Abstract
Amitriptyline was first introduced as a medication to treat depression. Over time, this substance has been used to treat other conditions, such as gastrointestinal disorders, fibromyalgia, neuropathic pain, and analgesia, among others. However, there are no published studies that provide a broad view of the possible motivations that have led to changes in the use of amitriptyline. In this study, we have identified the landscape of use for amitriptyline based on knowledge mapping of the 100 most-cited articles about this drug. We searched Web of Science Core Collection without time and language restrictions. We obtained 14,446 results, but we only used the 100 most-cited articles that had amitriptyline as the object of study. We collected the following information from each article: authors, country of the corresponding authors, year of publication, citation count, citation density (number of citations per year), and keywords. In addition, we seek to map in the chosen articles study design and research findings. We found that since 1980, the use of amitriptyline has expanded beyond depression, moving to off-label use to treat a variety of diseases and conditions, including post-herpetic neuralgia, neuropathic pain, primary fibrosis, fibromyalgia, and migraine, can be considered a drug with more clinical applicability than its original clinical indication.
1. Introduction
Amitriptyline [3-(10,11-dihydro-5Hdibenzo[a,d][7]annulen-5-ylidene)-N,N-dimethylpropan-1-amine], is a synthetic drug belonging to the class of tricyclic antidepressants (TCAs), characterized by the presence of three carbon rings in its structure (Figure 1). This drug is commonly used to treat depressive disorders and was introduced in the U.S. market in the early 1960s and is still used today, being referenced in the 2021 WHO List of Essential Medicines [1,2].
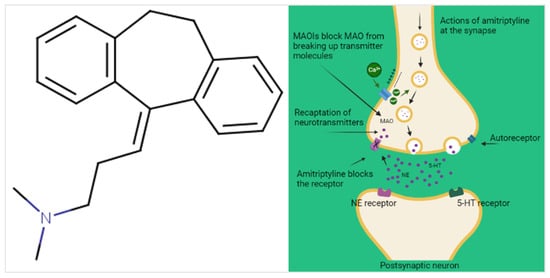
Figure 1.
The molecular structure of amitriptyline and its mechanism of action in depression.
It is mainly used in the form of amitriptyline hydrochloride, appearing as water-soluble white crystals, orally administered, with high absorption in the gastrointestinal tract, providing an initial bioavailability of 90–95%. However, amitriptyline undergoes intense hepatic first-pass metabolism, which reduces its availability to about 53%. Its main hepatic metabolite, nortriptyline, retains similar pharmacological properties [3,4,5].
First pharmacodynamic evidence of amitriptyline activity reveals its ability to block serotonin and noradrenaline reuptake in adrenergic and serotonergic neuronal terminals, identified as the main mechanisms associated with its antidepressant effect. Activity on noradrenergic, serotonergic, muscarinic, histaminergic, and opioid receptors, among others, has also been described, often related to its sedative effect adverse reactions, and ‘off-label’ indications [3,6]. Despite being formally registered for depressive disorders pharmacotherapy, since the 1980s, amitriptyline began to be used for other clinical applications, with an emphasis on painful conditions such as neuropathic pain and fibromyalgia, in addition to non-organic nocturnal enuresis, and non-motor Parkinson’s symptoms, among many others [6,7].
Therefore, an important trend of transformation in the patterns of amitriptyline use can be seen, with possible repositioning in therapy, but the scientific literature still lacks evidence to support the long list of different clinical applicabilities in practice, especially in ‘off-label’ use. Thus, this study aims to map the most cited studies focused on amitriptyline and its applicability, highlighting the knowledge produced, the evolution of amitriptyline use, and the gaps that need to be filled.
2. Results
2.1. Selected Studies and Bibliometric Analysis
Our search strategy produced 14,446 articles. After organizing the articles in descending order based on the number of citations, we evaluated a total of 189 articles. Of these, we selected 100 articles that met the eligibility criteria and excluded 89 because they did not meet the objective of this work (Figure 2).
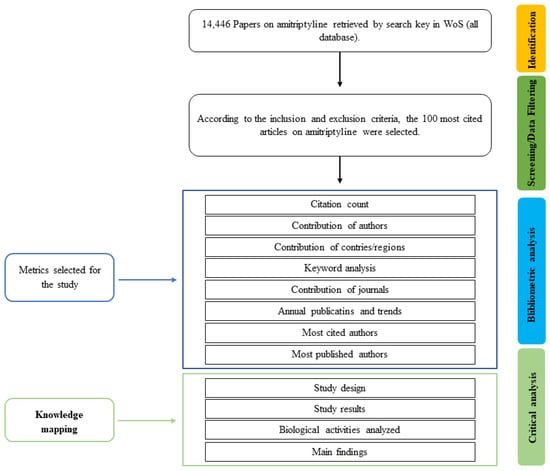
Figure 2.
Flowchart of article screening.
The 100 selected articles were cited a total of 41,707 times. Authors A. Cipriani, R. Dubner, M.B. Max, B. Smoller, K. Fuxe, and E.S. Paykel published the most articles on the use of amitriptyline, with three articles each. The most cited article, among the 100 studies, was that by Steru et al., 1985 [8], entitled “The tail suspension test: a new method for scree of antidepressants in mice,” had been cited 2671 times. The least cited article was by Guyatt et al. entitled “The n-of-1 randomized controlled trial: clinical usefulness; since its publication in 1990, it has been cited 256 times. (Table 1).

Table 1.
The 100 most-cited articles on amitriptyline.
2.1.1. Publication Year
The selected articles were published between 1968 and 2018. We divided this range into 10-year periods and determined the number of papers for each period and the total number of citations that these articles received up to the time of data collection. Most of the articles were published between 1999 and 2008 (n = 39), which represents more than double the second period with more publications, however, this decade had the lowest citation density, with 384.21 citations per article (cit./art.). Articles published between 2009 and 2018 had the highest citation density, with 495.58 cit./art., also being the decade with the lowest number of articles published (Table 2).

Table 2.
Publication periods of the 100 most-cited articles on amitriptyline.
2.1.2. Journal of Publication
The 100 articles selected were published in 58 journals. The journal with more contributions was “Archives of general psychiatry” (n = 9; 2981 citations; 331.22 cit./art.) followed by “Neurology” (n = 7; 2671 citations; 381.57 cit./art.) and “Pain” (n = 5; 2051 citations; 410.2 cit./art.). The journal of publication most cited was “Psychopharmacology” (n = 3; 3230 citations; 1076.67 cit./art.) (Figure 3).
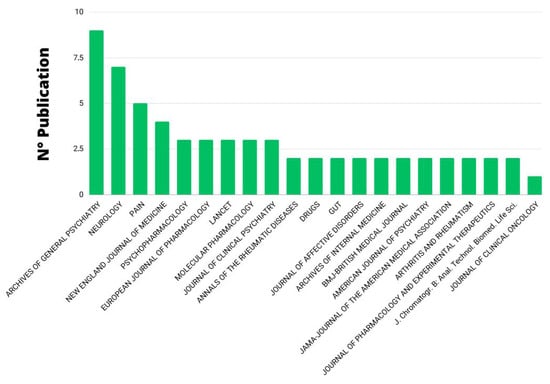
Figure 3.
Journal of publication with at least two articles.
2.1.3. Contributing Authors
Overall, there are a total of 493 authors among the 100 most-cited articles, with Steru, L, the most cited author in the Web of Science Core Collection (2671 citations). Cipriani, A.; Dubner, R.; Max, M.B.; Smoller, B.; Fuxe, K., and Paykel E.S. have published the most articles on the use of amitriptyline, with three articles each. In their study, Max, M.B. discussed the use of amitriptyline to treat diabetic neuropathy [10]. Cipriani A, and Paykel E.S., investigated the use of amitriptyline for depression [9,53]. Carlsson, A. and Fuxe, K. evaluated the ability of amitriptyline and other tertiary amines to block 5-hydroxytyramine uptake at central terminals [13].
The most cited study was by the author Steru, L. [8], with the title “The tail suspension test: a new method for the screening of antidepressants in mice” which had been cited 2671 times.
The second article with the most citations is by Cipriani, A., entitled “Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis” [9].
The least cited article among the top 100 studies was by author Lidbrink, P. [106] entitled “The effect of imipramine-like drugs and antihistamine drugs on uptake mechanisms in the central noradrenaline and 5-hydroxytryptamine neurons”, with a total of 245 citations. The author reports in his work that amitriptyline preferentially blocks 5-hydroxytryptamine receptors in central 5-hydroxytryptamine neurons.
We used VOSviewer to visualize the authorship citation density (Figure 4) and relationships between authors with the most links (Figure 5).
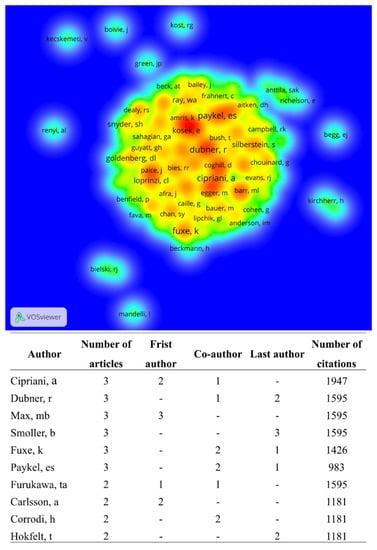
Figure 4.
