Chemical Constituents and Their Biological Activities from Genus Styrax
Abstract
1. Introduction
2. Results and Discussion
2.1. Chemical Constituents
2.1.1. Lignans
2.1.2. Terpenoids
2.1.3. Aromatic Compounds
2.1.4. Steroids
2.1.5. Others
2.2. Chemical Constituents Biological Activities
2.2.1. Cytotoxic Activity
2.2.2. Antibacterial and Antifungal Activity
2.2.3. Antiproliferative and Differentiation Effects
2.2.4. Anti-Complement Activity
2.2.5. Anti-Complement Activity
2.2.6. Induction of Apoptosis
2.2.7. Induction of Apoptosis
2.2.8. Acetylcholinesterase Inhibitors and Structure–Activity Relationships
2.2.9. Inhibitory Effect on Interleukin
2.2.10. Matrix Metalloproteinase’s Activity
2.2.11. Antiasthmatic, Antiulcer, and Anti-Inflammatory Activities
2.2.12. Other Activity
3. Materials and Methods
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| MCF-7 | Metastatic breast adenocarcinoma cell line |
| MDA-MB-231 | Human breast cancer cell line |
| Hep-2 | Human larynx carcinoma cell line |
| HeLa | Human cervix carcinoma cell lines |
| C6 | Rat glioma cell lines |
| HL-60 | Human leukemia cell line |
| A549 | Human lung cancer cell line |
| PC-3 | Human prostatic cancer cell line |
| Lu | Lung cancer cell lines |
| CCK-8 | Cell Counting Kit-8 |
| ATCC 6305 | Streptococcus pneumoniae |
| ATCC 19615 | Streptococcus pyogenes |
| ATCC 10211 | Hemophilus influenzae |
| ATCC 27853 | Pseudomonas aeruginosa |
| ATCC 10031 | Klebsiella pneumoniae |
| MIC | Minimum inhibitory concentration |
| DPPH | DPPH radical |
| HepG2 | Hepatocellular carcinoma cell line |
| KGN | Human ovarian granulosa cells |
| AChE | Acetylcholinesterase |
| EeAChE | Electrophorus electricus AChE |
| hAChE | Human AChE |
| BChE | Butyrylcholinesterase |
| CTX | Cyclophosphamide |
| IFN-γ | Interferon-γ |
| hCES1A | Human carboxylesterase 1A1 |
| MMP-1 | Matrix metalloproteinase-1 |
| PTP1B | The protein tyrosine phosphatase 1B |
| iNOS | Nitric oxide synthase |
| TNF-α | Tumor necrosis factor-α |
| IL-1β | Interleukin-1β |
| COX-1 | Cyclooxygenase-1 |
| COX-2 | Cyclooxygenase-2 |
| NF-κb | Nuclear factor-κB |
Appendix A
| Genus Styrax | Traditional Use |
|---|---|
| S. perkinsiae | Estrogen synthesis promotion |
| S. obassia | Anticancer activities |
| S. japonica | Cough, bronchitis, sore throat, inflammation, paralysis, laryngitis, and expectoration treatment |
| S. pohlii | / |
| S. camporum | Antimicrobial, anticancer, antifungal, hypolipidemic, and immunossupressive activities |
| S. macranthus | / |
| S. officinalis | Antiseptic and anti-respiratory disease |
| S. argentifolius | / |
| S. ferrugineus | / |
| S. agrestis | / |
| S. tonkinensis | Expectorant, antiseptic, and analgesic activities |
| S. suberifolius | Rheumatic disease cure |
| S. ramirezii | / |
Appendix B
| No. | Compound Class and Name | Source | Ref. |
|---|---|---|---|
| Lignans | |||
| 1 | 5-(2-Propen-1-one)-7-me-thoxy-2-(3,4-methylenedioxyphenyl) benzofuran | S. perkinsiae | [18] |
| 2 | 1″-Hydryoxyegonol gentiobioside | S. perkinsiae | [18] |
| S. obassia | [2] | ||
| S. ferrugineus | [19] | ||
| 3 | Obassioside B | S. perkinsiae | [18] |
| S. obassia | [2] | ||
| S. obassia S. obassia | [2,60] | ||
| 4 | Egonol | S. perkinsiae | [18] |
| S. japonica | [21,25] | ||
| S. obassia | [28,31] | ||
| S. agrestis | [10] | ||
| S. ferrugineus | [19] | ||
| S. pohlii | [69] | ||
| S. camporum | [11] | ||
| S. macranthus | [32] | ||
| S. officinalis L. | [35] | ||
| S. argentifolius | [43] | ||
| 5 | Egonol glucoside | S. perkinsiae | [18] |
| S. japonica | [20] | ||
| S. suberifolius | [40] | ||
| S. macranthus | [32] | ||
| S. obassia | [28] | ||
| [60] | |||
| 6 | Egonol gentiobioside | S. perkinsiae | [17,18] |
| S. macranthus | [32] | ||
| S. obassia | [2] | ||
| S. pohlii | [69] | ||
| 7 | Egonol gentiotrioside | S. perkinsiae | [17,18] |
| S. macranthus | [32] | ||
| 8 | MasutakesideI (sutakeside I) | S. perkinsiae | [18] |
| S. japonica | [22] | ||
| S. obassia | [27] | ||
| 9 | trans-5-(3-Hydroxypropyl)-7-methoxy-2-[3-methoxy-4-hydroxyphenyl)-benzofuran-5-yl]benzufuran | S. perkinsiae | [17] |
| 10 | (E)-5-(2-Formylvinyl)-7-metho-xy-2-(3,4-methylenedioxyphenyl)benzofuran | S. perkinsiae | [17] |
| 11 | 5-(3-Butanoyloxypropyl)-7-methoxy-2-(3,4-methylene dioxyphenyl)benzofuran | S. perkinsiae | [17] |
| 12 | 5-(3-Hydroxypropyl)-7-hydroxy-2-(3,4-methylene-dioxyphenyl) benzofuran | S. perkinsiae | [17] |
| S. macranthus | [32] | ||
| 12 | 5-(3-Hydroxypropyl)-7-hydroxy-2-(3,4-methylene-dioxyphenyl) benzofuran | S. perkinsiae | [17] |
| S. macranthus | [32] | ||
| 13 | Egonol acetate | S. perkinsiae | [17] |
