Beta Blockers Improve Prognosis When Used Early in Patients with Cardiogenic Shock: An Analysis of the FRENSHOCK Multicenter Prospective Registry
Abstract
:1. Introduction
2. Results
2.1. Baseline Characteristics and CS Management According to the Intake of Betablockers at 24 h
2.2. Betablockers Non-Discontinuation at 24 h
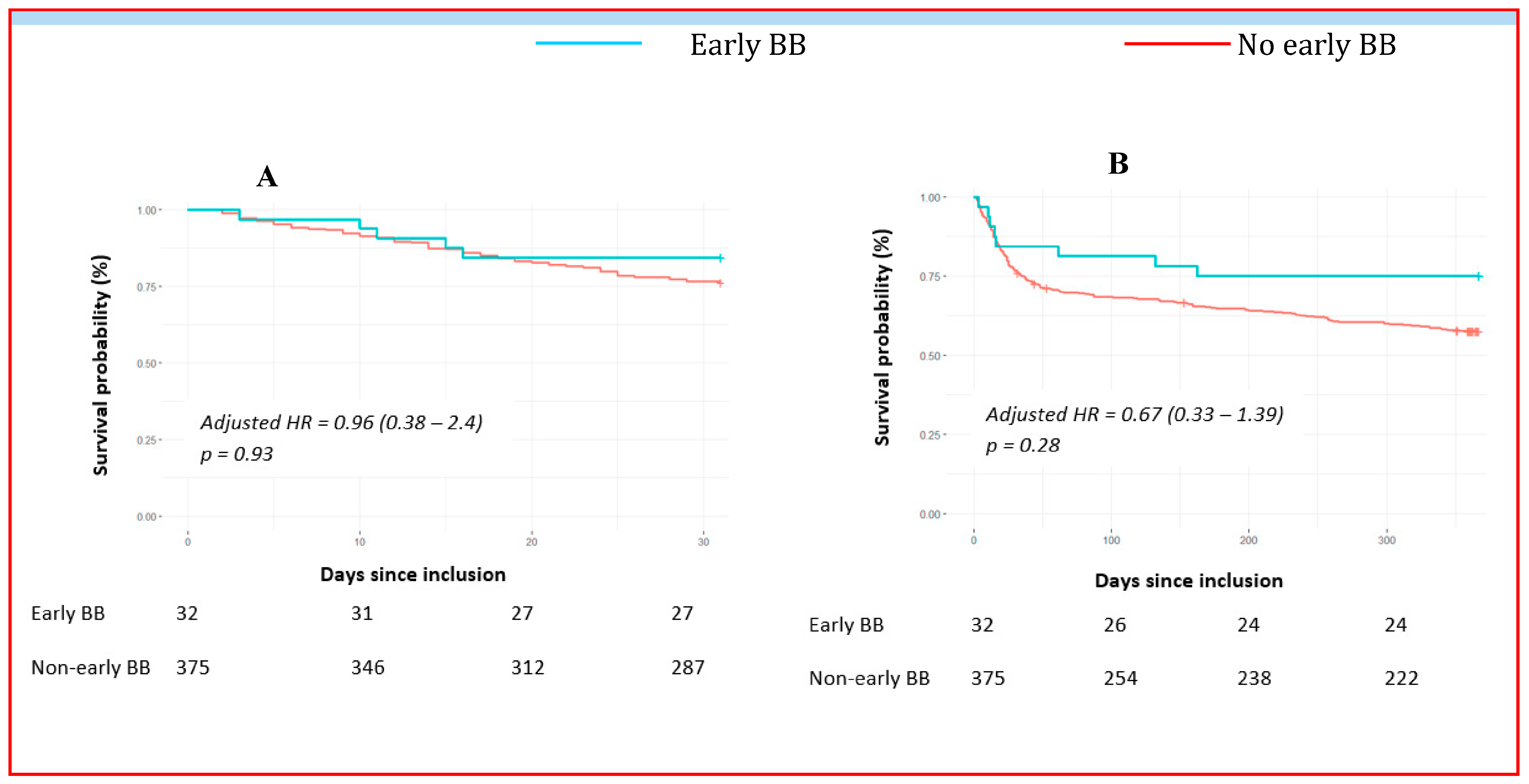
2.3. Early Betablocker Introduction (<24 h)
3. Discussion
Strengths and Limitations
4. Materials and Methods
4.1. Patient Population and Data Collection
4.2. Study Endpoints and Follow-Up
4.3. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mebazaa, A.; Davison, B.; Chioncel, O.; Cohen-Solal, A.; Diaz, R.; Filippatos, G.; Metra, M.; Ponikowski, P.; Sliwa, K.; Voors, A.A.; et al. Safety, tolerability and efficacy of up-titration of guideline-directed medical therapies for acute heart failure (STRONG-HF): A multinational, open-label, randomised, trial. Lancet 2022, 400, 1938–1952. [Google Scholar] [CrossRef] [PubMed]
- Bristow, M.R. β-Adrenergic Receptor Blockade in Chronic Heart Failure. Circulation 2000, 101, 558–569. [Google Scholar] [CrossRef] [PubMed]
- Tamaki, Y.; Yaku, H.; Morimoto, T.; Inuzuka, Y.; Ozasa, N.; Yamamoto, E.; Yoshikawa, Y.; Miyake, M.; Kondo, H.; Tamura, T.; et al. Lower In-Hospital Mortality with Beta-Blocker Use at Admission in Patients with Acute Decompensated Heart Failure. J. Am. Heart Assoc. 2021, 10, e020012. [Google Scholar] [CrossRef]
- Chatterjee, S.; Chaudhuri, D.; Vedanthan, R.; Fuster, V.; Ibanez, B.; Bangalore, S.; Mukherjee, D. Early intravenous beta-blockers in patients with acute coronary syndrome—A meta-analysis of randomized trials. Int. J. Cardiol. 2013, 168, 915–921. [Google Scholar] [CrossRef] [PubMed]
- Lacoursiere, L.; Woodruff, A.E.; Mills, K.; Chilbert, M.R. A Retrospective Review of Cardiogenic Shock Development in Patients with ST-Elevation Myocardial Infarction and Percutaneous Coronary Intervention Receiving Early Beta-Blockers. J. Cardiovasc. Pharmacol. 2023, 81, 355–360. [Google Scholar] [CrossRef] [PubMed]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef] [PubMed]
- Jondeau, G.; Neuder, Y.; Eicher, J.-C.; Jourdain, P.; Fauveau, E.; Galinier, M.; Jegou, A.; Bauer, F.; Trochu, J.N.; Bouzamondo, A.; et al. B-CONVINCED: Beta-blocker CONtinuation Vs. INterruption in patients with Congestive heart failure hospitalizED for a decompensation episode. Eur. Heart J. 2009, 30, 2186–2192. [Google Scholar] [CrossRef]
- O’Connor, C.M.; Abraham, W.T.; Albert, N.M.; Clare, R.; Stough, W.G.; Gheorghiade, M.; Greenberg, B.H.; Yancy, C.W.; Young, J.B.; Fonarow, G.C. Predictors of mortality after discharge in patients hospitalized with heart failure: An analysis from the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF). Am. Heart J. 2008, 156, 662–673. [Google Scholar] [CrossRef]