Visualization of authorship citation density. The colors indicate the author’s citation density, ranging from blue (lowest density) to red (highest density). The 493 authors formed 85 clusters. Authors with the highest number of published papers are identified, as are those with the highest number of citations, in order.
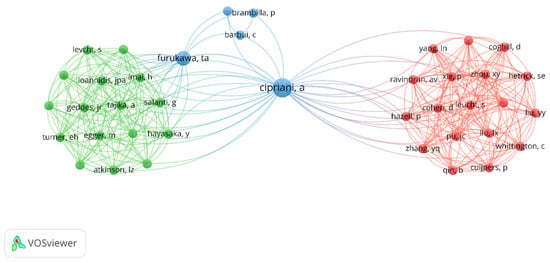
Figure 5.
View of the network of author connections for the top 100 most cited articles on amitriptyline. The node size represents the number of publications. Nodes with the same colors represent the same cluster. Furthermore, the greater the link thickness and the smaller the distance between nodes, the greater the relative strength of the relationship. The colors are represented by blue, green, and red and interconnect the intensities of interactions.
2.1.4. Keyword Network
In the 100 most-cited articles, there were 556 author keywords, behind ‘Double-blind’ (n = 16) and ‘Amitriptyline’ (n = 16), followed by ‘antidepressants’ (n = 10) and ‘placebo-controlled’ trial (n = 9) the most used (Figure 6). As amitriptyline is an antidepressant, the word antidepressant is also prominent in the network. Most of the studies were double-blind randomized clinical trials that addressed the use of amitriptyline or compared the effectiveness of amitriptyline with other TCAs such as imipramine and selective serotonin reuptake inhibitor antidepressants such as fluoxetine. Because amitriptyline can be used to treat pain and neuropathic diabetes, those words are also present in the keyword network.
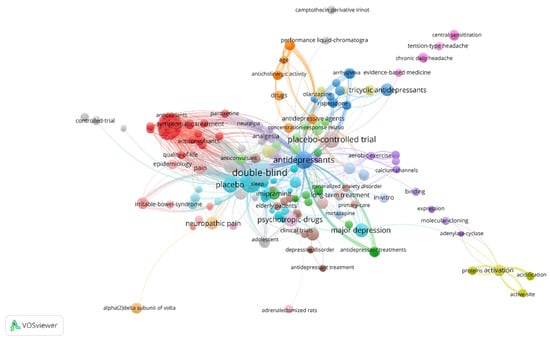
Figure 6.
Keyword network. The node size represents the keyword frequency. Nodes with the same color are part of the same cluster. The thicker the link and the smaller the distance between the nodes, the greater the relative strength of the relationship.
2.1.5. Distribution Map of the 100 Most-Cited Articles
Authors from North America, specifically the United States and Canada, are responsible for the majority of the 100 most-cited articles (n = 55), totaling 20,342 citations. Authors from European countries have also had a significant impact with 18,974 citations from 40 papers, with the most articles by authors from the United Kingdom (n = 16), Germany (n = 8), and Sweden (n = 3). On the other hand, there have been fewer articles from Asia and Oceania (Figure 7).
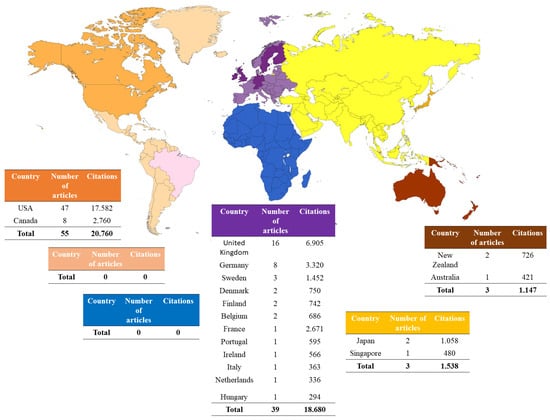
Figure 7.
Worldwide distribution of the 100 most cited articles on amitriptyline.
2.2. Content Analysis
2.2.1. Study Design
Regarding study types, the literature reviews were the most frequent (n = 31; totaling 11,968 citations). Randomized clinical trials appear as the second most frequent type of study in the top 100 (n = 18; totaling 6537 citations); in vivo animal studies come right after randomized clinical trials (n = 16; with 8116 citations). Next come the systematic reviews, also with a significant number of studies (n = 13; with 6162 citations) (Table 3).

Table 3.
Study types of the 100 most-cited articles on amitriptyline.
As previously demonstrated, the most cited article presents a murine model of depressive-like behavior, based on the tendency of rats to assume an immobility behavior when kept suspended by the tail for a prolonged period. The authors demonstrate that antidepressant drugs, including amitriptyline, reduce the immobility time of animals [107].
2.2.2. Application of Amitriptyline
Of the most cited articles, 69 discussed the indication for the use of amitriptyline involving both human beings and animals, with 32 articles focusing on its official indication for depressive disorder and 37 on other indications not regulated by the registration bodies. Figure 8 shows the main indications over the years, from 1971 (the first article on use) to 2018 (the year of the last article).
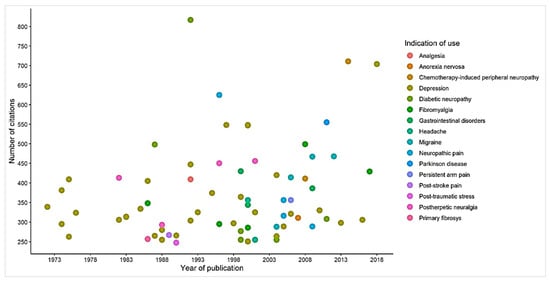
Figure 8.
Knowledge mapping of the indication for the use of amitriptyline.
Aiming to favor the analysis and interpretation of the central theme and relevance of the studies focused on the clinical application of amitriptyline, in Figure 9 we present the number of articles published in each year (Figure 9A), excluding the years in which there were no publications of selected articles, and the number of citations that the items received (Figure 9B).
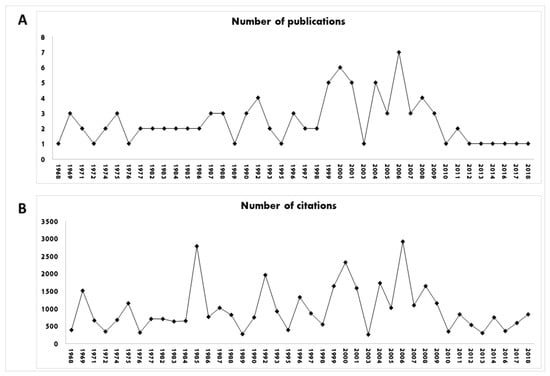
Figure 9.
Number of publications (A) and number of citations (B) of the studies during the years. Years in which there were no publications were excluded.
The other 31 articles selected were aimed at elucidating pharmacokinetic or pharmacodynamic aspects of amitriptyline through in vitro techniques. In 1969, Ross et al. [61] reported that amitriptyline was more active than nortriptyline, its metabolite, in inhibiting 5-hydroxytryptamine uptake in brain tissue in an in vitro study. This study obtained a total of 336 citations in WoS (Core Collection).
The work of the author Ueng Y.F. (1997; 316 citations) is focused on the study of drug biotransformation mechanisms by P450 3A4, the most abundant P450 enzyme in the liver and small intestine and has an important role in amitriptyline biotransformation, as well as other drugs. In it, an in vitro P450 3A4 reconstitution system capable of reflecting the catalytic specificity of liver microsomes was used. The study demonstrates the cooperativity pattern in the oxidation of amitriptyline, testosterone, 17β-estradiol and, more notably, aflatoxin (FA) B1 and the influence of alpha-naphthoflavone in this process. However, no clear differences in patterns of reductase dependence of activities in relation to NADPH-P450 concentration have been reported with either AFB1, amitriptyline, or 17β-estradiol as a substrate [67].
Another of these studies that did not have a clinical intervention, is by the author Pancrazio, J.J., published in 1998, totaling 251 citations. Through the patch-clamp technique, applied to bovine adrenal chromaffin cells, this author was able to determine in vitro that TCAs, including amitriptyline, triggered effects on sodium (Na+) channels similar to local anesthetic behavior, a mechanism that may contribute to understanding analgesic properties [105].
Studies In Vivo
In the preclinical studies included, the oldest study was published in 1969, which investigated the antidepressant effects of amitriptyline, and the most recent among this type of study was published in 2008, where the anticholinergic action of several drugs was evaluated, including amitriptyline. Overall, we retrieved 15 in vivo studies, and it is possible to note that the greatest research interest is in antidepressant effects (n = 9). However, we can point out that other objects of the investigation were also discussed, such as diabetic neuropathy (n = 1), cystic fibrosis (n = 1), migraine (n = 1), anticholinergic investigation (n = 1), inhibition, and catecholamine uptake (n = 2).
Among these in vivo studies, the most cited (n = 2671) was that of the author Steru et al. (1985), with the theme entitled “The tail suspension test—a new method for antidepressant screening in mice”. In this work, the author used a method that places the mouse suspended by the tail to test antidepressants by recording its movements. This test had a total duration of 6 min, divided into periods of immobility and agitation. As a result of this study, it was possible to observe that antidepressants, including amitriptyline, are able to decrease the duration of immobility in mice [8].