| S. japonica | [25] | ||
| S. obassia | [28,29,31] | ||
| S. agrestis | [10] | ||
| S. officinalis L. | [37] | ||
| 14 | Demethoxy egonol acetate | S. perkinsiae | [17] |
| S. japonica | [25] | ||
| 15 | Styraxlignolide B | S. perkinsiae | [18] |
| S. japonica | [7] | ||
| 16 | Styraxjaponoside C | S. perkinsiae | [18] |
| S. japonica | [7] | ||
| 17 | Nor-lignans5-(3″-hydroxypropyl)-7-methoxy-2-(3′,4′-methylenedioxyphenyl) benzofuran | S. ferrugineus | [19] |
| S. camporum | [11] | ||
| S. pohlii | [69] | ||
| 18 | 5-[3″-(β-D-Glucopyranosyloxy)propyl]-7-methoxy-2-(3′,4′-methylenedioxyphenyl) benzofuran | S. ferrugineus | [19] |
| S. pohlii | [69] | ||
| 19 | Dihydrodehydrodiconiferyl alcohol | S. ferrugineus | [19] |
| 20 | Styraxjaponoside C | S. japonica | [21] |
| 21 | Arctiin | S. japonica | [21] |
| 22 | Matairesinoside | S. japonica | [20,21] |
| 23 | Pinoresinol-4-O-β-D-glucopyranoside | S. japonica | [21] |
| 24 | 2R-(4′-hydroxy-3′-methoxyphenyl)-6R-(3″,4″-methylenedioxyphenyl)-8-oxo-3,7-dioxabicyclo [3.3.0]octane 4′-hydroxyl | S. japonica | [7] |
| 25 | Styraxjaponoside A | S. japonica | [20] |
| 26 | Styraxjaponoside B | S. japonica | [20] |
| 27 | Dihydrodehydrodiconiferyl alcohol 9-O-glucoside | S. japonica | [20] |
| 28 | Styraxlignolide A | S. japonica | [22] |
| 29 | Styraxlignolide B | S. japonica | [7] |
| 30 | Styraxlignolide C | S. japonica | [7] |
| 31 | Styraxlignolide D | S. japonica | [7] |
| 32 | Styrax lignolides F | S. japonica | [7,24] |
| 33 | (–)-Pinoresinol glucoside | S. japonica | [7] |
| 34 | Styrlignan A | S. japonica | [23] |
| 35 | 1R,2R,5S,6R-2-(4′-Hydroxy-3′-methoxyphenyl)-6-(3″,4″-dimethoxyphenyl)-3,7-dioxabicyclo-[3.3.0]octane4′-O-β-D-glucopyranoside | S. japonica | [24] |
| 36 | Obassioside A | S. japonica | [26] |
| 37 | Methyl 3-[7-methoxy-2-(3′,4′-methylene-dioxyphenyl)-5-benzofuranyl]-propionate | S. obassia | [31] |
| 38 | Methyl3-[2-(3′,4′-methylen-edioxyphenyl)-5-benzofuranyl]-propionate | S. obassia | [31] |
| 39 | 5-(3″-Propanoyloxypropyl)-7-methoxy-2-(3′,4′-methylenedioxyphenyl)-benzofuran | S. obassia | [28] |
| S. agrestis | [10] | ||
| 40 | Egonol-2-methylbutanoate | S. obassia | [31] |
| 41 | 7-Demethoxylegonol-2-methylbutanoate | S. obassia | [5] |
| 42 | Egonol propanoate | S. obassia | [29] |
| S. agrestis | [10] | ||
| 43 | 3-[7-Methoxy-2-(3,4-methylenedioxyphenyl)benzofuran-5-yl]propyl-3-[7-methoxy-2-(3,4-methylenedioxyphenyl)-benzofuran-5-yl]propanoate | S. macranthus | [32] |
| 44 | Demethoxy egonol gentiobioside | S. macranthus | [32] |
| 45 | 7-Methoxy-2-(3,4-methylenedioxyphenyl) benzofuran-5-carbaldehyde | S. macranthus | [32] |
| 46 | Demethoxy egonol | S. macranthus | [32] |
| S. obassia | [28] | ||
| S. japonica | [23] | ||
| 47 | 5-3″-(2-Methylbutanoyloxy)propyl]-7-methoxy-2-(3′,4′-dimethoxyphenyl) benzofuran | S. officinalis L. | [23] |
| 48 | 5-(3″Benzoyloxypropyl)-7-methoxy-2-(3′,4′-methylenedioxyphenyl)-benzofuran | S. officinalis L. | [36] |
| 49 | 4-[3″-(1c-methylbutanoyloxy)propyl]-2-methoxy-(3′,4′-methylenedioxyphenyl)-1a,5b-dihydrobenzo-[3,4]-cyclobutaoxirene | S. officinalis L. | [65] |
| 50 | Egonol-9(Z),12(Z) linoleate | S. agrestis | [10] |
| 51 | 7-Demethoxyegonol-9(Z),12(Z) linoleate | S. agrestis | [10] |
| 52 | 7-Demethoxyegonol oleate | S. agrestis | [10] |
| 53 | Egonol oleate | S. agrestis | [10] |
| 54 | 7-Demethoxylegonol acetate | S. agrestis | [10] |
| 55 | Egonol-2-methylpropanoat | S. agrestis | [10] |
| 56 | (±)Syringaresinol | S. camporum | [38] |
| 57 | Homoegonol gentiobioside | S. pohlii | [39] |
| 58 | Lariciresinol 4-O-β-D-glucoside | S. perkinsiae | [39] |
| 59 | (−)-Secoisolariciresinol 4-O-β-D-Glucopyranoside | S. perkinsiae | [39] |
| 60 | Lariciresinol4′-O-β-D-glucoside | S. perkinsiae | [39] |
| 61 | Lanicepside A | S. perkinsiae | [39] |
| 62 | Solariciresinol4-O-β-D-glucopyranoside | S. perkinsiae | [39] |
| 63 | (+)-Lariciresinol9-O-β-D-glucopyranoside | S. perkinsiae | [39] |
| 64 | 2R,3S-Dihydrodehydrodiconiferyl alcohol 4′-O-β-D-glucopyranoside | S. perkinsiae | [39] |
| 65 | Pinoresinol | S. perkinsiae | [39] |
| 66 | Homoegonol glucoside | S. suberifolius | [40] |
| 67 | 2-(4-Hydroxy3-methoxyphenyl)-5-(3-hydroxypropyl)-7-methoxybenzofuran | S. suberifolius | [40] |
| 68 | 2-(3-Hydroxy-4-methoxyphenyl)-7-methoxy-5benzofuranpropanol | S. suberifolius | [40] |
| 69 | (+)-Cedrusin | S. suberifolius | [40] |
| 70 | (−)-(7R,8S)-Dihydrodehydrodiconiferyl alcohol | S. suberifolius | [40] |
| 71 | (−)-(7R,8S)-Dihydrodehydrodiconiferyl alcohol 4-O-β-Dglucopyranoside | S. suberifolius | [40] |
| 72 | (−)-(7S,8R)-Dihydrodehydrodiconiferylalcohol 4-O-β-D-glucopyranoside | S. suberifolius | [40] |
