Preparation and Characterization of Ion-Sensitive Brimonidine Tartrate In Situ Gel for Ocular Delivery
Abstract
1. Introduction
2. Materials and Methods
2.1. Chemicals
2.2. Animals
2.3. Formulation Screening
2.3.1. Formulation Preparation
2.3.2. Gelation Ability
2.3.3. Viscosity Measurement
2.4. In Vitro Release Study
2.5. Permeation Studies
2.5.1. Dialysis Membrane Permeation Study
2.5.2. Ex Vivo Transcorneal and Transscleral Permeation Studies
2.5.3. Mathematical Modeling of Drug Release Kinetics
2.6. Pre-Corneal Retention Study
2.7. Ocular Irritation Studies
2.8. Stability Studies of BRT-ISG
2.9. Study on the Pharmacokinetics of Ophthalmic BRT-ISG in Rabbit Anterior Chamber
3. Results and Discussion
3.1. Formulation Screening
3.1.1. Gelation Ability
3.1.2. Viscosity Measurement
3.2. In Vitro Release Study
3.3. Permeation Studies
3.3.1. Dialysis Membrane Permeation Study
3.3.2. Ex Vivo Transcorneal and Transscleral Permeation Studies
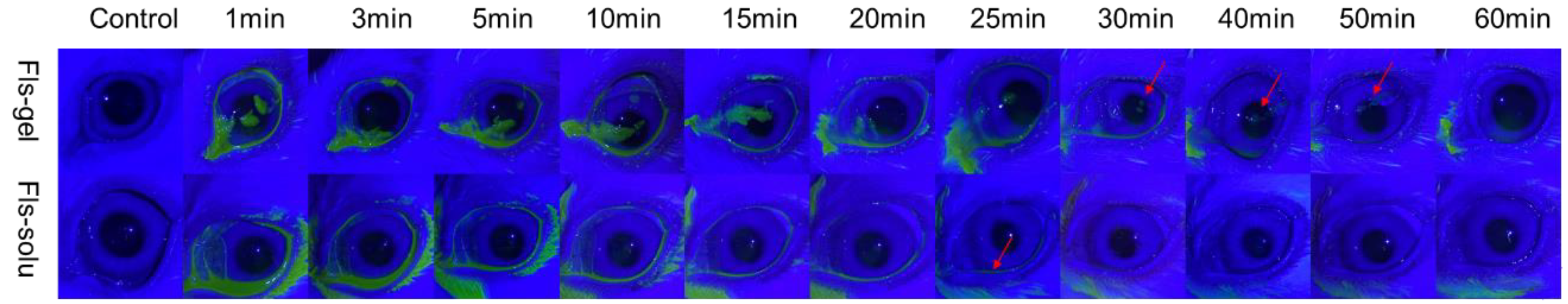
3.4. Pre-Corneal Retention Study
3.5. Ocular Irritation Studies
3.6. Stability Studies of BRT-ISG
3.7. Study on the Pharmacokinetics of Ophthalmic BRT-ISG in Rabbit Anterior Chamber
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhou, X.; Zhang, T.; Wu, J. Brimonidine enhances inhibitory postsynaptic activity of OFF- and ON-type retinal ganglion cells in a Wistar rat chronic glaucoma model. Exp. Eye Res. 2019, 189, 107833. [Google Scholar] [CrossRef] [PubMed]
- Cai, J.; Li, L.; Song, Y.; Xu, L.; Mao, Y.; Wang, H. Neuroprotective Effect of Brimonidine against Facial Nerve Crush Injury in Rats via Suppressing GFAP/PAF Activation and Neuroinflammation. ORL J. Otorhinolaryngol. Relat. Spec. 2021, 83, 449–456. [Google Scholar] [CrossRef] [PubMed]
- Litoriya, A.; Tiwari, U.S.; Pathak, R. Effect of various topical anti glaucoma drugs on cardiopulmonary system. A prospective study. Rom. J. Ophthalmol. 2019, 63, 142–145. [Google Scholar] [CrossRef] [PubMed]
- Krupin, T.; Liebmann, J.M.; Greenfield, D.S.; Ritch, R.; Gardiner, S.; Low-Pressure Glaucoma Study Group. A randomized trial of brimonidine versus timolol in preserving visual function: Results from the Low-Pressure Glaucoma Treatment Study. Am. J. Ophthalmol. 2011, 151, 671–681. [Google Scholar] [CrossRef] [PubMed]
- Chiang, B.; Kim, Y.C.; Doty, A.C.; Grossniklaus, H.E.; Schwendeman, S.P.; Prausnitz, M.R. Sustained reduction of intraocular pressure by supraciliary delivery of brimonidine-loaded poly(lactic acid) microspheres for the treatment of glaucoma. J. Control. Release 2016, 228, 48–57. [Google Scholar] [CrossRef]
- Castro, B.; Fulgêncio, G.; Domingos, L.C.; Cotta, O.; Fialho, S.L. Positively charged polymeric nanoparticles improve ocular penetration of tacrolimus after topical administration. J. Drug Deliv. Sci. Technol. 2020, 60, 101912. [Google Scholar] [CrossRef]
- Sun, J.; Zhou, Z. A novel ocular delivery of brinzolamide based on gellan gum: In vitro and in vivo evaluation. Drug Des. Dev. Ther. 2018, 12, 383–389. [Google Scholar] [CrossRef]