The second most cited (722) article among in vivo animal studies corresponds to the author Carlsson et al. (1969), entitled “Effect of antidepressant drugs on depletion of intraneuronal brain 5-hydroxytryptamine stores caused by 4-methyl-alpha-ethyl-meta-tyramine”. This study used mice to inject 4-methyl-alpha-ethyl-meta-tyramine in two doses of 100mg/kg intraperitoneally. After a period of four hours, the animals were euthanized to remove their brains for later analysis. After performing the analyses, the author suggested that 5-HT reuptake blockade is probably involved in the mood-elevating action of tricyclic antidepressants, including amitriptyline. On the other hand, the author suggests that the blockade of noradrenaline reuptake promotes the impulse in the depressed patient [108].
The third most cited article (n = 484), “Studies on the distinction between uptake inhibition and release of [h-3] dopamine in rat brain tissue slices,” is authored by Heikkila et al. (1975). This document evaluated the confusion over the classification of drugs as uptake inhibitors or biogenic amine-releasing agents by analyzing rat brain slices (neostriatum and cortex). It was possible through this study to conclude that, in the tissue analysis, it was possible to observe a real release experimentally (action not materially affected by the reuptake blockade); on the other hand, a releasing action evoked an apparent inhibition of the uptake of magnitude equal to the releasing action of these agents inhibitors, including amitriptyline [27].
Among these studies, the least cited article (n = 259) was by Green et al. (1977), who published the article “Tricyclic antidepressant drugs block histamine h-2 receptor in the brain”, which used four tricyclic antidepressants, including amitriptyline, to be tested on the H2 receptor that is linked to adenylate cyclase in homogenates of the hippocampus and cortex of adult pigs. The author suggested that tricyclic antidepressants, including amitriptyline, exert competitive histamine H2 antagonist activity [101].
Randomized Clinical Trials, Non-Randomized and Systematic Review
A change in study subjects on the clinical use of amitriptyline has been observed over the years. From 1973 to 2018, a wide range of studies pointed to the use of this drug to treat conditions other than depression. The study published by Radley et al. [23], that received 522 citations, identified amitriptyline hydrochloride as the second drug with the highest proportion of off-label use, corresponding to 81% of the drug prescriptions evaluated, using US-FDA registration as a reference.
Randomized placebo-controlled clinical trials have demonstrated the efficacy of amitriptyline in treating painful conditions, including fibromyalgia and neuropathies, such as postherpetic, diabetic, or chemotherapy-related neuropathies, and chronic arm pain, among others. We also identified studies that investigated the application of amitriptyline for post-traumatic stress treatment.
Of this top 100, we had a total of 18 randomized clinical trials that had amitriptyline as the object of study, 13 systematic reviews, and three non-randomized clinical trials. We will highlight some of the most cited studies in the text and Figure 10.
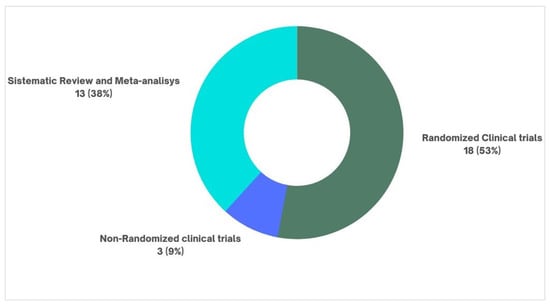
Figure 10.
Clinical studies and systematic reviews.
Among selected articles, the first randomized clinical trial aimed at evaluating the amitriptyline use in a specific painful condition was published in 1982, with the theme “Amitriptyline versus placebo in postherpetic neuralgia”. In it, Watson, C.P. evaluated 24 patients who received amitriptyline (median dose = 75 mg) or placebo, identifying good to excellent pain relief in 16 of the 24 patients (p ≤ 0.001), not associated with an antidepressant effect. Thus, the author concluded that amitriptyline is useful in the treatment of PHN [51]. A second study focused on the treatment of PHN, authored by Max M.B., in 1988, evaluated 58 patients treated for 6 weeks with amitriptyline (12.5–150 mg/day), lorazepam (0.5–6 mg/day) or placebo. They identified pain relief in 47% of patients receiving amitriptyline versus 16% in the placebo group. Greater relief was identified at higher doses [82].
In the article “A randomized, controlled trial of amitriptyline and naproxen in the treatment of patients with fibromyalgia”, published in 1986, receiving 354 citations, Goldenberg et al., followed 62 patients, divided into 4 groups, comparing 6 weeks of treatment with amitriptyline, naproxen, or amitriptyline + naproxen with a group that received placebo. Amitriptyline (25 mg/kg at night) alone promoted significant improvement in pain, sleep difficulty, fatigue on awakening and tender points score [58].
The study titled “Effects of Desipramine, Amitriptyline, and Fluoxetine on Pain in Diabetic Neuropathy” (1987) by author Max, M.B. compared amitriptyline (12.5 to 150 mg/day) with other drugs in the treatment of painful diabetic neuropathy. This study was performed on 84 patients, who were separated, allowing comparison between drugs. 74% of patients treated with amitriptyline experienced moderate to complete pain relief, significantly greater than placebo, regardless of the presence of depression [25].
In one randomized clinical trial, 46 veterans with chronic post-traumatic stress disorder were treated with amitriptyline or placebo for 8 weeks. The best results were seen on the Hamilton Depression Scale at 4 and 8 weeks, where amitriptyline was superior to placebo. However, there was no evidence of an effect based on the interview to diagnose post-traumatic stress disorder [104].
Therefore, although the study on the use of amitriptyline to treat depressive disorders concentrates the largest number of publications, in the selected top 100, we found more randomized clinical studies exploring other applications of the drug.
Regarding systematic reviews, the most cited studies were by the authors Cipriani, A., and Hershman, D.L., followed by the author McQuay, H.J. The authors had 842, 789, and 636 citations, respectively. Cipriani, A., was the author with the highest number of citations among the top 100 systematic reviews [54] with the theme entitled “Comparative effectiveness and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis”, with a total of 842 citations. The author described that antidepressants, including amitriptyline, were more effective than a placebo in adults with major depressive disorder.
Hershman D.L., author of the work “Prevention and Management of Chemotherapy-Imposed Peripheral Neuropathy in Survivors of Adult Cancers: American Society of Clinical Oncology Practice Guideline”, published in 2014 and totaling 789 citations, obtained the second-highest number among systematic reviews. From the analysis of 48 randomized clinical trials (RCTs), which addressed the treatment of chemotherapy-induced peripheral neuropathy (CIPN) in adult cancer survivors, it listed recommended and not recommended drugs for prevention or treatment. It concluded that amitriptyline should not be indicated for the prevention of neuropathy. Regarding the treatment, he stated that there is no evidence of specific benefits, but that it could be used based on its effectiveness for other conditions of neuropathic pain [11].
In a similar vein, in the study “Systematic review of antidepressants in neuropathic pain”, published in 1996 by McQuay, H.J., which received 636 citations, 17 randomized controlled trials were reviewed that explored the safety and efficacy of the antidepressants used in the treatment of painful neuropathic conditions, such as diabetic neuropathy, atypical facial pain, and PHN. It identified an average pain relief of ~50%, with 30% of patients having minor adverse reactions and 4% having to interrupt treatment due to more severe reactions. The study concludes that antidepressants, including amitriptyline, are effective in the treatment of neuropathic pain when compared with placebo [15].
3. Discussion
Using bibliometric analysis, we have provided an overview of the scientific interest and trends in the use of amitriptyline over the years and the academic impact of these studies (based on the number of citations). The selected studies have different levels of scientific evidence. Most of them are literature review studies (n = 31) on the mechanisms of action of amitriptyline and the evolution of its indication for use (or clinical application). In addition, we identified studies such as randomized clinical trials (n = 18) and systematic reviews (n = 13), which, after literature reviews, appeared a lot in this top 100. We have noticed that this drug is no longer used exclusively to treat depression; it is also used off-label. Figure 8 shows that before 1978, this selection included only studies of amitriptyline for depressive disorders. After this period, until 2018, we noticed that studies emerged directing the use of amitriptyline for other diseases, such as neuropathic pain and fibromyalgia, for example. In addition, we also note that amitriptyline is no longer a first-choice drug to treat depression, with selective serotonin reuptake inhibitors having this role [109].
Citation counting is recognized as an effective method for measuring the scientific impact of articles, researchers, and journals, and is also used as a promoter of academic research and clinical practice. It is important, however, to rationally select the database to collect the number of citations, as each database adopts its own criteria for counting citations, generally related to journal indexing [110]. Previous studies report that the Web of Science rescues studies from the beginning of the 20th century through the Web of Science’s Science Citation Index Expanded [111]. According to Bakkalbasi et al. [112] and Falagas et al. [113], the WoS is one of the best tools available for citation analysis, due to the possibility of retrieving publications since 1945 and covering quality journals that publish articles from around the world. In this work, we performed the search including all WoS databases to obtain the 100 most-cited articles that dealt with amitriptyline. The success of the search is evidenced by a large number of articles with a high number of citations that we found.
Among the bibliometric findings, we identified that the authors with the highest number of published articles were also, for the most part, those with articles with the highest number of citations. The most cited article (2671 citations), by Steru et al. [8], in 1985, received 3.17 times more citations than the second most cited (842 citations), by Cipriani, published in 2018. Despite this, the second presented 2.4 times more citations each year of publication than the first, showing that publication time is not a determining factor for a greater citation. In addition, some authors with more than one article in this top 100 received a total number of citations lower than others who have only one article on the list. The author Cipriani A. has two articles [9,54] on the list, which together were cited 1207 times, 1464 fewer citations than the article by Steru L. [8]. Such observations confirm the relevance of the number of citations as an indicator of the impact of articles on scientific development.