- Gattis, W.A.; O’Connor, C.M. Predischarge initiation of carvedilol in patients hospitalized for decompensated heart failure. Am. J. Cardiol. 2004, 93, 74–76. [Google Scholar] [CrossRef]
- Thiele, H.; Ohman, E.M.; Desch, S.; Eitel, I.; de Waha, S. Management of cardiogenic shock. Eur. Heart J. 2015, 36, 1223–1230. [Google Scholar] [CrossRef]
- Prins, K.W.; Neill, J.M.; Tyler, J.O.; Eckman, P.M.; Duval, S. Effects of Beta-Blocker Withdrawal in Acute Decompensated Heart Failure. JACC Heart Fail. 2015, 3, 647–653. [Google Scholar] [CrossRef] [PubMed]
- Puymirat, E.; Fagon, J.Y.; Aegerter, P.; Diehl, J.L.; Monnier, A.; Hauw-Berlemont, C.; Boissier, F.; Chatellier, G.; Guidet, B.; Danchin, N.; et al. Cardiogenic shock in intensive care units: Evolution of prevalence, patient profile, management and outcomes, 1997–2012. Eur. J. Heart Fail. 2017, 19, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Butler, J.; Young, J.B.; Abraham, W.T.; Bourge, R.C.; Adams, K.F.; Clare, R.; O’connor, C. Beta-Blocker Use and Outcomes among Hospitalized Heart Failure Patients. J. Am. Coll. Cardiol. 2006, 47, 2462–2469. [Google Scholar] [CrossRef] [PubMed]
- Felker, G.; Benza, R.L.; Chandler, A.; Leimberger, J.D.; Cuffe, M.S.; Califf, R.M.; Gheorghiade, M.; O’connor, C.M. Heart failure etiology and response tomilrinone in decompensated heart failure. J. Am. Coll. Cardiol. 2003, 41, 997–1003. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, A.F.; Hammill, B.G.; O’Connor, C.M.; Schulman, K.A.; Curtis, L.H.; Fonarow, G.C. Clinical Effectiveness of Beta-Blockers in Heart Failure. J. Am. Coll. Cardiol. 2009, 53, 184–192. [Google Scholar] [CrossRef]
- Fonarow, G.C.; Abraham, W.T.; Albert, N.M.; Stough, W.G.; Gheorghiade, M.; Greenberg, B.H.; O’Connor, C.M.; Sun, J.L.; Yancy, C.W.; Young, J.B. Influence of Beta-Blocker Continuation or Withdrawal on Outcomes in Patients Hospitalized with Heart Failure. J. Am. Coll. Cardiol. 2008, 52, 190–199. [Google Scholar] [CrossRef]
- Farmakis, D.; Parissis, J.; Karavidas, A.; Karvounis, C.; Triposkiadis, F.; Filippatos, G.; Lekakis, J.; Barbetseas, J.; Giannadaki, M.; Kakouros, S.; et al. In-hospital management of acute heart failure: Practical recommendations and future perspectives. Int. J. Cardiol. 2015, 201, 231–236. [Google Scholar] [CrossRef]