| 73 | (+)-(7S,8R)-Dihydrodehydrodiconiferyl alcohol | S. suberifolius | [40] |
| 74 | (+)-(7S,8R)-Erythro-4,7,9,9′-tetrahydroxy-3,3′-dimethoxy-8-O-4′-neolignan | S. suberifolius | [40] |
| 75 | (−)-Symplocosneolignan A | S. suberifolius | [40] |
| 76 | (−)-7-O-Ethylguaiacylglycerol (15) | S. suberifolius | [40] |
| 77 | 2[4-(3-Hydroxypropyl)-2-methoxyphenoxy]-1,3-propanediol | S. suberifolius | [40] |
| 78 | Dihydroconiferyl alcohol | S. suberifolius | [40] |
| 79 | 3,3-Bis(3,4-dihydro-6-methoxy-2H-1-benzopyran | S. tonkinensis | [41] |
| 80 | Rac-(8α,8′β)-4,4′-dihydroxy3,3′-dimethoxylignan-9,9′-diyldiacetate | S. tonkinensis | [41] |
| 81 | (–)-Secoisolariciresino | S. tonkinensis | [41] |
| 82 | 4,4′-Dihydroxy-3,3′dimethoxy-9-ethoxy-9,9′-epoxylignan | S. tonkinensis | [41] |
| 83 | (2S,3R,4R)-4-[1-Ethoxy-1-(4-hydroxy-3-methoxy)phenyl]methyl-2(4-hydroxy-3-methoxy)phenyl-3-hydroxymethyl-tetrahydrofuran | S. tonkinensis | [41] |
| 84 | (–)-Neo-olivil-(9-O-9″)-seco-isolariciresinol | S. tonkinensis | [41] |
| 85 | Isolariciresinol | S. tonkinensis | [41] |
| 86 | Stytonkinol A | S. tonkinensis | [42] |
| 87 | Stytonkinol B | S. tonkinensis | [42] |
| 88 | Styraxin | S. argentifolius | [43] |
| 89 | Vladinol D | S. argentifolius | [43] |
| 90 | 5-Carboxy7-methoxy-2-(3′,4′-methylenedioxyphenyl)benzofuran | S. argentifolius | [43] |
| 91 | 5-((E)-2-Carboxyvinyl)-7-methoxy-2-(3′,4′-methylenedioxyphenyl)benzofuran | S. argentifolius | [43] |
| 92 | (–)-Machicendiol | S. argentifolius | [43] |
| 93 | Machicendona | S. argentifolius | [43] |
| Terpenoids | |||
| 94 | Taraxerol | S. japonica | [7,45] |
| 95 | Oleanolic aldehyde acetate | S. japonica | [22,54] |
| 96 | Erythrodiol-3-acetate | S. japonica | [22,54] |
| 97 | Euphorginol | S. japonica | [22,54] |
| 98 | 3β-Acetoxyolean-12-en-28-acid | S. japonica | [45] |
| 99 | 3β-Acetoxy-17β-hydroxy-28-norolean-12-ene | S. japonica | [45] |
| 100 | Anhydrosophoradiol-3-acetate | S. japonica | [22,54] |
| 101 | Styraxosides B | S. japonica | [44] |
| 102 | Camellenodiol | S. japonica | [44] |
| 103 | Jegosaponins A | S. japonica | [46] |
| 104 | Jegosaponins B | S. japonica | [46] |
| 105 | Jegosaponins C | S. japonica | [46] |
| 106 | Jegosaponins D | S. japonica | [46] |
| 107 | 3β-Acetoxy-28-hydroxyolean-12-ene | S. japonica | [47] |
| 108 | 3β-Acetoxyolean-12-en-28-acid | S. japonica | [47] |
| 109 | 3β-Acetoxyolean-12-en-28-aldehyde | S. japonica | [47] |
| 110 | 3β-Acetoxy-17β-hydroxy-28-norolean-12-ene | S. japonica | [47] |
| 111 | 6β-Hydroxy-3-oxo-11α,12α-epoxyolean- 28,13β-olide | S. tonkinensis | [4] |
| 112 | 3β,6β-Dihydroxy-11α,12α-epoxyolean-28,13β-olide | S. tonkinensis | [4] |
| 113 | 3β,6β-Dihydroxy-11-oxo-olean-12-en-28-oic acid | S. tonkinensis | [4] |
| 114 | 3β-Hydroxy-12-oxo-13HR-olean-28,19β-olide | S. tonkinensis | [4] |
| 115 | 19β-Hydroxy-3-oxo-olean-12-en-28-oic acid | S. tonkinensis | [4] |
| 116 | 6β-Hydroxy-3-oxo-olean-12-en-28-oic acid | S. tonkinensis | [4] |
| 117 | Sumaresinolic acid | S. tonkinensis | [4,51] |
| 118 | Siaresinolic acid | S. tonkinensis | [4,51] |
| 119 | Oleanolic acid | S. tonkinensis | [4,51] |
| 120 | 21-Benzoylbarringtogenol C | S. officinalis L. | [4] |
| 121 | Styrax-saponin A | S. officinalis L. | [49] |
| 122 | Styrax-saponin B | S. officinalis L. | [49] |
| 123 | Styrax-saponin C | S. officinalis L. | [49] |
| 124 | Deacylsaponin | S. officinalis L. | [49] |
| 125 | Oleanonic acid | S. tonkinensis | [42,51] |
| 126 | Betulonic acid | S. tonkinensis | [42,51] |
| 127 | Corosolic acid | S. tonkinensis | [42,51] |
| 128 | Maslinic acid | S. tonkinensis | [42,51] |
| 129 | Epibetulinic acid | S. tonkinensis | [42] |
| 130 | Betulinic acid | S. tonkinensis | [42,51] |
| 131 | 2α,3α,24-trihydroxy-urs-12-en-28-oic acid | S. argentifolius | [43] |
| Aromatic Compounds | |||
| 132 | trans-(Tetrahydro-2-(4-hydroxy-3-methoxyphenyl)-5-oxofuran-3-yl)methylbenzoate | S. tonkinensis | [52] |
| 133 | 3-(4-Hydroxy-3-methoxyphenyl)-2-oxopropylbenzoate | S. tonkinensis | [52] |
| 134 | 4-(E)-3-Ethoxyprop-1-enyl)-2-methoxyphenol | S. tonkinensis | [52] |
| 135 | Benzoic acid | S. tonkinensis | [52] |
| 136 | Vanillin | S. tonkinensis | [52] |
| 137 | Dehydrodivanillin | S. tonkinensis | [52] |
| 138 | Vanillic acid | S. tonkinensis | [52] |
| 139 | Coniferyl aldehyde | S. tonkinensis | [52] |
| 140 | Methylsyringin | S. japonica | [21] |
| 141 | Syringin | S. japonica | [7,21] |
| 142 | Isotachioside | S. perkinsiae | [39] |
| 143 | (2R,3R)-3,7,4′-Trihydroxy-5,3′-dimethoxyflavan 7-O-β-D-glucopyranoside | S. suberifolius | [40] |
| 144 | Methyl orsellinate | S. suberifolius | [40] |
