 15 min | [23] |
| Supercritical fluid extraction | Flowers and dried fruit spikes | - | 30 | 2 h | [30] | |
| Ultrasonic | Leaf, spike inflorescence | DI water 70% methanol | 10:1 | 60 | 1 h | [20] |
| Ultrasonic | Herb | from 20 to 60% | from 10:1 to 50:1 | From 40 to 80 | From 10 to 50 | [35] |
| Deep eutectic solvent extraction | Water-deep eutectic solvent | 15 mL·g−1 | 83 | 42 min | [38] |
4. Chemical Composition of PV Plant Parts
5. Biological Activities of PV Extracts
5.1. Antiviral Activity
5.2. Antibacterial Activity
5.3. Antitumor Activity
5.4. Antioxidant Activity
5.5. Treatment of Thyroiditis-Associated Diseases
5.6. Other Activities
6. Dosage Forms and Clinical Applications
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wang, S.J.; Wang, X.H.; Dai, Y.Y.; Ma, M.H.; Rahman, K.; Nian, H.; Zhang, H. Prunella vulgaris: A Comprehensive Review of Chemical Constituents, Pharmacological Effects and Clinical Applications. Curr. Pharm. Des. 2019, 25, 359–369. [Google Scholar] [CrossRef]
- Cheremushkina, V.A.; Barsukova, I.N. Rhythm of seasonal development and small life cycle of Prunella vulgaris L. (Lamiaceae) in Khakassia. J. Sib. Fed. University. Biol. 2020, 13, 94–108. [Google Scholar] [CrossRef]
- Commission, C.P. The 2020 Edition of Pharmacopoeia of the People’s Republic of China Volume 1, 11th ed.; Chemical Industry Press: Beijing, China, 2020. [Google Scholar]
- Council of Europe. European Pharmacopoeia, 10th ed.; Deutscher Apotheker: Stuttgart, Germany, 2019. [Google Scholar]
- Huang, N.; Hauck, C.; Yum, M.Y.; Rizshsky, L.; Widrlechner, M.P.; McCoy, J.A.; Murphy, P.A.; Dixon, P.M.; Nikolau, B.J.; Birt, D.F. Rosmarinic acid in Prunella vulgaris ethanol extract inhibits lipopolysaccharide-induced prostaglandin E2 and nitric oxide in RAW 264.7 mouse macrophages. J. Agric. Food Chem. 2009, 57, 10579–10589. [Google Scholar] [CrossRef]
- Bai, Y.; Xia, B.; Xie, W.; Zhou, Y.; Xie, J.; Li, H.; Liao, D.; Lin, L.; Li, C. Phytochemistry and pharmacological activities of the genus Prunella. Food Chem. 2016, 204, 483–496. [Google Scholar] [CrossRef] [PubMed]
- Ryu, S.Y.; Oak, M.H.; Yoon, S.K.; Cho, D.I.; Yoo, G.S.; Kim, T.S.; Kim, K.M. Anti-allergic and anti-inflammatory triterpenes from the herb of Prunella vulgaris. Planta Med. 2000, 66, 358–360. [Google Scholar] [CrossRef] [PubMed]
- Psotová, J.; Kolár, M.; Sousek, J.; Svagera, Z.; Vicar, J.; Ulrichová, J. Biological activities of Prunella vulgaris extract. Phytother. Res. 2003, 17, 1082–1087. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Jung, E.; Koh, J.; Kim, Y.S.; Park, D. Effect of rosmarinic acid on atopic dermatitis. J. Dermatol. 2008, 35, 768–771. [Google Scholar] [CrossRef]
- Vostálová, J.; Zdarilová, A.; Svobodová, A. Prunella vulgaris extract and rosmarinic acid prevent UVB-induced DNA damage and oxidative stress in HaCaT keratinocytes. Arch. Dermatol. Res. 2010, 302, 171–181. [Google Scholar] [CrossRef]
- Pan, J.; Wang, H.; Chen, Y. Prunella vulgaris L.—A Review of its Ethnopharmacology, Phytochemistry, Quality Control and Pharmacological Effects. Front. Pharmacol. 2022, 13, 903171. [Google Scholar] [CrossRef]
- Malencic, D.J.; Gasic, O.; Popovic, M.; Boza, P. Screening for antioxidant properties of Salvia reflexa fornem. Phytother. Res. 2000, 14, 546–548. [Google Scholar] [CrossRef]
- Badekova, K.Z.; Levaya, Y.K.; Atazhanova, G.A.; Zholdasbayev, M.E. Biological properties of rosmarinic acid. Pharm. Kazakhstan 2020, 7–8, 29–34. [Google Scholar]
- Paly, A.E.; Melikov, F.M.; Grebennikova, O.A.; Rabotyagov, V.D. Rosmarinic acid and its raw materials in the Crimea. Pharm. Pharmacol. 2015, 3, 7–12. [Google Scholar] [CrossRef] [PubMed]
- al-Sereiti, M.R.; Abu-Amer, K.M.; Sen, P. Pharmacology of rosemary (Rosmarinus officinalis Linn.) and its therapeutic potentials. Indian J. Exp. Biol. 1999, 37, 124–130. [Google Scholar] [PubMed]
- Gamaro, G.D.; Suyenaga, E.; Borsoi, M.; Lermen, J.; Pereira, P.; Ardenghi, P. Effect of rosmarinic and caffeic acids on inflammatory and nociception process in rats. ISRN Pharmacol. 2011, 2011, 451682. [Google Scholar] [CrossRef]
- Soo Lee, Y.; Jin, D.Q.; Beak, S.M.; Lee, E.S.; Kim, J.A. Inhibition of ultraviolet-A-modulated signaling pathways by asiatic acid and ursolic acid in HaCaT human keratinocytes. Eur. J. Pharmacol. 2003, 476, 173–178. [Google Scholar] [CrossRef]
