Pulmonary-Renal Syndrome from Levamisole-Adulterated Cocaine-Induced Antineutrophil Cytoplasmic Antibody (ANCA)-Associated Vasculitis: A Systematic Review
Abstract
1. Introduction
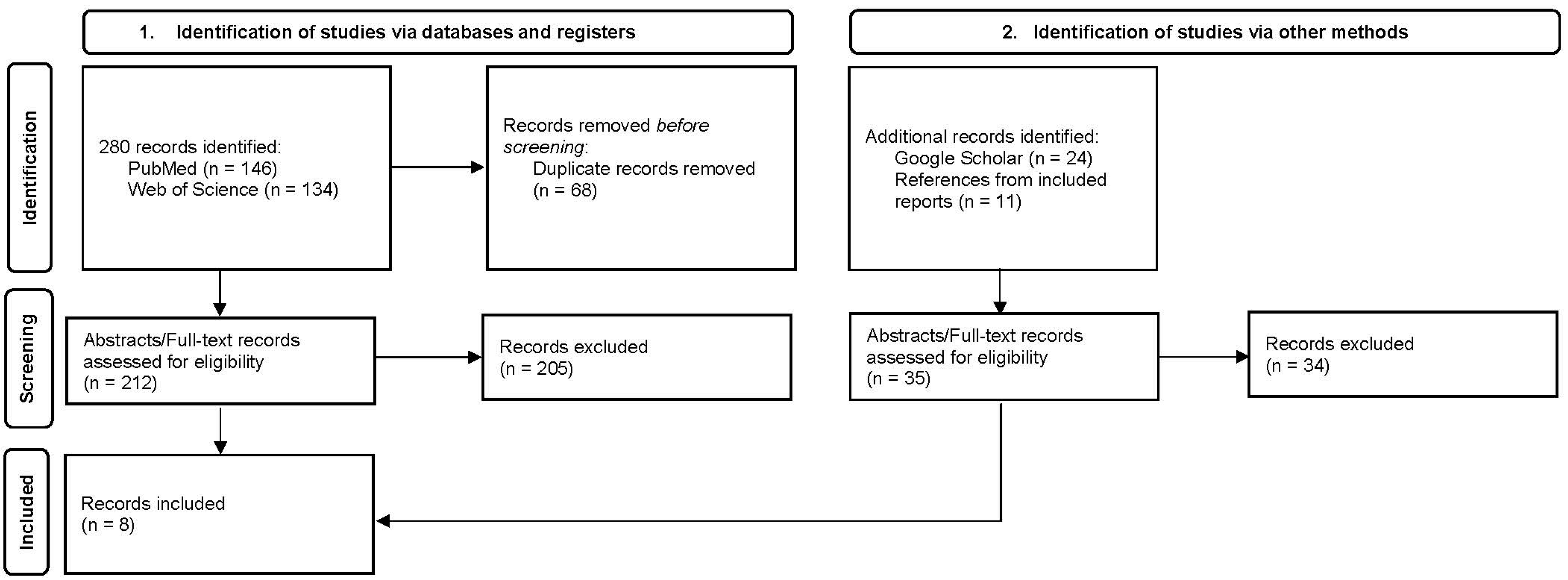
2. Methods
3. Results
3.1. Patient Characteristics
3.2. Clinical and Pathologic Features
3.3. Serologic and Other Laboratory Findings
3.4. Treatment and Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Amery, W.K.; Bruynseels, J.P. Levamisole, the story and the lessons. Int. J. Immunopharmacol. 1992, 14, 481–486. [Google Scholar] [CrossRef]
- Rattay, B.; Benndorf, R.A. Drug-Induced Idiosyncratic Agranulocytosis-Infrequent but Dangerous. Front. Pharmacol. 2021, 12, 727717. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.C.; Ladizinski, B.; Federman, D.G. Complications associated with use of levamisole-contaminated cocaine: An emerging public health challenge. Mayo Clin. Proc. 2012, 87, 581–586. [Google Scholar] [CrossRef]
- Berman, M.; Paran, D.; Elkayam, O. Cocaine-Induced Vasculitis. Rambam Maimonides Med. J. 2016, 7, e0036. [Google Scholar] [CrossRef] [PubMed]
- Aoun, B.; Alali, M.; Degheili, J.A.; Sanjad, S.; Vaquin, C.; Donadieu, J.; Ulinski, T.; Termos, S. Distinctive vasculopathy with systemic involvement due to levamisole long-term therapy: A case report. J. Med. Case Rep. 2018, 12, 209. [Google Scholar] [CrossRef]
- Barbano, G.; Ginevri, F.; Ghiggeri, G.M.; Gusmano, R. Disseminated autoimmune disease during levamisole treatment of nephrotic syndrome. Pediatr. Nephrol. 1999, 13, 602–603. [Google Scholar] [CrossRef]
- Tello, N.; Parra, J. Levamisole Induced Autoimmunity. J. Arthritis 2015, 5, 1–3. [Google Scholar] [CrossRef]
- Tallarida, C.S.; Egan, E.; Alejo, G.D.; Raffa, R.; Tallarida, R.J.; Rawls, S.M. Levamisole and cocaine synergism: A prevalent adulterant enhances cocaine’s action in vivo. Neuropharmacology 2014, 79, 590–595. [Google Scholar] [CrossRef] [PubMed]
- Castaldelli-Maia, J.M.; Bhugra, D. Analysis of global prevalence of mental and substance use disorders within countries: Focus on sociodemographic characteristics and income levels. Int. Rev. Psychiatry 2022, 34, 6–15. [Google Scholar] [CrossRef]
- Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950–2019: A comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1160–1203. [CrossRef]
- Centers for Disease Contral and Prevention (CDC). Agranulocytosis associated with cocaine use-four States, March 2008–November 2009. MMWR Morb. Mortal. Wkly. Rep. 2009, 58, 1381–1385. [Google Scholar]
- Hesse, M.; Thomsen, K.R.; Thylstrup, B.; Andersen, C.U.; Reitzel, L.A.; Worm-Leonhard, M.; Lindholst, C. Purity of street-level cocaine across Denmark from 2006 to 2019: Analysis of seized cocaine. Forensic Sci. Int. 2021, 329, 111050. [Google Scholar] [CrossRef]