| 145 | Ethyl orsellinate | S. suberifolius | [40] |
| 146 | Methyl β-orcinolcarboxylate | S. suberifolius | [40] |
| Steroids | |||
| 147 | Stigmasterol | S.macranthus | [32] |
| 148 | Styraxosides A | S. japonica | [32] |
| 149 | Daucosterol | S.macranthus | [32] |
| 150 | β-Sitosterol | S. perkinsiae | [17] |
| 151 | (20R)-24Ethylcholest-5,22-dien-7-one | S. argentifolius | [43] |
| Others | |||
| 152 | Kaempferol-3-O-(2″,4″-di-O-(E)-p-coumaroyl-β-D-glucopyranoside) | S. pohlii | [56] |
| S. camporum | [56] | ||
| 153 | Kaempferol-3-O-(2″,6″-di-O-(E)-p-coumaroyl)-β-D-glucopyranoside | S. pohlii | [56] |
| S. camporum | [56] | ||
| 154 | Quercetin | S. pohlii | [56] |
| S. camporum | [57] | ||
| 155 | Kaempferol | S. pohlii | [56] |
| S. camporum | [57] | ||
| 156 157 | Koninginin T Koninginin U | S. pohlii | [57] |
| S. pohlii | [57] | ||
| 158 | Jegosaponins A | S. japonica | [58] |
| 159 | Jegosaponins B | S. japonica | [58] |
Appendix C
| No. | Structure | Phytochemistry | Pharmacological Activity |
|---|---|---|---|
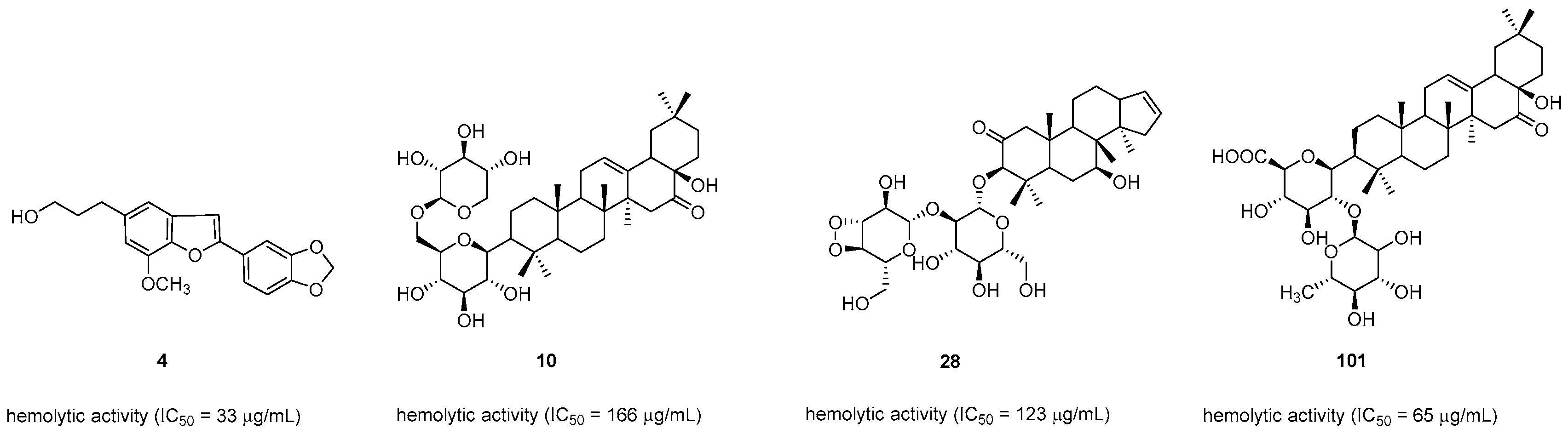
| 3 |  | S. perkinsiae S. obassia | MCF-7 (IC50 = 53.5 μg/mL) Hela (IC50 = 23.3 μg/mL) HL-60 (IC50 = 16.8 μg/mL) |
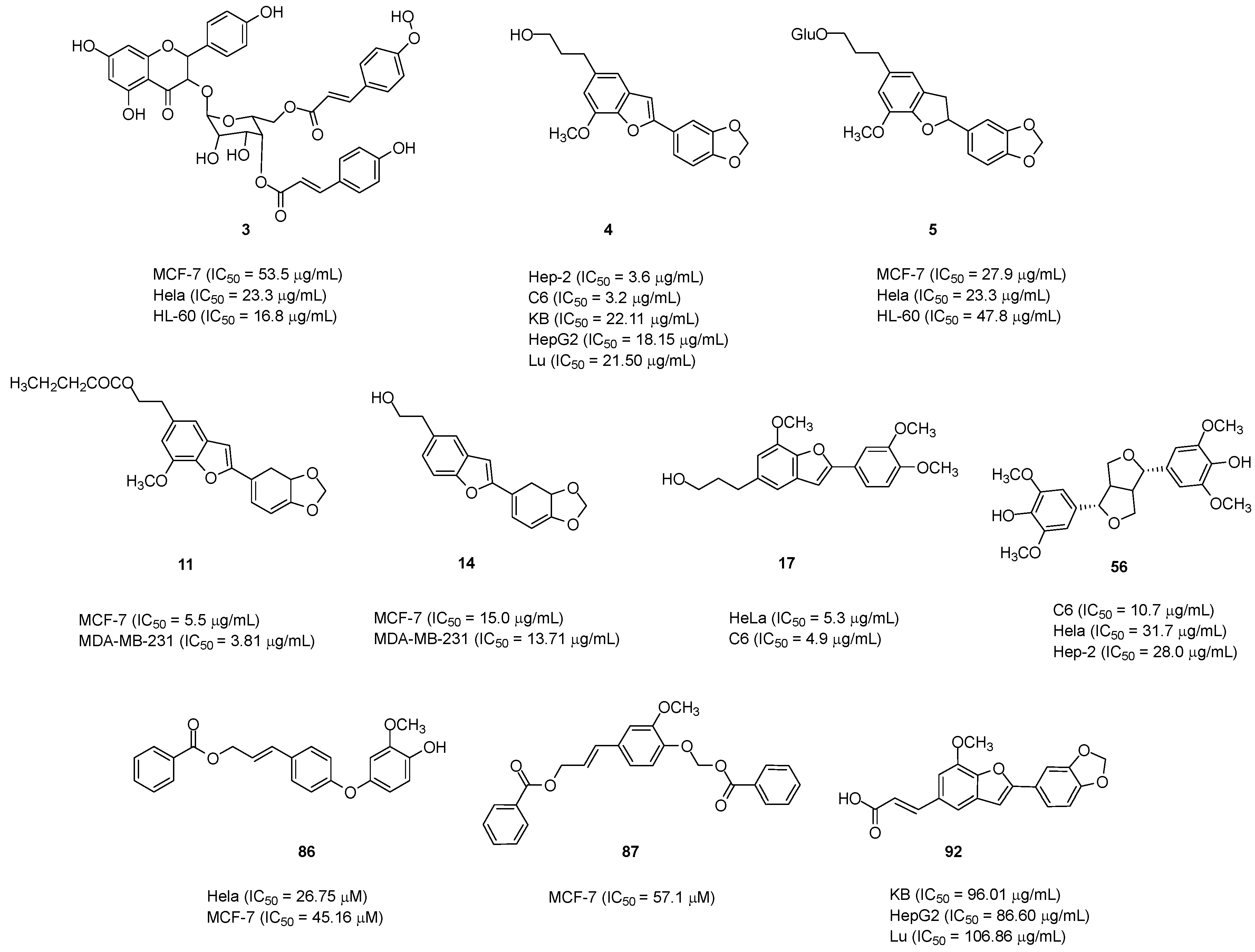
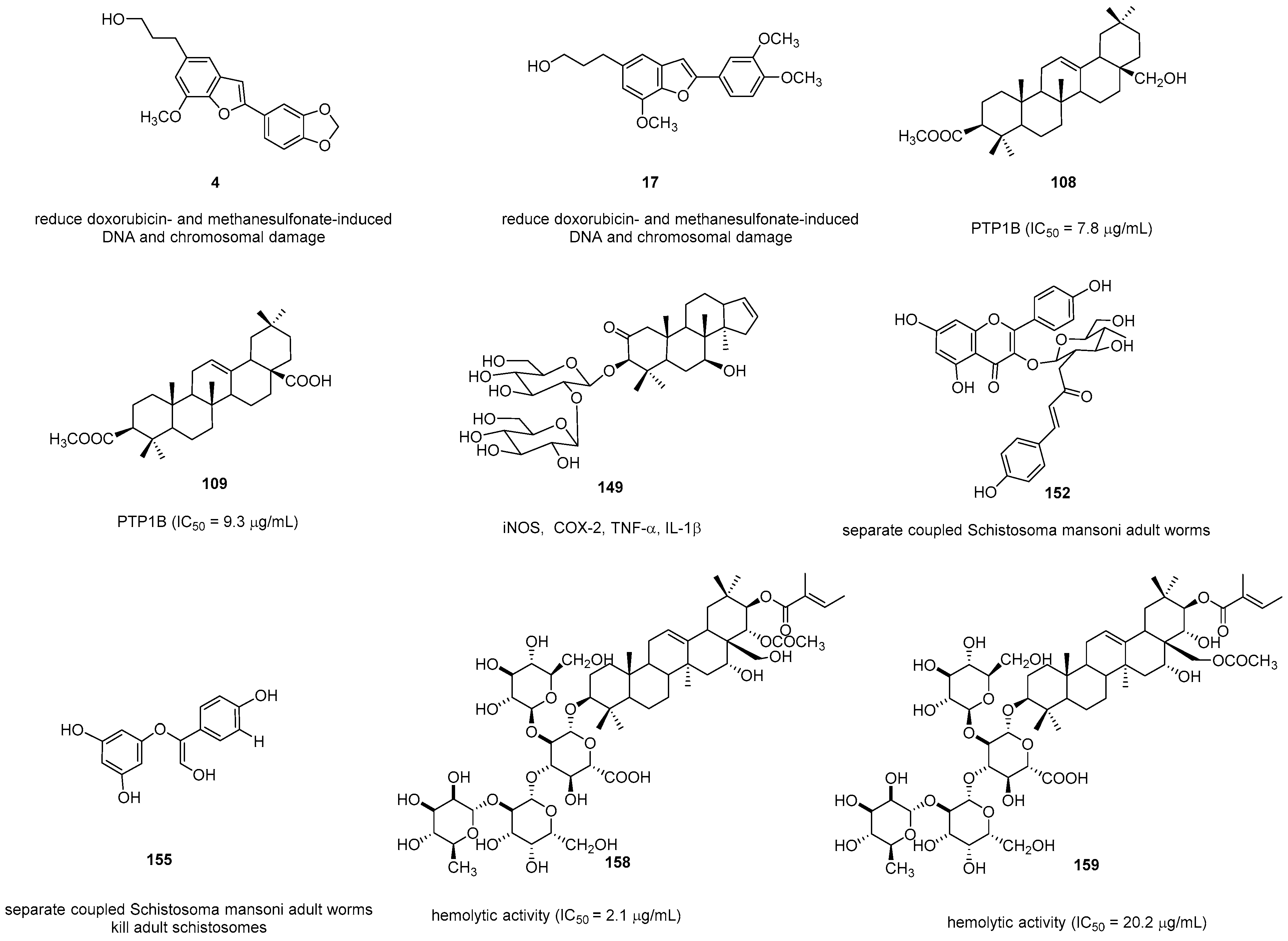
| 4 |  | S. perkinsiae S. japonica S. obassia S. agrestis S. ferrugineus S. pohlii S. camporum S. macranthus S. officinalis S. argentifolius | Hep-2 (IC50 = 3.6 μg/mL) C6 (IC50 = 3.2 μg/mL) KB (IC50 = 22.11 μg/mL) HepG2 (IC50 = 18.15 μg/mL) Lu (IC50 = 21.50 μg/mL) Hemolytic activity (IC50 = 33 μg/mL) C. sphaerospermum (MIC = 5 mg/mL) C. albicans (MIC = 10 μg/mL) S. aureus (MIC = 10 μg/mL) ATCC 27853 and ATCC 6305 (MIC = 400 mg/mL) COX-1 (inhibition rate = 35.7% at 30 μM) Reduce doxorubicin- and methanesulfonate-induced DNA and chromosomal damage |
| 5 | 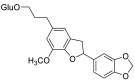 | S. perkinsiae S. japonica S. suberifolius S. macranthus S. obassia | MCF-7 (IC50 = 27.9 μg/mL) Hela (IC50 = 23.3 μg/mL) S. aureus (MIC = 20 μg/mL) C. albicans (MIC = 15 μg/mL) HL-60 (IC50 = 47.8 μg/mL) |
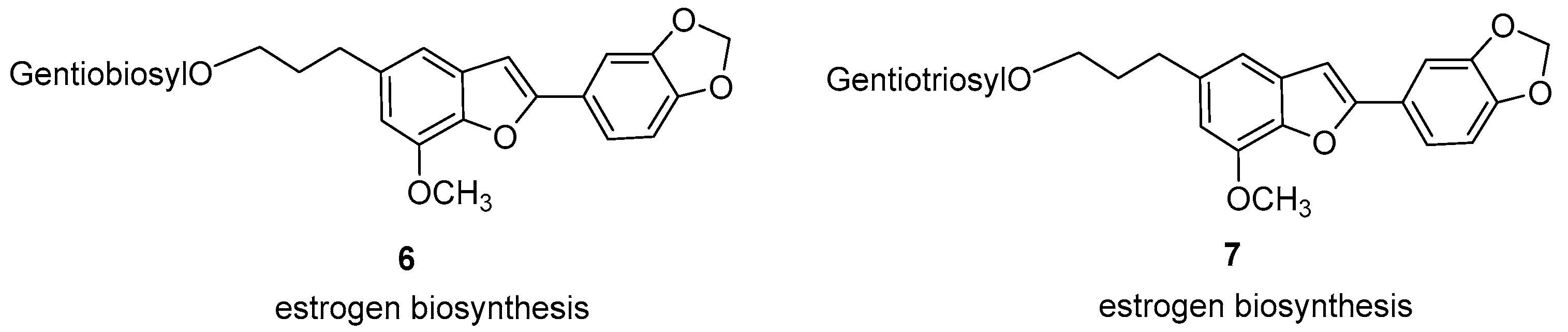
| 6 | 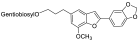 | S. perkinsiae S. macranthus S. obassia S. pohlii | Estrogen biosynthesis |
| 7 | 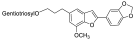 | S. perkinsiae S. macranthus | Estrogen biosynthesis |
| 10 | 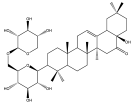 | S. perkinsiae | Hemolytic activity (IC50 = 166 μg/mL) |
| 11 |  | S. perkinsiae | MCF-7 (IC50 = 5.5 μg/mL) MDA-MB-231 (IC50 = 3.81 μg/mL) |
| 14 | 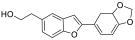 | S. perkinsiae S. japonica | MCF-7 (IC50 = 15.0 μg/mL) MDA-MB-231 (IC50 = 13.71 μg/mL) |
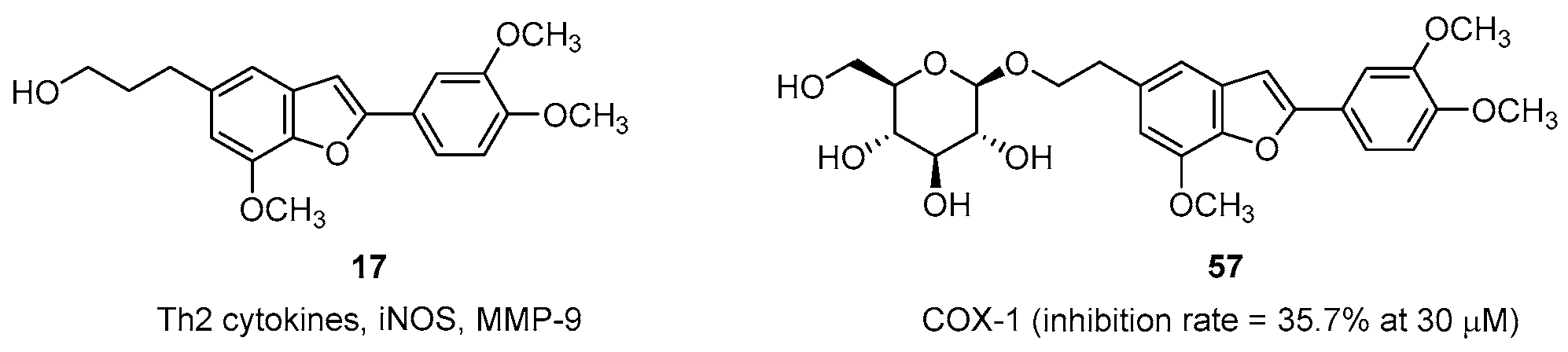
| 17 | 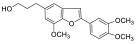 | S. ferrugineus S. camporum S. pohlii | HeLa (IC50 = 5.3 μg/mL) C6 (IC50 = 4.9 μg/mL) C. sphaerospermum (MIC = 10 μg/mL) C. albicans (MIC = 12 μg/mL) S. aureus (MIC = 10 μg/mL) Th2 cytokines, iNOS, MMP-9 Reduce doxorubicin- and methanesulfonate-induced DNA and chromosomal damage |
| 18 | 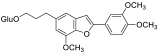 | S. ferrugineus S. pohlii | S. aureus (MIC = 20 μg/mL) C. albicans (MIC = 20 μg/mL) |
| 19 | 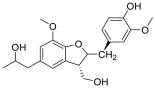 | S. ferrugineus | S. aureus (MIC = 20 μg/mL) C. albicans (MIC = 15 μg/mL) |
| 26 | 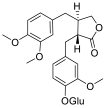 | S. japonica | MMP-1 (inhibition rate = 62.1% at 10 μM) |
| 28 | 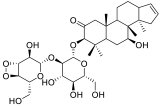 | S. japonica | Hemolytic activity (IC50 = 123 μg/mL) |
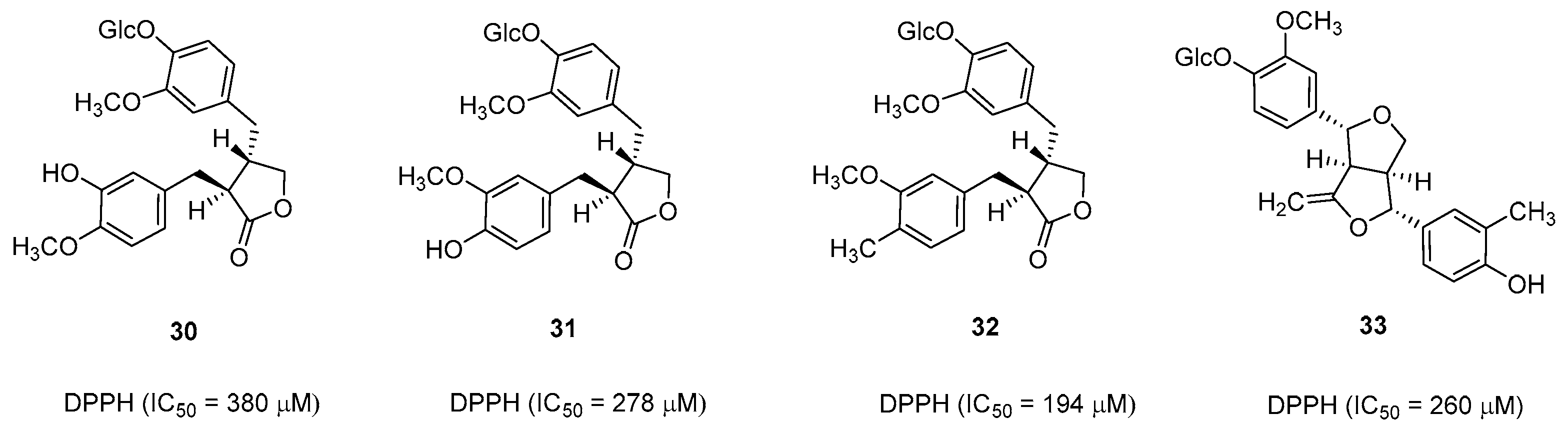
| 30 | 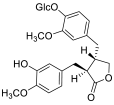 | S. japonica | DPPH (IC50 = 380 μM) |
| 31 |  | S. japonica | DPPH (IC50 = 278 μM) |
| 32 | 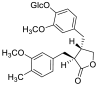 | S. japonica | DPPH (IC50 = 194 μM) |
| 33 | 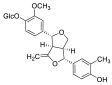 | S. japonica | DPPH (IC50 = 260 μM) |
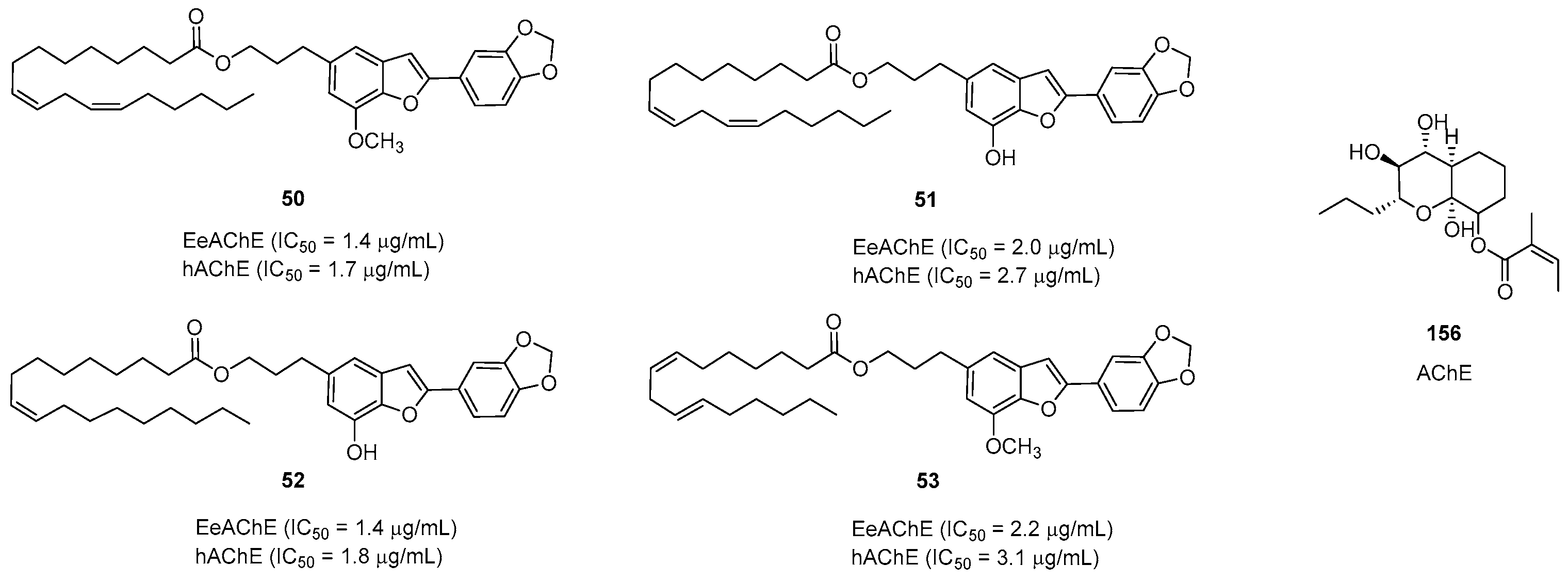
| 50 | 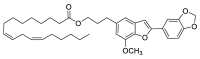 | S. agrestis | EeAChE (IC50 = 1.4 μg/mL) hAChE (IC50 = 1.7 μg/mL) |
| 51 |  | S. agrestis | EeAChE (IC50 = 2.0 μg/mL) hAChE (IC50 = 2.7 μg/mL) |
| 52 | 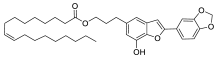 | S. agrestis | EeAChE (IC50 = 1.4 μg/mL) hAChE (IC50 = 1.8 μg/mL) |
| 53 |  | S. agrestis | EeAChE (IC50 = 2.2 μg/mL) hAChE (IC50 = 3.1 μg/mL) |
| 86 | 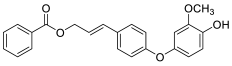 | S. tonkinensis | Hela (IC50 = 26.75 μM) MCF-7 (IC50 = 45.16 μM) |
| 87 |  | S. tonkinensis | MCF-7 (IC50 = 57.1 μM) Hemolytic activity (IC50 = 65 μg/mL) |
| 92 |  | S. argentifolius | KB (IC50 = 96.01 μg/mL) HepG2 (IC50 = 86.60 μg/mL) Lu (IC50 = 106.86 μg/mL) |
