The Autoinducer N-Octanoyl-L-Homoserine Lactone (C8-HSL) as a Potential Adjuvant in Vaccine Formulations
Abstract
1. Introduction
2. Results
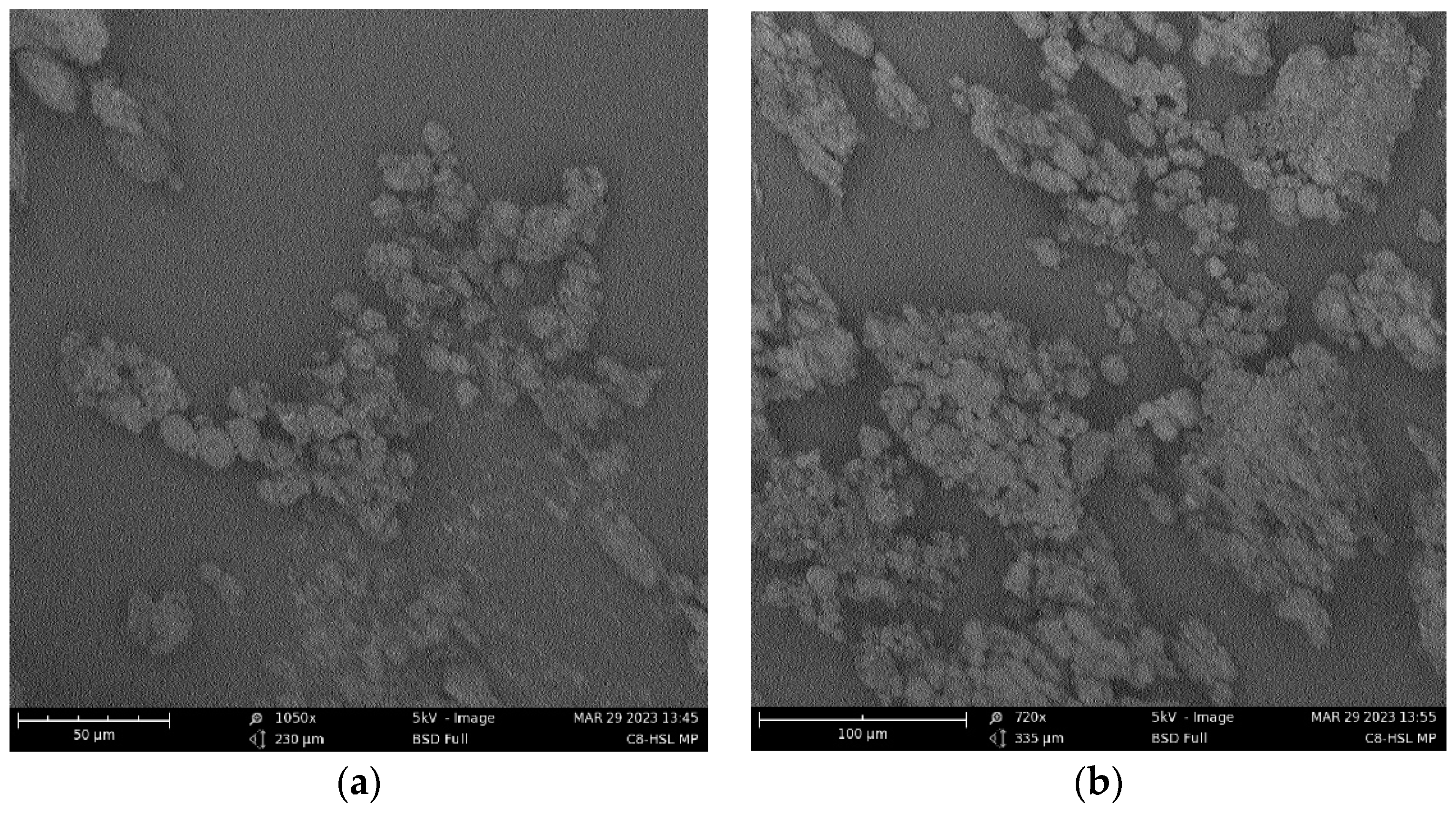
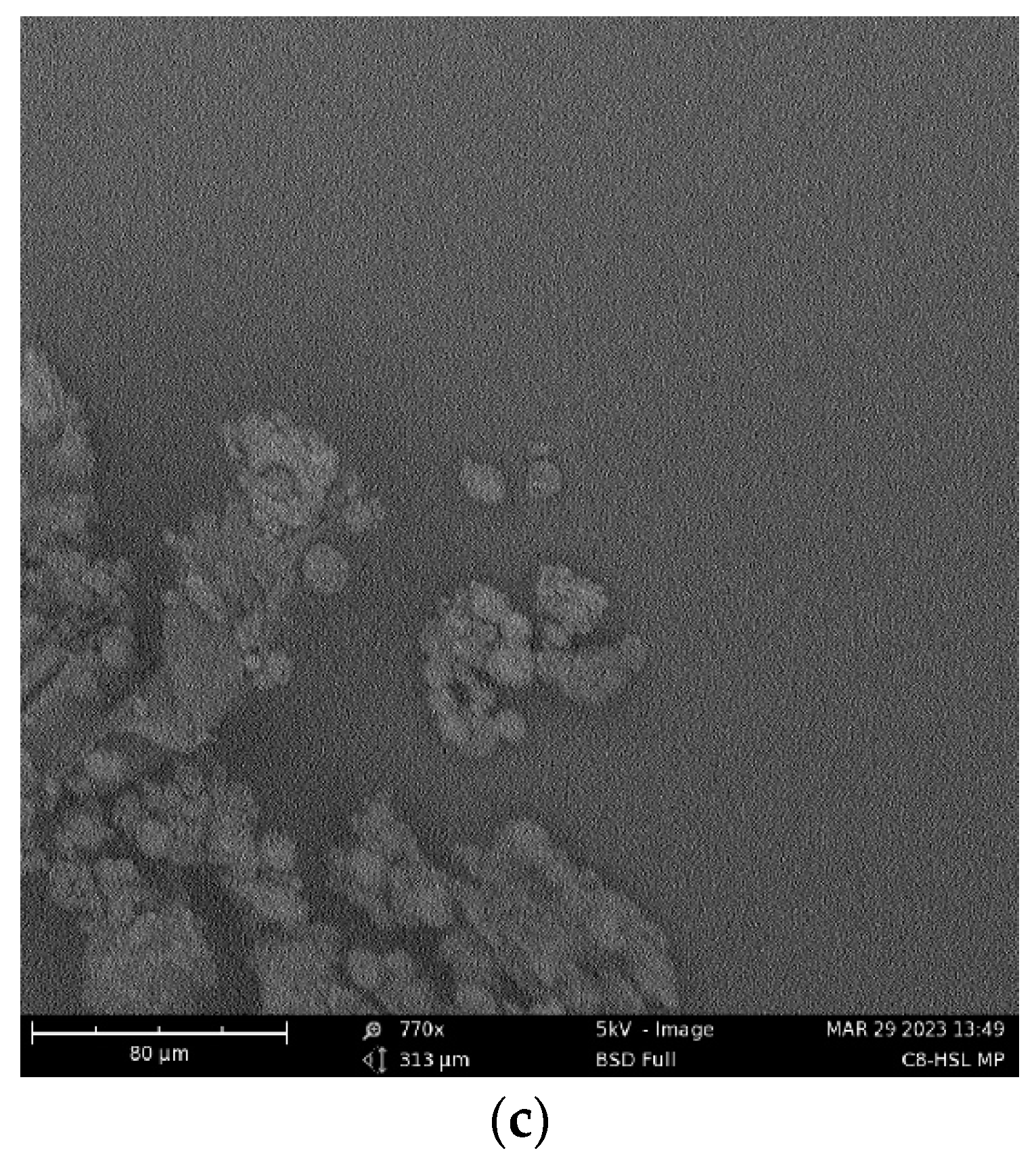
2.1. Characterization of Antigen and Adjuvant Microparticles
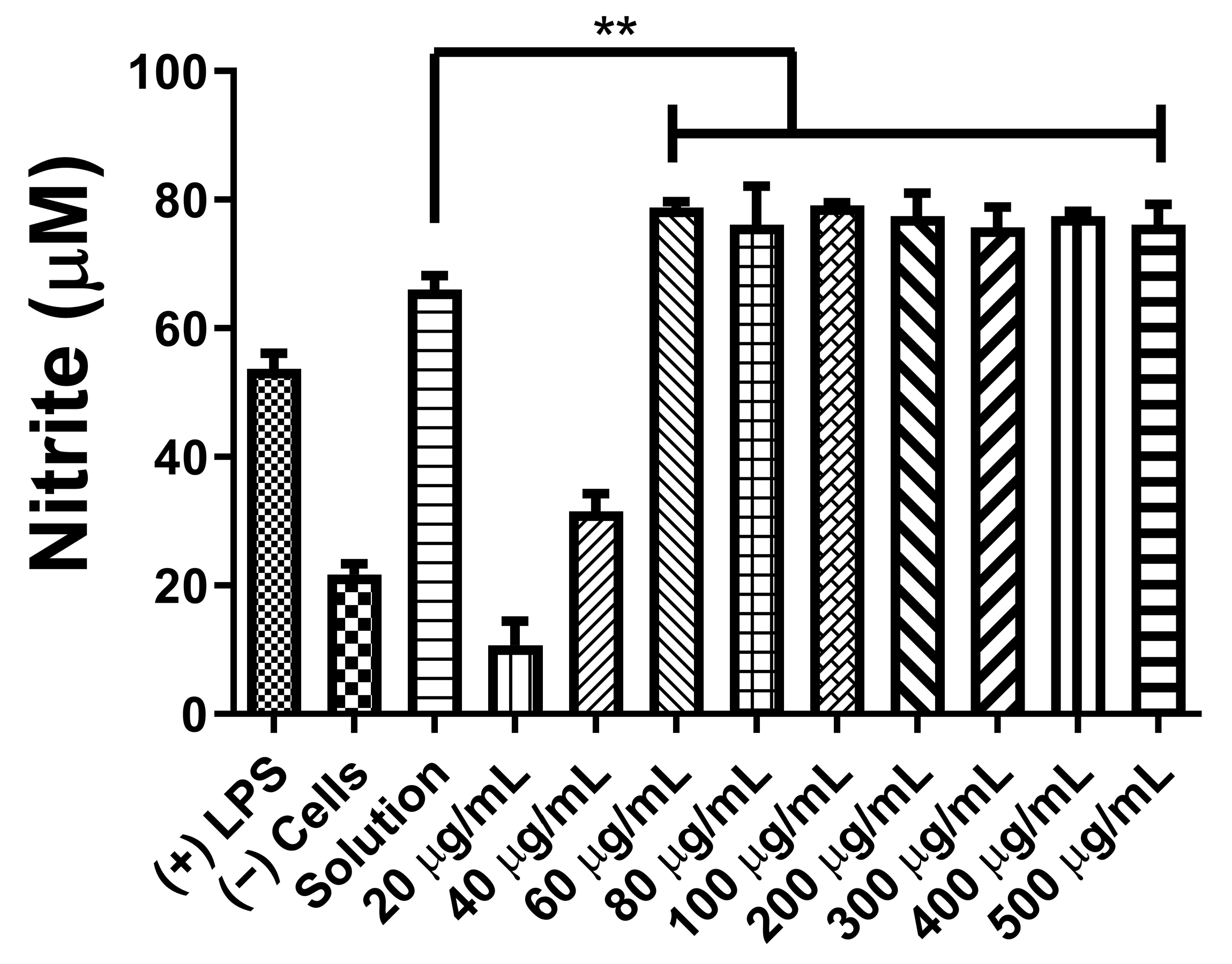
2.2. Autoinducer C8-HSL Microparticulate Concentration Optimization
2.3. Cytotoxicity Profile of C8-HSL MPs
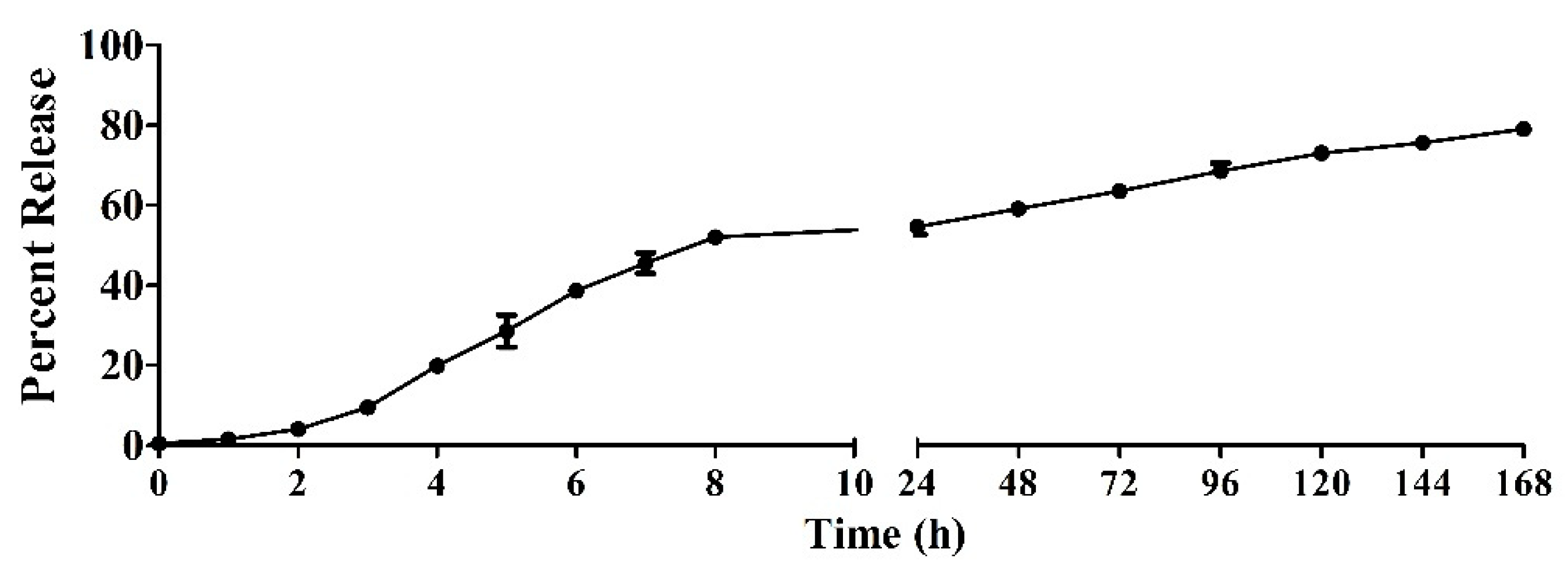
2.4. In Vitro Release Study of C8-HSL
2.5. Evaluation of C8-HSL MP Induction of Autophagosomes
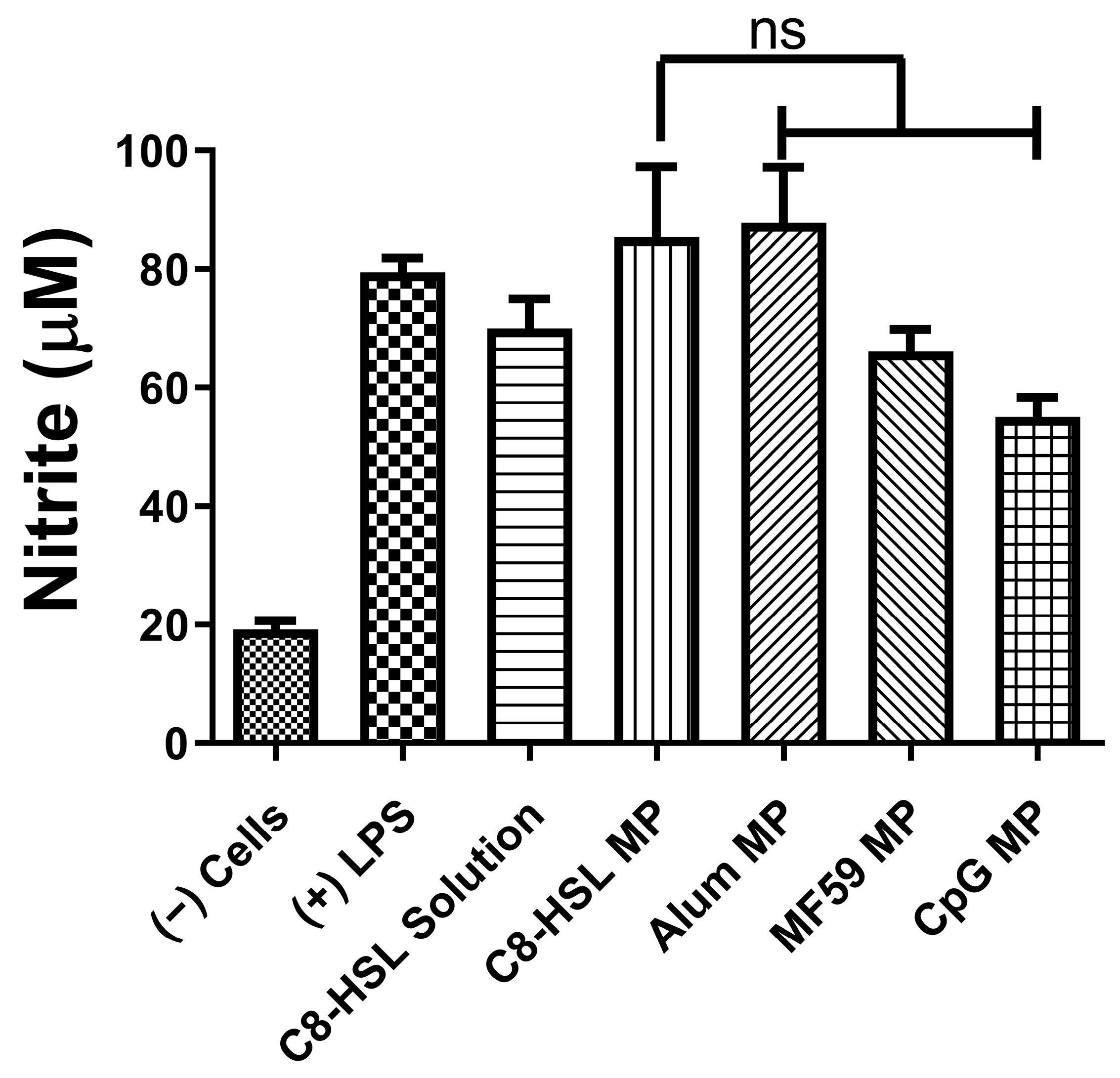
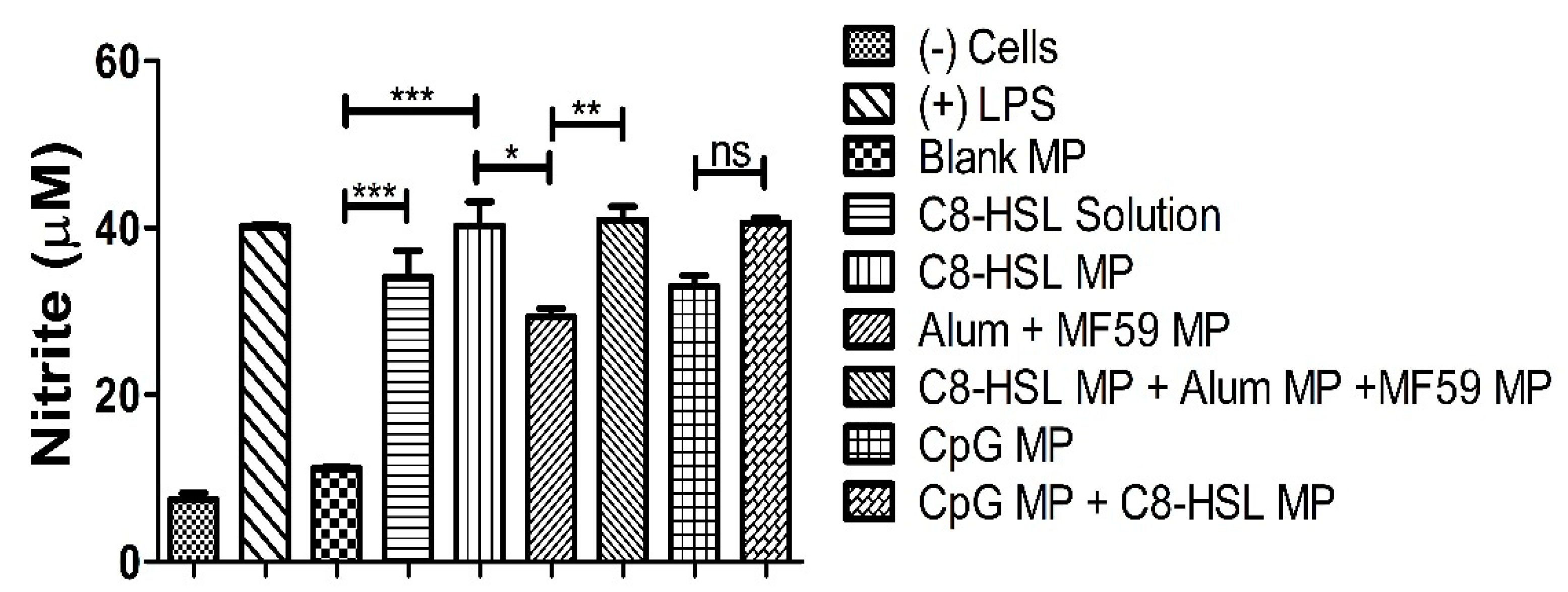
2.6. Immunostimulatory Potential of C8-HSL Microparticles
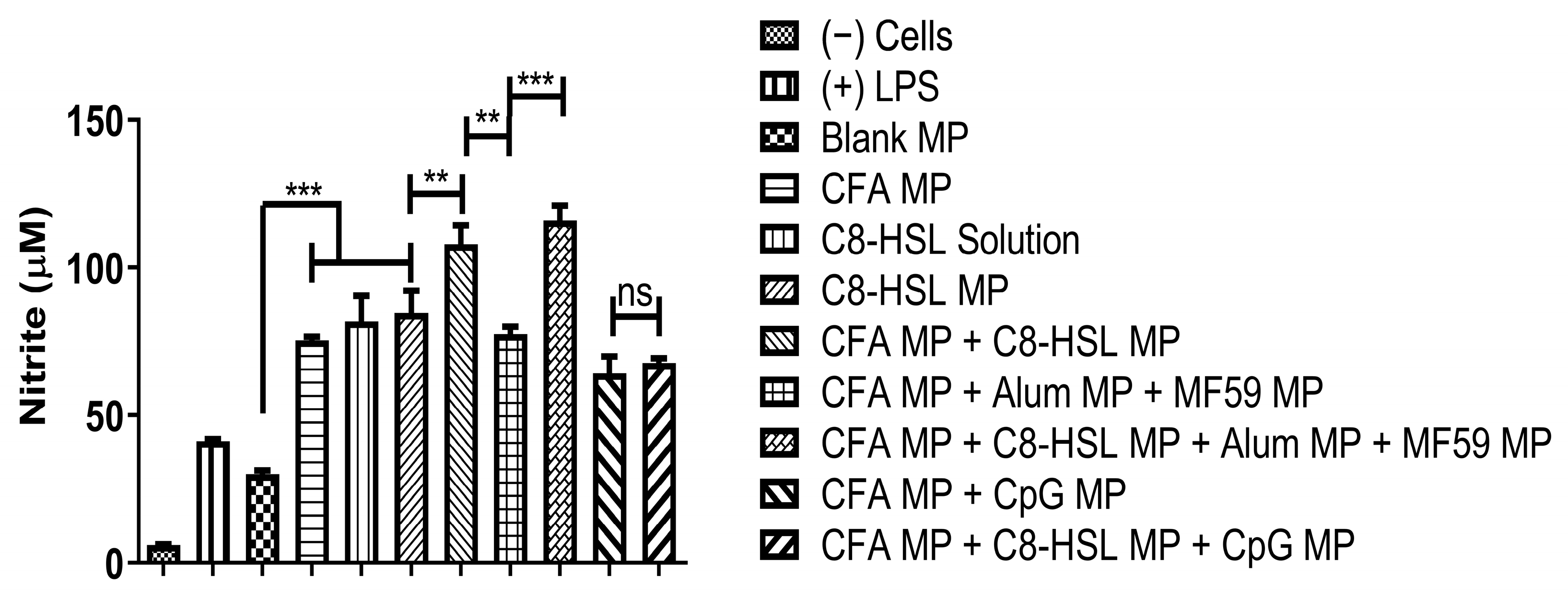
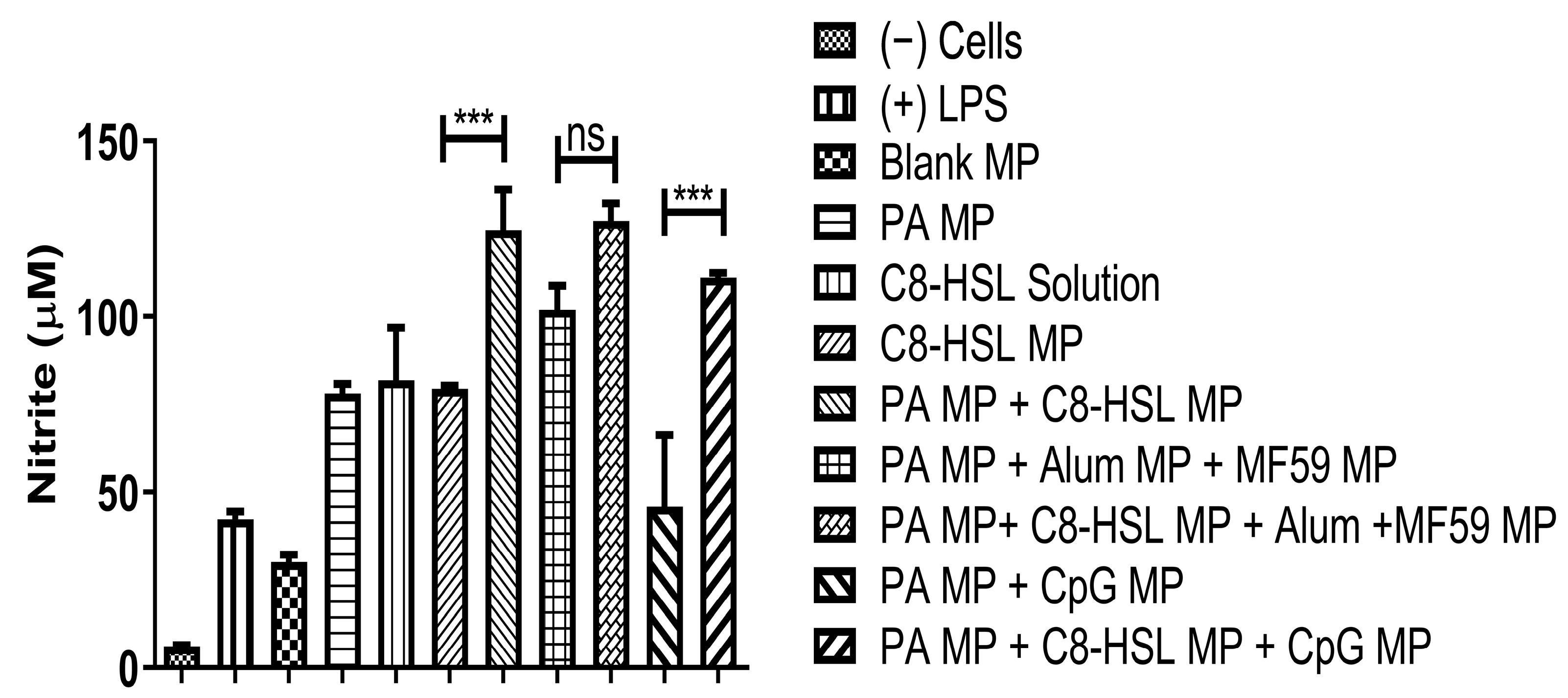
2.7. Evaluation of Adjuvant Effect with Bacterial Antigens: CFA and PA Antigens
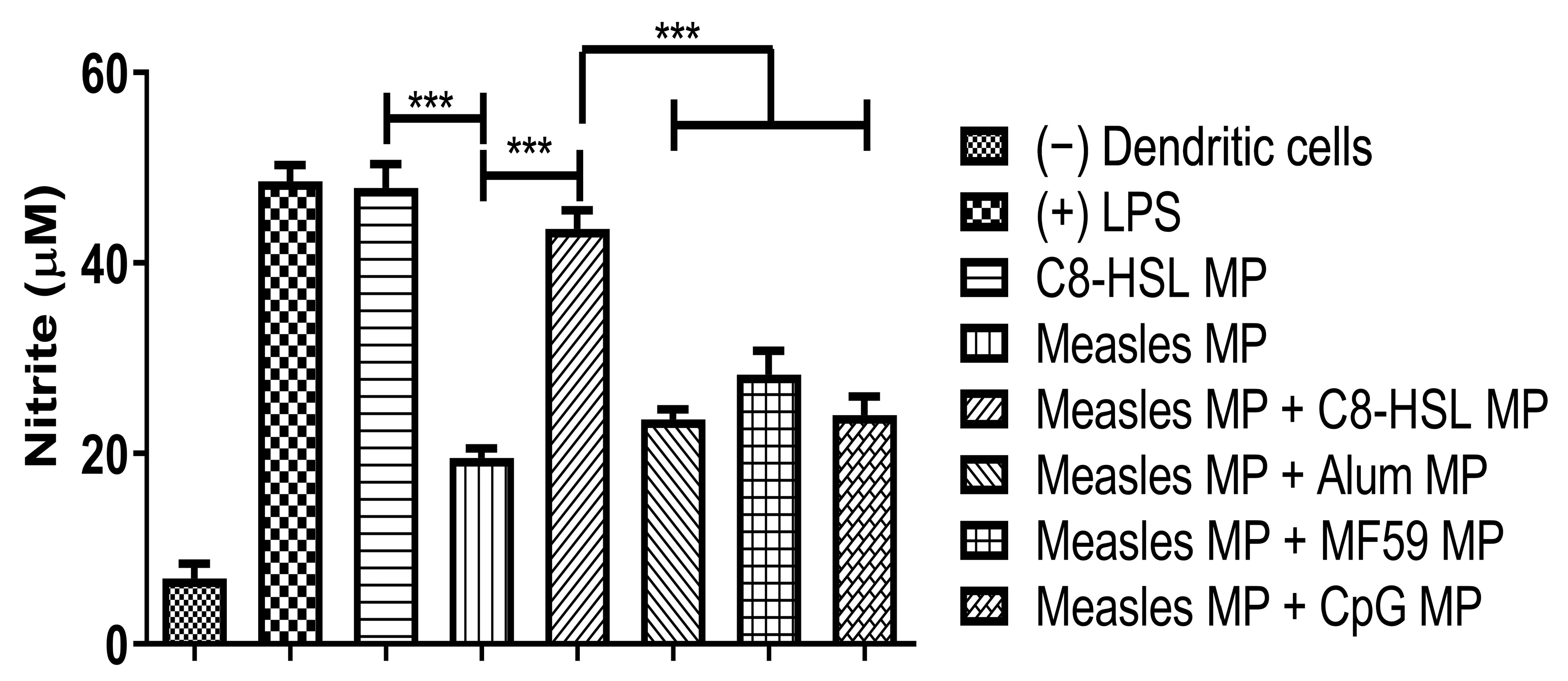
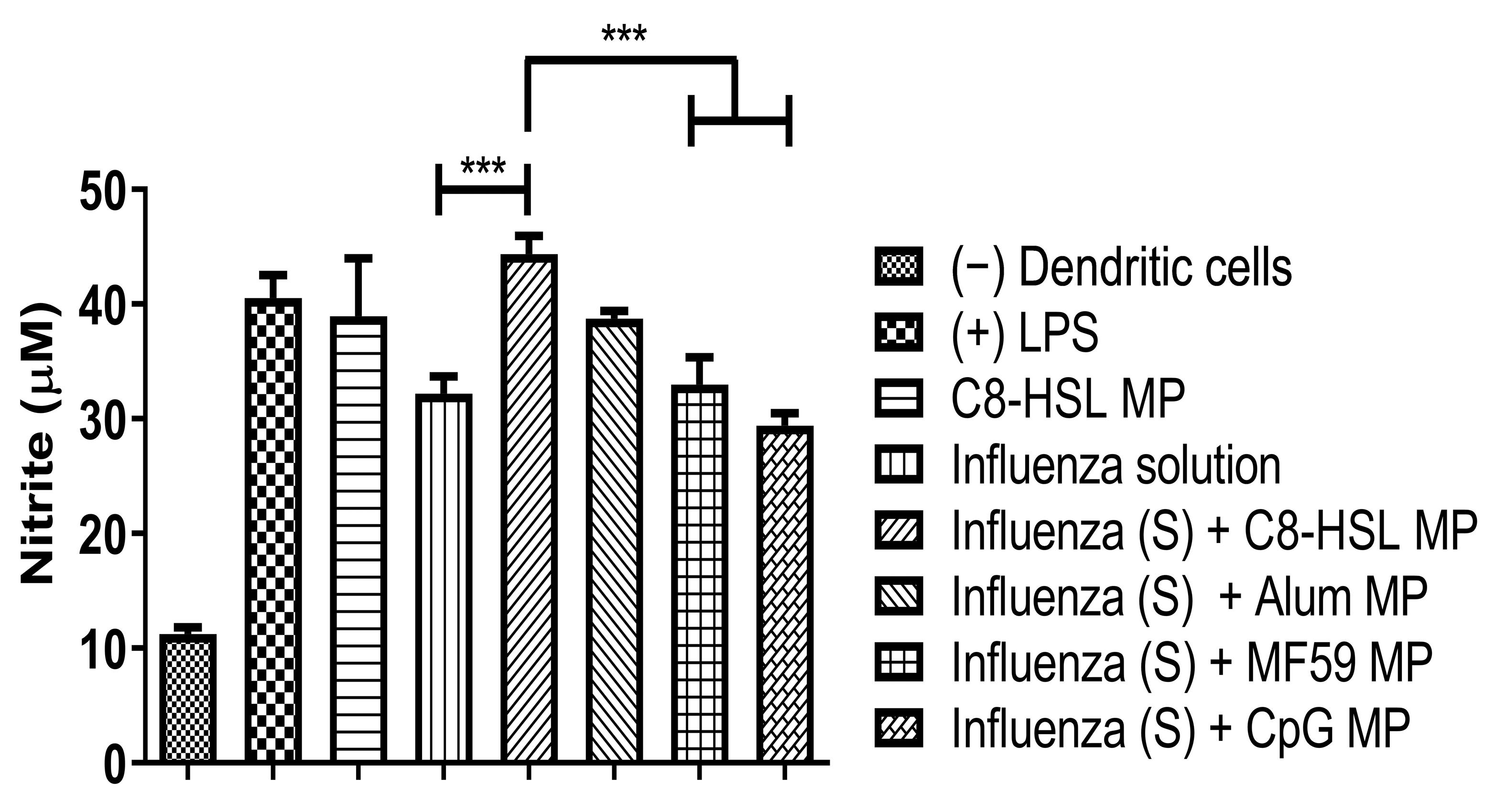
2.8. Evaluation of Adjuvant Effect with Viral Antigens: Zika, Measles, and the Marketed Influenza Vaccine
3. Discussion
4. Materials and Methods
4.1. Materials
4.2. Methods
4.2.1. Formulation of Microparticles
4.2.2. Microparticle Recovery Yield
4.2.3. Particle Size and Zeta Potential Measurement of Microparticles
4.3. Morphology of Microparticles
4.4. Cytotoxicity Assay
4.5. Number of Particles Measurement
4.6. In Vitro Release Study of C8-HSL
4.7. In Vitro Immunogenicity Griess’ Assays for Nitrite