- Lynch, K.L.; Dominy, S.S.; Graf, J.; Kral, A.H. Detection of levamisole exposure in cocaine users by liquid chromatography-tandem mass spectrometry. J. Anal. Toxicol. 2011, 35, 176–178. [Google Scholar] [CrossRef] [PubMed]
- McGrath, M.M.; Isakova, T.; Rennke, H.G.; Mottola, A.M.; Laliberte, K.A.; Niles, J.L. Contaminated cocaine and antineutrophil cytoplasmic antibody-associated disease. Clin. J. Am. Soc. Nephrol. 2011, 6, 2799–2805. [Google Scholar] [CrossRef] [PubMed]
- Dartevel, A.; Chaigne, B.; Moachon, L.; Grenier, F.; Dupin, N.; Guillevin, L.; Bouillet, L.; Mouthon, L. Levamisole-induced vasculopathy: A systematic review. Semin. Arthritis Rheum. 2019, 48, 921–926. [Google Scholar] [CrossRef]
- Khokhar, B.; Jette, N.; Metcalfe, A.; Cunningham, C.T.; Quan, H.; Kaplan, G.G.; Butalia, S.; Rabi, D. Systematic review of validated case definitions for diabetes in ICD-9-coded and ICD-10-coded data in adult populations. BMJ Open 2016, 6, e009952. [Google Scholar] [CrossRef]
- Perkovic, V.; Jardine, M.J.; Neal, B.; Bompoint, S.; Heerspink, H.J.L.; Charytan, D.M.; Edwards, R.; Agarwal, R.; Bakris, G.; Bull, S.; et al. Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. N. Engl. J. Med. 2019, 380, 2295–2306. [Google Scholar] [CrossRef]
- Cregler, L.L.; Mark, H. Medical complications of cocaine abuse. N. Engl. J. Med. 1986, 315, 1495–1500. [Google Scholar] [CrossRef]
- Trimarchi, M.; Gregorini, G.; Facchetti, F.; Morassi, M.L.; Manfredini, C.; Maroldi, R.; Nicolai, P.; Russell, K.A.; McDonald, T.J.; Specks, U. Cocaine-induced midline destructive lesions: Clinical, radiographic, histopathologic, and serologic features and their differentiation from Wegener granulomatosis. Medicine 2001, 80, 391–404. [Google Scholar] [CrossRef]
- Haim, D.Y.; Lippmann, M.L.; Goldberg, S.K.; Walkenstein, M.D. The pulmonary complications of crack cocaine. A comprehensive review. Chest 1995, 107, 233–240. [Google Scholar] [CrossRef]
- Godwin, J.E.; Harley, R.A.; Miller, K.S.; Heffner, J.E. Cocaine, pulmonary hemorrhage, and hemoptysis. Ann. Intern. Med. 1989, 110, 843. [Google Scholar] [CrossRef] [PubMed]
- Kannan, L. Renal manifestations of recreational drugs: A narrative review of the literature. Medicine 2022, 101, e31888. [Google Scholar] [CrossRef]
- Boyle, N.; O’Callaghan, M.; Ataya, A.; Gupta, N.; Keane, M.P.; Murphy, D.J.; McCarthy, C. Pulmonary renal syndrome: A clinical review. Breathe 2022, 18, 220208. [Google Scholar] [CrossRef] [PubMed]
- West, S.C.; Arulkumaran, N.; Ind, P.W.; Pusey, C.D. Pulmonary-renal syndrome: A life threatening but treatable condition. Postgrad. Med. J. 2013, 89, 274–283. [Google Scholar] [CrossRef] [PubMed]