| 95 | 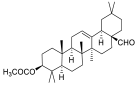 | S. japonica | Human dermal fibroblasts (IC50 = 20 μM) |
| 96 |  | S. japonica | MMP-1 (inhibition rate = 73.1% at 0.01 μM) |
| 100 | 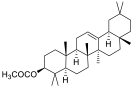 | S. japonica | Human dermal fibroblasts (IC50 = 1.12 μM) |
| 101 | 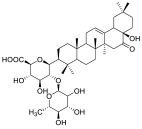 | S. tonkinensis | Hemolytic activity (IC50 = 65 μg/mL) |
| 108 |  | S. japonica | PTP1B (IC50 = 7.8 μg/mL) |
| 109 |  | S. japonica | PTP1B (IC50 = 9.3 μg/mL) |
| 112 | 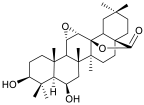 | S. tonkinensis | HL-60 (IC50 = 27.5 μg/mL) |
| 116 | 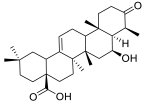 | S. tonkinensis | HL-60 (IC50 = 14.2 μg/mL) |
| 118 |  | S. tonkinensis | HL-60 (IC50 = 29.0 μg/mL) |
| 119 | 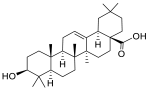 | S. tonkinensis | HL-60 (IC50 = 8.9 μg/mL) |
| 125 | 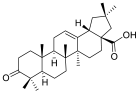 | S. tonkinensis | hCES1A (IC50 = 0.49 mg/mL) |
| 126 | 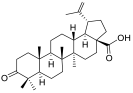 | S. tonkinensis | hCES1A (IC50 = 1.48 μg/mL) |
| 129 | 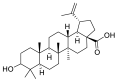 | S. tonkinensis | hCES1A (IC50 = 0.041 μg/mL) |
| 144 | 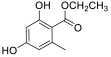 | S. suberifolius | A. solani (inhibition rate = 58.41% at 100 μg/mL) F. oxysporum (inhibition rate = 67.39% at 100 μg/mL) |
| 145 | 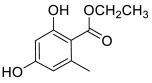 | S. suberifolius | A. solani (inhibition rate = 59.31% at 100 μg/mL) F. oxysporum (inhibition rate = 45.65% at 100 μg/mL) |
| 146 | 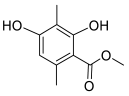 | S. suberifolius | F. oxysporum (inhibition rate = 61.41% at 100 μg/mL) P. cytospore (inhibition rate = 86.72% at 100 μg/mL) |
| 149 | 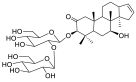 | S.macranthus | iNOS, COX-2, TNF-a, and IL-1b |
| 152 | 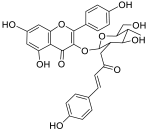 | S. pohlii S. camporum | Separate coupled Schistosoma mansoni adult worms |
| 155 | 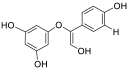 | S. pohlii S. camporum | Separate coupled Schistosoma mansoni adult worms Kill adult schistosomes |
| 156 | 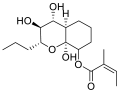 | S. pohlii | AChE |
| 158 | 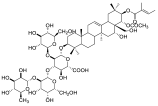 | S. japonica | Hemolytic activity (IC50 = 2.1 μg/mL) |
| 159 | 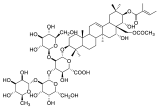 | S. japonica | Hemolytic activity (IC50 = 20.2 μg/mL) |
References
- Fritsch, P.W.; Almeda, F.; Renner, S.S.; Martins, A.B.; Cruz, B.C. Phylogeny and circumscription of the near-endemic Brazilian tribe Microlicieae (Melastomataceae). Am. J. Bot. 2004, 91, 1105–1114. [Google Scholar] [CrossRef]
- Pauletti, P.M.; Teles, H.L.; Silva, D.H.S.; Araújo, A.R.; Bolzani, V.S. The Styracaceae. Rev. Bras. Farmacogn. 2006, 16, 576–590. [Google Scholar] [CrossRef]
- Jiang, S. Dictionary of Chinese Materia Medical; Shanghai Scientific and Technical Publishing House: Shanghai, China, 1997; pp. 1723–1725. [Google Scholar]
- Wang, F.; Hua, H.; Pei, Y.; Chen, D.; Jing, K.Y. Triterpenoids from the Resin of Styrax tonkinensis and Their Antiproliferative and Differentiation Effects in Human Leukemia HL-60 Cells. J. Nat. Prod. 2006, 69, 807–810. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.B. Illustrated Flora of Korea; Hwang Mun Sa: Seoul, Republic of Korea, 1982; p. 614. [Google Scholar]
- Kitagawa, I.; Imakura, Y.; Hayashi, T.; Yosioka, I. Structure of deacyl-jegosaponin, a common deacyl derivative of jegosaponin isolated from pericarps of Styrax japonica Sieb. et Zucc. Chem. Pharm. Bull. 1974, 22, 1675–1677. [Google Scholar] [CrossRef] [PubMed]
- Min, B.S.; Na, M.K.; Oh, S.R.; Ahn, K.S.; Jeong, G.S.; Li, G.; Lee, S.K.; Joung, H.; Lee, H.K. New Furofuran and Butyrolactone Lignans with Antioxidant Activity from the Stem Bark of Styrax japonica. J. Nat. Prod. 2004, 67, 1980–1984. [Google Scholar] [CrossRef] [PubMed]
- He, L.; Zhou, Y.; Wan, G.J.; Wang, W.C.; Zhang, N.; Yao, L. Antinociceptive effects of flower extracts and the active fraction from Styrax japonicus. J. Ethnopharmacol. 2022, 284, 114779–114788. [Google Scholar] [CrossRef]
- Xie, Z.W. Compilation of Chinese Herbal Medicine; People’s Medical Publishing House: Beijing, China, 1975. [Google Scholar]
- Liu, J.; Dumontet, V.; Simonin, A. Benzofurans from Styrax agrestis as acetylcholinesterase inhibitors: Structure–activity relationships and molecular modeling studies. J. Nat. Prod. 2011, 74, 2081–2088. [Google Scholar] [CrossRef]
- Francielli de Oliveira, P.; Furtado, R.A.; Acésio, N.O.; Leandro, L.F.; Montanheiro, G.; de Padua, F.C.; Correa, M.B.; Braguini, C.G.; Pauletti, P.M.; Tavares, D.C. In Vivo Protective Activity of Styrax camporum Hydroalcoholic Extract against Genotoxicity Induced by Doxorubicin and Methyl Methanesulfonate in the Micronucleus and Comet Assays. Planta Med. 2012, 78, 1899–1905. [Google Scholar] [CrossRef]