- Li, P.; Wang, S.; Chen, H.; Zhang, S.; Yu, S.; Li, Y.; Cui, M.; Pan, W.; Yang, X. A novel ion-activated in situ gelling ophthalmic delivery system based on κ-carrageenan for acyclovir. Drug Dev. Ind. Pharm. 2018, 44, 829–836. [Google Scholar] [CrossRef]
- Terreni, E.; Zucchetti, E.; Tampucci, S.; Burgalassi, S.; Monti, D.; Chetoni, P. Combination of nanomicellar technology and in situ gelling polymer as ocular drug delivery system (ODDS) for cyclosporine-A. Pharmaceutics 2021, 13, 192. [Google Scholar] [CrossRef]
- Sun, J.; Sun, X. Preparation of a novel tacrolimus ion sensitive ocular in situ gel and in vivo evaluation of curative effect of immune conjunctivitis. Pharm. Dev. Technol. 2022, 27, 399–405. [Google Scholar] [CrossRef]
- Gilani, S.J.; Jumah, M.; Zafar, A.; Imam, S.S.; Yasir, M.; Khalid, M.; Alshehri, S.; Ghuneim, M.M.; Albohairy, F.M. Formulation and evaluation of nano lipid carrier-based ocular gel system: Optimization to antibacterial activity. Gels 2022, 8, 255. [Google Scholar] [CrossRef] [PubMed]
- Tenci, M.; Rossi, S.; Giannino, V.; Vigani, B.; Sandri, G.; Bonferoni, M.C.; Daglia, M.; Longo, L.M.; Macelloni, C.; Ferrari, F. An in situ gelling system for the local treatment of inflammatory bowel disease (ibd). The loading of maqui (aristotelia chilensis) berry extract as an antioxidant and anti-inflammatory agent. Pharmaceutics 2019, 11, 611. [Google Scholar] [CrossRef] [PubMed]
- Destruel, P.L.; Zeng, N.; Brignole-Baudouin, F.; Douat, S.; Seguin, J.; Olivier, E.; Dutot, M.; Rat, P.; Dufaÿ, S.; Dufaÿ-Wojcicki, A.; et al. In situ gelling ophthalmic drug delivery system for the optimization of diagnostic and preoperative mydriasis: In vitro drug release, cytotoxicity and mydriasis pharmacodynamics. Pharmaceutics 2020, 12, 360. [Google Scholar] [CrossRef] [PubMed]
- Nair, A.B.; Shah, J.; Jacob, S.; Al-Dhubiab, B.E.; Sreeharsha, N.; Morsy, M.A.; Gupta, S.; Attimarad, M.; Shinu, P.; Venugopala, K.N. Experimental design, formulation and in vivo evaluation of a novel topical in situ gel system to treat ocular infections. PLoS ONE 2021, 16, e0248857. [Google Scholar] [CrossRef]
- Rupenthal, I.D.; Green, C.R.; Alany, R.G. Comparison of ion-activated in situ gelling systems for ocular drug delivery. Part 1: Physicochemical characterisation and in vitro release. Int. J. Pharm. 2011, 411, 69–77. [Google Scholar] [CrossRef]
- Fernández-Ferreiro, A.; González Barcia, M.; Gil-Martínez, M.; Vieites-Prado, A.; Lema, I.; Argibay, B.; Blanco Méndez, J.; Lamas, M.J.; Otero-Espinar, F.J. In vitro and in vivo ocular safety and eye surface permanence determination by direct and Magnetic Resonance Imaging of ion-sensitive hydrogels based on gellan gum and kappa-carrageenan. Eur. J. Pharm. Biopharm. 2015, 94, 342–351. [Google Scholar] [CrossRef]
- Wang, J.; Li, B.; Huang, D.; Norat, P.; Grannonico, M.; Cooper, R.C.; Gui, Q.; Chow, W.N.; Liu, X.; Yang, H. Nano-in-Nano dendrimer gel particles for efficient topical delivery of antiglaucoma drugs into the eye. Chem. Eng. J. 2021, 425, 130498. [Google Scholar] [CrossRef]