- Berlioz, A.R.; Garner, O.; Wiesner, E.; Iardino, A.; Bhairavarasu, K. Severe ANCA Associated Vasculitis in the Setting of Cocaine Abuse: A Case Report. Clin. Med. Rev. Case Rep. 2017, 4, 177. [Google Scholar] [CrossRef]
- Carlson, A.Q.; Tuot, D.S.; Jen, K.Y.; Butcher, B.; Graf, J.; Sam, R.; Imboden, J.B. Pauci-Immune Glomerulonephritis in Individuals With Disease Associated With Levamisole-Adulterated Cocaine A Series of 4 Cases. Medicine 2014, 93, 290–297. [Google Scholar] [CrossRef]
- Collister, D.; Sathianathan, C.; Ryz, K.; Karpinski, M.; Bernstein, K.; Gibson, I.W. ANCA Associated Vasculitis Secondary to Levamisole-Adultered Cocaine with Associated Membranous Nephropathy: A Case Series. Am. J. Nephrol. 2017, 45, 209–216. [Google Scholar] [CrossRef]
- Habibullah, J.M.; Lou, B.; Tsegaye, A. It’s in Her Story a Case of Cocaine Vasculitis. Am. J. Respir. Crit. Care Med. 2019, 199, A1480. [Google Scholar]
- Pecci, E.; Gregorini, G.; Sinigaglia, P.; Bozzola, G.; Tassi, G.; Ferremi, P.; Latronico, N. Diffuse alveolar haemorrhage (DAH) in levamisole-adultered cocaine abuser resolved by rFVIIa infusion. Presse Medicale 2013, 42, 671–672. [Google Scholar] [CrossRef]
- Neynaber, S.; Mistry-Burchardi, N.; Rust, C.; Samtleben, W.; Burgdorf, W.H.; Seitz, M.A.; Messer, G.; Wollenberg, A. PR3-ANCA-positive necrotizing multi-organ vasculitis following cocaine abuse. Acta Derm. Venereol. 2008, 88, 594–596. [Google Scholar] [CrossRef]
- Restrepo-Escobar, M.; Sylva, D.; Gamboa, J.G.; Echeverri, A.; Márquez, J.; Pinto, L.F. Pulmonary-renal syndrome secondary to cocaine-levamisole-induced vasculitis: A case report. Reumatol. Clin. 2020, 16, 239–241. [Google Scholar] [CrossRef] [PubMed]
- Voong, C.; Patel, H. Levamisole-Adulterated Cocaine Leading to Pulmonary Renal Syndrome: A Case Report. Am. J. Respir. Crit. Care Med. 2022, 205, A2630. [Google Scholar]
- Chung, S.A.; Langford, C.A.; Maz, M.; Abril, A.; Gorelik, M.; Guyatt, G.; Archer, A.M.; Conn, D.L.; Full, K.A.; Grayson, P.C.; et al. 2021 American College of Rheumatology/Vasculitis Foundation Guideline for the Management of Antineutrophil Cytoplasmic Antibody-Associated Vasculitis. Arthritis Rheumatol. 2021, 73, 1366–1383. [Google Scholar] [CrossRef] [PubMed]
- Jayne, D.R.W.; Merkel, P.A.; Schall, T.J.; Bekker, P. Avacopan for the Treatment of ANCA-Associated Vasculitis. N. Engl. J. Med. 2021, 384, 599–609. [Google Scholar] [CrossRef]
- Marquez, J.; Aguirre, L.; Muñoz, C.; Echeverri, A.; Restrepo, M.; Pinto, L.F. Cocaine-Levamisole-Induced Vasculitis/Vasculopathy Syndrome. Curr. Rheumatol. Rep. 2017, 19, 36. [Google Scholar] [CrossRef]