- Mebazaa, A.; Yilmaz, M.B.; Levy, P.; Ponikowski, P.; Peacock, W.F.; Laribi, S.; Ristic, A.D.; Lambrinou, E.; Masip, J.; Riley, J.P.; et al. Recommendations on pre-hospital & early hospital management of acute heart failure: A consensus paper from the Heart Failure Association of the European Society of Cardiology, the European Society of Emergency Medicine and the Society of Academic Emergenc. Eur. J. Heart Fail. 2015, 17, 544–558. [Google Scholar] [CrossRef]
- Metra, M.; Torp-Pedersen, C.; Cleland, J.G.; Di Lenarda, A.; Komajda, M.; Remme, W.J.; Cas, L.D.; Spark, P.; Swedberg, K.; Poole-Wilson, P.A.; et al. Should beta-blocker therapy be reduced or withdrawn after an episode of decompensated heart failure? Results from COMET. Eur. J. Heart Fail. 2007, 9, 901–909. [Google Scholar] [CrossRef]
- Di Santo, P.; Mathew, R.; Jung, R.G.; Simard, T.; Skanes, S.; Mao, B.; Ramirez, F.D.; Marbach, J.A.; Abdel-Razek, O.; Motazedian, P.; et al. Impact of baseline beta-blocker use on inotrope response and clinical outcomes in cardiogenic shock: A subgroup analysis of the DOREMI trial. Crit. Care 2021, 25, 289. [Google Scholar] [CrossRef]
- Mert, K.U.; Mert, G.Ö.; Morrad, B.; Tahmazov, S.; Mutlu, F.; Çavuşoglu, Y. Effects of ivabradine and beta-blocker therapy on dobutamine-induced ventricular arrhythmias. Kardiol. Pol. 2017, 75, 786–793. [Google Scholar] [CrossRef] [PubMed]
- Böhm, M.; Link, A.; Cai, D.; Nieminen, M.S.; Filippatos, G.S.; Salem, R.; Solal, A.C.; Huang, B.; Padley, R.J.; Kivikko, M.; et al. Beneficial association of β-blocker therapy on recovery from severe acute heart failure treatment: Data from the Survival of Patients with Acute Heart Failure in Need of Intravenous Inotropic Support trial*. Crit. Care Med. 2011, 39, 940–944. [Google Scholar] [CrossRef] [PubMed]
- Delmas, C.; Orloff, E.; Bouisset, F.; Moine, T.; Citoni, B.; Biendel, C.; Porterie, J.; Carrié, D.; Galinier, M.; Elbaz, M.; et al. Predictive factors for long-term mortality in miscellaneous cardiogenic shock: Protective role of beta-blockers at admission. Arch. Cardiovasc. Dis. 2019, 112, 738–747. [Google Scholar] [CrossRef] [PubMed]
- Gattis, W.A.; O’Connor, C.M.; Leimberger, J.D.; Felker, G.M.; Adams, K.F.; Gheorghiade, M. Clinical outcomes in patients on beta-blocker therapy admitted with worsening chronic heart failure. Am. J. Cardiol. 2003, 91, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Koracevic, G.; Micic, S.; Stojanovic, M.; Tomasevic, M.; Kostic, T.; Radovanovic, R.V.; Lovic, D.; Djordjevic, D.; Randjelovic, M.; Koracevic, M.; et al. Beta blocker rebound phenomenon is important, but we do not know its definition, incidence or optimal prevention strategies. Hypertens. Res. 2020, 43, 591–596. [Google Scholar] [CrossRef] [PubMed]
- Gorre, F.; Vandekerckhove, H. Beta-blockers: Focus on mechanism of action Which beta-blocker, when and why? Acta Cardiol. 2010, 65, 565–570. [Google Scholar] [CrossRef] [PubMed]