Among the ten most cited articles, only four [9,11,16] are published in open-access journals, not being the case of the most cited article. In addition, the most cited articles are widely cited because they are freely available in several databases.
The high impact of Steru L. [8] can be explained by the fact that it presents a simple, practical, and relatively low-cost behavioral model, with a good degree of prediction for compounds with antidepressant potential, using a methodology of suspension by the tail of rats as a basis for the evaluation of drug candidates ever since.
We believe it is important to use the corresponding author’s country of origin as a criterion to delineate the geographical distribution of articles. Even recognizing that science is increasingly a global enterprise, integrating researchers from different regions of the planet in collaborative work, we consider that generally, the corresponding author assumes a leadership role in the working group, allowing the visualization of the regions and countries that led the engagement on this topic. We also verified that the United States gained a prominent place within the studies, concentrating 55% of the 100 selected studies, followed by the United Kingdom as the highlight of the European continent. This understanding is important for us to know where these studies are originating from and what contributions they are making to supply the scientific community with relevant information.
From the research, we found that amitriptyline, since its origin, has been registered in regulatory bodies, specifically for the treatment of depressive disorders, and is still found in reference bodies such as the US-FDA [3,114]. Naturally, the first published studies aimed to understand its mechanisms of action, pharmacokinetic characteristics, safety, and efficacy in the treatment of depression. However, it is also important to emphasize that amitriptyline is no longer a first-choice drug for depression, as it has lost this space to selective serotonin reuptake inhibitors [109].
It is already well established that amitriptyline is easily dissolved in an aqueous medium, with excellent gastrointestinal absorption and an intense first-pass effect in the liver, as well as its action in the central nervous system. However, ongoing investigations have also revealed its ability to act directly on receptors, such as adrenergic (alpha-1), histaminergic, and muscarinic (M1 and M3), which have been associated with side effects of its use, such as xerostomia and sedation, which shows its great importance and variety of actions in different places, which also facilitates the understanding of the therapeutic repositioning by this drug [3,6].
However, between the 1970s and 1980s, articles began to appear exploring the benefits of amitriptyline for the management of painful conditions, as seen in Figure 8, especially those associated with neuropathies, such as diabetic neuropathy, [25,82,89,90] and PHN [30], but not exclusively. We also looked at studies on the treatment of chronic tension headaches [50,97], migraines [21,26,32,88], and complex conditions such as fibromyalgia [16,24,58,78,86], among others. Non-painful conditions were also studied, such as fibrositis [102], gastrointestinal disorders [35,44,57], post-traumatic stress [104], and non-motor symptoms of Parkinson’s disease [17]. This transformation in the paradigms studied follows its use in clinical practice and seeks to subsidize the long list of uses currently classified as “off-label”, as they do not correspond to registration in official agencies [3]. We also observed that these studies were published in specific journals in the area, such as Pain, Psychopharmacology, and Psychiatry.
Considering the relative ineffectiveness of selective serotonin reuptake inhibitors in relieving neuropathic pain and the significant effect of antidepressants that inhibit noradrenaline reuptake, it is theorized that this latter is more relevant for analgesic activity, and may subsidize, at least in part, the action of amitriptyline [114]. In fact, intrathecal administration of α1-adrenergic agonists in rats induces analgesia, which may be related to the consequent increase in GABA release in the spinal cord. On the other hand, it is suggested that the NA elevation in the medulla dorsal horn can inhibit the synaptic transmission of the peripheral afferent fibers through the activation of pre-synaptic α2 receptors, Gi/0 protein-coupled receptors, which inhibit the cAMP synthesis and activate K+ hyperpolarizing currents. This mechanism seems to have a poor effect on triggering noxious stimuli but effectively controls hyperalgesia and allodynia linked to neuropathic pain. Increased NA levels also appear to normalize the descending inhibitory function of the Locus Coeruleos, which is impaired in persistent painful conditions associated with nerve damage, improving endogenous analgesia [99,114]. Other mechanisms that potentially contribute to the analgesic activity of amitriptyline are the inhibition of the neural reuptake of adenosine, increasing adenosine activity in the peripheral and central nervous systems [115]; blockade of Na+ channels, inhibiting ectopic discharges present in injured nerves; activation of opioid receptors, inhibition of nitric oxide synthesis, increased production of BDNF, among others [116].
Although the use as an antidepressant (15.928 citations) brings together the largest number of articles in our sample, if we group the articles that studied its use for other diseases (14.581 citations), that number is not surpassed. Currently, amitriptyline is still widely used for the treatment of depressive disorders, but it is generally left as a second or third choice in clinical protocols, due to its pattern of adverse reactions and greater chances of non-adherence. On the other hand, its use as an analgesic gained significant prominence, becoming a first-line drug for the treatment of neuropathic painful conditions and fibromyalgia [15,24,58,117].
This study may have limitations, as it does not guarantee a methodological evaluation of the selected articles, nor does it guarantee the certainty of the evidence. It presents an overview of the use of amitriptyline, provides more widespread information in the scientific community, and is not an instrument for clinical decision-making. For other proposals for the application of amitriptyline, the scenario can be challenging, given the scarcity or lack of studies that support the prescription for other diseases or conditions. We also wish to make clear some limitations on the use of research databases. We used Wos, SCOPUS, and Google Scholar to retrieve the citation number of some articles. However, only the Wos—Core Collection was used as a data source for information such as authors’ names, paper keywords, and corresponding author’s country of origin. WoS, SCOPUS, and Google Scholar have broad data coverage, with differences in coverage in certain languages (mainly) and some research areas. We selected the Web of Science Core Collection as a data source because it has a high index of indexed English documents in the area of Life Science and Biomedicine. Another point worth mentioning is that the database we use, has some limitations, such as not providing complete data on some open-access articles, and this database also belongs to a commercial provider that ends up demanding an access fee for access obtaining the studies in full [118]. Thus, more comprehensive studies are needed to support the use of amitriptyline. In this sense, our mapping should serve as a guide for future research on amitriptyline.
4. Materials and Methods
4.1. Data and Search Strategy
We employed the bibliometric method, which consists of selecting the most cited articles because the articles with the highest number of citations have had a great impact on the scientific community [112]. We searched the Web of Science Core Collection in March 2023, without restrictions of time and language, using the following search key topics described in the table below (Table 4). The Web of Science Core Collection includes Science Citation Index Expanded (SCIEXPANDED), Social Sciences Citation Index (SSCI), Arts & Humanities Citation Index (A&HCI), Conference Proceedings Citation Index-Science (CPCI-S), Conference Proceedings Citation Index-Social Science & Humanities (CPCI-SSH), Book Citation Index Science (BKCI-S), Book Citation Index Social Sciences & Humanities (BKCI-SSH), Emerging Sources Citation Index (ESCI), Current Chemical Reactions (CCR-EXPANDED), and Index Chemicus (IC) [118].

Table 4.
Web of Science (WoS) search strategy.
We selected the 100 most cited articles by organizing the results in descending order based on the number of citations. Two researchers (C.S.C. and J.N.C) carried out the selection independently; discrepancies in the selection of articles were resolved using the concordance method, steps already pre-established in the work by Nascimento et al. (2022) [119].
4.2. Eligibility Criteria
We included original research articles and review articles in which the pharmacological properties of amitriptyline had been investigated. We excluded all editorials and articles from conferences and studies that did not correspond to the specific theme. Studies, where amitriptyline was not the focus of investigation, were also excluded.
4.3. Extraction of Bibliometric Parameters
In an Excel file, available as a document extraction method in WoS itself, we collect the title, authors, year of publication, number of citations, citation density (number of citations per year), keywords, country, and continent of the author corresponding. We also performed searches in the Scopus and Google Scholar databases to compare the number of citations for selected articles. Google Scholar includes citations from books, free online journals, and non-academic sources in its database, in addition to offering a broader view of its content around the world, which generates more hits and consequently more citations. WoS and Scopus retrieve more citations from articles in peer-reviewed journals [112]. However, as these databases are commercial and subscription-based products, their use in the world results in a high price, which means that an institution is forced to choose one or the other [120].
We ranked articles according to the number of citations in the Web of Science Core Collection. In the event of a tie in the number of citations, we based the position of the citation density. We represented the country and continent results with maps created using an online tool (https://mapchart.net/ (accessed on 15 May 2023)).
4.4. Data Analysis
We analyzed the collected data and generated bibliometric networks regarding co-authorship and co-occurrences of all keywords by using the Visualization of Similarities Viewer software (VOSviewer 1.6.16) [121,122]. For the co-authorship map, we introduced the names of authors with at least one article into the software as a unit of analysis. We linked them together based on the number of articles of joint authorship. These results are shown in the network and density visualization. For the co-occurrence map, we introduced author keywords with at least one occurrence into the software as the unit of analysis. These results are shown in the network view.
After analyzing the metrics, we completely read the articles to extract important information. This endeavor allowed us to map knowledge about the therapeutic use of amitriptyline. We generated a graph showing the therapeutic use of amitriptyline over time.
4.5. Content Analysis
After selection, the articles were read in full, and information was extracted regarding their content, study design, when they were published, which country the corresponding authors belong to, and the application of the use of amitriptyline over the years in the selected documents. Studies were classified by type based on work by Higgins et al. [107]. This classification is based on the Cochrane Collaboration Glossary: in vivo, in vitro, literature review, systematic review, meta-analysis, observational, and randomized clinical trials studies.