- Nolan, A.L.; Jen, K.Y. Pathologic manifestations of levamisole-adulterated cocaine exposure. Diagn. Pathol. 2015, 10, 48. [Google Scholar] [CrossRef]
- Gulati, S.; Donato, A.A. Lupus anticoagulant and ANCA associated thrombotic vasculopathy due to cocaine contaminated with levamisole: A case report and review of the literature. J. Thromb. Thrombolysis 2012, 34, 7–10. [Google Scholar] [CrossRef] [PubMed]
- Savige, J.; Pollock, W.; Trevisin, M. What do antineutrophil cytoplasmic antibodies (ANCA) tell us? Best Pr. Res. Clin. Rheumatol. 2005, 19, 263–276. [Google Scholar] [CrossRef]
- Graf, J.; Lynch, K.; Yeh, C.L.; Tarter, L.; Richman, N.; Nguyen, T.; Kral, A.; Dominy, S.; Imboden, J. Purpura, cutaneous necrosis, and antineutrophil cytoplasmic antibodies associated with levamisole-adulterated cocaine. Arthritis Rheum. 2011, 63, 3998–4001. [Google Scholar] [CrossRef]
- Wiesner, O.; Russell, K.A.; Lee, A.S.; Jenne, D.E.; Trimarchi, M.; Gregorini, G.; Specks, U. Antineutrophil cytoplasmic antibodies reacting with human neutrophil elastase as a diagnostic marker for cocaine-induced midline destructive lesions but not autoimmune vasculitis. Arthritis Rheum. 2004, 50, 2954–2965. [Google Scholar] [CrossRef]
- Wiik, A. Drug-induced vasculitis. Curr. Opin. Rheumatol. 2008, 20, 35–39. [Google Scholar] [CrossRef]
- Larocque, A.; Hoffman, R.S. Levamisole in cocaine: Unexpected news from an old acquaintance. Clin. Toxicol. 2012, 50, 231–241. [Google Scholar] [CrossRef]
- Lood, C.; Hughes, G.C. Neutrophil extracellular traps as a potential source of autoantigen in cocaine-associated autoimmunity. Rheumatology 2017, 56, 638–643. [Google Scholar] [CrossRef]
- Kouassi, E.; Caillé, G.; Léry, L.; Larivière, L.; Vézina, M. Novel assay and pharmacokinetics of levamisole and p-hydroxylevamisole in human plasma and urine. Biopharm. Drug Dispos. 1986, 7, 71–89. [Google Scholar] [CrossRef] [PubMed]
- Reid, J.M.; Kovach, J.S.; O’Connell, M.J.; Bagniewski, P.G.; Moertel, C.G. Clinical and pharmacokinetic studies of high-dose levamisole in combination with 5-fluorouracil in patients with advanced cancer. Cancer Chemother. Pharm. 1998, 41, 477–484. [Google Scholar] [CrossRef] [PubMed]
- Cascio, M.J.; Jen, K.Y. Cocaine/levamisole-associated autoimmune syndrome: A disease of neutrophil-mediated autoimmunity. Curr. Opin. Hematol. 2018, 25, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Cohen Tervaert, J.W. Rituximab in ANCA-associated vasculitis: A revolution? Nephrol. Dial. Transpl. 2011, 26, 3077–3079. [Google Scholar] [CrossRef] [PubMed]
- Walsh, M.; Merkel, P.A.; Peh, C.A.; Szpirt, W.M.; Puéchal, X.; Fujimoto, S.; Hawley, C.M.; Khalidi, N.; Floßmann, O.; Wald, R.; et al. Plasma Exchange and Glucocorticoids in Severe ANCA-Associated Vasculitis. N. Engl. J. Med. 2020, 382, 622–631. [Google Scholar] [CrossRef] [PubMed]