- Ross, P.J.; Lewis, M.J.; Sheridan, D.J.; Henderson, A.H. Adrenergic hypersensitivity after beta-blocker withdrawal. Heart 1981, 45, 637–642. [Google Scholar] [CrossRef]
- Levy, B.; Clere-Jehl, R.; Legras, A.; Morichau-Beauchant, T.; Leone, M.; Frederique, G.; Quenot, J.-P.; Kimmoun, A.; Cariou, A.; Lassus, J.; et al. Epinephrine Versus Norepinephrine for Cardiogenic Shock After Acute Myocardial Infarction. J. Am. Coll. Cardiol. 2018, 72, 173–182. [Google Scholar] [CrossRef]
- Naidu, S.S.; Baran, D.A.; Jentzer, J.C.; Hollenberg, S.M.; van Diepen, S.; Basir, M.B.; Grines, C.L.; Diercks, D.B.; Hall, S.; Kapur, N.K.; et al. SCAI SHOCK Stage Classification Expert Consensus Update: A Review and Incorporation of Validation Studies. J. Am. Coll. Cardiol. 2022, 79, 933–946. [Google Scholar] [CrossRef]
- Delmas, C.; Puymirat, E.; Leurent, G.; Elbaz, M.; Manzo-Silberman, S.; Bonello, L.; Gerbaud, E.; Bataille, V.; Levy, B.; Lamblin, N.; et al. Design and preliminary results of FRENSHOCK 2016: A prospective nationwide multicentre registry on cardiogenic shock. Arch. Cardiovasc. Dis. 2019, 112, 343–353. [Google Scholar] [CrossRef]
- Delmas, C.; Roubille, F.; Lamblin, N.; Bonello, L.; Leurent, G.; Levy, B.; Elbaz, M.; Danchin, N.; Champion, S.; Lim, P.; et al. Baseline characteristics, management, and predictors of early mortality in cardiogenic shock: Insights from the FRENSHOCK registry. ESC Heart Fail. 2022, 9, 408–419. [Google Scholar] [CrossRef] [PubMed]



| Overall Population (n = 693) | BB Group (n = 95) | Non-BB Group (n = 598) | p Value | |
|---|---|---|---|---|
| Age, mean ± SD, years | 66 ± 14.6 | 68.3 ± 15.1 | 65.7 ± 14.5 | 0.07 |
| Male, n (%) | 495 (71.4) | 53 (55.8) | 442 (73.9) | <0.01 |
| Body mass index, mean ± SD, kg/m² | 25.7 ± 5.5 | 26.5 ± 6.5 | 25.6 ± 5.3 | 0.44 |
| Risk factors, n (%) | ||||
| Diabetes mellitus | 195 (28.2) | 36 (37.9) | 159 (26.6) | 0.03 |
| Hypertension | 329 (47.5) | 57 (60) | 272 (45.5) | 0.01 |
| Dyslipidemia | 254 (36.7) | 40 (42.1) | 214 (35.8) | 0.25 |
| Current smoker | 183 (27.4) | 28 (30.1) | 155 (27) | 0.53 |
| Medical history, n (%) | ||||
| Peripheral artery disease | 84 (12.1) | 13 (13.7) | 71 (11.9) | 0.61 |
| Chronic kidney disease | 151 (21.8) | 21 (22.1) | 130 (21.8) | 1 |
| COPD | 44 (6.4) | 6 (6.3) | 38 (6.4) | 1 |
| ICD | 111 (16) | 18 (18.9) | 93 (15.6) | 0.45 |
| Active cancer | 47 (6.8) | 3 (3.2) | 44 (7.4) | 0.18 |
| Stroke | 54 (7.8) | 10 (10.5) | 44 (7.4) | 0.3 |
| NYHA functional status, n (%) | ||||
| ≥3 | 265 (39.2) | 34 (37) | 231 (39.6) | 0.76 |
| History of cardiac disease, n (%) | ||||