4.8. Evaluation of Adjuvant Effect: Griess’ Assay for Nitrite
4.9. Autophagy
4.10. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Awate, S.; Babiuk, L.A.; Mutwiri, G. Mechanisms of Action of Adjuvants. Front. Immunol. 2013, 4, 114. [Google Scholar] [CrossRef] [PubMed]
- Pulendran, B.; Arunachalam, P.S.; O’Hagan, D.T. Emerging concepts in the science of vaccine adjuvants. Nat. Rev. Drug Discov. 2021, 20, 454–475. [Google Scholar] [CrossRef]
- Nooraei, S.; Lotfabadi, A.S.; Akbarzadehmoallemkolaei, M.; Rezaei, N. Immunogenicity of Different Types of Adjuvants and Nano-Adjuvants in Veterinary Vaccines: A Comprehensive Review. Vaccines 2023, 11, 453. [Google Scholar] [CrossRef] [PubMed]
- Ivanov, K.; Garanina, E.; Rizvanov, A.; Khaiboullina, S. Inflammasomes as Targets for Adjuvants. Pathogens 2020, 9, 252. [Google Scholar] [CrossRef] [PubMed]
- Joshi, D.; Chbib, C.; Uddin, M.N.; D’Souza, M.J. Evaluation of Microparticulate (S)-4,5-Dihydroxy-2,3-pentanedione (DPD) as a Potential Vaccine Adjuvant. AAPS J. 2021, 23, 84. [Google Scholar] [CrossRef] [PubMed]
- Vendeville, A.; Winzer, K.; Heurlier, K.; Tang, C.M.; Hardie, K.R. Making ‘sense’ of metabolism: Autoinducer-2, LUXS and pathogenic bacteria. Nat. Rev. Microbiol. 2005, 3, 383–396. [Google Scholar] [CrossRef]
- Mouriès, J.; Moron, G.; Schlecht, G.; Escriou, N.; Dadaglio, G.; Leclerc, C. Plasmacytoid dendritic cells efficiently cross-prime naive T cells in vivo after TLR activation. Blood 2008, 112, 3713–3722. [Google Scholar] [CrossRef]