- Nauka. Flora of Kazakhstan, 7th ed.; Nauka: Alma-Ata Kazakhstan, Kazakh, 1964. [Google Scholar]
- Komal, S.; Kazmi, S.A.J.; Khan, J.A.; Gilani, M.M. Antimicrobial activity of Prunella vulgaris extracts against multi-drug resistant Escherichia coli from patients of urinary tract infection. Pak. J. Med. Sci. 2018, 34, 616–620. [Google Scholar] [CrossRef] [PubMed]
- Groşan, A.; Ștefănescu, R.; Vari, C.E.; Jîtcă, G.; Bătrânu, M.; Muntean, L.D. Phytochemical Characterization of Transilvanian Prunella vulgaris. Acta Biol. Marisiensis 2020, 3, 62–69. [Google Scholar] [CrossRef]
- Lone, B.A.; Chishti, M.Z.; Bhat, F.A.; Tak, H.; Bandh, S.A. Anthelmintic Activities of Aqueous and Methanol Extracts of Prunella vulgaris L. Nat. Prod. Chem. Res. 2017, 5, 269. [Google Scholar] [CrossRef]
- Danthine, S.; Paul, A.; Jansen, O.; Ducrey, A.; Richel, A.; Lognay, G.; Maesen, P.; Mutwale Kapepula, P.; Mouithys-Mickalad, A.; Franck, T.; et al. Prunella vulgaris L. seeds: A promising source of lipids, proteins, and original phenolic compounds presenting high antioxidant and anti-inflammatory activity. Biotechnol. Agron. Soc. Environ. 2022, 26, 1–15. [Google Scholar] [CrossRef]
- Tan, R.; Lai, J.X.; Loke, W.M. Antioxidant and Anti-inflammatory Properties of Prunella vulgaris Tea. Curr. Res. Nutr. Food Sci. 2022, 10, 521–531. [Google Scholar] [CrossRef]
- Wu, H.; Gao, M.; Ha, T.; Kelley, J.; Young, A.; Breuel, K. Prunella vulgaris aqueous extract attenuates IL-1β-induced apoptosis and NF-κB activation in INS-1 cells. Exp. Ther. Med. 2012, 3, 919–924. [Google Scholar] [CrossRef] [PubMed]
- Küpeli Akkol, E.; Renda, G.; İlhan, M.; Bektaş, N.Y. Wound healing acceleration and anti-inflammatory potential of Prunella vulgaris L.: From conventional use to preclinical scientific verification. J. Ethnopharmacol. 2022, 295, 115411. [Google Scholar] [CrossRef] [PubMed]
- Hwang, Y.J.; Lee, E.J.; Kim, H.R.; Hwang, K.A. In vitro antioxidant and anticancer effects of solvent fractions from Prunella vulgaris var. lilacina. BMC Complement Altern Med 2013, 13, 310. [Google Scholar] [CrossRef]
- Lin, T.F.; Qiu, J.N.; Zhang, S.; Zhang, Y.; Zhang, Y.; Sun, M.; Zhang, J.H.; Liu, B.; Cheng, F.F.; Jiang, Y.Y. Screening out the anti-insomnia components from Prunella vulgaris L. based on plasma pharmacochemistry combined with pharmacodynamic experiments and UPLC-MS/MS analysis. J Ethnopharmacol 2021, 279, 114373. [Google Scholar] [CrossRef]
- Zhang, Z.; Zhou, Y.; Lin, Y.; Li, Y.; Xia, B.; Lin, L.; Liao, D. GC-MS-based metabolomics research on the anti-hyperlipidaemic activity of Prunella vulgaris L. polysaccharides. Int. J. Biol. Macromol. 2020, 159, 461–473. [Google Scholar] [CrossRef] [PubMed]
- Özbek, O.; Saglam, B.; Canan Usta, N.; Budak, Y. GC–MS analysis and anti–microbial activity of Prunella vulgaris L. extracts. J. Indian Chem. Soc. 2022, 99, 100460. [Google Scholar] [CrossRef]
- Lin, Y.; Yang, C.; Tang, J.; Zhang, Z.; Xia, B.; Li, Y.; Lin, L.; Liao, D. Characterization and anti-uterine tumor effect of extract from Prunella vulgaris L. BMC Complement. Med. Ther. 2020, 20, 189. [Google Scholar] [CrossRef] [PubMed]
- Swami Soumya, S.B.; Sawant, A.A.; Khandetod, Y.P.; Mohod, A.G.; Dhekale, J.S. Extraction methods used for extraction of anthocyanin: A review. Pharma Innov. J. 2019, 8, 280–285. [Google Scholar]
- Carpentieri, S.; Režek, J.A.; Ferrari, G.; Pataro, G. Pulsed Electric Field-Assisted Extraction of Aroma and Bioactive Compounds From Aromatic Plants and Food By-Products. Front. Nutr. 2022, 8, 792203. [Google Scholar] [CrossRef]
- Puri, M.; Sharma, D.; Barrow, C.J. Enzyme-assisted extraction of bioactives from plants. Trends Biotechnol. 2012, 30, 37–44. [Google Scholar] [CrossRef]
- Nieto, A.; Borrull, F.; Pocurull, E.; Marce, R.M. Pressurized liquid extraction: A useful technique to extract pharmaceuticals and personal-care products from sewage sludge. TrAC Trends Anal. Chem. 2010, 29, 752–764. [Google Scholar] [CrossRef]
- Levaya, Y.K.; Zholdasbayev, M.E.; Atazhanova, G.A.; Akhmetova, S.B.; Ishmuratova, M.Y. Antibacterial activity of ultrasonic extracts of Salvia stepposa growing in Kazakhstan. Bull. Karaganda Univ. Ser. Biol. Med. Geogr. 2021, 1, 45–49. [Google Scholar] [CrossRef]
- Levaya, Y.K.; Zholdasbayev, M.E.; Atazhanova, G.A.; Akhmetova, S.B. Evaluation of Antibacterial Activity of Salvia stepposa Extracts Isolated using Microwave Extraction, Growing Wild in Kazakhstan. Trends Sci. 2022, 19, 3217. [Google Scholar] [CrossRef]