- Sharma, P.K.; Chauhan, M.K. Optimization and characterization of brimonidine tartrate nanoparticles-loaded in situ gel for the treatment of glaucoma. Curr. Eye Res. 2021, 46, 1703–1716. [Google Scholar] [CrossRef]
- Barse, R.K.; Tagalpallewar, A.A.; Kokare, C.R.; Sharma, J.P.; Sharma, P.K. Formulation and ex vivo-in vivo evaluation of pH-triggered brimonidine tartrate in situ gel for the glaucoma treatment using application of 32 factorial design. Drug Dev. Ind. Pharm. 2018, 44, 800–807. [Google Scholar] [CrossRef]
- Pek, Y.S.; Wu, H.; Mohamed, S.T.; Ying, J.Y. Long-term subconjunctival delivery of brimonidine tartrate for glaucoma treatment using a microspheres/carrier system. Adv. Healthc. Mater. 2016, 5, 2823–2831. [Google Scholar] [CrossRef]
- Peng, Y.F.; Huang, H.; Wang, H.; Zhu, Y.L.; Huang, B. Optimization of the preparation technology of brimonidine tartrate ophthalmic thermosensitive in situ gel by central composite design—Response surface methodology. China Pharm. 2014, 25, 4279–4281. [Google Scholar]
- Geethalakshmi, A.; Karki, R.; Jha, S.K.; Venkatesh, D.P.; Nikunj, B. Sustained ocular delivery of brimonidine tartrate using ion activated in situ gelling system. Curr. Drug Deliv. 2012, 9, 197–204. [Google Scholar] [CrossRef] [PubMed]
- Boyaci, E.; Lendor, S.; Bojko, B.; Reyes-Garcés, N.; Gómez-Ríos, G.A.; Olkowicz, M.; Diwan, M.; Palmer, M.; Hamani, C.; Pawliszyn, J. Comprehensive investigation of metabolic changes occurring in the rat brain hippocampus after fluoxetine administration using two complementary in vivo techniques: Solid phase microextraction and microdialysis. ACS Chem. Neurosci. 2020, 11, 3749–3760. [Google Scholar] [CrossRef] [PubMed]
- Jørgensen, A.R.; Hanberg, P.; Bue, M.; Thomassen, M.B.; Pedersen Jørgensen, N.; Stilling, M. Double-dose cefuroxime concentrations in bone, synovial fluid of the knee joint and subcutaneous adipose tissue—A randomised porcine microdialysis study. Eur. J. Pharm. Sci. 2021, 160, 105754. [Google Scholar] [CrossRef] [PubMed]
- El-Sherbeni, A.A.; Stocco, M.R.; Wadji, F.B.; Tyndale, R.F. Addressing the instability issue of dopamine during microdialysis: The determination of dopamine, serotonin, methamphetamine and its metabolites in rat brain. J. Chromatogr. A 2020, 1627, 461403. [Google Scholar] [CrossRef]
- Boddu, S.H.; Gunda, S.; Earla, R.; Mitra, A.K. Ocular microdialysis: A continuous sampling technique to study pharmacokinetics and pharmacodynamics in the eye. Bioanalysis 2010, 2, 487–507. [Google Scholar] [CrossRef]
- Li, J.; Tian, S.; Tao, Q.; Zhao, Y.; Gui, R.; Yang, F.; Zang, L.; Chen, Y.; Ping, Q.; Hou, D. Montmorillonite/chitosan nanoparticles as a novel controlled-release topical ophthalmic delivery system for the treatment of glaucoma. Int. J. Nanomed. 2018, 13, 3975–3987. [Google Scholar] [CrossRef]
- Xia, Z.F.; Tang, Z.; Wang, L.; Wang, Q.; Feng, H. Microdialysis recovery of brimonidine tartrate in vitro and in vivo. Chin. Pharm. J. 2018, 53, 1676–1681. [Google Scholar]
