Gut Microbiota and Endometriosis: Exploring the Relationship and Therapeutic Implications
Abstract
:1. Introduction
2. Methods
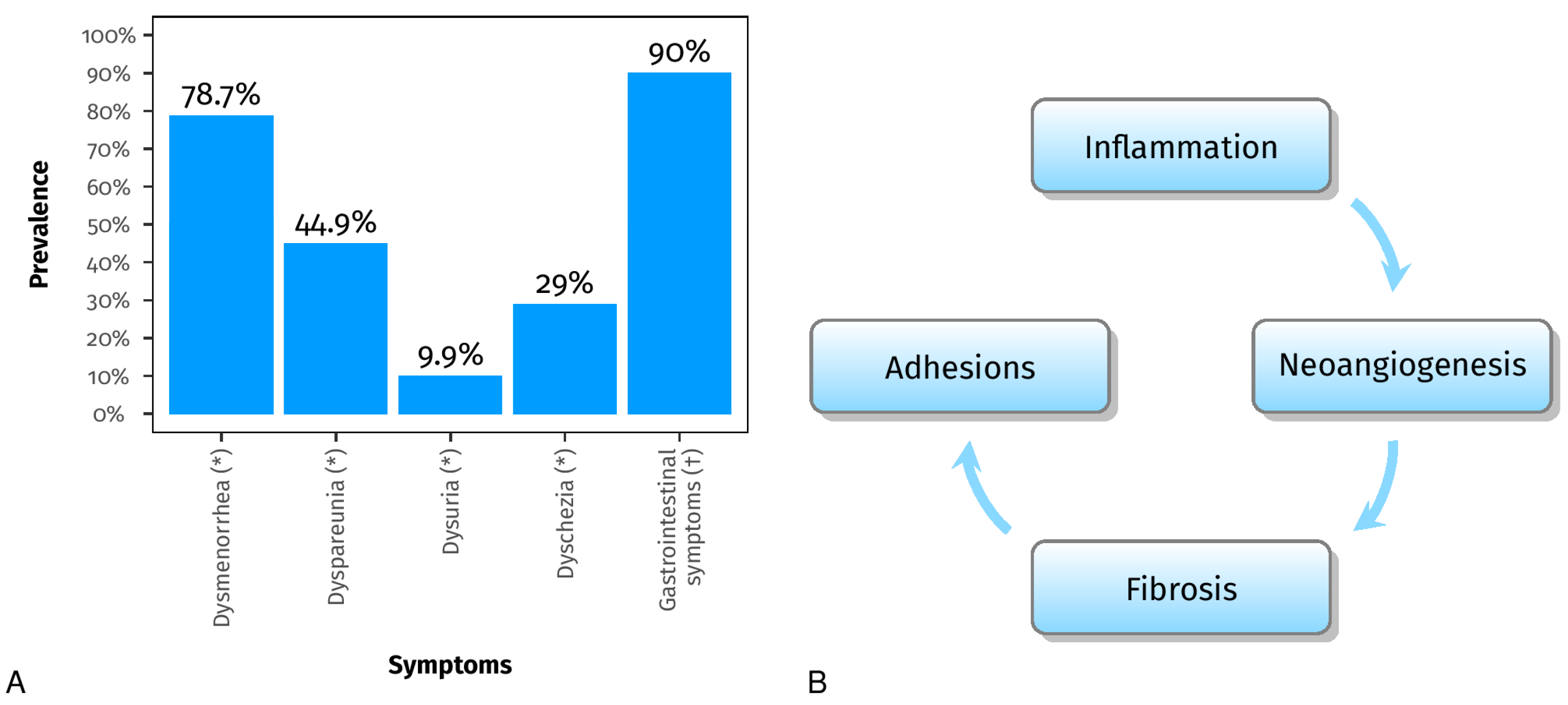
3. Mechanisms Underlying Endometriosis
4. The Bidirectional Relationship between Endometriosis and Microbiota
4.1. Gut Microbiota and Estrogens
4.2. Dysbiosis and Chronic Inflammation
4.3. Insights from Human and Animal Studies
| Study | N | Animal Species | Endometriosis Model | Sample | Technic | Aim and Conclusion |
|---|---|---|---|---|---|---|
| Bailey & Coe, 2002 [56] | 18 | Female Rhesus Monkeys (Macaca Mulatta) | Spontaneous occurring endometriosis, diagnosed with USG and MRI and confirmed by surgery and histology | Fecal samples | Coprocolture | Aim: demonstrate that monkeys have an altered profile of intestinal microflora, in particular altered Lactobacilli Conclusion: decreased Lactobacilli and increased gram-negative anaerobes and facultative anaerobes |
| Yuan et al., 2018 [66] | Cases: 16 Controls: 20 | C57BL6 mice | Induced: intraperitoneal injection of endometrial tissue from sacrificed donor mice | Fecal pellets | NGS Illumina: V4 16S rRNA | Aim: determine the changes in gut microbiota in a murine endometriosis model by 16S ribosomal-RNA gene sequencing Conclusion: Firmicutes/Bacteroidetes ratio was elevated in mice with endometriosis, indicating that endometriosis may induce dysbiosis |
| Chadchan et al., 2019 [62] | Cases: 5 with endometriosis treated with vehicle and 4 with endometriosis and treated with broad spectrum antibiotics Controls: 5 | C57BL/6 mice | Induced: autologous transplantation of endometrial tissue onto the peritoneal wall | Fecal pellets, peritoneal fluid, endometriotic lesions | NGS Illumina: V1-V9 16S rRNA | Aim: investigate if altering gut microbiota with antibiotic treatment has any impact on endometriosis progression Conclusion: oral antibiotic treatment is effective in reducing the progression of endometriosis and administering fecal material from mice with endometriosis via oral gavage restored both the growth of endometriotic lesions and inflammation |
| Cao et al., 2020 [71] | Cases: 24 Controls: 8 | Sprague Dawley rats | Induced: autologous transplantation of uterine tissue fragments onto the peritoneal wall | Fecal pellets | NGS Illumina: V3-V4 16S rRNA | Aim: investigate if letrozole and SFZYD can act on microbiota, inhibiting the progression of lesions Conclusion: Letrozole and SFZYD reduce the inflammatory response in both ectopic and eutopic endometrial tissues, which could be associated with the decrease in the Firmicutes/Bacteroidetes ratio. |
| Ni et al., 2020 [72] | Cases: 16 Controls: 20 | C57BL/6J mice | Induced: estrogen solution subcutaneous injection on days 1, 4, and 7, transplantation of endometrial fragments on day 8. Estrogen injection again on day 9, 11, and 14. After 3 weeks, mice were dissected to obtain faces from cecum. | Feces from cecum | NGS Illumina: V3-V4 16S rRNA | Aim: uncover the interaction between fecal metabolomics and gut microbiota in mice with endometriosis Conclusion: The abnormal fecal metabolites, particularly those related to secondary bile acid biosynthesis and the alpha-linolenic acid pathways, influenced by dysbiosis, may serve as distinctive features in mice with endometriosis and as potential markers for distinguishing the disease |
| Study | N | Age (Years) | Endometriosis Diagnosis Type | Sample | Technic | Aim and Conclusion |
|---|---|---|---|---|---|---|
| Khan et al., 2016 [73] | Cases: 32 Controls: 32 In each group 16 in treatment with GnRHa | 21–52 | Surgery and histology | Endometrial swabs and cystic fluid | NGS Illumina: 16S rRNA | Aim: investigate microbial colonization in intrauterine environment and cystic fluid Conclusion: presence of sub-clinical infections in intrauterine environment and cystic fluid of ovarian endometriomas. Potential additional side effect of GnRHa treatment in promoting silent intrauterine and/or ovarian infections (abundance of Streptococcaceae, Staphylococaceae, Enterobacteriaceae and lowered Lactobacillae in GnRHa treated women) |