5. Conclusions
Our review is the first to report bibliometric characteristics and knowledge mapping for the use of amitriptyline. We also reported, through the analysis of the articles in this top 100, that there was a therapeutic repositioning of amitriptyline. From the early 1960s to the early 1980s, this drug was mostly used to treat depressive disorders, but since the early 1980s, it has been used to treat other conditions such as headache, fibromyalgia, neuropathic pain, gastrointestinal disorders, and other types of painful diseases.
Author Contributions
Conceptualization, C.d.S.P., J.N.C. and R.R.L.; methodology, C.d.S.P., M.K.M.F., J.N.C. and D.C.B.-d.-S.; software and formal analysis C.d.S.P., M.K.M.F. and D.C.B.-d.-S.; research, data curation, and writing—original draft preparation, C.d.S.P., M.K.M.F., J.N.C. and D.C.B.-d.-S.; writing—proofreading and editing, C.d.S.P., M.K.M.F., J.N.C., E.A.F.-J. and D.C.B.-d.-S.; supervision, R.R.L. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by Coordination for the Improvement of Higher Education Personnel (CAPES, Brazil), Finance Code 001. R.R.L. is a researcher from Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) and received grants under numbers 312275/2021-8 and 408329/2022-0. The APC was funded by Pró-Reitoria de Pesquisa e Pós-graduação from Federal University of Pará (PROPESP-UFPA).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data is contained within the article.
Conflicts of Interest
The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results. The authors declare no conflict of interest.
References
- Thour, A.; Marwaha, R. Amitriptyline; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- World Health Organization. WHO Model List of Essential Medicines. Available online: http://www.who.int/medicines/organization/par/edl/expcom13/eml13_en.pdf (accessed on 19 July 2023).
- McClure, E.W.; Daniels, R.N. Classics in Chemical Neuroscience: Amitriptyline. ACS Chem. Neurosci. 2021, 12, 354–362. [Google Scholar] [CrossRef]
- Pereira, V.S.; Hiroaki-Sato, V.A. A Brief History of Antidepressant Drug Development: From Tricyclics to beyond Ketamine. Acta Neuropsychiatr. 2018, 30, 307–322. [Google Scholar] [CrossRef]
- Leucht, C.; Huhn, M.; Leucht, S. Amitriptyline versus Placebo for Major Depressive Disorder. In Cochrane Database of Systematic Reviews; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2011. [Google Scholar]
- Reinert, J.P.; Veronin, M.A.; Medina, C. Tricyclic Antidepressants in Nociceptive and Neuropathic Pain: A Review of Their Analgesic Properties in Combination With Opioids. J. Pharm. Technol. 2023, 39, 35–40. [Google Scholar] [CrossRef]
- Huang, Y.; Chen, H.; Chen, S.R.; Pan, H.L. Duloxetine and Amitriptyline Reduce Neuropathic Pain by Inhibiting Primary Sensory Input to Spinal Dorsal Horn Neurons via A1- and A2-Adrenergic Receptors. ACS Chem. Neurosci. 2023, 14, 1261–1277. [Google Scholar] [CrossRef]
- Steru, L.; Chermat, R.; Thierry, B.; Simon, P. The Tail Suspension Test: A New Method for Screening Antidepressants in Mice. Psychopharmacology 1985, 85, 367–370. [Google Scholar] [CrossRef]
- Cipriani, A.; Furukawa, T.A.; Salanti, G.; Chaimani, A.; Atkinson, L.Z.; Ogawa, Y.; Leucht, S.; Ruhe, H.G.; Turner, E.H.; Higgins, J.P.T.; et al. Comparative Efficacy and Acceptability of 21 Antidepressant Drugs for the Acute Treatment of Adults With Major Depressive Disorder: A Systematic Review and Network Meta-Analysis. Focus (Madison) 2018, 16, 420–429. [Google Scholar] [CrossRef]
- Max, M.B.; Lynch, S.A.; Muir, J.; Shoaf, S.E.; Smoller, B.; Dubner, R. Effects of Desipramine, Amitriptyline, and Fluoxetine on Pain in Diabetic Neuropathy. N. Engl. J. Med. 1992, 326, 1250–1256. [Google Scholar] [CrossRef]
- Hershman, D.L.; Lacchetti, C.; Dworkin, R.H.; Lavoie Smith, E.M.; Bleeker, J.; Cavaletti, G.; Chauhan, C.; Gavin, P.; Lavino, A.; Lustberg, M.B.; et al. Prevention and Management of Chemotherapy-Induced Peripheral Neuropathy in Survivors of Adult Cancers: American Society of Clinical Oncology Clinical Practice Guideline. J. Clin. Oncol. 2014, 32, 1941–1967. [Google Scholar] [CrossRef]
- Furukawa, T.A.; Barbui, C.; Cipriani, A.; Brambilla, P.; Watanabe, N. Imputing Missing Standard Deviations in Meta-Analyses Can Provide Accurate Results. J. Clin. Epidemiol. 2006, 59, 7–10. [Google Scholar] [CrossRef] [PubMed]
- Carlsson, A.; Corrodi, H.; Fuxe, K.; Hökfelt, T. Effect of Antidepressant Drugs on the Depletion of Intraneuronal Brain 5-Hydroxytryptamine Stores Caused by 4-Methyl-α-Ethyl-Meta-Tyramine. Eur. J. Pharmacol. 1969, 5, 357–366. [Google Scholar] [CrossRef]
- Shen, Y.; Monsma, F.J.; Metcalf, M.A.; Jose, P.A.; Hamblin, M.W.; Sibley, D.R. Molecular Cloning and Expression of a 5-Hydroxytryptamine7 Serotonin Receptor Subtype. J. Biol. Chem. 1993, 268, 18200–18204. [Google Scholar] [CrossRef] [PubMed]
- McQuay, H.J.; Tramèr, M.; Nye, B.A.; Carroll, D.; Wiffen, P.J.; Moore, R.A. A Systematic Review of Antidepressants in Neuropathic Pain. Pain 1996, 68, 217–227. [Google Scholar] [CrossRef]
- Macfarlane, G.J.; Kronisch, C.; Dean, L.E.; Atzeni, F.; Häuser, W.; Flub, E.; Choy, E.; Kosek, E.; Amris, K.; Branco, J.; et al. EULAR Revised Recommendations for the Management of Fibromyalgia. Ann. Rheum. Dis. 2017, 76, 318–328. [Google Scholar] [CrossRef]
- Seppi, K.; Weintraub, D.; Coelho, M.; Perez-Lloret, S.; Fox, S.H.; Katzenschlager, R.; Hametner, E.M.; Poewe, W.; Rascol, O.; Goetz, C.G.; et al. The Movement Disorder Society Evidence-Based Medicine Review Update: Treatments for the Non-Motor Symptoms of Parkinson’s Disease. Mov. Disord. 2011, 26, S42–S80. [Google Scholar] [CrossRef]
- Lanquillon, S.; Krieg, J.C.; Bening-Abu-Shach, U.; Vedder, H. Cytokine Production and Treatment Response in Major Depressive Disorder. Neuropsychopharmacology 2000, 22, 370–379. [Google Scholar] [CrossRef] [PubMed]
- Anderson, I.M. Selective Serotonin Reuptake Inhibitors versus Tricyclic Antidepressants: A Meta-Analysis of Efficacy and Tolerability. J. Affect. Disord. 2000, 58, 19–36. [Google Scholar] [CrossRef]
- Kelly, J.P.; Wrynn, A.S.; Leonard, B.E. The Olfactory Bulbectomized Rat as a Model of Depression: An Update. Pharmacol. Ther. 1997, 74, 299–316. [Google Scholar] [CrossRef]
- Silberstein, S.D.; Holland, S.; Freitag, F.; Dodick, D.W.; Argoff, C.; Ashman, E. Evidence-Based Guideline Update: Pharmacologic Treatment for Episodic Migraine Prevention in Adults Report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology 2012, 78, 1337–1345. [Google Scholar] [CrossRef] [PubMed]
- Kirchheiner, J.; Nickchen, K.; Bauer, M.; Wong, M.L.; Licinio, J.; Roots, I.; Brockmöller, J. Pharmacogenetics of Antidepressants and Antipsychotics: The Contribution of Allelic Variations to the Phenotype of Drug Response. Mol. Psychiatry 2004, 9, 442–473. [Google Scholar] [CrossRef]
- Radley, D.C.; Finkelstein, S.N.; Stafford, R.S. Off-Label Prescribing among Office-Based Physicians. Arch. Intern. Med. 2006, 166, 1021–1026. [Google Scholar] [CrossRef]
- Carville, S.F.; Arendt-Nielsen, S.; Bliddal, H.; Blotman, F.; Branco, J.C.; Buskila, D.; Da Silva, J.A.P.; Danneskiold-Samsøe, B.; Dincer, F.; Henriksson, C.; et al. EULAR Evidence-Based Recommendations for the Management of Fibromyalgia Syndrome. Ann. Rheum. Dis. 2008, 67, 536–541. [Google Scholar] [CrossRef]