| All causes | 392 (56.6) | 57 (60) | 335 (56) | 0.5 |
| Ischemic | 205 (29.6) | 35 (36.8) | 170 (28.4) | 0.12 |
| Hypertrophic | 11 (1.6) | 2 (2.1) | 9 (1.5) | 0.65 |
| Toxic | 29 (4.2) | 4 (4.2) | 25 (4.2) | 1 |
| Dilated | 72 (10.4) | 9 (9.5) | 63 (10.5) | 0.86 |
| Valvular | 58 (8.4) | 5 (5.3) | 53 (8.9) | 0.32 |
| Hypertensive | 22 (3.2) | 2 (2.1) | 20 (3.3) | 0.76 |
| Previous medications, n (%) | ||||
| Aspirin | 255 (36.8) | 33 (34.7) | 222 (37.1) | 0.73 |
| P2Y12 inhibitors | 120 (17.3) | 12 (12.6) | 108 (18.1) | 0.24 |
| Oral anticoagulant (VKA or DOAC) | 201 (29) | 39 (41.1) | 162 (27.1) | < 0.01 |
| ACEi, ARB or ARNi | 271 (40.2) | 46 (48.9) | 225 (38.8) | 0.07 |
| Statins | 256 (36.9) | 37 (38.9) | 219 (36.6) | 0.73 |
| Loop diuretics | 340 (49.1) | 56 (58.9) | 284 (47.5) | 0.046 |
| Aldosterone antagonist | 100 (14.4) | 9 (9.5) | 91 (15.2) | 0.16 |
| Cardiogenic shock triggers, n (%) | ||||
| Ischemic | 254 (36.7) | 42 (44.2) | 212 (35.5) | 0.11 |
| Non-ischemic | 365 (52.7) | 44 (46.3) | 321 (53.7) | |
| Supraventricular tachycardia | 96 (13.9) | 13 (13.7) | 83 (13.9) | 1 |
| Infectious disease | 80 (11.5) | 8 (8.4) | 72 (12) | 0.39 |
| Ventricular arrhythmia | 86 (12.4) | 15 (15.8) | 71 (11.9) | 0.31 |
| Iatrogenesis | 41 (5.9) | 3 (3.2) | 38 (6.4) | 0.35 |
| Non-observance | 27 (3.9) | 3 (3.2) | 24 (4) | 1 |
| Mechanical complications | 21 (3) | 2 (2.1) | 19 (3.2) | 0.76 |
| Conduction disorder | 14 (2) | 0 (0) | 14 (2.3) | 0.24 |
| Clinical presentation at admission | ||||
| Heart rate, mean ± SD, bpm | 95.4 ± 29.7 | 100.9 ± 35.9 | 94.6 ± 28.6 | 0.33 |
| SBP, mean ± SD, mmHg | 102 ± 25.1 | 108.2 ± 20.9 | 101.1 ± 25.6 | <0.01 |
| Sinus rhythm, n (%) | 355 (51.4) | 35 (36.8) | 320 (53.8) | <0.01 |
| Cardiac arrest, n (%) | 66 (9.5) | 11 (11.6) | 55 (9.2) | 0.45 |
| Blood tests at admission, median (IQR) | ||||
| Sodium, mmol/L | 135 (132–139) | 137 (133.5–140) | 135 (131–139) | 0.03 |
| Creatinin, μmol/L | 132.5 (94–188) | 116 (83.5–152) | 134 (97–194) | 0.01 |
| Bilirubin, mg/L | 16 (9.5–28) | 18 (10–30) | 16 (9.1–28) | 0.51 |
| Haemoglobin, g/dL | 12.7 (11–14) | 12 (10.6–13.6) | 13 (11–14) | 0.049 |
| Arterial blood lactates, mmol/L | 3.0 (2.0–4.2) | 2.2 (1.9–3.0) | 3.0 (2.0–5.0) | <0.01 |
| ASAT, UI/L | 87 (38.3–292.5) | 51 (36–180) | 91 (39–301) | 0.08 |
| Nt-proBNP, pg/mL | 10,293.5 (4442.5–26,322.5) | 5922 (4846–13,701) | 10,626 (4389–27,884) | 0.23 |
| Baseline echocardiography | ||||
| LVEF, mean ± SD, % | 26.7 ± 13.3 | 29.9 ± 13 | 26.1 ± 13.3 | <0.01 |
| TAPSE, median (IQR), mm | 13 (10–17) | 13 (10–16) | 13 (10–17) | 0.85 |
| PSVtdi, median (IQR), cm/s | 8 (6–10) | 8 (7–10.3) | 8 (6–10) | 0.77 |