- Ji, J.B.; Lu, X.H.; Cai, M.Q.; Xu, Z.C. Improvement of leaching process of Geniposide with ultrasound. Ultrason. Sonochem 2006, 13, 455–462. [Google Scholar] [CrossRef]
- Gaete-Garretón, L.; Vargas-Hernández, Y.; Cares-Pacheco, M.G.; Sainz, J.; Alarcón, J. Ultrasonically enhanced extraction of bioactive principles from Quillaja Saponaria Molina. Ultrasonics 2011, 51, 581–585. [Google Scholar] [CrossRef]
- Guowen, Z.; Li, H.; Hu, M. Optimized ultrasonic-assisted extraction of flavonoids from Prunella vulgaris L. and evaluation of antioxidant activities in vitro. Innov. Food Sci. Emerg. Technol. 2011, 12, 18–25. [Google Scholar] [CrossRef]
- Groșan, A.; Stefănescu, R.; Gurzu, S.; Muntean, D.; Vlase, L.; Vari, C. Study of the potential antiulcerous action of hydroalcoholic extracts from Prunella vulgaris L. of romanian origin. Farmacia 2020, 68, 5. [Google Scholar] [CrossRef]
- Mak, W.; Walsh, S. The Characterization of Steam Distillation as an Extraction Method to Extract Volatile Compounds from Prunella vulgaris and the Investigation of Their Anti-Tumorous Effect. J. Biosci. Med. 2021, 9, 120–142. [Google Scholar] [CrossRef]
- Xia, B.H.; Xiong, S.H.; Tang, J.; Zhang, Z.M.; Li, Y.M.; Li, M.J.; Lin, L.M. Extraction of flavonoids in Prunella vulgaris based on deep eutectic solvent method: Application of new green solvent. Zhongguo Zhong Yao Za Zhi 2018, 43, 3484–3492. (In Chinese) [Google Scholar] [CrossRef] [PubMed]
- Alupului, A.; Călinescu, I.; Lavric, V. Microwave extraction of active principles from medicinal plants. U.P.B. Sci. Bull. Series B 2012, 74, 129–142. [Google Scholar]
- Bagade, S.B.; Patil, M. Recent Advances in Microwave Assisted Extraction of Bioactive Compounds from Complex Herbal Samples: A Review. Crit. Rev. Anal. Chem. 2021, 51, 138–149. [Google Scholar] [CrossRef] [PubMed]
- Akhtar, I.; Javad, S.; Yousaf, Z.; Iqbal, S.; Jabeen, K. Review: Microwave assisted extraction of phytochemicals an efficient and modern approach. Pak. J. Pharm. Sci. 2019, 32, 223–230. [Google Scholar] [PubMed]
- Zhang, X.R.; Chen, Y.H.; Guo, Q.S.; Wang, W.M.; Liu, L.; Fan, J. Short-term UV-B radiation effects on morphology, physiological traits and accumulation of bioactive compounds in Prunella vulgaris L. J. Plant Interact. 2017, 12, 348–354. [Google Scholar] [CrossRef]
- Chen, Y.; Zhang, X.; Guo, Q.; Cao, L.; Qin, Q.; Li, C.; Zhao, M.; Wang, W. Plant morphology, physiological characteristics, accumulation of secondary metabolites and antioxidant activities of Prunella vulgaris L. under UV solar exclusion. Biol. Res. 2019, 52, 17. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Huang, Q.; Fu, X.; Yue, X.J.; Liu, R.H.; You, L.J. Characterization, antioxidant and immunomodulatory activities of polysaccharides from Prunella vulgaris Linn. Int. J. Biol. Macromol. 2015, 75, 298–305. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.X.; Qin, F.; Pan, Y.J. In vitro and in vivo immunosuppressive activity of Spica Prunellae ethanol extract on the immune responses in mice. J. Ethnopharmacol. 2005, 101, 31–36. [Google Scholar] [CrossRef]
- Fazal, H.; Abbasi, B.H.; Ahmad, N.; Ali, S.S.; Akbar, F.; Kanwal, F. Correlation of different spectral lights with biomass accumulation and production of antioxidant secondary metabolites in callus cultures of medicinally important Prunella vulgaris L. J. Photoch. Photobio. B 2016, 159, 1–7. [Google Scholar] [CrossRef]
- Myadelets, M.A.; Kukushkina, T.A.; Barsukova, I.N. The content of biologically active substances in Prunella vulgaris L. (lamiaceae) depending on the phase of development. Sib. Med. J. 2014, 127, 102–105. [Google Scholar]
- Qiu, H.; Zhang, J.; Guo, Q.; Zhang, Y.; Zhong, X. Prunella vulgaris L. attenuates experimental autoimmune thyroiditis by inducing indoleamine 2,3-dioxygenase 1 expression and regulatory T cell expansion. Biomed. Pharmacother. 2020, 128, 110288. [Google Scholar] [CrossRef]
- Yang, A.; Zheng, Z.; Liu, F.; Liu, J.; Wang, R.; Yang, H.; Huang, Z.; Huang, P.; Liu, H. Screening for Potential Antibreast Cancer Components from Prunellae Spica Using MCF-7 Cell Extraction Coupled with HPLC-ESI-MS/MS. Nat. Prod. Commun. 2020, 15, 1–5. [Google Scholar] [CrossRef]
- Plugatar, Y.V.; Shevchuk, O.M.; Logvinenko, L.A. Species of the genus Prunella vulgaris L. are sources of valuable biologically active substances. Agrar. Bull. Ural. 2017, 8, 37–45. [Google Scholar]