- Destruel, P.L.; Zeng, N.; Seguin, J.; Douat, S.; Rosa, F.; Brignole-Baudouin, F.; Dufaÿ, S.; Dufaÿ-Wojcicki, A.; Maury, M.; Mignet, N.; et al. Novel in situ gelling ophthalmic drug delivery system based on gellan gum and hydroxyethylcellulose: Innovative rheological characterization, in vitro and in vivo evidence of a sustained precorneal retention time. Int. J. Pharm. 2020, 574, 118734. [Google Scholar] [CrossRef]
- Kerdmanee, K.; Phaechamud, T.; Limsitthichaikoon, S. Thermoresponsive azithromycin-loaded niosome gel based on poloxamer 407 and hyaluronic interactions for periodontitis treatment. Pharmaceutics 2022, 14, 2032. [Google Scholar] [CrossRef]
- Sipos, B.; Budai-Szűcs, M.; Kókai, D.; Orosz, L.; Burián, K.; Csorba, A.; Nagy, Z.Z.; Balogh, G.T.; Csóka, I.; Katona, G. Erythromycin-loaded polymeric micelles: In situ gel development, in vitro and ex vivo ocular investigations. Eur. J. Pharm. Biopharm. 2022, 180, 81–90. [Google Scholar] [CrossRef] [PubMed]
- Okur, N.Ü.; Yozgatli, V.; Okur, M.E. In vitro-in vivo evaluation of tetrahydrozoline-loaded ocular in situ gels on rabbits for allergic conjunctivitis management. Drug Dev. Res. 2020, 81, 716–727. [Google Scholar] [CrossRef] [PubMed]
- Liang, Z.; Zhang, Z.; Yang, J.; Lu, P.; Zhou, T.; Li, J.; Zhang, J. Assessment to the antifungal effects in vitro and the ocular pharmacokinetics of solid-lipid nanoparticle in rabbits. Int. J. Nanomed. 2021, 16, 7847–7857. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.M.; Han, H.; Hong, H.K.; Park, J.H.; Park, K.H.; Kim, H.; Woo, S.J. Permeability of the retina and RPE-Choroid-Sclera to three ophthalmic drugs and the associated factors. Pharmaceutics 2021, 13, 655. [Google Scholar] [CrossRef]
- Kang, S.; Hou, S.; Chen, X.; Yu, D.G.; Wang, L.; Li, X.; Williams, G.R. Energy-saving electrospinning with a concentric teflon-core rod spinneret to create medicated nanofibers. Polymers 2020, 12, 2421. [Google Scholar] [CrossRef]
- Ortiz, A.C.; Yañez, O.; Salas-Huenuleo, E.; Morales, J.O. Development of a nanostructured lipid carrier (NLC) by a low-energy method, comparison of release kinetics and molecular dynamics simulation. Pharmaceutics 2021, 13, 531. [Google Scholar] [CrossRef]
- Sha, X.; Chan, L.; Fan, X.; Guo, P.; Chen, T.; Liu, L.; Zhong, J. Thermosensitive Tri-block polymer nanoparticle-hydrogel composites as Payloads of natamycin for antifungal therapy against fusarium solani. Int. J. Nanomed. 2022, 17, 1463–1478. [Google Scholar] [CrossRef]
- Shi, H.; Wang, Y.; Bao, Z.; Lin, D.; Liu, H.; Yu, A.; Lei, L.; Li, X.; Xu, X. Thermosensitive glycol chitosan-based hydrogel as a topical ocular drug delivery system for enhanced ocular bioavailability. Int. J. Pharm. 2019, 570, 118688. [Google Scholar] [CrossRef]
- Shen, T.; Yang, Z. In vivo and in vitro evaluation of in situ gel formulation of pemirolast potassium in allergic conjunctivitis. Drug Des. Dev. Ther. 2021, 15, 2099–2107. [Google Scholar] [CrossRef]
- Tang, Z.; Li, X.; Xu, H.; Chen, S.; Wang, B.; Wang, Q. HPLC-MS/MS studies of brimonidine in rabbit aqueous humor by microdialysis. Bioanalysis 2021, 13, 1487–1499. [Google Scholar] [CrossRef]