- Chbib, C. Impact of the structure-activity relationship of AHL analogues on quorum sensing in Gram-negative bacteria. Bioorg. Med. Chem. 2020, 28, 115282. [Google Scholar] [CrossRef]
- Chbib, C.; Shah, S.M.; Gala, R.P.; Uddin, M.N. Potential Applications of Microparticulate-Based Bacterial Outer Membrane Vesicles (OMVs) Vaccine Platform for Sexually Transmitted Diseases (STDs): Gonorrhea, Chlamydia, and Syphilis. Vaccines 2021, 9, 1245. [Google Scholar] [CrossRef]
- Jazayeri, S.D.; Lim, H.X.; Shameli, K.; Yeap, S.K.; Poh, C.L. Nano and Microparticles as Potential Oral Vaccine Carriers and Adjuvants against Infectious Diseases. Front. Pharmacol. 2021, 12, 682286. [Google Scholar] [CrossRef]
- O’Hagan, D.T.; Jeffery, H.; Roberts, M.J.; McGee, J.P.; Davis, S.S. Controlled release microparticles for vaccine development. Vaccine 1991, 9, 768–771. [Google Scholar] [CrossRef]
- O’Hagan, D.T.; Rahman, D.; McGee, J.P.; Jeffery, H.; Davies, M.C.; Williams, P.; Davis, S.S.; Challacombe, S.J. Biodegradable microparticles as controlled release antigen delivery systems. Immunology 1991, 73, 239–242. [Google Scholar] [PubMed]
- Storni, T.; Kündig, T.M.; Senti, G.; Johansen, P. Immunity in response to particulate antigen-delivery systems. Adv. Drug Deliv. Rev. 2005, 57, 333–355. [Google Scholar] [CrossRef] [PubMed]
- Joshi, D.; Gala, R.P.; Uddin, M.N.; D’Souza, M.J. Novel ablative laser mediated transdermal immunization for microparticulate measles vaccine. Int. J. Pharm. 2021, 606, 120882. [Google Scholar] [CrossRef]