- Golembiovska, O.; Tsurkan, A.; Vynogradov, B. Components of Prunella vulgaris L. Grown in Ukraine. J. Pharmacogn. Phytochem. 2014, 2, 140–146. [Google Scholar]
- Sárosi, S.; Bernáth, J.; Burchi, G.; Antonetti, M.; Bertoli, A.; Pistelli, L.; Benvenuti, S. Effect of different plant origins and climatic conditions on the total phenolic content and total antioxidant capacity of self-heal (Prunella vulgaris L.). Acta Hortic. 2011, 925, 49–55. [Google Scholar] [CrossRef]
- Şahin, S.; Işık, E.; Demir, C. Prediction of Total Phenolic Content in Extracts of Prunella Species from HPLC Profiles by Multivariate Calibration. Int. Sch. Res. Not. 2012, 2012, 120780. [Google Scholar]
- Ahn, E.Y.; Lee, Y.J.; Park, J.; Chun, P.; Park, Y. Antioxidant Potential of Artemisia capillaris, Portulaca oleracea, and Prunella vulgaris Extracts for Biofabrication of Gold Nanoparticles and Cytotoxicity Assessment. Nanoscale Res. Lett. 2018, 13, 348. [Google Scholar] [CrossRef]
- Tosun, M.N.; Demirel Zorba, N.N.; Yüceer, Y. The anti-quorum sensing and antitumor activity of Prunella vulgaris, Sambucus nigra, Calendula officinalis: Potential use in food industry: Potential use in food industry. J. Microbiol. Biotechnol. Food Sci. 2021, 10, e2774. [Google Scholar] [CrossRef]
- Mahboubi, M.; Mahboubi, A.; Kazempour, N. The antimicrobial activity of Prunella vulgaris extracts. Herba Pol. 2015, 61, 31–38. [Google Scholar] [CrossRef][Green Version]
- Gazanfar, A.; Mubashir, H.M.; Nahida, T.; Sameer, A.M.; Mir, J.I. In vivo hepatoprotective potential of extracts obtained from floral spikes of Prunella vulgaris L. J. Ayurveda Integr. Med. 2020, 11, 502–507. [Google Scholar] [CrossRef]
- Rasool, R.; Ganai, B.A. Prunella vulgaris L.: A Literature Review on its Therapeutic Potentials. Pharmacologia 2013, 4, 441–448. [Google Scholar] [CrossRef][Green Version]
- Chi Keung Mak, W.; Walsh, S. The Anti-Viral Activity of Prunella vulgaris: A Narrative Review. Integr. Med. Rep. 2022, 1, 107–122. [Google Scholar] [CrossRef]
- Behl, T.; Rocchetti, G.; Chadha, S.; Zengin, G.; Bungau, S.; Kumar, A.; Mehta, V.; Uddin, M.S.; Khullar, G.; Setia, D.; et al. Phytochemicals from Plant Foods as Potential Source of Antiviral Agents: An Overview. Pharmaceuticals 2021, 14, 381. [Google Scholar] [CrossRef] [PubMed]
- Ao, Z.; Chan, M.; Ouyang, M.J.; Olukitibi, T.A.; Mahmoudi, M.; Kobasa, D.; Yao, X. Identification and evaluation of the inhibitory effect of Prunella vulgaris extract on SARS-coronavirus 2 virus entry. PLoS ONE 2021, 16, e0251649. [Google Scholar] [CrossRef] [PubMed]
- Ao, Z.; Chan, M.; Jing Ouyang, M.; Titus Abiola, O.; Mahmoudi, M.; Kobasa, D.; Yao, X. Prunella vulgaris extract and suramin block SARS-coronavirus 2 virus Spike protein D614 and G614 variants mediated receptor association and virus entry in cell culture system. bioRxiv 2020, 270306. [Google Scholar] [CrossRef]
- Groşan, A.; Vari, C.; Ştefănescu, R.; Danciu, C.; Pavel, I.; Dehelean, C.; Man, A.; David, R.; Vlase, L.; Muntean, L. Antibacterial and antitumor activity of the species Prunella vulgaris L. Rev. Romana Med. Lab. 2020, 28, 405–417. [Google Scholar] [CrossRef]
- Man, A.; Gâz Florea, S.A.; Mare, A.D.; Berta, L. Effects of low-molecular weight alcohols on bacterial viability. Rev. Romana Med. Lab. 2017, 25, 335–343. [Google Scholar] [CrossRef]
- Patel, J.K.; Joshi, C.K.; Sharma, M.K. Prunella vulgaris L. Potentiates Answer to the Emergence of Dreaded Antibiotic Resistance. J. Pure Appl. Microbiol. 2021, 15, 1429–1441. [Google Scholar] [CrossRef]
- Zhao, J.; Ji, D.; Zhai, X.; Zhang, L.; Luo, X.; Fu, X. Oral Administration of Prunella vulgaris L Improves the Effect of Taxane on Preventing the Progression of Breast Cancer and Reduces Its Side Effects. Front. Pharmacol. 2018, 9, 806. [Google Scholar] [CrossRef]
- Feng, L.; Jia, X.; Zhu, M.M.; Chen, Y.; Shi, F. Antioxidant activities of total phenols of Prunella vulgaris L. in vitro and in tumor-bearing mice. Molecules 2010, 15, 9145–9156. [Google Scholar] [CrossRef]
- Chen, Y.; Zhang, X.; Guo, Q.; Liu, L.; Li, C.; Cao, L.; Qin, Q.; Zhao, M.; Wang, W. Effects of UV-B Radiation on the Content of Bioactive Components and the Antioxidant Activity of Prunella vulgaris L. Spica during Development. Molecules 2018, 23, 989. [Google Scholar] [CrossRef]