- Lu, D.; Yang, L.; Li, Q.L.; Gao, X.P.; Wang, F.; Zhang, G.L. Egonol gentiobioside and egonol gentiotrioside from Styrax perkinsiae promote the biosynthesis of estrogen by aromatase. Eur. J. Pharmacol. 2012, 691, 275–282. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhao, X.C.; Xie, Y.G.; Fan, C.; Huang, Y.Y.; Yan, S.K.; Zhang, Y.; Jin, H.Z.; Zhang, W.D. Eight new γ-lactam alkaloids from the roots of the Hemerocallis minor Mill. Fitoterapia 2017, 118, 80–86. [Google Scholar] [CrossRef]
- Xie, Q.; Wu, G.Z.; Yang, N.; Shen, Y.H.; Tang, J.; Zhang, W.D. Delavatine A, an unusual isoquinoline alkaloid exerts anti-inflammation on LPS-induced proinflammatory cytokines production by suppressing NF-κB activation in BV-2 microglia. Biochem. Biophys. Res. Commun. 2018, 502, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Zhao, Q.; Lu, J.Z.; Ye, D.; Mu, S.; Yang, X.D.; Zhang, W.D.; Ma, B.L. Natural Nano-Drug Delivery System in Coptidis rhizoma Extract with Modified Berberine Hydrochloride Pharmacokinetics. Int. J. Nanomed. 2021, 16, 6297–6311. [Google Scholar] [CrossRef]
- Yuan, W.L.; Huang, Z.H.; Li, B.; Xiao, S.J.; Shen, X.P.; He, Y.Q.; Zhang, W.D.; Shen, Y.H. Trisecocycloartane triterpene dilactones from the cones of Pseudolarix amabilis. Phytochem. Lett. 2021, 45, 88–92. [Google Scholar] [CrossRef]
- Li, Q.; Guo, Y.; He, X.; Li, G. Bifunctional Cu(II)-containing PDA-PEI copolymer dots: Demonstration of a dual-mode platform for colorimetric-fluorescent detection of glyphosate in the environment. Talanta 2023, 265, 124865. [Google Scholar] [CrossRef]
- Chen, Q.F.; Chen, X.Z.; Li, G.Y.; Wang, C.; Zhang, G.L. Two new 2-phenylbenzofurans from the bark of Styrax perkinsiae. Chin. J. Nat. Med. 2012, 10, 92–97. [Google Scholar] [CrossRef]
- Pauletti, P.M.; Araújo, A.R.; Young, M.C.M.; Giesbrecht, A.M.; Bolzani, V.D.S. nor-Lignans from the leaves of Styrax ferrugineus (Styracaceae) with antibacterial and antifungal activity. Phytochemistry 2000, 55, 597–601. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Moon, H.; Chung, J.H.; Moon, Y.H.; Hahm, K.; Woo, E. Matrix metalloproteinase-1 inhibitor from the stem bark of Styrax japonica S. et Z. Chem. pharm. Bull. 2004, 52, 1466–1469. [Google Scholar] [CrossRef]
- Kim, M.; Moon, H.T.; Lee, D.G.; Woo, E.R. A new lignan glycoside from the stem bark of Styrax japonica S. et Z. Arch. Pharm. Res. 2007, 30, 425–430. [Google Scholar] [CrossRef]
- Min, B.; Oh, S.; Ahn, K. Anti-complement activity of norlignans and terpenes from the stem bark of Styrax japonica. Planta Med. 2004, 70, 1210–1215. [Google Scholar] [CrossRef]
- Wu, N.; Wang, L.; Chzn, Y.; Liao, Z.; Yang, G.Y.; Hu, Q.F. Lignans from the Stem of Styrax japonica. Asian J. Chem. 2011, 23, 931–932. [Google Scholar]
- KwanKwonwon, Y.; UnKim, S. Phytochemical studies on seeds of Styrax japonica Sieb. et Zucc. J. Appl. Biol. Chem. 2002, 45, 28–30. [Google Scholar]
- Hung, T.M.; Lee, M.K.; Min, B.; Kim, J.C.; Choi, J.S.; Lee, H.K. Two Lignans from the stem bark of Styrax japonica. J. Korean Soc. Appl. Biol. 2009, 52, 560–563. [Google Scholar] [CrossRef]
- Kinoshita, T.; Haga, Y.; Narimatsu, S. New nor-neolignan glycosides from Styrax obassla (Styracaceae). Heterocycles 2005, 65, 1471–1480. [Google Scholar] [CrossRef]
- Takanashi, M.; Takizawa, Y. New Egonol Glycoside Having D-Xylose, from Immature Seeds of Styrax obassia Sieb. et Zucc. J. Oleo Sci. 2002, 51, 423–426. [Google Scholar] [CrossRef]
- Takanashi, M.; Takizawa, Y. New benzofurans related to egonol from immature seeds of Styrax obassia. Phytochemistry 1988, 27, 1224–1226. [Google Scholar] [CrossRef]
- Takanashi, M.; Takizawa, Y.; Mitsuhashi, T. Determination of Mercury by Direct Heating of Mercury-Adsorbed Ion-Exchange Resin in Electrothermal Atomic Absorption Spectrometr. Chem. Lett. 1974, 8, 869–871. [Google Scholar] [CrossRef]
- Park, S.Y.; Lee, H.; Lee, O.; Kang, H.; Choi, D.H.; Paik, K.H.; Khan, M. Benzofurans from the Seeds of Styrax obassia. Bull. Korean Chem. Soc. 2007, 28, 1874. [Google Scholar]
- Lee, H.J.; Park, S.Y.; Lee, O.K.; Jo, H.J.; Kang, H.Y.; Choi, D.H.; Paik, K.H.; Khan, M. Benzofurans and sterol from the seeds of Styrax obassia. Chem. Nat. Compd. 2008, 44, 435–439. [Google Scholar] [CrossRef]
- Luo, Y.; He, Z.; Li, H. 2-Aryl benzofurans and their derivatives from seeds of Styrax macranthus. Fitoterapia 2007, 78, 211–214. [Google Scholar] [CrossRef]
- Schneiders, G.E.; Stevenson, R. Synthesis of (.+-.)-machicendiol. J. Org. Chem. 1979, 44, 4710–4711. [Google Scholar] [CrossRef]