- Sarkar, I.; Garg, R.; van Drunen Littel-van den Hurk, S. Selection of adjuvants for vaccines targeting specific pathogens. Expert. Rev. Vaccines 2019, 18, 505–521. [Google Scholar] [CrossRef]
- He, P.; Zou, Y.; Hu, Z. Advances in aluminum hydroxide-based adjuvant research and its mechanism. Hum. Vaccines Immunother. 2015, 11, 477–488. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guidelines on the Non-Clinical Evaluation of Vaccine Adjuvants and Adjuvanted Vaccines, Annex 2, TRS No 987; World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- Kale, A.; Joshi, D.; Menon, I.; Bagwe, P.; Patil, S.; Vijayanand, S.; Gomes, K.B.; D’Souza, M. Novel microparticulate Zika vaccine induces a significant immune response in a preclinical murine model after intramuscular administration. Int. J. Pharm. 2022, 624, 121975. [Google Scholar] [CrossRef]
- Jones, K.S. Biomaterials as vaccine adjuvants. Biotechnol. Prog. 2008, 24, 807–814. [Google Scholar] [CrossRef]
- Seubert, A.; Monaci, E.; Pizza, M.; O’Hagan, D.T.; Wack, A. The Adjuvants Aluminum Hydroxide and MF59 Induce Monocyte and Granulocyte Chemoattractants and Enhance Monocyte Differentiation toward Dendritic Cells. J. Immunol. 2008, 180, 5402–5412. [Google Scholar] [CrossRef]
- Akalkotkar, A.; Tawde, S.A.; Chablani, L.; D’Souza, M.J. Oral delivery of particulate prostate cancer vaccine: In vitro and in vivo evaluation. J. Drug Target 2012, 20, 338–346. [Google Scholar] [CrossRef]