| Akiyama et al., 2019 [74] | Cases: 30 Controls: 39 | 20–44 | Surgery and histology | Cervical Mucus | NGS Illumina: V5-V6 16S rRNA | Aim: investigating pattern of microbiota in the cervical mucus Conclusion: Enterobacteriaceae and Streptococcus were more commonly found in women with endometriosis |
| Ata et al., 2019 [61] | Cases: 14 Controls: 14 | 18–45 | Surgery and histology (only stage 3–4) | Stool sample Vaginal and endocervical swabs | NGS Illumina: V3- V4 16S rRNA | Aim: comparing gut, vaginal, and cervical microbiota in endometriosis vs. controls Conclusion: no differences in species level analysis, but they found a possible difference at genus level analysis |
| Chen et al., 2020 [75] | Cases: 20 endometriosis, 19 adenomyosis and 7 adenomyosis-endometriosis Controls: 36 | 18–45 | Surgery, histology, transvaginal ultrasound, and MRI | Cervical swabs and posterior fornix swabs | NGS Illumina: V3-V4 16S rRNA | Aim: create a microbiota profile model for endometriosis and investigate and identify significant microbiota associated with endometriosis or adenomyosis conditions. Conclusion: Higher prevalence of Atopobium in endometriosis-adenomysosis group |
| Hernandes et al., 2020 [63] | Cases: 10 Controls: 11 | 18–50 | Surgery and histology | Vaginal fluid, eutopic endometrium (collected by curettage), and endometrial lesion tissue samples (collected by surgery) | NGS Illumina: V3-V4 rRNA | Aim: Investigate and compare the microbiome profile Conclusion:
|
| Wei et al., 2020 [65] | Cases: 36 Controls: 14 | 23–44 | Surgery and histology | Lower reproductive tract swabs: lower third of the vagina, posterior vaginal fornix, cervical mucus Upper reproductive tract samples: surgery (endometrial and peritoneal lavage) | NGS Ion Torrent PGM: V4-V5 16S rRNA | Aim: study the flora distribution and bacterial community across the upper and lower reproductive tract Conclusion: shift in microbiota distribution starting from the cervical samples (microbiota in cervical samples as an indicator for the risk of endometriosis) and progressively increasing upward the reproductive tract, decreased Lactobacillus in lower tract, enriched Sphingobium sp. and Pseudomonas viridiflava in endometrium and peritoneal fluid |
| Khan et al., 2021 [69] | Cases: 53 (21 untreated, 11 GnRHa, 15 LVFX, 6 LVFX+ GnRHa) Controls: 47 (11 untreated, 12 GnRHa, 10 LVFX, 14 LVFX+ GnRHa | 18–51 | Surgery and histology | Endometrial samples | NGS Illumina: V5-V6 16S rRNA Immunohistochimical analysis: Ab against CD138, CD68, Ki-67, and CD31 | Aim: demonstrate the hypothesis that antibiotic treatment with or without GnRHa may decrease intrauterine infection with consequent decrease in tissue inflammation, cell proliferation and angiogenesis in human endometriosis Conclusion: Decreased Gardnerella, Prevotella, Acidibactor, Atopobium, Megasphaera, and Bradyrhizobium in patients with endometriosis in treatment with LVFX or LVFX + GnRHa, reduced occurrence rate of chronic endometritis after GnRHa + LVFX treatment comparison to GnRHa treatment group and decreased CD68, Ki-67, and CD31 |
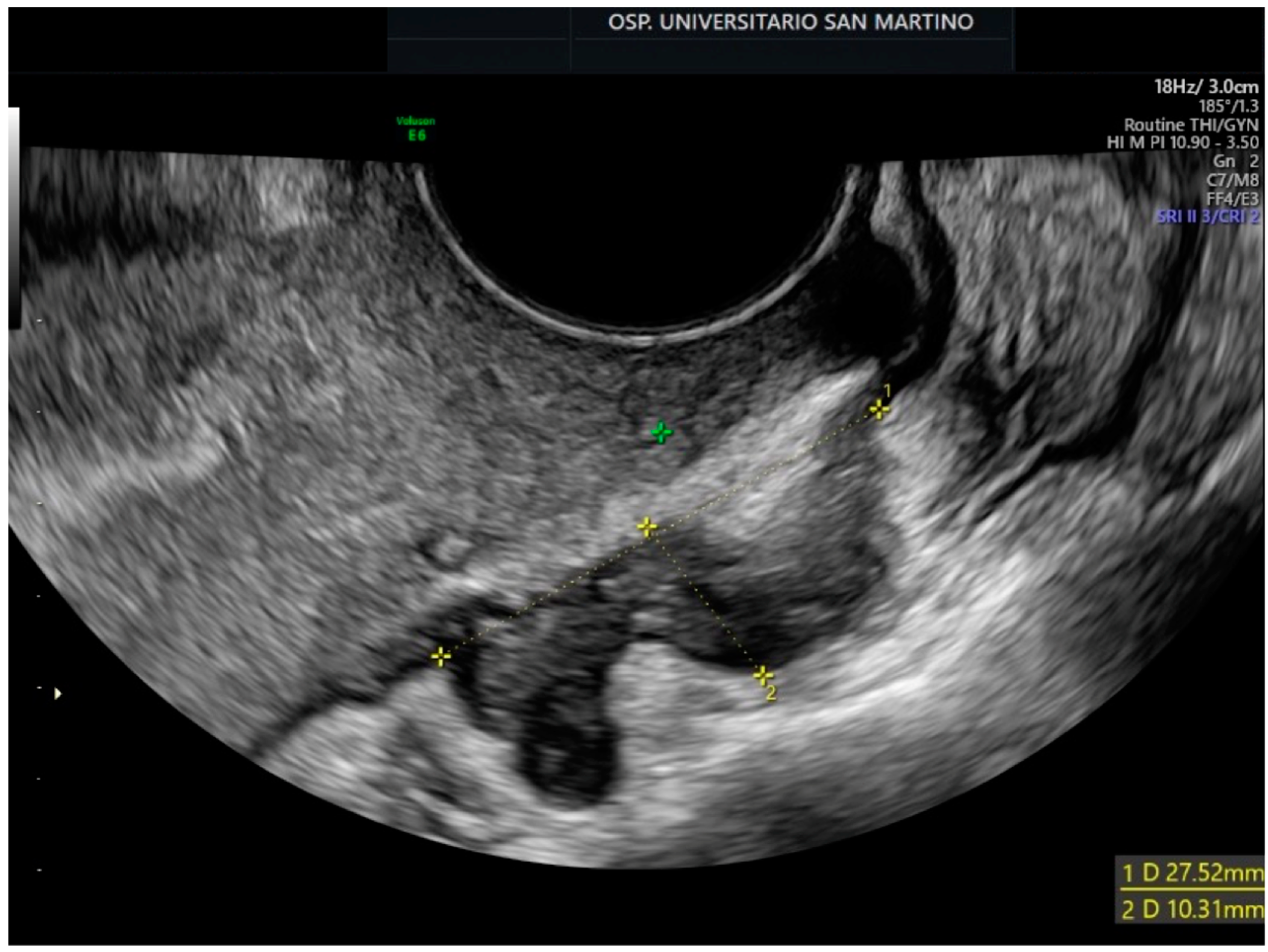
5. Microbiome Testing: A Promising Non-Invasive Approach for Endometriosis Diagnosis
6. Restoring Gut Microbiota Balance in Endometriosis: The Potential of Probiotics as a Therapeutic Approach
7. Role of Intestinal Permeability in Endometriosis-Related Gastrointestinal Symptoms
8. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Giudice, L.C.; Kao, L.C. Endometriosis. Lancet 2004, 364, 1789–1799. [Google Scholar] [CrossRef]
- Ahn, S.H.; Monsanto, S.P.; Miller, C.; Singh, S.S.; Thomas, R.; Tayade, C. Pathophysiology and Immune Dysfunction in Endometriosis. BioMed. Res. Int. 2015, 2015, 795976. [Google Scholar] [CrossRef] [PubMed]
- Nisolle, M.; Donnez, J. Peritoneal endometriosis, ovarian endometriosis, and adenomyotic nodules of the rectovaginal septum are three different entities. Fertil. Steril. 1997, 68, 585–596. [Google Scholar] [CrossRef] [PubMed]