- Anil, H. Four benzofurans glycosides from Styrax officinalis. Phytochemistry 1980, 19, 2784–2786. [Google Scholar] [CrossRef]
- Akgul, Y.Y.; Anil, H. Benzofuran from seeds of Styrax officinalis. Fitoterapia 2003, 74, 743–745. [Google Scholar] [CrossRef] [PubMed]
- Akgul, Y.Y.; Anil, H. Benzofurans and another constituent from seeds of Styrax officinalis. Phytochemistry 2003, 63, 939–943. [Google Scholar] [CrossRef] [PubMed]
- Bacchi, E.M.; Sertie, J.A.; Villa, N.; Katz, H. Antiulcer action and toxicity of Styrax camporum and Caesalpinia ferrea. Planta Med. 1995, 61, 204–207. [Google Scholar] [CrossRef] [PubMed]
- Teles, H.L.; Hemerly, J.P.; Pauletti, P.M. Cytotoxic lignans from the stems of Styrax camporum (Styracaceae). Nat. Prod. Res. 2005, 19, 319–323. [Google Scholar] [CrossRef]
- Zhang, P.Z.; Zhang, Y.M. Tetrahydrofuranoid Lignans from Stem Bark of Styrax perkinsiae. Chin. J. Exp. Tradit. Med. Formulae 2015, 21, 91–94. [Google Scholar]
- Liu, B.L.; Ding, W.B.; Huang, S.Y.; Sun, W.H.; Li, Y.Z. Chemotaxonomic significance of phenylpropanoids from Styrax suberifolius Hook. Et Arn. Biochem. Syst. Ecol. 2018, 78, 35–38. [Google Scholar] [CrossRef]
- Hu, W.L.; Li, Z.L.; Chen, Q.J.; Sun, Y.W.; Zhai, S.; Lu, F.; Zhang, C.F. Triterpenes and lignans from the leaves of Styrax tonkinensis. Biochem. Systemat. Ecol. 2019, 86, 103891. [Google Scholar] [CrossRef]
- Wang, F.; Zhang, L.; Zhang, Q.; Chen, A.; Wang, S.M.; Fang, Z.F. Two new phenylpropanoids from the resin of Styrax tonkinensis (Pierre) Craib ex Hartw. J. Nat. Med. 2020, 74, 819–824. [Google Scholar] [CrossRef]
- Tra, N.T.; Tuyen, N.V.; Cuong, P.V.; Ha, N.T.T.; Anh, L.T.T.; Son, T.N. Chemical constituents from the leaves of Styrax argentifolius H.L. Li and their biological activities. Phytochem. Lett. 2021, 41, 70–73. [Google Scholar] [CrossRef]
- Moon, H.; Kim, M.; Woo, E.; Chung, J.H. Triterpenoid from Styrax japonica SIEB. et ZUCC, and its effects on the expression of matrix metalloproteinases-1 and type 1 procollagen caused by ultraviolet irradiated cultured primary human skin fibroblasts. Biol. Pharm. Bull. 2005, 28, 2003–2006. [Google Scholar] [CrossRef] [PubMed]
- Yun, K.; Min, B.; Kim, J.; Lee, K.T. Styraxoside A isolated from the stem bark of Styrax japonica inhibits lipopolysaccharide-induced expression of inducible nitric oxide synthase and cyclooxygenase-2 in RAW 264.7 cells by suppressing nuclear factor-kappa B activation. Biol. Pharm. Bull. 2007, 30, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Yoshikawa, K.; Hirai, H.; Tanaka, M. Antisweet Natural Products. XV. Structures of Jegosaponins AD from Styrax japonica SIEB. et Zucc. Chem. Pharm. Bull. 2000, 48, 1093–1096. [Google Scholar] [CrossRef] [PubMed]
- Kwon, J.H.; Chang, M.J.; Seo, H.W.; Lee, J.H.; Min, B.S.; Na, M.; Kim, J.C.; Woo, M.H.; Choi, J.S.; Lee, H.K. Triterpenoids and a sterol from the stem-bark of Styrax japonica and their protein tyrosine phosphatase 1B inhibitory activities. Phytother. Res. 2008, 22, 1303–1306. [Google Scholar] [CrossRef] [PubMed]
- Anil, H. 21-Benzoyl-barringtogenol C, a sapogenin from Styrax officinalis. Phytochemistry 1979, 18, 1760–1761. [Google Scholar] [CrossRef]
- Yayla, Y.; Alankuş-Çalışkan, Ö.; Anıl, H.; BBates, R.; Stessman, C.; Kane, V. Saponins from Styrax officinalis. Fitoterapia 2002, 73, 320–326. [Google Scholar] [CrossRef]
- Tayoub, G.; Schwob, I.; Bessiere, J.; Masotti, V.; Rabier, J.; Ruzzier, M.; Viano, J. Composition of volatile oils of Styrax (Styrax officinalis L.) leaves at different phenological stages. Biochem. Syst. Ecol. 2006, 34, 705–709. [Google Scholar] [CrossRef]
- Wang, L.; Guan, X.Q.; He, R.J.; Huo, P.C.; Qin, W.W.; Cui, L.T.; Hu, Q.; Hou, J.; Mamat, M.; Jia, S.N.; et al. Discovery and characterization of pentacyclic triterpenoid acids in Styrax as potent and reversible pancreatic lipase inhibitors. J. Funct. Foods 2020, 74, 104159. [Google Scholar] [CrossRef]
- Wang, F.; Hua, H.; Bian, X.; Pei, Y.H.; Jing, K.Y. Two new aromatic compounds from the resin of Styrax tonkinensis (Pier.) Craib. J. Asian Nat. Prod. Res. 2006, 8, 137–141. [Google Scholar] [CrossRef]
- Wang, F.; Fang, Z.F. Chemical Constituents from Resin of Styrax tonkinensis. Chin. J. Exp. Tradi. Med. Formulae 2012, 18, 17. [Google Scholar]
- Kim, M.; Lee, H.; Hahm, K.; Moon, Y.H.; Woo, E. Pentacyclic triterpenoids and their cytotoxicity from the stem bark of Styrax japonica S. et Z. Arch. Pharm. Res. 2004, 27, 283–286. [Google Scholar] [CrossRef]
- Vardar, Y.; Oflas, S. Preliminary studies on the Styrax oil. Qual. Plant. Mater. Veg. 1973, 22, 145–148. [Google Scholar] [CrossRef]