- Garg, L.; Gupta, S.; Swami, A.; Zhang, P. Levamisole/Cocaine Induced Systemic Vasculitis and Immune Complex Glomerulonephritis. Case Rep. Nephrol. 2015, 2015, 372413. [Google Scholar] [CrossRef]
- Olives, T.D.; Kornas, R.L.; Fujisawa, R.; Cole, J.B. Unexpected Complication of Cocaine-Associated Anti-Neutrophil Cytoplasmic Antibody Vasculitis Related to Persistent In-Hospital Cocaine Use. J. Addict. Med. 2017, 11, 157–160. [Google Scholar] [CrossRef]
| Reference | Age (Years) | Sex | Race, Ethnicity | Duration of Vasculitis Prior to PRS | Evidence for Levamisole Exposure | Evidence for DAH | Evidence for RPGN | Skin Lesions | Other Vasculitis Findings | Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Neynaber et al., 2008 [30] | 22 | M | NR, NR | PRS at presentation | Cocaine use x 2 years by history | CXR: dense infiltrates in the RUL and RML compatible with pneumonia and intra-alveolar hemorrhage; Bronchoscopy: no infectious agent; No response to Abx therapy and rapid response to immune-suppression | Renal bx: focal and segmental pauci-immune, crescentic RPGN | Nodules and plaques; skin bx: leukocytoclastic vasculitis of small and medium-sized dermal vessels with fibrinoid necrosis; direct IF: positive for IgM (large), and lesser amounts of IgG, IgA and C3 | Destruction of nasal septum, testicular vasculitis, venous thrombosis | oral CYC, high-dose steroids | Recovery |
| Pecci et al., 2013 [29] | 37 | M | NR, NR | PRS at presentation | Cocaine use by history | CT chest: right interstitial diffuse alveolar infiltrates; Bronchoscopy: ongoing bleeding from the right bronchial tree & no infectious agent; Bronchial bx: vasculitis | Urinalysis: Hematuria, proteinuria | Purpura and necrosis of legs and earlobes | Arthralgia, malaise, perforated nasal septum | high-dose steroids, plasmapheresis, intravenous rFVIIa for refractory DAH | Recovery |
| Carlson et al., 2014 [26] | 49 | F | NR, NR | Five months (untreated renal involvement preceding PRS) | UDS: +cocaine | CXR: Bilateral pulmonary infiltrates; Bronchoscopy consistent with DAH | Renal bx: Focal segmental and global sclerosing glomerulopathy with cellular crescents, pauci-immune | Leg ulcers; skin bx: leukocytoclastic vasculitis with fibrin thrombi of superficial and deep dermal vessels | None reported | IV CYC, high-dose steroids, plasmapheresis, hemodialysis | Dialysis dependent |