- Max, M.B.; Culnane, M.; Schafer, S.C.; Gracely, R.H.; Walther, D.J.; Smoller, B.; Dubner, R. Amitriptyline Relieves Diabetic Neuropathy Pain in Patients with Normalor Depressed Mood. Neurology 1987, 37, 589–596. [Google Scholar] [CrossRef] [PubMed]
- Evers, S.; Áfra, J.; Frese, A.; Goadsby, P.J.; Linde, M.; May, A.; Sándor, P.S. EFNS Guideline on the Drug Treatment of Migraine—Revised Report of an EFNS Task Force. Eur. J. Neurol. 2009, 16, 968–981. [Google Scholar] [CrossRef]
- Heikkila, R.E.; Orlansky, H.; Cohen, G. Studies on the Distinction between Uptake Inhibition and Release of [3H]Dopamine in Rat Brain Tissue Slices. Biochem. Pharmacol. 1975, 24, 847–852. [Google Scholar] [CrossRef] [PubMed]
- Hu, Z.; Yang, X.; Ho, P.C.L.; Sui, Y.C.; Heng, P.W.S.; Chan, E.; Duan, W.; Hwee, L.K.; Zhou, S. Herb-Drug Interactions: A Literature Review. Drugs 2005, 65, 1239–1282. [Google Scholar] [CrossRef]
- Rice, A.S.C.; Maton, S. Gabapentin in Postherpetic Neuralgia: A Randomised, Double Blind, Placebo Controlled Study. Pain 2001, 94, 215–224. [Google Scholar] [CrossRef]
- Kost, R.G.; Straus, S.E. Postherpetic Neuralgia—Pathogenesis, Treatment, and Prevention. N. Engl. J. Med. 1996, 335, 32–42. [Google Scholar] [CrossRef]
- Wolf, S.; Barton, D.; Kottschade, L.; Grothey, A.; Loprinzi, C. Chemotherapy-Induced Peripheral Neuropathy: Prevention and Treatment Strategies. Eur. J. Cancer 2008, 44, 1507–1515. [Google Scholar] [CrossRef]
- Ayata, C.; Jin, H.; Kudo, C.; Dalkara, T.; Moskowitz, M.A. Suppression of Cortical Spreading Depression in Migraine Prophylaxis. Ann. Neurol. 2006, 59, 652–661. [Google Scholar] [CrossRef]
- Katon, W.; Von Korff, M.; Lin, E.; Bush, T.; Ormel, J. Adequacy and Duration of Antidepressant Treatment in Primary Care. Med. Care 1992, 30, 67–76. [Google Scholar] [CrossRef] [PubMed]
- Teichgräber, V.; Ulrich, M.; Endlich, N.; Riethmüller, J.; Wilker, B.; De Oliveira-Munding, C.C.; Van Heeckeren, A.M.; Barr, M.L.; Von Kürthy, G.; Schmid, K.W.; et al. Ceramide Accumulation Mediates Inflammation, Cell Death and Infection Susceptibility in Cystic Fibrosis. Nat. Med. 2008, 14, 382–391. [Google Scholar] [CrossRef] [PubMed]
- Rasquin-Weber, A.; Hyman, P.E.; Cucchiara, S.; Fleisher, D.R.; Hyams, J.S.; Milla, P.J.; Staiano, A. Childhood Functional Gastrointestinal Disorders. Gut 1999, 45, ii60–ii68. [Google Scholar] [CrossRef]
- Snyder, S.H.; Yamamura, H.I. Antidepressants and the Muscarinic Acetylcholine Receptor. Arch. Gen. Psychiatry 1977, 34, 236–239. [Google Scholar] [CrossRef]
- Jick, H.; Kaye, J.A.; Jick, S.S. Antidepressants and the Risk of Suicidal Behaviors. JAMA 2004, 292, 338–343. [Google Scholar] [CrossRef]
- Benfield, P.; Heel, R.C.; Lewis, S.P. Fluoxetine: A Review of Its Pharmacodynamic and Pharmacokinetic Properties, and Therapeutic Efficacy in Depressive Illness. Drugs 1986, 32, 481–508. [Google Scholar] [CrossRef] [PubMed]
- Gillman, P.K. Tricyclic Antidepressant Pharmacology and Therapeutic Drug Interactions Updated. Br. J. Pharmacol. 2007, 151, 737–748. [Google Scholar] [CrossRef]
- Horn, A.S.; Coyle, J.T.; Snyder, S.H. Catecholamine Uptake by Synaptosomes from Rat Brain. Structure-Activity Relationships of Drugs with Differential Effects on Dopamine and Norepinephrine Neurons. Mol. Pharmacol. 1971, 7, 66–80. [Google Scholar]
- Onghena, P.; Van Houdenhove, B. Antidepressant-Induced Analgesia in Chronic Non-Malignant Pain: A Meta-Analysis of 39 Placebo-Controlled Studies. Pain 1992, 49, 205–219. [Google Scholar] [CrossRef]
- Watson, C.P.; Evans, R.J.; Reed, K.; Merskey, H.; Goldsmith, L.; Warsh, J. Amitriptyline versus Placebo in Postherpetic Neuralgia. Neurology 1982, 32, 671–673. [Google Scholar] [CrossRef]
- Maas, J.W. Biogenic Amines and Depression: Biochemical and Pharmacological Separation of Two Types of Depression. Arch. Gen. Psychiatry 1975, 32, 1357–1361. [Google Scholar] [CrossRef] [PubMed]
- Ford, A.C.; Talley, N.J.; Schoenfeld, P.S.; Quigley, E.M.M.; Moayyedi, P. Efficacy of Antidepressants and Psychological Therapies in Irritable Bowel Syndrome: Systematic Review and Meta-Analysis. Gut 2009, 58, 367–378. [Google Scholar] [CrossRef]
- Mills, D.C.B.; Robb, I.A.; Roberts, G.C.K. The Release of Nucleotides, 5-hydroxytryptamine and Enzymes from Human Blood Platelets during Aggregation. J. Physiol. 1968, 195, 715–729. [Google Scholar] [CrossRef]
- Mynors-Wallis, L.M.; Gath, D.H.; Lloyd-Thomas, A.R.; Tomlinson, D. Randomised Controlled Trial Comparing Problem Solving Treatment with Amitriptyline and Placebo for Major Depression in Primary Care. BMJ 1995, 310, 441. [Google Scholar] [CrossRef]
- Klerman, G.L.; Dimascio, A.; Weissman, M.; Prusoff, B.; Paykel, E.S. Treatment of Depression by Drugs and Psychotherapy. Am. J. Psychiatry 1974, 131, 186–191. [Google Scholar] [CrossRef]
- Saarto, T.; Wiffen, P.J. Antidepressants for Neuropathic Pain: A Cochrane Review. J. Neurol. Neurosurg. Psychiatry 2010, 81, 1372–1373. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, C.; Hyttel, J. Comparison of the Effects of Antidepressants and Their Metabolites on Reuptake of Biogenic Amines and on Receptor Binding. Cell. Mol. Neurobiol. 1999, 19, 467–489. [Google Scholar] [CrossRef]
- Bendtsen, L. Central Sensitization in Tension-Type Headache—Possible Pathophysiological Mechanisms. Cephalalgia 2000, 20, 486–508. [Google Scholar] [CrossRef] [PubMed]
- Richelson, E.; Souder, T. Binding of Antipsychotic Drugs to Human Brain Receptors Focus on Newer Generation Compounds. Life Sci. 2000, 68, 29–39. [Google Scholar] [CrossRef]
- Kaptchuk, T.J.; Stason, W.B.; Davis, R.B.; Legedza, A.T.R.; Schnyer, R.N.; Kerr, C.E.; Stone, D.A.; Nam, B.H.; Kirsch, I.; Goldman, R.H. Sham Device versus Inert Pill: Randomised Controlled Trial of Two Placebo Treatments. Br. Med. J. 2006, 332, 391–394. [Google Scholar] [CrossRef]
- Paykel, E.S.; Scott, J.; Teasdale, J.D.; Johnson, A.L.; Garland, A.; Moore, R.; Jenaway, A.; Cornwall, P.L.; Hayhurst, H.; Abbott, R.; et al. Prevention of Relapse in Residual Depression by Cognitive Therapy. A Controlled Trial. Arch. Gen. Psychiatry 1999, 56, 829–835. [Google Scholar] [CrossRef] [PubMed]
- Cipriani, A.; Zhou, X.; Del Giovane, C.; Hetrick, S.E.; Qin, B.; Whittington, C.; Coghill, D.; Zhang, Y.; Hazell, P.; Leucht, S.; et al. Comparative Efficacy and Tolerability of Antidepressants for Major Depressive Disorder in Children and Adolescents: A Network Meta-Analysis. Lancet 2016, 388, 881–890. [Google Scholar] [CrossRef]
- Serretti, A.; Mandelli, L. Antidepressants and Body Weight: A Comprehensive Review and Meta-Analysis. J. Clin. Psychiatry 2010, 71, 1259–1272. [Google Scholar] [CrossRef]
- Anttila, S.A.K.; Leinonen, E.V.J. A Review of the Pharmacological and Clinical Profile of Mirtazapine. CNS Drug Rev. 2001, 7, 249–264. [Google Scholar] [CrossRef]
- Jackson, J.L.; O’Malley, P.G.; Tomkins, G.; Balden, E.; Santoro, J.; Kroenke, K. Treatment of Functional Gastrointestinal Disorders with Antidepressant Medications: A Meta-Analysis. Am. J. Med. 2000, 108, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Goldenberg, D.L.; Felson, D.T.; Dinerman, H. A Randomized, Controlled Trial of Amitriptyline and Naproxen in the Treatment of Patients with Fibromyalgia. Arthritis Rheum. 1986, 29, 1371–1377. [Google Scholar] [CrossRef]