- Münz, C. Antigen Processing for MHC Class II Presentation via Autophagy. Front. Immunol. 2012, 3, 9. [Google Scholar] [CrossRef]
- Øynebråten, I. Involvement of autophagy in MHC class I antigen presentation. Scand. J. Immunol. 2020, 92, e12978. [Google Scholar] [CrossRef]
- Del Giudice, G.; Rappuoli, R.; Didierlaurent, A.M. Correlates of adjuvanticity: A review on adjuvants in licensed vaccines. Semin. Immunol. 2018, 39, 14–21. [Google Scholar] [CrossRef]
- Abisado, R.G.; Benomar, S.; Klaus, J.R.; Dandekar, A.A.; Chandler, J.R. Bacterial Quorum Sensing and Microbial Community Interactions. mBio 2018, 9, e02331-17. [Google Scholar] [CrossRef] [PubMed]
- Warrier, A.; Satyamoorthy, K.; Murali, T.S. Quorum-sensing regulation of virulence factors in bacterial biofilm. Future Microbiol. 2021, 16, 1003–1021. [Google Scholar] [CrossRef] [PubMed]
- Wusiman, A.; Gu, P.; Liu, Z.; Xu, S.; Zhang, Y.; Hu, Y.; Liu, J.; Wang, D.; Huang, X. Cationic polymer modified PLGA nanoparticles encapsulating Alhagi honey polysaccharides as a vaccine delivery system for ovalbumin to improve immune responses. Int. J. Nanomed. 2019, 4, 3221–3234. [Google Scholar] [CrossRef]
- Oyewumi, M.O.; Kumar, A.; Cui, Z. Nano-microparticles as immune adjuvants: Correlating particle sizes and the resultant immune responses. Expert Rev. Vaccines 2010, 9, 1095–1107. [Google Scholar] [CrossRef] [PubMed]