- Wang, J.; Zhao, F.; Liu, R.; Chen, J.; Zhang, Q.; Lao, R.; Wang, Z.; Jin, X.; Liu, C. Novel cationic lipid nanoparticles as an ophthalmic delivery system for multicomponent drugs: Development, characterization, in vitro permeation, in vivo pharmacokinetic, and molecular dynamics studies. Int. J. Nanomed. 2017, 12, 8115–8127. [Google Scholar] [CrossRef] [PubMed]
- Morsi, N.; Ibrahim, M.; Refai, H.; El Sorogy, H. Nanoemulsion-based electrolyte triggered in situ gel for ocular delivery of acetazolamide. Eur. J. Pharm. Sci. 2017, 104, 302–314. [Google Scholar] [CrossRef] [PubMed]
- Loftsson, T.; Stefánsson, E. Cyclodextrins and topical drug delivery to the anterior and posterior segments of the eye. Int. J. Pharm. 2017, 531, 413–423. [Google Scholar] [CrossRef]
- Mazyed, E.A.; Abdelaziz, A.E. Fabrication of transgelosomes for enhancing the ocular delivery of acetazolamide: Statistical optimization, in vitro characterization, and in vivo study. Pharmaceutics 2020, 12, 465. [Google Scholar] [CrossRef] [PubMed]
- Sai, N.; Dong, X.; Huang, P.; You, L.; Yang, C.; Liu, Y.; Wang, W.; Wu, H.; Yu, Y.; Du, Y.; et al. A novel gel-forming solution based on PEG-DSPE/Solutol HS 15 mixed micelles and gellan gum for ophthalmic delivery of curcumin. Molecules 2019, 25, 81. [Google Scholar] [CrossRef] [PubMed]
- Sonanis, M.C.; Rajput, A.P. Development and validation of a new stability indicating analytical method for the determination of related components of brimonidine tartrate in drug substances and drug product using UPLC. Int. J. Pharm. Pharm. Sci. 2011, 3, 145–150. [Google Scholar]
- Madhavi, A.; Naidu, A.; Rao, D.; Srinivasu, P. Development and validation of a new LC method for analysis of brimonidine tartrate and related compounds. Chromatographia 2009, 69, 1413–1419. [Google Scholar] [CrossRef]
- Acheampong, A.A.; Shackleton, M.; Tang-Liu, D.D. Comparative ocular pharmacokinetics of brimonidine after a single dose application to the eyes of albino and pigmented rabbits. Drug Metab. Dispos. Biol. Fate Chem. 1995, 23, 708–712. [Google Scholar]
- Acheampong, A.A.; Small, D.; Baumgarten, V.; Welty, D.; Tang-Liu, D. Formulation effects on ocular absorption of brimonidine in rabbit eyes. J. Ocul. Pharmacol. Ther. 2002, 18, 325–337. [Google Scholar] [CrossRef]







| Formulations | Gellan Gum/% | HPMC/% | Gelling Capacity |
|---|---|---|---|
| 1 | 0.3 | + | |
| 2 | 0.4 | ++ | |
| 3 | 0.45 | ++ | |
| 4 | 0.45 | 0.1 | ++ |
| 5 | 0.45 | 0.2 | ++ |
| 6 | 0.5 | ++ | |
| 7 | 0.6 | ++ |
| Methods | Zero-Order Equation | First-Order Equation | Higuchi Equation | Ritger–Peppas Equation | |
|---|---|---|---|---|---|
| R2 | R2 | R2 | R2 | n | |
| Dialysis bag model | 0.548 | 0. 963 | 0.680 | 0.804 | 0.157 |
| Dialysis membrane permeation model | 0.862 | 0.997 | 0.980 | 0.968 | 0.564 |
| Transscleral permeation model | 0.932 | 0.984 | 0.978 | 0.963 | 0.754 |
| Transcorneal permeation model | 0.978 | 0.985 | 0.992 | 0.980 | 0.950 |
| Temperature /°C | Time /Day | Appearance Characters | pH | Osmolarity /mOsmol/kg | Contents /% | Impurity Contents/% |