- Seo, J.K.; Kang, M.-J.; Shin, J.-H.; Lee, S.-J.; Jeong, H.-G.; Sung, N.-J.; Chung, Y.-C. Antibacterial and antioxidant activities of solvent extracts from different parts of hagocho (Prunella vulgaris). J. Korean Soc. Food. Sci. Nutr. 2010, 39, 1425–1432. [Google Scholar] [CrossRef]
- Ohanyan, A.D.; Shishkoyan, N.D.; Kazaryan, S.A.; Hovhannisyan, A.A.; Tiratsuyan, S.G.; Elbekyan, K.S.; Koshel, V.I.; Khodzhayan, A.B. Antioxidant and hemolytic properties of different extracts from Prunella vulgaris L. leaves. Med. Bull. North Cauc. 2018, 13, 507–510. [Google Scholar] [CrossRef]
- Zhang, W.; Wuhan, Q.; Na, M.; Hu, R.; Mu, Q.; Bao, X. Emerging therapeutic role of Prunella vulgaris in thyroid disease. Chin. Herb. Med. 2022, 14, 403–413. [Google Scholar] [CrossRef] [PubMed]
- Han, Q.; Xu, N.; Chen, B.; Wu, W.; Sheng, L. Safety and efficacy of Prunella vulgaris preparation in adjuvant treatment of thyroid nodules: A meta-analysis. Medicine 2021, 100, e27490. [Google Scholar] [CrossRef] [PubMed]
- Gan, X.X.; Zhong, L.K.; Shen, F.; Feng, J.H.; Li, Y.Y.; Li, S.J.; Cai, W.S.; Xu, B. Network Pharmacology to Explore the Molecular Mechanisms of Prunella vulgaris for Treating Hashimoto’s Thyroiditis. Front. Pharmacol. 2021, 12, 700896. [Google Scholar] [CrossRef]
- Shen, X.; Yang, R.; An, J.; Zhong, X. Analysis of the Molecular Mechanisms of the Effects of Prunella vulgaris against Subacute Thyroiditis Based on Network Pharmacology. Evid. Based Complement. Altern. Med. 2020, 2020, 9810709. [Google Scholar] [CrossRef]
- Li, B.; Guo, J.; Wang, F.; Cheng, S.; Zeng, L. Effect of Prunella vulgaris polysaccharides on cultured orbit fibroblasts in vitro from patients with thyroid-associated ophthalmopathy. Exp. Eye Res. 2020, 201, 108276. [Google Scholar] [CrossRef] [PubMed]
- Li, B.Y.; Hu, Y.; Li, J.; Shi, K.; Shen, Y.F.; Zhu, B.; Wang, G.X. Ursolic acid from Prunella vulgaris L. efficiently inhibits IHNV infection in vitro and in vivo. Virus Res. 2019, 273, 197741. [Google Scholar] [CrossRef] [PubMed]
- Gu, X.; Li, Y.; Mu, J.; Zhang, Y. Chemical constituents of Prunella vulgaris. J. Environ. Sci. 2013, 25 (Suppl. S1), S161–S163. [Google Scholar] [CrossRef] [PubMed]
- Eskova, A.Y.; Kubyshkin, A.V.; Fomochkina, I.I. Ointment for the Treatment of Burns. Federal State Autonomous Educational Institution of Higher Education; M.V. Frunze Crimean University: Crimea, Russia, 2012. [Google Scholar]
- Gong, X.J.; Liu, W.G.; Zhong, H. Prunella tablets treatment of benign prostatic hyperplasia in 40 cases. J. Pract. Tradit. Chin. Med. 2014, 30, 964–965. [Google Scholar]
- Mo, Y.T.; Liu, P. Clinical study of prunella combined with glucocorticoids on subacute thyroiditis. Asia-Pac. Tradit. Med. 2015, 11, 119–120. [Google Scholar]
- Fan, Z.Y.; Zhang, L.L.; Mi, R. Effect of Xiakucao capsule on Hashimoto thyroiditis and the ultrasonic diagnosis of thyroid morphology before and after treatment. J. Hebei Med. Univ. 2017, 38, 446–449. [Google Scholar] [CrossRef]

| № | Compound Name | RT | Method | Solvent | Plant Part | Reference |
|---|---|---|---|---|---|---|
| 1 | Gluconic acid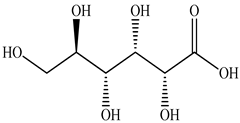 | 0.88 | UPLC-ESI-MS | Water | Spike | [47] |
| 2 | Malic acid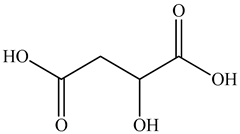 | 1.05 | UPLC-ESI-MS | Water | Spike | [47] |
| 3 | Citric acid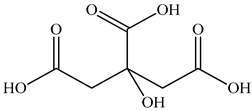 | 1.26 | UPLC-ESI-MS | Water | Spike | [47] |
| 6.58 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] | ||
| 4 | Caftaric acid 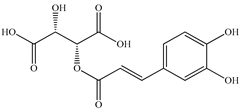 | 2.10 | HPLC-UV/MS | Methanol/Water | Seed | [36] |
| 5 | Gentisic acid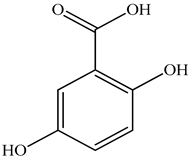 | 2.15 | HPLC-UV/MS | Methanol/Water | Seed | [36] |
| 6 | Danshensu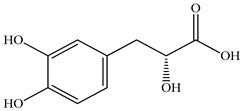 | 2.62 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 7 | Long-chain fatty acid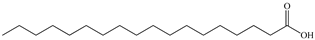 | 2.65 | UPLC-ESI-MS | Water | Spike | [47] |
| 8 | Protocatechuic acid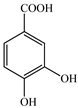 | 3.25 | UPLC-ESI-MS | Water | Spike | [47] |
| 5.79 | HPLC-ESI-MS/M | Water | Spike | [48] | ||
| 9 | m-Dimethylbenzene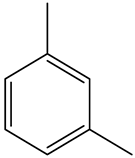 | 4.76 | GC-MS | Ethyl acetate | Spike | [30] |
| 10 | Protocatechuic aldehyde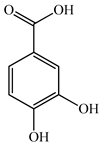 | 5.85 | UPLC-ESI-MS | Water | Spike | [47] |
| 7.06 | HPLC-ESI-MS/M | Water | Spike | [48] | ||