| Collister et al., 2017 [27] | 35 | M | White, NR | PRS at presentation | UDS: +cocaine; LC-MS: +levamisole | CT chest: bilateral ground glass opacifications in the setting of hemoptysis and iron deficiency anemia | Renal bx: Membranous nephropathy with fibrinoid necrosis and crescent formation; IF: mesangial and capillary loop IgG (1-2+), IgM (1+), C3 (1+), trace C1q, and lambda (1+) and negative for IgA, fibrinogen, and kappa | NR | Distal symmetric polyarthritis, chronic epistaxis | IV CYC, high-dose steroids followed by steroid taper, maintenance azathioprine (did not tolerate) and ACEI | Recovery with residual CKD stage 3A |
| Berlioz et al., 2017 [25] | 41 | F | NR, Hispanic | Six years | UDS: +cocaine | CT chest: prominent bilateral patchy infiltrates and symmetric moderate pleural effusions; Bronchoscopy: confirmed DAH | Renal bx: Focal segmental necrotizing and sclerosing GN; membranous nephropathy also present | Tender skin erythema of nose, extremities; skin bx: neutrophil-rich infiltrate around the vessels of the dermis with fibrin thrombi within the superficial vessels → widespread skin bullae & necrosis | Arthralgia, Generalized weakness, new onset systolic heart failure | High-dose steroids, rituximab, then CYC (for worsening renal function) | Immune suppression complicated by a severe skin infection, but, ultimately, recovery |
| Habibullah, Lou, & Tsegaye, 2019 [28] | 53 | F | NR, NR | PRS at presentation | Cocaine use by history | CT chest: bilateral ground-glass and consolidated opacities; Bronchoscopy: confirmed DAH with increasing blood on serial aliquots | Renal bx: Advanced global and segmental glomerulosclerosis with healed, chronic, crescentic GN | NR | Fever, epistaxis | High-dose steroids, hemodialysis | Dialysis dependent |
| Restrepo-Escobar et al., 2020 [31] | 34 | M | NR, NR | PRS at presentation | Cocaine abuse by history | CXR: diffuse pulmonary infiltrates; CT chest: generalized mixed opacities bilateral lungs; Bronchoscopy: confirmed DAH with 40% hemosiderin-laden macrophages | Renal bx: Diffuse endocapillary GN with immune complex depositis and tubulointerstitial nephritis | NR | Generalized discomfort; perforated nasal septum | High-dose steroids → IV CYC (for only partial renal improvement) | Partial renal recovery |
| Voong & Patel, 2022 [32] | 58 | F | NR, NR | Existing diagnosis of LAC-induced AAV of duration not reported | UDS: +cocaine | CXR: severe pulm edema with bilateral opacities in the setting of severe hemoptysis | Renal bx: Diffuse necrotizing and crescentic GN | NR | NR | High-dose steroids, rituximab, hemodialysis | Respiratory status improved; renal status not reported |
| Reference | Age (Years) | Sex | Race, Ethnicity | C-ANCA | P-ANCA | PR3 Ab | MPO Ab | APLA | ANA | Other Abs | Cr (mg/dL) | Urine Protein | Urine Blood | Urine Microscopy |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Neynaber et al., 2008 [30] | 22 | M | NR, NR | pos 1:640 | neg | pos | neg | NR | neg | NR | 1.5 | pos (nephrotic range) | pos | NR |