|---|---|---|---|---|---|---|
| 0 | light yellow, odorless and transparent | 6.74 ± 0.05 | 289.0 ± 1.0 | 99.96 ± 0.25 | Signal 0.0% All 0.0% | |
| 40 | 5 | light yellow, odorless and transparent | 6.72 ± 0.04 | 288.0 ± 2.6 | 100.51 ± 0.03 | |
| 10 | light yellow, odorless and transparent | 6.71 ± 0.03 | 292.0 ± 4.2 | 101.83 ± 0.52 | Signal 0.0% All 0.04% | |
| 60 | 5 | light yellow, odorless and transparent | 6.75 ± 0.03 | 296.0 ± 2.6 | 102.22 ± 0.05 | |
| 10 | light yellow, odorless and transparent | 6.79 ± 0.02 | 302.0 ± 4.0 | 100.67 ± 0.35 | Signal 0.0% All 0.02% | |
| 4500 lx ± 500 lx | 5 | light yellow, odorless and transparent | 6.73 ± 0.05 | 288.0 ± 1.5 | 99.40 ± 0.05 | |
| 10 | light yellow, odorless and transparent | 6.75 ± 0.03 | 292.0 ± 3.1 | 100.86 ± 0.22 | Signal 0.02% All 0.41% |
| Temperature /°C | Time /Month | Appearance Characters | pH | Osmolarity /mOsmol/kg | Contents /% | Impurity Contents/% |
|---|---|---|---|---|---|---|
| 0 | light yellow, odorless and transparent | 6.74 ± 0.05 | 289.0 ± 1.0 | 99.96 ± 0.25 | Signal 0.0% All 0.0% | |
| 40 | 1 | light yellow, odorless and transparent | 6.73 ± 0.02 | 296.0 ± 2.1 | 99.24 ± 0.86 | Signal 0.02% All 0.06% |
| 2 | light yellow, odorless and transparent | 6.75 ± 0.03 | 294.0 ± 1.5 | 99.11 ± 1.02 | Signal 0.05% All 0.14% | |
| 3 | light yellow, odorless and transparent | 6.79 ± 0.02 | 298.0 ± 2.5 | 100.46 ± 1.02 | Signal 0.06% All 0.15% | |
| 6 | light yellow, odorless and transparent | 6.85 ± 0.04 | 301.0 ± 2.9 | 100.55 ± 0.19 | Signal 0.14% All 0.33% |
| Parameter | Eye Drops | BRT−ISG | |
|---|---|---|---|
| AUC(0-t) | mg·min/L | 412.61 ± 204.31 | 1397.08 ± 444.57 ** |
| AUC(0-∞) | mg·min/L | 426.34 ± 212.54 | 1514.91 ± 504.58 ** |
| MRT(0-t) | min | 110.28 ± 18.17 | 140.06 ± 17.50 ** |
| MRT(0-∞) | min | 121.04 ± 20.02 | 165.31 ± 22.36 ** |
| t1/2 | min | 64.99 ± 19.18 | 75.60 ± 17.66 |
| Tmax | min | 60 ± 21.21 | 93.00 ± 28.98 ** |
| Cmax | mg/L | 3.06 ± 1.42 | 8.16 ± 2.62 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu, H.; Liu, Y.; Jin, L.; Chen, X.; Chen, X.; Wang, Q.; Tang, Z. Preparation and Characterization of Ion-Sensitive Brimonidine Tartrate In Situ Gel for Ocular Delivery. Pharmaceuticals 2023, 16, 90. https://doi.org/10.3390/ph16010090
Xu H, Liu Y, Jin L, Chen X, Chen X, Wang Q, Tang Z. Preparation and Characterization of Ion-Sensitive Brimonidine Tartrate In Situ Gel for Ocular Delivery. Pharmaceuticals. 2023; 16(1):90. https://doi.org/10.3390/ph16010090
Chicago/Turabian StyleXu, Haonan, Ye Liu, Lu Jin, Xu Chen, Xinghao Chen, Qiao Wang, and Zhan Tang. 2023. "Preparation and Characterization of Ion-Sensitive Brimonidine Tartrate In Situ Gel for Ocular Delivery" Pharmaceuticals 16, no. 1: 90. https://doi.org/10.3390/ph16010090
APA StyleXu, H., Liu, Y., Jin, L., Chen, X., Chen, X., Wang, Q., & Tang, Z. (2023). Preparation and Characterization of Ion-Sensitive Brimonidine Tartrate In Situ Gel for Ocular Delivery. Pharmaceuticals, 16(1), 90. https://doi.org/10.3390/ph16010090