| 11 | Chlorogenic acid 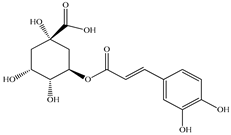 | 5.01 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 5.6 | HPLC-UV/MS | Methanol/Water | Seed | [36] | ||
| 13.01 | HPLC | Ethanol/Water | Aerial part | [49] | ||
| 12 | Thymine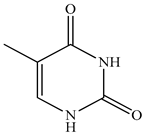 | 5.39 | GC-MS | Methanol | Whole plant | [29] |
| 13 | Dihydrocaffeic acid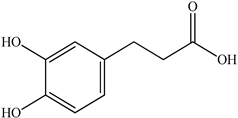 | 5.65 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 14 | Caffeic acid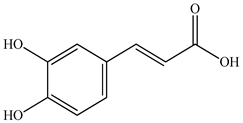 | 5.6 | HPLC-UV/MS | Methanol/Water | Seed | [36] |
| 6.67 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] | ||
| 8.46 | HPLC-ESI-MS/M | Water | Spike | [48] | ||
| 9.17 | UPLC-ESI-MS | Water | Spike | [47] | ||
| 14.08 | HPLC | Ethanol/Water | Aerial part | [49] | ||
| 20.99 | HPLC | Methanol | Seed | [22] | ||
| 15 | Esculetin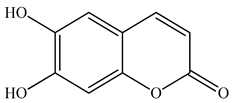 | 5.85 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 16 | Trans-caran | 6.13 | GC-MS | Hexane | Whole plant | [29] |
| 17 | 2-dodecan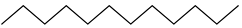 | 6.2 | GC-MS | Ethyl acetate | Whole plant | [29] |
| 18 | Coumaran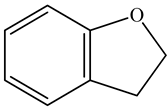 | 6.43 | GC-MS | Methanol | Whole plant | [29] |
| 19 | 5-hydroxymethylfurfural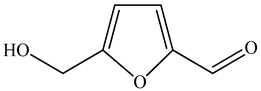 | 6.53 | GC-MS | Methanol | Whole plant | [29] |
| 20 | Carvacrol | 7.05 | GC-MS | Hexane | Whole plant | [29] |
| 7.14 | GC-MS | Ethyl acetate | Whole plant | [29] | ||
| 21 | Thymol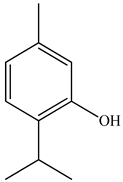 | 7.05 | GC-MS | Ethyl acetate | Whole plant | [29] |
| 7.14 | GC-MS | Hexane | Whole plant | [29] | ||
| 22 | Eugenol methylether | 8.25 | GC-MS | Methanol | Whole plant | [29] |
| 23 | P-Coumaric acid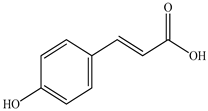 | 8.7 | HPLC-UV/MS | Methanol/Water | Seed | [27] |
| 24 | 2-hydroxy-5-methylbenzaldehyde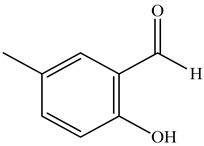 | 8.7 | GC-MS | Methanol | Whole plant | [29] |
| 25 | D-Limonene | 8.5 | GC-MS | Water | Roots | [50] |
| 9.61 | GC-MS | Ethyl acetate | Spike | [30] | ||
| 26 | Mangiferin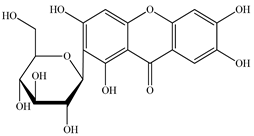 | 9.96 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 27 | Isorosmarinic acid glycoside | 10.05 | UPLC-ESI-MS | Water | Spike | [47] |
| 28 | Scopoletin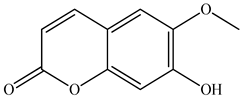 | 10.78 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 29 | Rosmarinic acid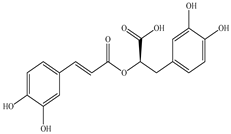 | 10.88 | UPLC-ESI-MS | Water | Spike | [47] |
| 12.08 | HPLC-ESI-MS/M | Water | Spike | [48] | ||
| 20.51 | HPLC | Ethanol/Water | Aerial part | [49] | ||
| 21.09 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] | ||
| 33.1 | HPLC | Methanol | Seed | [22] | ||
| 30 | Linalool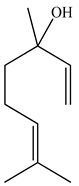 | 11.48 | GC-MS | Ethyl acetate | Roots | [50] |
| 31 | Ferulic acid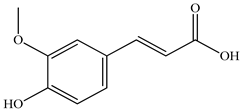 | 12.10 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 12.2 | HPLC-UV/MS | Methanol/Water | Seed | [36] | ||
| 32 | Ursolic acid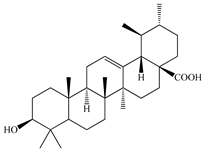 | 12.10 47.21 | UPLC-ESI-MS UPLC-ESI-MS | Water Ethanol/Water | Spike Whole plant | [47] [27] |
| 33 | Isoorientin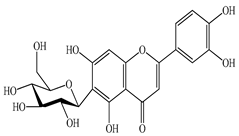 | 12.47 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 34 | Dihydroferulic acid | 14.05 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 35 | Caprylic acid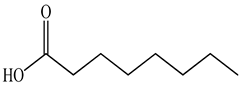 | 14.13 | GC-MS | Ethyl acetate | Leaves | [50] |
| 36 | Jacoesidin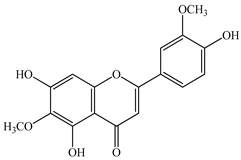 | 14.58 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 37 | Cynaroside | 15.88 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 38 | Hyperoside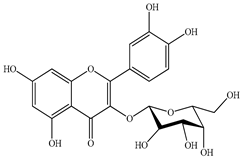 | 16.26 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 18.6 | HPLC-UV/MS | Methanol/Water | Seed | [36] | ||
| 39 | Rutin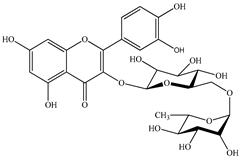 | 16.92 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 19.76 | HPLC | Ethanol/Water | Aerial part | [49] | ||
| 20.2 | HPLC-UV/MS | Methanol/Water | Seed | [36] | ||
| 40 | Lavandulol acetate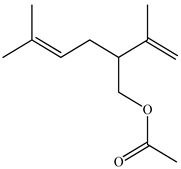 | 17.26 | GC-MS | Ethyl acetate | Whole plant | [29] |
| 41 | β-Cyclocitrale 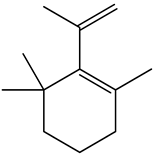 | 17.31 | GC-MS | Ethyl acetate | Leaves | [50] |
| 42 | Salviaflaside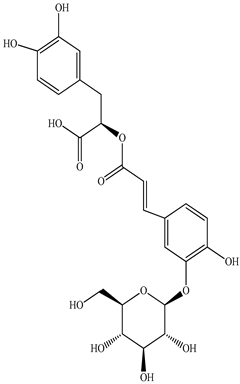 | 17.76 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 29.2 | HPLC | Methanol | Seed | [22] | ||