- Braithwaite, R.A.; Goulding, R.; Theano, G.; Bailey, J.; Coppen, A. Plasma Concentration of Amitriptyline and Clinical Response. Lancet 1972, 299, 1297–1300. [Google Scholar] [CrossRef] [PubMed]
- Spiker, D.G.; Perel, J.M.; Hanin, I.; Dealy, R.S.; Griffin, S.J.; Soloff, P.H.; Cofsky Weiss, J. The Pharmacological Treatment of Delusional Depression: Part II. J. Clin. Psychopharmacol. 1986, 6, 339–342. [Google Scholar] [CrossRef]
- Ross, S.B.; Renyi, A.L. Inhibition of the Uptake of Tritiated 5-Hydroxytryptamine in Brain Tissue. Eur. J. Pharmacol. 1969, 7, 270–277. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.; Shapiro, D.A.; George, S.R.; Setola, V.; Lee, D.K.; Cheng, R.; Rauser, L.; Lee, S.P.; Lynch, K.R.; Roth, B.L.; et al. Discovery of a Novel Member of the Histamine Receptor Family. Mol. Pharmacol. 2001, 59, 427–433. [Google Scholar] [CrossRef]
- Kirchherr, H.; Kühn-Velten, W.N. Quantitative Determination of Forty-Eight Antidepressants and Antipsychotics in Human Serum by HPLC Tandem Mass Spectrometry: A Multi-Level, Single-Sample Approach. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2006, 843, 100–113. [Google Scholar] [CrossRef]
- Miyasaki, J.M.; Shannon, K.; Voon, V.; Ravina, B.; Kleiner-Fisman, G.; Anderson, K.; Shulman, L.M.; Gronseth, G.; Weiner, W.J. Practice Parameter: Evaluation and Treatment of Depression, Psychosis, and Dementia in Parkinson Disease (an Evidence-Based Review): Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2006, 66, 996–1002. [Google Scholar] [CrossRef] [PubMed]
- Reul, J.M.H.M.; Stec, I.; Soder, M.; Holsboer, F. Chronic Treatment of Rats with the Antidepressant Amitriptyline Attenuates the Activity of the Hypothalamic-Pituitary-Adrenocortical System. Endocrinology 1993, 133, 312–320. [Google Scholar] [CrossRef]
- Bulik, C.M.; Berkman, N.D.; Brownley, K.A.; Sedway, J.A.; Lohr, K.N. Anorexia Nervosa Treatment: A Systematic Review of Randomized Controlled Trials. Int. J. Eat. Disord. 2007, 40, 310–320. [Google Scholar] [CrossRef]
- Bielski, R.J.; Friedel, R.O. Prediction of Tricyclic Antidepressant Response: A Critical Review. Arch. Gen. Psychiatry 1976, 33, 1479–1489. [Google Scholar] [CrossRef] [PubMed]
- Ueng, Y.F.; Kuwabara, T.; Chun, Y.J.; Guengerich, F.P. Cooperativity in Oxidations Catalyzed by Cytochrome P450 3A4. Biochemistry 1997, 36, 370–381. [Google Scholar] [CrossRef]
- O’Connor, A.B. Neuropathic Pain: Quality-of-Life Impact, Costs and Cost Effectiveness of Therapy. Pharmacoeconomics 2009, 27, 95–112. [Google Scholar] [CrossRef]
- Heninger, G.R.; Charney, D.S.; Sternberg, D.E. Lithium Carbonate Augmentation of Antidepressant Treatment. J. Clin. Psychopharmacol. 1984, 4, 167. [Google Scholar] [CrossRef]
- Hicks, J.K.; Swen, J.J.; Thorn, C.F.; Sangkuhl, K.; Kharasch, E.D.; Ellingrod, V.L.; Skaar, T.C.; Müller, D.J.; Gaedigk, A.; Stingl, J.C. Clinical Pharmacogenetics Implementation Consortium Guideline for CYP2D6 and CYP2C19 Genotypes and Dosing of Tricyclic Antidepressants. Clin. Pharmacol. Ther. 2013, 93, 402–408. [Google Scholar] [CrossRef]
- Montigny, C.; Cournoyer, G.; Morissette, R.; Langlois, R.; Caillè, G. Lithium Carbonate Addition in Tricyclic Antidepressant—Resistant Unipolar Depression: Correlations With the Neurobiologic Actions of Tricyclic Antidepressant Drugs and Lithium Ion on the Serotonin System. Arch. Gen. Psychiatry 1983, 40, 1327–1334. [Google Scholar] [CrossRef] [PubMed]
- Sherman, A.D.; Sacquitne, J.L.; Petty, F. Specificity of the Learned Helplessness Model of Depression. Pharmacol. Biochem. Behav. 1982, 16, 449–454. [Google Scholar] [CrossRef] [PubMed]
- Ray, W.A.; Fought, R.L.; Decker, M.D. Psychoactive Drugs and the Risk of Injurious Motor Vehicle Crashes in Elderly Drivers. Am. J. Epidemiol. 1992, 136, 873–883. [Google Scholar] [CrossRef] [PubMed]
- Chew, M.L.; Mulsant, B.H.; Pollock, B.G.; Lehman, M.E.; Greenspan, A.; Mahmoud, R.A.; Kirshner, M.A.; Sorisio, D.A.; Bies, R.R.; Gharabawi, G. Anticholinergic Activity of 107 Medications Commonly Used by Older Adults. J. Am. Geriatr. Soc. 2008, 56, 1333–1341. [Google Scholar] [CrossRef] [PubMed]
- Pond, S.M.; Tozer, T.N. First-Pass Elimination Basic Concepts and Clinical Consequences. Clin. Pharmacokinet. 1984, 9, 1–25. [Google Scholar] [CrossRef]
- Thapa, P.B.; Gideon, P.; Cost, T.W.; Milam, A.B.; Ray, W.A. Antidepressants and the Risk of Falls among Nursing Home Residents. N. Engl. J. Med. 1998, 339, 875–882. [Google Scholar] [CrossRef]
- Goldenberg, D.; Mayskiy, M.; Mossey, C.; Ruthazer, R.; Schmid, C. A Randomized, Double-Blind Crossover Trial of Fluoxetine and Amitriptyline in the Treatment of Fibromyalgia. Arthritis Rheum. 1996, 39, 1852–1859. [Google Scholar] [CrossRef] [PubMed]
- Mann, J.J. The Medical Management of Depression. N. Engl. J. Med. 2005, 353, 1819–1834. [Google Scholar] [CrossRef]
- Nii, T.; Ishii, F. Encapsulation Efficiency of Water-Soluble and Insoluble Drugs in Liposomes Prepared by the Microencapsulation Vesicle Method. Int. J. Pharm. 2005, 298, 198–205. [Google Scholar] [CrossRef]
- Morris, J.B.; Beck, A.T. The Efficacy of Antidepressant Drugs: A Review of Research (1958 to 1972). Arch. Gen. Psychiatry 1974, 30, 667–674. [Google Scholar] [CrossRef]
- Max, M.B.; Schafer, S.C.; Culnane, M.; Smoller, B.; Dubner, R.; Gracely, R.H. Amitriptyline, but Not Lorazepam, Relieves Postherpetic Neuralgia. Neurology 1988, 38, 1427–1432. [Google Scholar] [CrossRef]
- Bodnoff, S.R.; Suranyi-Cadotte, B.; Aitken, D.H.; Quirion, R.; Meaney, M.J. The Effects of Chronic Antidepressant Treatment in an Animal Model of Anxiety. Psychopharmacology 1988, 95, 298–302. [Google Scholar] [CrossRef]
- Gardiner, S.J.; Begg, E.J. Pharmacogenetics, Drug-Metabolizing Enzymes, and Clinical Practice. Pharmacol. Rev. 2006, 58, 521–590. [Google Scholar] [CrossRef] [PubMed]
- Pacher, P.; Kecskemeti, V. Cardiovascular Side Effects of New Antidepressants and Antipsychotics: New Drugs, Old Concerns? Curr. Pharm. Des. 2005, 10, 2463–2475. [Google Scholar] [CrossRef]
- Arnold, L.M.; Keck, P.E.; Welge, J.A. Antidepressant Treatment of Fibromyalgia. A Meta-Analysis and Review. Psychosomatics 2000, 41, 104–113. [Google Scholar] [CrossRef] [PubMed]
- Fava, M. Weight Gain and Antidepressants. J. Clin. Psychiatry 2000, 61, 37–41. [Google Scholar]
- Lewis, D.W.; Ashwal, S.; Dahl, G.; Dorbad, D.; Hirtz, D.; Prensky, A.; Jarjour, I. Practice Parameter: Evaluation of Children and Adolescents with Recurrent Headaches: Report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology 2002, 59, 490–498. [Google Scholar] [CrossRef] [PubMed]
- Bril, V.; England, J.; Franklin, G.M.; Backonja, M.; Cohen, J.; Del Toro, D.; Feldman, E.; Iverson, D.J.; Perkins, B.; Russell, J.W.; et al. Evidence-Based Guideline: Treatment of Painful Diabetic Neuropathy: Report of the American Academy of Neurology, the American Association of Neuromuscular and Electrodiagnostic Medicine, and the American Academy of Physical Medicine and Rehabilitation. Neurology 2011, 76, 1758–1765. [Google Scholar] [CrossRef]