- Santulli, P.; Tran, C.; Gayet, V.; Bourdon, M.; Maignien, C.; Marcellin, L.; Pocate-Cheriet, K.; Chapron, C.; de Ziegler, D. Oligo-anovulation is not a rarer feature in women with documented endometriosis. Fertil. Steril. 2018, 110, 941–948. [Google Scholar] [CrossRef] [PubMed]
- Vercellini, P.; Parazzini, F.; Oldani, S.; Panazza, S.; Bramante, T.; Crosignani, P.G. Surgery: Adenomyosis at hysterectomy: A study on frequency distribution and patient characteristics. Hum. Reprod. 1995, 10, 1160–1162. [Google Scholar] [CrossRef] [PubMed]
- Xholli, A.; Londero, A.P.; Mattos, L.C.; Vujosevic, S.; Cagnacci, A. Gynaecological pathologies leading to emergency department admissions: A cross-sectional study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2023, 282, 38–42. [Google Scholar] [CrossRef]
- Nnoaham, K.E.; Hummelshoj, L.; Webster, P.; d’Hooghe, T.; de Cicco Nardone, F.; de Cicco Nardone, C.; Jenkinson, C.; Kennedy, S.H.; Zondervan, K.T. Impact of endometriosis on quality of life and work productivity: A multicenter study across ten countries. Fertil. Steril. 2011, 96, 366–373.e8. [Google Scholar] [CrossRef] [PubMed]
- Tai, F.-W.; Chang, C.Y.-Y.; Chiang, J.-H.; Lin, W.-C.; Wan, L. Association of Pelvic Inflammatory Disease with Risk of Endometriosis: A Nationwide Cohort Study Involving 141,460 Individuals. J. Clin. Med. 2018, 7, 379. [Google Scholar] [CrossRef]
- Domenis, R.; Pilutti, D.; Orsaria, M.; Marzinotto, S.; Candotti, V.; Bosisio, G.; Bulfoni, M.; Ruaro, M.E.; Di Loreto, C.; Della Mea, V.; et al. Expression and modulation of S100A4 protein by human mast cells. Cell. Immunol. 2018, 332, 85–93. [Google Scholar] [CrossRef]
- Mariuzzi, L.; Domenis, R.; Orsaria, M.; Marzinotto, S.; Londero, A.P.; Bulfoni, M.; Candotti, V.; Zanello, A.; Ballico, M.; Mimmi, M.C.; et al. Functional expression of aryl hydrocarbon receptor on mast cells populating human endometriotic tissues. Lab. Investig. 2016, 96, 959–971. [Google Scholar] [CrossRef]
- Jiang, I.; Yong, P.J.; Allaire, C.; Bedaiwy, M.A. Intricate Connections between the Microbiota and Endometriosis. Int. J. Mol. Sci. 2021, 22, 5644. [Google Scholar] [CrossRef]
- DiVasta, A.D.; Vitonis, A.F.; Laufer, M.R.; Missmer, S.A. Spectrum of symptoms in women diagnosed with endometriosis during adolescence vs adulthood. Am. J. Obstet. Gynecol. 2018, 218, 324.e1–324.e11. [Google Scholar] [CrossRef] [PubMed]
- Bloski, T.; Pierson, R. Endometriosis and chronic pelvic pain: Unraveling the mystery behind this complex condition. Nurs. Women’s Health 2008, 12, 382–395. [Google Scholar] [CrossRef] [PubMed]
- Maroun, P.; Cooper, M.J.W.; Reid, G.D.; Keirse, M.J.N.C. Relevance of gastrointestinal symptoms in endometriosis. Aust. N. Z. J. Obstet. Gynaecol. 2009, 49, 411–414. [Google Scholar] [CrossRef] [PubMed]
- Luscombe, G.M.; Markham, R.; Judio, M.; Grigoriu, A.; Fraser, I.S. Abdominal bloating: An under-recognized endometriosis symptom. J. Obstet. Gynaecol. Can. 2009, 31, 1159–1171. [Google Scholar] [CrossRef]
- Svensson, A.; Brunkwall, L.; Roth, B.; Orho-Melander, M.; Ohlsson, B. Associations between endometriosis and gut microbiota. Reprod. Sci. 2021, 28, 2367–2377. [Google Scholar] [CrossRef]
- Martin, D.H. The Microbiota of the Vagina and Its Influence on Women’s Health and Disease. Am. J. Med. Sci. 2012, 343, 2–9. [Google Scholar] [CrossRef]
- Nelson, D.B.; Rockwell, L.C.; Prioleau, M.D.; Goetzl, L. The role of the bacterial microbiota on reproductive and pregnancy health. Anaerobe 2016, 42, 67–73. [Google Scholar] [CrossRef]
- Qin, R.; Tian, G.; Liu, J.; Cao, L. The gut microbiota and endometriosis: From pathogenesis to diagnosis and treatment. Front. Cell. Infect. Microbiol. 2022, 12, 1069557. [Google Scholar] [CrossRef]
- Sinaii, N.; Plumb, K.; Cotton, L.; Lambert, A.; Kennedy, S.; Zondervan, K.; Stratton, P. Differences in characteristics among 1000 women with endometriosis based on extent of disease. Fertil. Steril. 2008, 89, 538–545. [Google Scholar] [CrossRef]