- Chikaura, H.; Nakashima, Y.; Fujiwara, Y.; Komohara, Y.; Takeya, M.; Nakanishi, Y. Effect of particle size on biological response by human monocyte-derived macrophages. Biosurf. Biotribol. 2016, 2, 18–25. [Google Scholar] [CrossRef]
- Cao, J.; Choi, J.-S.; Oshi, M.A.; Lee, J.; Hasan, N.; Kim, J.; Yoo, J.-W. Development of PLGA micro- and nanorods with high capacity of surface ligand conjugation for enhanced targeted delivery. Asian J. Pharm. Sci. 2019, 14, 86–94. [Google Scholar] [CrossRef]
- Dasgupta, S.; Auth, T.; Gompper, G. Shape and Orientation Matter for the Cellular Uptake of Nonspherical Particles. Nano Lett. 2014, 14, 687–693. [Google Scholar] [CrossRef]
- Barua, S.; Yoo, J.-W.; Kolhar, P.; Wakankar, A.; Gokarn, Y.R.; Mitragotri, S. Particle shape enhances specificity of antibody-displaying nanoparticles. Proc. Natl. Acad. Sci. USA 2013, 110, 3270–3275. [Google Scholar] [CrossRef] [PubMed]
- Dilawar, N.; Ur-Rehman, T.; Shah, K.U.; Fatima, H.; Alhodaib, A. Development and Evaluation of PLGA Nanoparticle-Loaded Organogel for the Transdermal Delivery of Risperidone. Gels 2022, 8, 709. [Google Scholar] [CrossRef] [PubMed]
- Ebensen, T.; Delandre, S.; Prochnow, B.; Guzmán, C.A.; Schulze, K. The Combination Vaccine Adjuvant System Alum/c-di-AMP Results in Quantitative and Qualitative Enhanced Immune Responses Post Immunization. Front. Cell Infect. Microbiol. 2019, 9, 31. [Google Scholar] [CrossRef] [PubMed]
- Krieg, A.M. CpG Oligodeoxynucleotides for Mucosal Vaccines. Mucosal Immunol. 2005, 959–965. [Google Scholar] [CrossRef]