| 43 | Genistein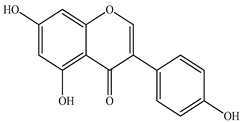 | 18.5 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 44 | Hesperidin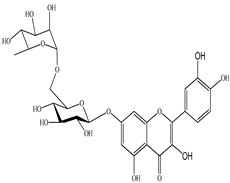 | 19.08 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 45 | Isoquercitrin  | 19.6 | HPLC-UV/MS | Methanol/Water | Seed | [36] |
| 46 | Abscisic acid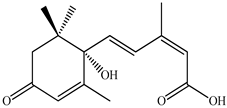 | 19.19 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 47 | Kaempferol-7-O-glucoside | 19.56 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 48 | β-Bourbonene 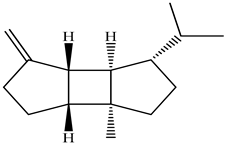 | 19.98 | GC-MS | Ethyl acetate | Leaves | [50] |
| 49 | Quercitin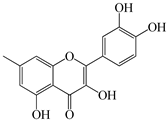 | 20.24 | HPLC | Ethanol/Water | Aerial part | [49] |
| 23.0 | HPLC-UV/MS | Methanol/Water | Seed | [36] | ||
| 50 | Methyl caffeate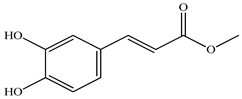 | 21.22 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 51 | β-Farnesene 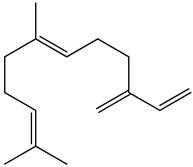 | 21.56 | GC-MS | Ethyl acetate | Roots | [50] |
| 52 | Humulene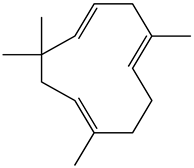 | 22.01 | GC-MS | Ethyl acetate | Roots | [50] |
| 53 | γ-Nonalactone (Prunolide)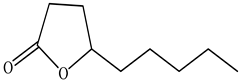 | 22.31 | GC-MS | Ethyl acetate | Stems | [50] |
| 54 | Geranyl acetone 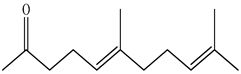 | 22.53 | GC-MS | Ethyl acetate | Stems | [50] |
| 55 | Germacren D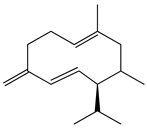 | 22.66 | GC-MS | Ethyl acetate | Leaves | [50] |
| 56 | Cyanidin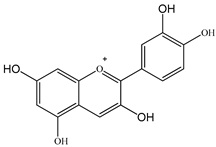 | 24.97 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 57 | Phytol | 25.13 | GC-MS | Ethyl acetate | Whole plant | [29] |
| 25.15 | GC-MS | Methanol | Whole plant | [29] | ||
| 58 | Spathulenol | 25.23 | GC-MS | Ethyl acetate | Flowers, leaves | [50] |
| 59 | Ethyl caffeate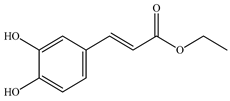 | 25.34 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 60 | Quercetol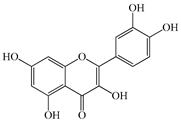 | 26.8 | HPLC-UV/MS | Methanol/Water | Seed | [36] |
| 61 | Myristic acid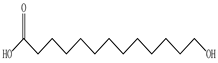 | 27.15 | GC-MS | Ethyl acetate | Leaves, stems, roots | [50] |
| 62 | Acacetin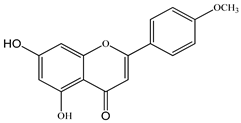 | 27.81 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 63 | Methyl rosinate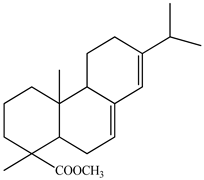 | 28.44 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 64 | Pentadecane | 28.80 | GC-MS | Ethyl acetate | Spike | [30] |
| 65 | Luteolin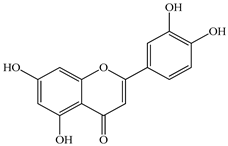 | 29.64 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 66 | Kaempferol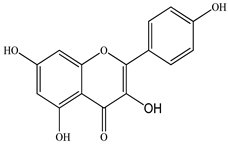 | 31.6 | HPLC-UV/MS | Methanol/Water | Seed | [36] |
| 32.79 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] | ||
| 67 | Ethyl rosemary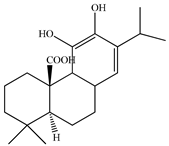 | 32.38 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 68 | Hexadecane | 23.18 | GC-MS | Ethyl acetate | Flowers, leaves, stems, roots | [50] |
| 32.53 | GC-MS | Ethyl acetate | Spike | [30] | ||
| 69 | Apigenin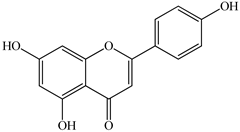 | 33.1 | HPLC-UV/MS | Methanol/Water | Seed | [36] |
| 33.51 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] | ||
| 70 | Daidzein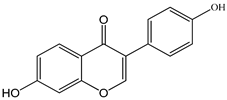 | 35.93 | UPLC-MS/MS | Ethanol/Water | Whole plant | [36] |
| 71 | Heptadecane | 24.84 | GC-MS | Ethyl acetate | Flowers, leaves, stems, roots, spikes | [50] |
| 32.53 | GC-MS | Ethyl acetate | [30] | |||
| 72 | Amolsamic acid A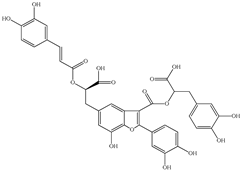 | 40.2 | HPLC | Methanol | Seed | [22] |
| 73 | Amolsamic acid B | 41.6 | HPLC | Methanol | Seed | [22] |
| 74 | Prunelloside A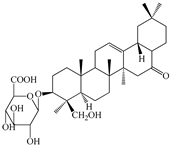 | 46.09 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 75 | Maslinic acid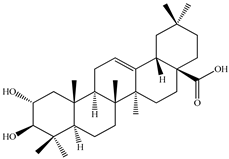 | 46.33 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 76 | Corosolic acid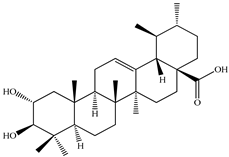 | 46.74 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 77 | Oleanic acid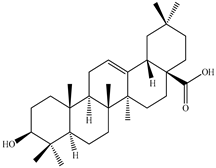 | 46.95 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] |
| 78 | Linolenic acid | 25.90 | GC-MS | Methanol | Whole plant | [29] |
| 25.92 | GC-MS | Ethyl acetate | Whole plant | [29] | ||
| 25.99 | GC-MS | Hexane | Whole plant | [29] | ||