- Knapp, V.J. How old is endometriosis? Late 17th- and 18th-century European descriptions of the disease. Fertil. Steril. 1999, 72, 10–14. [Google Scholar] [PubMed]
- Sampson, J.A. Peritoneal endometriosis due to the menstrual dissemination of endometrial tissue into the peritoneal cavity. Am. J. Obstet. Gynecol. 1927, 14, 422–469. [Google Scholar] [CrossRef]
- Seli, E.; Arici, A. Endometriosis: Interaction of immune and endocrine systems. Semin. Reprod. Med. 2003, 21, 135–144. [Google Scholar] [PubMed]
- Halban, J. Hysteroadenosis metastatica Die lymphogene Genese der sog. Adenofibromatosis heterotopica. Arch. Gynecol. 1925, 124, 457–482. [Google Scholar] [CrossRef]
- Halban, J. Metastatic hysteroadenosis. Klin. Wchnschr. 1924, 57, 1205–1214. [Google Scholar]
- Taylor, H.S. Endometrial cells derived from donor stem cells in bone marrow transplant recipients. JAMA 2004, 292, 81–85. [Google Scholar] [CrossRef]
- Du, H.; Taylor, H.S. Stem cells and reproduction. Curr. Opin. Obstet. Gynecol. 2010, 22, 235–241. [Google Scholar] [CrossRef]
- Schüring, A.N.; Dahlhues, B.; Korte, A.; Kiesel, L.; Titze, U.; Heitkötter, B.; Ruckert, C.; Götte, M. The endometrial stem cell markers notch-1 and numb are associated with endometriosis. Reprod. Biomed. Online 2018, 36, 294–301. [Google Scholar] [CrossRef]
- Strauß, T.; Greve, B.; Gabriel, M.; Achmad, N.; Schwan, D.; Espinoza-Sanchez, N.A.; Laganà, A.S.; Kiesel, L.; Poutanen, M.; Götte, M.; et al. Impact of Musashi-1 and Musashi-2 Double Knockdown on Notch Signaling and the Pathogenesis of Endometriosis. Int. J. Mol. Sci. 2022, 23, 2851. [Google Scholar] [CrossRef]
- Meyer, R. Zur Frage der heterotopen Epithelwucherung, insbesondere des Peritonealepithels und in den Ovarien. Virchows Arch. Pathol. Anat. Physiol. Klin. Med. 1924, 250, 595–610. [Google Scholar] [CrossRef]
- Elias, M.H.; Lazim, N.; Sutaji, Z.; Abu, M.A.; Karim, A.K.A.; Ugusman, A.; Syafruddin, S.E.; Mokhtar, M.H.; Ahmad, M.F. HOXA10 DNA Methylation Level in the Endometrium Women with Endometriosis: A Systematic Review. Biology 2023, 12, 474. [Google Scholar] [CrossRef] [PubMed]
- Scutiero, G.; Iannone, P.; Bernardi, G.; Bonaccorsi, G.; Spadaro, S.; Volta, C.A.; Greco, P.; Nappi, L. Oxidative Stress and Endometriosis: A Systematic Review of the Literature. Oxidative Med. Cell. Longev. 2017, 2017, 7265238. [Google Scholar] [CrossRef] [PubMed]
- Vinatier, D.; Orazi, G.; Cosson, M.; Dufour, P. Theories of endometriosis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2001, 96, 21–34. [Google Scholar] [CrossRef]
- Biasioli, A.; Londero, A.P.; Orsaria, M.; Scrimin, F.; Mangino, F.P.; Bertozzi, S.; Mariuzzi, L.; Cagnacci, A. Atypical polypoid adenomyoma follow-up and management: Systematic review of case reports and series and meta-analysis. Medicine 2020, 99, e20491. [Google Scholar] [CrossRef] [PubMed]
- Didziokaite, G.; Biliute, G.; Gudaite, J.; Kvedariene, V. Oxidative Stress as a Potential Underlying Cause of Minimal and Mild Endometriosis-Related Infertility. Int. J. Mol. Sci. 2023, 24, 3809. [Google Scholar] [CrossRef] [PubMed]
- Kruitwagen, R.F.; Poels, L.G.; Willemsen, W.N.; Jap, P.H.; Thomas, C.M.; Rolland, R. Retrograde seeding of endometrial epithelial cells by uterine-tubal flushing. Fertil. Steril. 1991, 56, 414–420. [Google Scholar] [CrossRef] [PubMed]
- Halme, J.; Hammond, M.G.; Hulka, J.F.; Raj, S.G.; Talbert, L.M. Retrograde menstruation in healthy women and in patients with endometriosis. Obstet. Gynecol. 1984, 64, 151–154. [Google Scholar]
- Guo, S.-W. Emerging drugs for endometriosis. Expert Opin. Emerg. Drugs 2008, 13, 547–571. [Google Scholar] [CrossRef]
- Vercellini, P.; Crosignani, P.; Somigliana, E.; Viganò, P.; Frattaruolo, M.P.; Fedele, L. ‘Waiting for Godot’: A commonsense approach to the medical treatment of endometriosis. Hum. Reprod. 2010, 26, 3–13. [Google Scholar] [CrossRef]