- Vaccine Adjuvants Review|InvivoGen. Available online: https://www.invivogen.com/review-vaccine-adjuvants (accessed on 13 February 2023).
- Germic, N.; Frangez, Z.; Yousefi, S.; Simon, H.-U. Regulation of the innate immune system by autophagy: Monocytes, macrophages, dendritic cells and antigen presentation. Cell Death Differ. 2019, 26, 715–727. [Google Scholar] [CrossRef]
- Bungener, L.; Geeraedts, F.; Veer, W.T.; Medema, J.; Wilschut, J.; Huckriede, A. Alum boosts TH2-type antibody responses to whole-inactivated virus influenza vaccine in mice but does not confer superior protection. Vaccine 2008, 26, 2350–2359. [Google Scholar] [CrossRef]
- Bagwe, P.; Bajaj, L.; Gala, R.P.; D’Souza, M.J.; Zughaier, S.M. Assessment of In Vitro Immunostimulatory Activity of an Adjuvanted Whole-Cell Inactivated Neisseria gonorrhoeae Microparticle Vaccine Formulation. Vaccines 2022, 10, 983. [Google Scholar] [CrossRef]
- Jordan, S.L.P. Inactivation of Glutaraldehyde by Reaction with Sodium Bisulfite. J. Toxicol. Environ. Health 1996, 47, 299–309. [Google Scholar] [CrossRef]




| Parameter | Adjuvant | |||
|---|---|---|---|---|
| C8-HSL MP | Alum MP | MF59® MP | CpG MP | |
| Recovery yield | 74% | 85% | 84% | 85.6% |
| Particle size (μm) | 4.43 ± 0.29 | 2.32 ± 0.42 | 2.58 ± 1.32 | 3.25 ± 0.16 |
| Polydispersity index (PDI) | 0.468 ± 0.345 | 0.576 ± 0.357 | 0.656 ± 0.735 | 0.345 ± 0.1674 |
| Zeta potential (mV) | −32.0 ± 0.92 | −21.1 ± 1.52 | −20.2 ± 2.38 | −28.0 ± 2.45 |