| 47.02 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] | ||
| 79 | Linoleic acid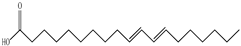 | 25.70 | GC-MS | Methanol | Whole plant | [29] |
| 25.72 | GC-MS | Ethyl acetate | Whole plant | [29] | ||
| 25.79 | GC-MS | Hexane | Whole plant | [29] | ||
| 47.45 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] | ||
| 51.18 | GC-MS | Ethyl acetate | Spike | [30] | ||
| 80 | Palmitic acid 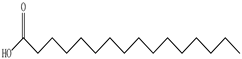 | 20.73 | GC-M | Methanol | Whole plant | [29] |
| 20.74 | GC-MS | Ethyl acetate | Whole plant | [29] | ||
| 20.8 | GC-MS | Hexane | Whole plant | [29] | ||
| 29.84 | GC-MS | Ethyl acetate | Leaves | [50] | ||
| 45.67 | GC-MS | Ethyl acetate | Spike | [30] | ||
| 47.90 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] | ||
| 81 | Oleic acid 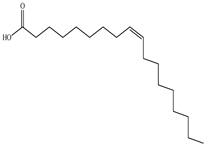 | 32.15 | GC-MS | Ethyl acetate | Leaves, roots | [50] |
| 48.01 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] | ||
| 82 | Stearic acid | 26.52 | GC-MS | Ethyl acetate | Whole plant | [29] |
| 26.55 | GC-MS | Methanol | Whole plant | [29] | ||
| 48.82 | UPLC-MS/MS | Ethanol/Water | Whole plant | [27] | ||
| 83 | Squalene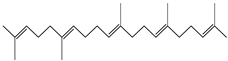 | 38.7 | GC-MS | Ethyl acetate | Flowers, roots | [50] |
| 67.36 | GC-MS | Ethyl acetate | Whole plant | [29] |
| Type of Extract | Plant Part | Strain | MIC | MBC | Reference |
|---|---|---|---|---|---|
| Organic Fraction of PV | Herb | S. aureus ATCC3953 | 256 mg/mL | - | [8] |
| S. aureus ATCC4223 | 128 mg/mL | - | |||
| Methanolic | Leaves | K. pneumoniae ATCC13883 | 25 mg/mL | 50 mg/mL | [63] |
| E. coli ATCC25922 | 50 mg/mL | 50 mg/mL | |||
| P. aeruginosa ATCC27853 | 12.5 mg/mL | 50 mg/mL | |||
| MRSA ATCC 43300 | 25 mg/mL | 25 mg/mL | |||
| Flowers | K. pneumoniae ATCC13883 | 25 mg/mL | 25 mg/mL | [63] | |
| E. coli ATCC25922 | 25 mg/mL | 25 mg/mL | |||
| P. aeruginosa ATCC27853 | 6.25 mg/mL | 25 mg/mL | |||
| MRSA ATCC 43300 | 25 mg/mL | 25 mg/mL | |||
| Aqueous | Leaves | K. pneumoniae ATCC13883 | >50 mg/mL | >50 mg/mL | [63] |
| E. coli ATCC25922 | >50 mg/mL | >50 mg/mL | |||
| P. aeruginosa ATCC27853 | >50 mg/mL | >50 mg/mL | |||
| MRSA ATCC 43300 | >50 mg/mL | >50 mg/mL | |||
| Flowers | K. pneumoniae ATCC13883 | 50 mg/mL | >50 mg/mL | [63] | |
| E. coli ATCC25922 | >50 mg/mL | >50 mg/mL | |||
| P. aeruginosa ATCC27853 | 25 mg/mL | >50 mg/mL | |||
| MRSA ATCC 43300 | >50 mg/mL | >50 mg/mL | |||
| Aqueous | Whole plant | E. coli ATCC25922 | 2 μg/mL | - | [19] |
| Ethanolic | Whole plant | E.coli ATCC25922 | 1.33 μg/mL | - | [19] |
| Ethyl acetate | Whole plant | C. perfringens | 1.56 μg/mL | - | [29] |
| S. aureus | 6.25 μg/mL | - | |||
| E. coli | 0.195 μg/mL | - | |||
| S. marcescens | 6.25 μg/mL | - | |||
| K. pneumoniae | 0.78 μg/mL | - | |||
| P. aeruginosa | 1.56 μg/mL | - | |||
| Hexane | Whole plant | C. perfringens | 6.25 μg/mL | - | [29] |
| S. pyogenes | 3.12 μg/mL | - | |||
| S. typhimurium | 1.56 μg/mL | - | |||
| E. coli | 6.25 μg/mL | - | |||
| P. vulgaris | 3.12 μg/mL | - | |||
| P. aeruginosa | 6.25 μg/mL | - | |||
| Methanolic | Whole plant | B. cereus | 1.56 μg/mL | - | [29] |
| C. perfringens | 6.25 μg/mL | - | |||
| S. marcescens | 6.25 μg/mL | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zholdasbayev, M.E.; Atazhanova, G.A.; Musozoda, S.; Poleszak, E. Prunella vulgaris L.: An Updated Overview of Botany, Chemical Composition, Extraction Methods, and Biological Activities. Pharmaceuticals 2023, 16, 1106. https://doi.org/10.3390/ph16081106
Zholdasbayev ME, Atazhanova GA, Musozoda S, Poleszak E. Prunella vulgaris L.: An Updated Overview of Botany, Chemical Composition, Extraction Methods, and Biological Activities. Pharmaceuticals. 2023; 16(8):1106. https://doi.org/10.3390/ph16081106
Chicago/Turabian StyleZholdasbayev, Mussa E., Gayane A. Atazhanova, Safol Musozoda, and Ewa Poleszak. 2023. "Prunella vulgaris L.: An Updated Overview of Botany, Chemical Composition, Extraction Methods, and Biological Activities" Pharmaceuticals 16, no. 8: 1106. https://doi.org/10.3390/ph16081106
APA StyleZholdasbayev, M. E., Atazhanova, G. A., Musozoda, S., & Poleszak, E. (2023). Prunella vulgaris L.: An Updated Overview of Botany, Chemical Composition, Extraction Methods, and Biological Activities. Pharmaceuticals, 16(8), 1106. https://doi.org/10.3390/ph16081106