- Vercellini, P.; Somigliana, E.; Viganò, P.; Abbiati, A.; Barbara, G.; Fedele, L. Chronic pelvic pain in women: Etiology, pathogenesis and diagnostic approach. Gynecol. Endocrinol. 2009, 25, 149–158. [Google Scholar] [CrossRef]
- I Lebovic, D.; Mueller, M.D.; Taylor, R.N. Immunobiology of endometriosis. Fertil. Steril. 2001, 75, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Laschke, M.W.; Menger, M.D. The gut microbiota: A puppet master in the pathogenesis of endometriosis? Am. J. Obstet. Gynecol. 2016, 215, 68.e1–68.e4. [Google Scholar] [CrossRef] [PubMed]
- Zhu, S.; Jiang, Y.; Xu, K.; Cui, M.; Ye, W.; Zhao, G.; Jin, L.; Chen, X. The progress of gut microbiome research related to brain disorders. J. Neuroinflamm. 2020, 17, 25. [Google Scholar] [CrossRef] [PubMed]
- Talwar, C.; Singh, V.; Kommagani, R. The gut microbiota: A double-edged sword in endometriosis. Biol. Reprod. 2022, 107, 881–901. [Google Scholar] [CrossRef]
- Possemiers, S.; Bolca, S.; Verstraete, W.; Heyerick, A. The intestinal microbiome: A separate organ inside the body with the metabolic potential to influence the bioactivity of botanicals. Fitoterapia 2011, 82, 53–66. [Google Scholar] [CrossRef]
- Elkafas, H.; Walls, M.; Al-Hendy, A.; Ismail, N. Gut and genital tract microbiomes: Dysbiosis and link to gynecological disorders. Front. Cell. Infect. Microbiol. 2022, 12, 1059825. [Google Scholar] [CrossRef]
- Wei, Y.; Tan, H.; Yang, R.; Yang, F.; Liu, D.; Huang, B.; OuYang, L.; Lei, S.; Wang, Z.; Jiang, S.; et al. Gut dysbiosis-derived β-glucuronidase promotes the development of endometriosis. Fertil. Steril. 2023, 120, 682–694. [Google Scholar] [CrossRef]
- Pai, A.H.-Y.; Wang, Y.-W.; Lu, P.-C.; Wu, H.-M.; Xu, J.-L.; Huang, H.-Y. Gut Microbiome–Estrobolome Profile in Reproductive-Age Women with Endometriosis. Int. J. Mol. Sci. 2023, 24, 16301. [Google Scholar] [CrossRef]
- Troha, N.; Rižner, T.L. Medsebojni vpliv estrogenov in mikrobioma prebavil in rodil. Slov. Med. J. 2023, 92, 335–344. [Google Scholar] [CrossRef]
- Baker, J.M.; Al-Nakkash, L.; Herbst-Kralovetz, M.M. Estrogen–gut microbiome axis: Physiological and clinical implications. Maturitas 2017, 103, 45–53. [Google Scholar] [CrossRef]
- E Salliss, M.; Farland, L.V.; Mahnert, N.D.; Herbst-Kralovetz, M.M. The role of gut and genital microbiota and the estrobolome in endometriosis, infertility and chronic pelvic pain. Hum. Reprod. Updat. 2021, 28, 92–131. [Google Scholar] [CrossRef] [PubMed]
- Beaud, D.; Tailliez, P.; Anba-Mondoloni, J. Genetic characterization of the β-glucuronidase enzyme from a human intestinal bacterium, Ruminococcus gnavus. Microbiology 2005, 151, 2323–2330. [Google Scholar] [CrossRef] [PubMed]
- Leonardi, M.; Hicks, C.; El-Assaad, F.; El-Omar, E.; Condous, G. Endometriosis and the microbiome: A systematic review. BJOG Int. J. Obstet. Gynaecol. 2019, 127, 239–249. [Google Scholar] [CrossRef] [PubMed]
- Qi, X.; Yun, C.; Pang, Y.; Qiao, J. The impact of the gut microbiota on the reproductive and metabolic endocrine system. Gut Microbes 2021, 13, 1894070. [Google Scholar] [CrossRef] [PubMed]
- Hu, S.; Ding, Q.; Zhang, W.; Kang, M.; Ma, J.; Zhao, L. Gut microbial beta-glucuronidase: A vital regulator in female estrogen metabolism. Gut Microbes 2023, 15, 2236749. [Google Scholar] [CrossRef] [PubMed]
- Bailey, M.T.; Coe, C.L. Endometriosis is associated with an altered profile of intestinal microflora in female rhesus monkeys. Hum. Reprod. 2002, 17, 1704–1708. [Google Scholar] [CrossRef]
- Sobstyl, A.; Chałupnik, A.; Mertowska, P.; Grywalska, E. How Do Microorganisms Influence the Development of Endometriosis? Participation of Genital, Intestinal and Oral Microbiota in Metabolic Regulation and Immunopathogenesis of Endometriosis. Int. J. Mol. Sci. 2023, 24, 10920. [Google Scholar] [CrossRef]
- Huang, L.; Liu, B.; Liu, Z.; Feng, W.; Liu, M.; Wang, Y.; Peng, D.; Fu, X.; Zhu, H.; Cui, Z.; et al. Gut microbiota exceeds cervical microbiota for early diagnosis of endometriosis. Front. Cell. Infect. Microbiol. 2021, 11, 788836. [Google Scholar] [CrossRef]