| Parameter | Antigen | |||
| Colonization Factor Antigen (CFA) MP | Protective Antigen (PA) MP | Zika MP | Measles MP | |
| Recovery yield | 68% | 70.2% | 86% | 84% |
| Particle size (μm) | 3.20 ± 0.58 | 3.90 ± 0.38 | 5.71 ± 1.85 | 4.67 ± 0.89 |
| Polydispersity index (PDI) | 0.535 ± 0.176 | 0.389 ± 0.194 | 0.356 ± 0.158 | 0.485 ± 0.102 |
| Zeta potential (mV) | −22.3 ± 1.58 | 22.4 ± 1.84 | –25.1 ± 1.25 | –19.5 ± 1.32 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shah, S.M.; Joshi, D.; Chbib, C.; Roni, M.A.; Uddin, M.N. The Autoinducer N-Octanoyl-L-Homoserine Lactone (C8-HSL) as a Potential Adjuvant in Vaccine Formulations. Pharmaceuticals 2023, 16, 713. https://doi.org/10.3390/ph16050713
Shah SM, Joshi D, Chbib C, Roni MA, Uddin MN. The Autoinducer N-Octanoyl-L-Homoserine Lactone (C8-HSL) as a Potential Adjuvant in Vaccine Formulations. Pharmaceuticals. 2023; 16(5):713. https://doi.org/10.3390/ph16050713
Chicago/Turabian StyleShah, Sarthak M., Devyani Joshi, Christiane Chbib, Monzurul A. Roni, and Mohammad N. Uddin. 2023. "The Autoinducer N-Octanoyl-L-Homoserine Lactone (C8-HSL) as a Potential Adjuvant in Vaccine Formulations" Pharmaceuticals 16, no. 5: 713. https://doi.org/10.3390/ph16050713
APA StyleShah, S. M., Joshi, D., Chbib, C., Roni, M. A., & Uddin, M. N. (2023). The Autoinducer N-Octanoyl-L-Homoserine Lactone (C8-HSL) as a Potential Adjuvant in Vaccine Formulations. Pharmaceuticals, 16(5), 713. https://doi.org/10.3390/ph16050713