- Morello, C.M.; Leckband, S.G.; Stoner, C.P.; Moorhouse, D.F.; Sahagian, G.A. Randomized Double-Blind Study Comparing the Efficacy of Gabapentin with Amitriptyline on Diabetic Peripheral Neuropathy Pain. Arch. Intern. Med. 1999, 159, 1931–1937. [Google Scholar] [CrossRef]
- Duby, J.J.; Campbell, R.K.; Setter, S.M.; White, J.R.; Rasmussen, K.A. Diabetic Neuropathy: An Intensive Review. Am. J. Health-Syst. Pharm. 2004, 61, 160–176. [Google Scholar] [CrossRef]
- Venkatakrishnan, K.; Von Moltke, L.L.; Greenblatt, D.J. Human Drug Metabolism and the Cytochromes P450: Application and Relevance of in Vitro Models. J. Clin. Pharmacol. 2001, 41, 1149–1179. [Google Scholar] [CrossRef]
- Leijon, G.; Boivie, J. Central Post-Stroke Pain—A Controlled Trial of Amitriptyline and Carbamazepine. Pain 1989, 36, 27–36. [Google Scholar] [CrossRef]
- Linkowski, P.; Mendlewicz, J.; Kerkhofs, M.; Leclercq, R.; Golstein, J.; Brasseur, M.; Copinschi, G.; Cauter, E. Van 24-Hour Profiles of Adrenocorticotropin, Cortisol, and Growth Hormone in Major Depressive Illness: Effect of Antidepressant Treatment. J. Clin. Endocrinol. Metab. 1987, 65, 141–152. [Google Scholar] [CrossRef] [PubMed]
- Frahnert, C.; Rao, M.L.; Grasmäder, K. Analysis of Eighteen Antidepressants, Four Atypical Antipsychotics and Active Metabolites in Serum by Liquid Chromatography: A Simple Tool for Therapeutic Drug Monitoring. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2003, 794, 35–47. [Google Scholar] [CrossRef] [PubMed]
- Reimherr, F.W.; Chouinard, G.; Cohn, C.K.; Cole, J.O.; Itil, T.M.; LaPierre, Y.D.; Masco, H.L.; Mendels, J. Antidepressant Efficacy of Sertraline: A Double-Blind, Placebo- and Amitriptyline-Controlled, Multicenter Comparison Study in Outpatients with Major Depression. J. Clin. Psychiatry 1990, 51, 18–27. [Google Scholar] [PubMed]
- Holroyd, K.A.; O’Donnell, F.J.; Stensland, M.; Lipchik, G.L.; Cordingley, G.E.; Carlson, B.W. Management of Chronic Tension-Type Headache with Tricyclic Antidepressant Medication, Stress Management Therapy, and Their Combination: A Randomized Controlled Trial. JAMA 2001, 285, 2208–2215. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.R.; Nelson, D.R.; Johnson, A.M. Biochemical Effects of the Antidepressant Paroxetine, a Specific 5-Hydroxytryptamine Uptake Inhibitor. Psychopharmacology 1987, 93, 193–200. [Google Scholar] [CrossRef]
- Field, M.J.; McCleary, S.; Hughes, J.; Singh, L. Gabapentin and Pregabalin, but Not Morphine and Amitriptyline, Block Both Static and Dynamic Components of Mechanical Allodynia Induced by Streptozocin in the Rat. Pain 1999, 80, 391–398. [Google Scholar] [CrossRef]
- Beckmann, H.; Goodwin, F.K. Antidepressant Response to Tricyclics and Urinary MHPG in Unipolar Patients: Clinical Response to Imipramine or Amitriptyline. Arch. Gen. Psychiatry 1975, 32, 17–21. [Google Scholar] [CrossRef] [PubMed]
- Green, J.P.; Maayani, S. Tricyclic Antidepressant Drugs Block Histamine H2 Receptor in Brain. Nature 1977, 269, 163–165. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Keller, J.L.; Jaeschke, R.; Rosenbloom, D.; Adachi, J.D.; Newhouse, M.T. The N-of-1 Randomized Controlled Trial: Clinical Usefulness. Our Three-Year Experience. Ann. Intern. Med. 1990, 112, 293–299. [Google Scholar] [CrossRef]
- Paykel, E.S.; Hollyman, J.A.; Freeling, P.; Sedgwick, P. Predictors of Therapeutic Benefit from Amitriptyline in Mild Depression: A General Practice Placebo-Controlled Trial. J. Affect. Disord. 1988, 14, 83–95. [Google Scholar] [CrossRef]
- Davidson, J.; Kudler, H.; Smith, R.; Mahorney, S.L.; Lipper, S.; Hammett, E.; Saunders, W.B.; Cavenar, J.O. Treatment of Posttraumatic Stress Disorder with Amitriptyline and Placebo. Arch. Gen. Psychiatry 1990, 47, 259–266. [Google Scholar] [CrossRef]
- Pancrazio, J.J.; Kamatchi, G.L.; Roscoe, A.K.; Lynch, C. Inhibition of Neuronal Na+ Channels by Antidepressant Drugs. J. Pharmacol. Exp. Ther. 1998, 284, 208–214. [Google Scholar]
- Lidbrink, P.; Jonsson, G.; Fuxe, K. The Effect of Imipramine-like Drugs and Antihistamine Drugs on Uptake Mechanisms in the Central Noradrenaline and 5-Hydroxytryptamine Neurons. Neuropharmacology 1971, 10, 521–530. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions; Wiley: Hoboken, NJ, USA, 2019; ISBN 9781119536604. [Google Scholar]
- Carlsson, A.; Corrodi, H.; Fuxe, K.; Hökfelt, T. Effects of Some Antidepressant Drugs on the Depletion of Intraneuronal Brain Catecholamine Stores Caused by 4,α-Dimethyl-Meta-Tyramine. Eur. J. Pharmacol. 1969, 5, 367–373. [Google Scholar] [CrossRef] [PubMed]
- Strothers, H.S. Depression in the Primary Care Setting. Ethn. Dis. 2002, 12, 559–568. [Google Scholar] [CrossRef]
- De Granda-Orive, J.I.; Alonso-Arroyo, A.; Roig-Vázquez, F. Which Data Base Should We Use for Our Literature Analysis? Web of Science versus SCOPUS. Arch. Bronconeumol. 2011, 47, 213. [Google Scholar] [CrossRef]
- Liu, W. The Changing Role of Non-English Papers in Scholarly Communication: Evidence from Web of Science’s Three Journal Citation Indexes. Learn. Publ. 2017, 30, 115–123. [Google Scholar] [CrossRef]
- Bakkalbasi, N.; Bauer, K.; Glover, J.; Wang, L. Three Options for Citation Tracking: Google Scholar, Scopus and Web of Science. Biomed. Digit. Libr. 2006, 3, 7. [Google Scholar] [CrossRef]
- Falagas, M.E.; Pitsouni, E.I.; Malietzis, G.A.; Pappas, G. Comparison of PubMed, Scopus, Web of Science, and Google Scholar: Strengths and Weaknesses. FASEB J. 2008, 22, 338–342. [Google Scholar] [CrossRef]
- López-Muñoz, F.; Srinivasan, V.; de Berardis, D.; Álamo, C.; Kato, T.A. Melatonin, Neuroprotective Agents and Antidepressant Therapy; Springer: Delhi, India, 2016. [Google Scholar]
- Ulugol, A.; Karadag, H.C.; Tamer, M.; Firat, Z.; Aslantas, A.; Dokmeci, I. Involvement of Adenosine in the Anti-Allodynic Effect of Amitriptyline in Streptozotocin-Induced Diabetic Rats. Neurosci. Lett. 2002, 328, 129–132. [Google Scholar] [CrossRef]
- Lawson, K. A Brief Review of the Pharmacology of Amitriptyline and Clinical Outcomes in Treating Fibromyalgia. Biomedicines 2017, 5, 24. [Google Scholar] [CrossRef] [PubMed]
- Obata, H. Analgesic Mechanisms of Antidepressants for Neuropathic Pain. Int. J. Mol. Sci. 2017, 18, 2483. [Google Scholar] [CrossRef] [PubMed]
- Jacso, P. The Scientometric Portrait of Eugene Garfield through the Free ResearcherID Service from the Web of Science Core Collection of 67 Million Master Records and 1.3 Billion References. Scientometrics 2018, 114, 545–555. [Google Scholar] [CrossRef]
- Nascimento, P.C.; Ferreira, M.K.M.; Bittencourt, L.O.; Martins-Júnior, P.A.; Lima, R.R. Global Research Trends on Maternal Exposure to Methylmercury and Offspring Health Outcomes. Front. Pharmacol. 2022, 13, 973118. [Google Scholar] [CrossRef]
- Pranckutė, R. Web of Science (Wos) and Scopus: The Titans of Bibliographic Information in Today’s Academic World. Publications 2021, 9, 12. [Google Scholar] [CrossRef]
- Waltman, L.; van Eck, N.J.; Noyons, E.C.M. A Unified Approach to Mapping and Clustering of Bibliometric Networks. J. Informetr. 2010, 4, 629–635. [Google Scholar] [CrossRef]
- van Eck, N.J.; Waltman, L. Software Survey: VOSviewer, a Computer Program for Bibliometric Mapping. Scientometrics 2010, 84, 523–538. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).