- Sakamoto, Y.; Harada, T.; Horie, S.; Iba, Y.; Taniguchi, F.; Yoshida, S.; Iwabe, T.; Terakawa, N. Tumor necrosis factor-α-induced interleukin-8 (IL-8) expression in endometriotic stromal cells, probably through nuclear factor-κB activation: Gonadotropin-releasing hormone agonist treatment reduced IL-8 expression. J. Clin. Endocrinol. Metab. 2003, 88, 730–735. [Google Scholar] [CrossRef]
- Khan, K.N.; Fujishita, A.; Kitajima, M.; Hiraki, K.; Nakashima, M.; Masuzaki, H. Intra-uterine microbial colonization and occurrence of endometritis in women with endometriosis. Hum. Reprod. 2014, 29, 2446–2456. [Google Scholar] [CrossRef]
- Ata, B.; Yildiz, S.; Turkgeldi, E.; Brocal, V.P.; Dinleyici, E.C.; Moya, A.; Urman, B. The endobiota study: Comparison of vaginal, cervical and gut microbiota between women with stage 3/4 endometriosis and healthy controls. Sci. Rep. 2019, 9, 2204. [Google Scholar] [CrossRef] [PubMed]
- Chadchan, S.B.; Cheng, M.; A Parnell, L.; Yin, Y.; Schriefer, A.; Mysorekar, I.U.; Kommagani, R. Antibiotic therapy with metronidazole reduces endometriosis disease progression in mice: A potential role for gut microbiota. Hum. Reprod. 2019, 34, 1106–1116. [Google Scholar] [CrossRef] [PubMed]
- Hernandes, C.; Silveira, P.; Rodrigues Sereia, A.F.; Christoff, A.P.; Mendes, H.; Valter de Oliveira, L.F.; Podgaec, S. Microbiome profile of deep endometriosis patients: Comparison of vaginal fluid, endometrium and lesion. Diagnostics 2020, 10, 163. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.-R.; Lee, J.-C.; Kim, S.-H.; Oh, Y.-S.; Chae, H.-D.; Seo, H.; Kang, C.-S.; Shin, T.-S. Altered Composition of Microbiota in Women with Ovarian Endometrioma: Microbiome Analyses of Extracellular Vesicles in the Peritoneal Fluid. Int. J. Mol. Sci. 2021, 22, 4608. [Google Scholar] [CrossRef] [PubMed]
- Wei, W.; Zhang, X.; Tang, H.; Zeng, L.; Wu, R. Microbiota composition and distribution along the female reproductive tract of women with endometriosis. Ann. Clin. Microbiol. Antimicrob. 2020, 19, 15. [Google Scholar] [CrossRef] [PubMed]
- Yuan, M.; Li, D.; Zhang, Z.; Sun, H.; An, M.; Wang, G. Endometriosis induces gut microbiota alterations in mice. Hum. Reprod. 2018, 33, 607–616. [Google Scholar] [CrossRef]
- Liu, Z.; Chen, P.; Luo, L.; Liu, Q.; Shi, H.; Yang, X. Causal effects of gut microbiome on endometriosis: A two-sample mendelian randomization study. BMC Women’s Health 2023, 23, 637. [Google Scholar] [CrossRef]
- Uzuner, C.; Mak, J.; El-Assaad, F.; Condous, G. The bidirectional relationship between endometriosis and microbiome. Front. Endocrinol. 2023, 14, 1110824. [Google Scholar] [CrossRef]
- Khan, K.N.; Fujishita, A.; Muto, H.; Masumoto, H.; Ogawa, K.; Koshiba, A.; Mori, T.; Itoh, K.; Teramukai, S.; Matsuda, K.; et al. Levofloxacin or gonadotropin releasing hormone agonist treatment decreases intrauterine microbial colonization in human endometriosis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2021, 264, 103–116. [Google Scholar] [CrossRef]
- Kalinkina, O.B.; Tezikov, Y.V.; Lipatov, I.S.; Aravina, O.R.; Morozova, O.N. Study of urogenital tract and gut microbiota in women with stage III and IV ovarian endometriosis. Perm Med. J. 2020, 37, 14–21. [Google Scholar] [CrossRef]
- Cao, Y.; Jiang, C.; Jia, Y.; Xu, D.; Yu, Y. Letrozole and the Traditional Chinese Medicine, Shaofu Zhuyu Decoction, Reduce Endometriotic Disease Progression in Rats: A Potential Role for Gut Microbiota. Evid.-Based Complement. Altern. Med. 2020, 2020, 3687498. [Google Scholar] [CrossRef] [PubMed]
- Ni, Z.; Sun, S.; Bi, Y.; Ding, J.; Cheng, W.; Yu, J.; Zhou, L.; Li, M.; Yu, C. Correlation of fecal metabolomics and gut microbiota in mice with endometriosis. Am. J. Reprod. Immunol. 2020, 84, e13307. [Google Scholar] [CrossRef] [PubMed]