| Pecci et al., 2013 [29] | 37 | M | NR, NR | NR | NR | NR | pos | neg (NOS which Abs) | NR | NR | “Normal” | pos | pos | NR |
| Carlson et al., 2014 [26] | 49 | F | NR, NR | neg | pos 1:5120 | neg | pos | Cardiolipin IgM: pos LAC: pos | neg | NR | 7.31 | pos (nephrotic range) | pos | Dysmorphic RBCs |
| Collister et al., 2017 [27] | 35 | M | White, NR | neg | pos | 24 RU/mL * | pos | NR | neg | GBM Ab: neg Cryo: neg dsDNA: 9 IU/mL * RF: 11 IU/mL * | 1.7 | pos (nephrotic range) | pos | Dysmorphic RBCs |
| Berlioz et al., 2017 [25] | 41 | F | NR, Hispanic | neg | pos 1:5120 | neg | pos | Cardiolipin IgG: neg Cardiolipin IgM: neg Beta-2-glycoprotein: neg (Ig not specified) | pos 1:160, speckled | dsDNA: pos 1:160 RF: neg Anti-SMA: neg Anti-CCP: neg | 6.3 | pos | pos | NR |
| Habibullah, Lou, & Tsegaye, 2019 [28] | 53 | F | NR, NR | neg | pos 1:80 | neg | neg | NR | NR | NR | “Acute renal failure” | NR | NR | NR |
| Restrepo-Escobar et al., 2020 [31] | 34 | M | NR, NR | NR | NR | pos | pos | Cardiolipin IgM: pos Cardiolipin IgG: neg LAC: pos Beta-2-glycoprotein-1 IgG: neg Beta-2-glycoprotein-1 IgM: neg | pos 1:160, spotted | GBM Ab: neg Anti-Ro: pos Anti-La: pos Anti-Sm: neg Anti-RNP: neg RF: pos | 2.15 | pos (non-nephrotic range) | pos | 70% crenated RBCs |
| Voong & Patel, 2022 [32] | 58 | F | NR, NR | NR | NR | NR | NR | NR | NR | NR | 11.07 | NR | NR | NR |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bucur, P.; Weber, M.; Agrawal, R.; Madera-Acosta, A.I.; Elam, R.E. Pulmonary-Renal Syndrome from Levamisole-Adulterated Cocaine-Induced Antineutrophil Cytoplasmic Antibody (ANCA)-Associated Vasculitis: A Systematic Review. Pharmaceuticals 2023, 16, 846. https://doi.org/10.3390/ph16060846
Bucur P, Weber M, Agrawal R, Madera-Acosta AI, Elam RE. Pulmonary-Renal Syndrome from Levamisole-Adulterated Cocaine-Induced Antineutrophil Cytoplasmic Antibody (ANCA)-Associated Vasculitis: A Systematic Review. Pharmaceuticals. 2023; 16(6):846. https://doi.org/10.3390/ph16060846
Chicago/Turabian StyleBucur, Philip, Marshall Weber, Rashi Agrawal, Adria Irina Madera-Acosta, and Rachel E. Elam. 2023. "Pulmonary-Renal Syndrome from Levamisole-Adulterated Cocaine-Induced Antineutrophil Cytoplasmic Antibody (ANCA)-Associated Vasculitis: A Systematic Review" Pharmaceuticals 16, no. 6: 846. https://doi.org/10.3390/ph16060846
APA StyleBucur, P., Weber, M., Agrawal, R., Madera-Acosta, A. I., & Elam, R. E. (2023). Pulmonary-Renal Syndrome from Levamisole-Adulterated Cocaine-Induced Antineutrophil Cytoplasmic Antibody (ANCA)-Associated Vasculitis: A Systematic Review. Pharmaceuticals, 16(6), 846. https://doi.org/10.3390/ph16060846