- Braguine, C.G.; Bertanha, C.S.; Gonçalves, U.O.; Magalhães, L.G.; Rodrigues, V.; Gimenez, V.M.M. Schistosomicidal evaluation of flavonoids from two species of Styrax against Schistosoma mansoni adult worms. Pharm. Biol. 2012, 50, 925–929. [Google Scholar] [CrossRef] [PubMed]
- Biasettoa, C.R.; Somensia, A.; Sordia, R.; Chaplab, V.M.; Ebrahimic, S.N.; Silvad, G.H.; Telese, H.L.; Bolzania, V.S.; Youngf, M.C.M.; Pfenningg, L.H.; et al. The new koninginins T-U from Phomopsis stipata, an endophytic fungus isolated from Styrax camporum Pohl. Phytochem. Lett. 2020, 36, 106–110. [Google Scholar] [CrossRef]
- Nishimura, M.; Fuchino, H.; Takayanagi, K.; Kawakami, H.; Nakayama, H.; Kawahara, H.; Shimada, Y. Toxicity of Jegosaponins A and B from Styrax japonica Siebold et al., Zuccarini in Prostate Cancer Cells and Zebrafish Embryos Resulting from Increased Membrane Permeability. Int. J. Mol. Sci. 2021, 22, 6354. [Google Scholar] [CrossRef]
- Francielli de Oliveira, P.; Damasceno, J.L.; Bertanha, C.S.; Bertanha, C.S.; Araujo, A.R.B.; Pauletti, P.M.; Tavares, D.C. Study of the cytotoxic activity of Styrax camporum extract and its chemical markers, egonol and homoegonol. Cytotechnology 2016, 68, 1597–1602. [Google Scholar] [CrossRef]
- Cao, T.Q.; Lee, B.M.; Jung, Y.W.; Nguyen, V.T.; Kim, J.A.; Min, B.S. Cytotoxic Activity of Compounds from Styrax obassia. Nat. Prod. Commun. 2017, 12, 259–260. [Google Scholar] [CrossRef]
- Bertanha, C.S.; Utrera, S.H.; Gimenez, V.M.M.; Groppo, M.; Silva, M.; Cunhua, W.R.; Martins, C.H.G.; Januário, A.H.; Pauletti, P.M. Antibacterial evaluation of Styrax pohlii and isolated compounds. Braz. J. Med. Biol. Res. 2013, 49, 653–658. [Google Scholar] [CrossRef]
- Lee, J.; Lim, K. Apoptotic activity of ethanol extract from Styrax Japonica Siebold et al. Zuccarini in HepG2 cells. J. Ethnopharmacol. 2010, 131, 210–215. [Google Scholar] [CrossRef]
- Lee, J.; Lim, K. Inhibitory effect of Styrax Japonica Siebold et al., Zuccarini glycoprotein (38 kDa) on interleukin-1β and induction proteins in chromium (VI)-treated BNL CL. 2 cells. Mol. Cell Biochem. 2012, 367, 103–111. [Google Scholar] [CrossRef]
- Lee, J.; Lim, K. SJSZ glycoprotein (38 kDa) modulates expression of IL-2, IL-12, and IFN-γ in cyclophosphamide-induced Balb/c. Inflamm. Res. 2012, 61, 1319–1328. [Google Scholar] [CrossRef] [PubMed]
- Schreiber, F.G.; Stevenson, R. Synthesis of benzofuran Styrax extractives. J. Chem. Soc. Perkin Trans. 1976, 1, 1514–1518. [Google Scholar] [CrossRef]
- Moon, H.; Lee, J.; Chung, J.H. The effect of erythrodiol-3-acetate on the expressions of matrix metalloproteinase-1 and type-1 procollagen caused by ultraviolet irradiated cultured primary old aged human skin fibroblasts. Phytomedicine 2006, 13, 707–711. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Lim, K. Inhibitory effect of phytoglycoprotein (38 kDa) on expression of matrix metalloproteinase-9 in 12-O-tetradecanoylphorbol-13-acetate-treated HepG2cells. Naunyn Schmiedebergs Arch. pharmacol. 2011, 384, 185–196. [Google Scholar] [CrossRef] [PubMed]
- Bacchi, E.M.; Sertie, J.A. Antiulcer action of Styrax camporum and Caesalpinia ferrea in rats. Planta Med. 1994, 60, 118–120. [Google Scholar] [CrossRef]
- Bertanha, C.S.; Braguine, C.G.; Moraes, A.G.; Gimenez, V.M.; Groppo, M.; Silva, M.; Cunhua, W.R.; Januário, A.H.; Pauletti, P.M. Cyclooxygenase inhibitory properties of nor-neolignans from Styrax pohlii. Nat. Prod. Res. 2012, 26, 2323–2329. [Google Scholar] [CrossRef]
- Bertanha, C.S.; Soares, E.; Gonçalves, U.O.; Francielli de Oliveira, P.; Magalhães, L.G.; Rodrigues, V.; Tavares, D.C.; Andrade e Silva, M.L.; Cunha, W.R.; Januário, A.H.; et al. In vitro Antischistosomal and Cytotoxic Activities of Norneolignans from Styrax pohlii A. DC. J. Herbs Spices Med. Plants 2014, 20, 394–401. [Google Scholar] [CrossRef]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xia, D.-D.; Han, X.-Y.; Zhang, Y.; Zhang, N. Chemical Constituents and Their Biological Activities from Genus Styrax. Pharmaceuticals 2023, 16, 1043. https://doi.org/10.3390/ph16071043
Xia D-D, Han X-Y, Zhang Y, Zhang N. Chemical Constituents and Their Biological Activities from Genus Styrax. Pharmaceuticals. 2023; 16(7):1043. https://doi.org/10.3390/ph16071043
Chicago/Turabian StyleXia, Ding-Ding, Xin-Yu Han, Yu Zhang, and Na Zhang. 2023. "Chemical Constituents and Their Biological Activities from Genus Styrax" Pharmaceuticals 16, no. 7: 1043. https://doi.org/10.3390/ph16071043
APA StyleXia, D.-D., Han, X.-Y., Zhang, Y., & Zhang, N. (2023). Chemical Constituents and Their Biological Activities from Genus Styrax. Pharmaceuticals, 16(7), 1043. https://doi.org/10.3390/ph16071043