- Khan, K.N.; Fujishita, A.; Masumoto, H.; Muto, H.; Kitajima, M.; Masuzaki, H.; Kitawaki, J. Molecular detection of intrauterine microbial colonization in women with endometriosis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2016, 199, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Akiyama, K.; Nishioka, K.; Khan, K.N.; Tanaka, Y.; Mori, T.; Nakaya, T.; Kitawaki, J. Molecular detection of microbial colonization in cervical mucus of women with and without endometriosis. Am. J. Reprod. Immunol. 2019, 82, e13147. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Gu, Z.; Zhang, W.; Jia, S.; Wu, Y.; Zheng, P.; Dai, Y.; Leng, J. Microbiome of the lower genital tract in Chinese women with endometriosis by 16s-rRNA sequencing technique: A pilot study. Ann. Transl. Med. 2020, 8, 1440. [Google Scholar] [CrossRef] [PubMed]
- Greene, R.; Stratton, P.; Cleary, S.D.; Ballweg, M.L.; Sinaii, N. Diagnostic experience among 4,334 women reporting surgically diagnosed endometriosis. Fertil. Steril. 2009, 91, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Iavarone, I.; Greco, P.F.; La Verde, M.; Morlando, M.; Torella, M.; de Franciscis, P.; Ronsini, C. Correlations between Gut Microbial Composition, Pathophysiological and Surgical Aspects in Endometriosis: A Review of the Literature. Medicina 2023, 59, 347. [Google Scholar] [CrossRef]
- Ser, H.-L.; Yong, S.-J.A.; Shafiee, M.N.; Mokhtar, N.M.; Ali, R.A.R. Current Updates on the Role of Microbiome in Endometriosis: A Narrative Review. Microorganisms 2023, 11, 360. [Google Scholar] [CrossRef]
- Chernukha, C.G.E.; Pronina, P.V.A.; Priputnevich, P.T.V.; Academician, V.I.; Kulakov National Medical Research Center of Obstetrics, Gynecology, and Perinatology, Ministry of Health of the Russian Federation, Moscow, Russia. Gut and genital microbiota in endometriosis. Akush. Ginekol. 2022, 8, 22–29. [Google Scholar] [CrossRef]
- Khan, K.N.; Kitajima, M.; Hiraki, K.; Yamaguchi, N.; Katamine, S.; Matsuyama, T.; Nakashima, M.; Fujishita, A.; Ishimaru, T.; Masuzaki, H. Escherichia coli contamination of menstrual blood and effect of bacterial endotoxin on endometriosis. Fertil. Steril. 2010, 94, 2860–2863.e3. [Google Scholar] [CrossRef]
- Norfuad, F.A.; Mokhtar, M.H.; Azurah, A.G.N. Beneficial Effects of Probiotics on Benign Gynaecological Disorders: A Review. Nutrients 2023, 15, 2733. [Google Scholar] [CrossRef] [PubMed]
- Singh, P.; Srivastava, R.K. Microbiota and its therapeutic implications in reproductive health and diseases. In Microbiome Therapeutics; Elsevier: Amsterdam, The Netherlands, 2023; pp. 355–386. Available online: https://linkinghub.elsevier.com/retrieve/pii/B9780323993364000033 (accessed on 3 December 2023).
- Xu, M.-Q.; Cao, H.-L.; Wang, W.-Q.; Wang, S.; Cao, X.-C.; Yan, F.; Wang, B.-M. Fecal microbiota transplantation broadening its application beyond intestinal disorders. World J. Gastroenterol. 2015, 21, 102–111. [Google Scholar] [CrossRef] [PubMed]
- Yalçın Bahat, P.; Ayhan, I.; Üreyen Özdemir, E.; İnceboz, Ü.; Oral, E. Dietary supplements for treatment of endometriosis: A review. Acta Biomed. Atenei Parm. 2022, 93, e2022159. [Google Scholar]
- Melkozerova, O.; Braslavskaya, E.; Mikhelson, A.; Okulova, E.; Avseenko, M. The role of the intestinal and reproductive tract microbiota in the progression and recurrence of genital endometriosis. Probl. Reproduktsii 2023, 29, 68. [Google Scholar] [CrossRef]
- Ni, Z.; Ding, J.; Zhao, Q.; Cheng, W.; Yu, J.; Zhou, L.; Sun, S.; Yu, C. Alpha-linolenic acid regulates the gut microbiota and the inflammatory environment in a mouse model of endometriosis. Am. J. Reprod. Immunol. 2021, 86, e13471. [Google Scholar] [CrossRef] [PubMed]
- Chiantera, V.; Laganà, A.S.; Basciani, S.; Nordio, M.; Bizzarri, M. A Critical Perspective on the Supplementation of Akkermansia muciniphila: Benefits and Harms. Life 2023, 13, 1247. [Google Scholar] [CrossRef] [PubMed]
- Sari, F.M.; Mirkalantari, S.; Nikoo, S.; Sepahvand, F.; Allahqoli, L.; Asadi, A.; Talebi, M. Potential of Lactobacillus acidophilus to modulate cytokine production by peripheral blood monocytes in patients with endometriosis. Iran. J. Microbiol. 2022, 14, 698–704. Available online: https://publish.kne-publishing.com/index.php/IJM/article/view/10965 (accessed on 3 December 2023).