| Severe mitral regurgitation, n (%) | 96 (14.6) | 8 (8.6) | 88 (15.5) | 0.08 |
| Severe aortic stenosis, n (%) | 31 (4.5) | 4 (4.3) | 27 (4.6) | 1 |
| Severe aortic regurgitation, n (%) | 9 (1.3) | 1 (1.1) | 8 (1.4) | 1 |
| Overall Population (n = 693) | BB Group (n = 95) | Non-BB Group (n = 598) | p Value | |
|---|---|---|---|---|
| Medications used, n (%) | ||||
| Dobutamine | 566 (81.8) | 59 (62.1) | 507 (84.9) | <0.01 |
| Norepinephrine | 361 (52.2) | 25 (26.3) | 336 (56.3) | <0.01 |
| Epinephrine | 87 (12.6) | 10 (10.5) | 77 (12.9) | 0.62 |
| Levosimendan | 50 (7.2) | 4 (4.2) | 46 (7.7) | 0.29 |
| Loop diuretics | 467 (67.4) | 73 (76.8) | 394 (65.9) | 0.03 |
| Respiratory support, n (%) | ||||
| Non-invasive | 184 (26.6) | 43 (45.7) | 141 (23.6) | <0.01 |
| Invasive | 249 (36) | 15 (15.8) | 234 (39.2) | <0.01 |
| Short-term mechanical circulatory support, n (%) | 121 (17.5) | 9 (9.5) | 112 (18.8) | 0.03 |
| Renal replacement therapy, n (%) | 107 (15.4) | 7 (7.4) | 100 (16.7) | 0.02 |
| Any PCI, n (%) | 206 (70.8) | 27 (75) | 179 (0.2) | 0.7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cardelli, L.S.; Cherbi, M.; Huet, F.; Schurtz, G.; Bonnefoy-Cudraz, E.; Gerbaud, E.; Bonello, L.; Leurent, G.; Puymirat, E.; Casella, G.; et al. Beta Blockers Improve Prognosis When Used Early in Patients with Cardiogenic Shock: An Analysis of the FRENSHOCK Multicenter Prospective Registry. Pharmaceuticals 2023, 16, 1740. https://doi.org/10.3390/ph16121740
Cardelli LS, Cherbi M, Huet F, Schurtz G, Bonnefoy-Cudraz E, Gerbaud E, Bonello L, Leurent G, Puymirat E, Casella G, et al. Beta Blockers Improve Prognosis When Used Early in Patients with Cardiogenic Shock: An Analysis of the FRENSHOCK Multicenter Prospective Registry. Pharmaceuticals. 2023; 16(12):1740. https://doi.org/10.3390/ph16121740
Chicago/Turabian StyleCardelli, Laura Sofia, Miloud Cherbi, Fabien Huet, Guillaume Schurtz, Eric Bonnefoy-Cudraz, Edouard Gerbaud, Laurent Bonello, Guillaume Leurent, Etienne Puymirat, Gianni Casella, and et al. 2023. "Beta Blockers Improve Prognosis When Used Early in Patients with Cardiogenic Shock: An Analysis of the FRENSHOCK Multicenter Prospective Registry" Pharmaceuticals 16, no. 12: 1740. https://doi.org/10.3390/ph16121740
APA StyleCardelli, L. S., Cherbi, M., Huet, F., Schurtz, G., Bonnefoy-Cudraz, E., Gerbaud, E., Bonello, L., Leurent, G., Puymirat, E., Casella, G., Delmas, C., & Roubille, F. (2023). Beta Blockers Improve Prognosis When Used Early in Patients with Cardiogenic Shock: An Analysis of the FRENSHOCK Multicenter Prospective Registry. Pharmaceuticals, 16(12), 1740. https://doi.org/10.3390/ph16121740