- Khodaverdi, S.; Mohammadbeigi, R.; Khaledi, M.; Mesdaghinia, L.; Sharifzadeh, F.; Nasiripour, S.; Gorginzadeh, M. Beneficial Effects of Oral Lactobacillus on Pain Severity in Women Suffering from Endometriosis: A Pilot Placebo-Controlled Randomized. Clinical Trial. Int. J. Fertil. Steril. 2019, 13, 178–183. [Google Scholar]
- Molina, N.M.; Sola-Leyva, A.; Saez-Lara, M.J.; Plaza-Diaz, J.; Tubić-Pavlović, A.; Romero, B.; Clavero, A.; Mozas-Moreno, J.; Fontes, J.; Altmäe, S. New opportunities for endometrial health by modifying uterine microbial composition: Present or future? Biomolecules 2020, 10, 593. [Google Scholar] [CrossRef]
- Uchida, M.; Kobayashi, O. Effects of Lactobacillus gasseri OLL2809 on the Induced endometriosis in rats. Biosci. Biotechnol. Biochem. 2013, 77, 1879–1881. [Google Scholar] [CrossRef]
- Itoh, H.; Sashihara, T.; Hosono, A.; Kaminogawa, S.; Uchida, M. Interleukin-12 inhibits development of ectopic endometriotic tissues in peritoneal cavity via activation of NK cells in a murine endometriosis model. Cytotechnology 2011, 63, 133–141. [Google Scholar] [CrossRef] [PubMed]
- Putra, A.K.; Saadi, A.; Surono, I.S.; Ansori, A.N.M.; Nidom, R.V. The Downregulation of Pro-inflammatory Cytokine Interleukin-6 after Oral Administration of Lactobacillus plantarum IS-10506 in Mice Model for Endometriosis. Indian J. Anim. Res. 2023, 57, 620–625. Available online: http://arccjournals.com/journal/indian-journal-of-animal-research/BF-1536 (accessed on 3 December 2023). [CrossRef]
- Mohling, S.I.; Holcombe, J.; Furr, R.S. Intestinal Permeability and Endometriosis: A pilot investigation. J. Endometr. Uterine Disord. 2023, 3, 100045. [Google Scholar] [CrossRef]
- Camilleri, M. Leaky gut: Mechanisms, measurement and clinical implications in humans. Gut 2019, 68, 1516–1526. [Google Scholar] [CrossRef] [PubMed]
- Sapone, A.; de Magistris, L.; Pietzak, M.; Clemente, M.G.; Tripathi, A.; Cucca, F.; Lampis, R.; Kryszak, D.; Cartenì, M.; Generoso, M.; et al. Zonulin upregulation is associated with increased gut permeability in subjects with type 1 diabetes and their relatives. Diabetes 2006, 55, 1443–1449. [Google Scholar] [CrossRef] [PubMed]
- Heickman, L.K.W.; DeBoer, M.D.; Fasano, A. Zonulin as a potential putative biomarker of risk for shared type 1 diabetes and celiac disease autoimmunity. Diabetes/Metab. Res. Rev. 2020, 36, e3309. [Google Scholar] [CrossRef] [PubMed]
- Fasano, A. Zonulin and Its Regulation of Intestinal Barrier Function: The Biological Door to Inflammation, Autoimmunity, and Cancer. Physiol. Rev. 2011, 91, 151–175. [Google Scholar] [CrossRef] [PubMed]
- Paixão-Barradas, F.P.; Sousa, V.; Pereira, D.; Lopes, A.P.; Marques, I. Endometriosis and Crohn’s Disease Side by Side: A Case Report. J. Endometr. Pelvic Pain Disord. 2016, 8, 24–27. [Google Scholar] [CrossRef]
- Viganò, D.; Zara, F.; Usai, P. Irritable bowel syndrome and endometriosis: New insights for old diseases. Dig. Liver Dis. 2018, 50, 213–219. [Google Scholar] [CrossRef]
- Salmeri, N.; Sinagra, E.; Dolci, C.; Buzzaccarini, G.; Sozzi, G.; Sutera, M.; Candiani, M.; Ungaro, F.; Massimino, L.; Danese, S.; et al. Microbiota in Irritable Bowel Syndrome and Endometriosis: Birds of a Feather Flock Together—A Review. Microorganisms 2023, 11, 2089. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xholli, A.; Cremonini, F.; Perugi, I.; Londero, A.P.; Cagnacci, A. Gut Microbiota and Endometriosis: Exploring the Relationship and Therapeutic Implications. Pharmaceuticals 2023, 16, 1696. https://doi.org/10.3390/ph16121696
Xholli A, Cremonini F, Perugi I, Londero AP, Cagnacci A. Gut Microbiota and Endometriosis: Exploring the Relationship and Therapeutic Implications. Pharmaceuticals. 2023; 16(12):1696. https://doi.org/10.3390/ph16121696
Chicago/Turabian StyleXholli, Anjeza, Francesca Cremonini, Isabella Perugi, Ambrogio Pietro Londero, and Angelo Cagnacci. 2023. "Gut Microbiota and Endometriosis: Exploring the Relationship and Therapeutic Implications" Pharmaceuticals 16, no. 12: 1696. https://doi.org/10.3390/ph16121696
APA StyleXholli, A., Cremonini, F., Perugi, I., Londero, A. P., & Cagnacci, A. (2023). Gut Microbiota and Endometriosis: Exploring the Relationship and Therapeutic Implications. Pharmaceuticals, 16(12), 1696. https://doi.org/10.3390/ph16121696







